
A PRELIMINARY STUDY FOR A BIOMECHANICAL MODEL
OF THE RESPIRATORY SYSTEM
Jacques Saadé, Anne-Laure Didier, Romain Buttin, Jean-Michel Moreau
Michaël Beuve, Behzad Shariat
LIRIS CNRS UMR 5205, Université Claude Bernard Lyon 1, 43 Boulevard du 11 novembre 1918
69622 Villeurbanne, France
Pierre-Frédéric Villard
LORIA, Nancy University, 615 rue du Jardin Botanique, 54602 Villers les Nancy, France
Keywords: Biomechanics, Respiratory system, Finite element method, Motion.
Abstract: Tumour motion is an essential source of error for treatment planning in radiation therapy. This motion is
mostly due to patient respiration. To account for tumour motion, we propose a solution that is based on the
biomechanical modelling of the respiratory system. To compute deformations and displacements, we use
continuous mechanics laws solved with the finite element method. In this paper, we propose a preliminary
study of a complete model of the respiratory system including lungs, chest wall and a simple model of the
diaphragm. This feasibility study is achieved by using the data of a “virtual patient”. Results are in
accordance with the anatomic reality, showing the feasibility of a complete model of the respiratory system.
1 INTRODUCTION
Patients internal motions have large implications in
different domains such as imaging and treatment
(chirurgical operations or radiation therapy).
Thereby the respiratory motion reduces the
efficiency of radiotherapy benefits. Indeed, thoracic
and abdominal tumours can move and deform due to
respiration. It is then essential to know their position
and shape deformation to be able to optimize the
dose to tumour and healthy tissues. Lung tumours
are particularly concerned by this motion (Mori et
al, 2007; Seppenwoolde et al., 2002). Several
management strategies including breath holding
(Gagel et al, 2007; Wong et al, 1999), beam gating
(Ozhasoglu and Murphy, 2002) and tracking have
been discussed in the literature to account for
tumour displacement (Giraud et al, 2006). A
disadvantage of breath holding and beam gating is
that, part of the time, the beam is off. Another
disadvantage is that they do not take into account
some irregularities in the breathing cycle. Indeed,
both methods deduce tumour position from an
external breathing parameter (spirometry, abdominal
or thoracic height...). Ozhasoglu and Murphy (2002)
demonstrated that respiratory compensation
strategies that use an external breathing signal to
infer tumour position lack the ability to detect and
adapt to continuously changing characteristics of
respiratory motion during treatment. Other studies
(Shirato et al, 2006) show that the respiratory motion
has some non-reproducible aspects that need to be
taken into account during radiotherapy. This non-
reproducibility will be explained later in the
anatomy part. Tracking fiducial markers implanted
inside the tumour or tracking the tumour using the
CyberKnife® robotic radiosurgery system are
techniques that take into account the non-
reproducibility of the breathing cycle. While the
implantation of fiducial markers is an intrusive
method that may lead to medical complications such
as pneumothorax (Jiang, 2006), the CyberKnife®
system has also some inconveniences such like the
long treatment time requirement and the irradiation
of the patient by the tracking device.
Alternatively we propose a model based solution
that takes into account the non-reproducible aspects
of breathing motion: a biomechanical modelling of
the respiratory system monitored by at least two
external parameters (Thoracic motion and
509
Saadé J., Didier A., Buttin R., Moreau J., Beuve M., Shariat B. and Villard P. (2010).
A PRELIMINARY STUDY FOR A BIOMECHANICAL MODEL OF THE RESPIRATORY SYSTEM.
In Proceedings of the International Conference on Computer Vision Theory and Applications, pages 509-515
DOI: 10.5220/0002892405090515
Copyright
c
SciTePress
spirometry). Ribs and diaphragm displacements can
be computed out of thorax outer-surface motion and
spirometry measurements. Lungs deformations, and
then tumour displacements, can be deduced
considering the organ interactions. All deformations
and displacements are calculated using continuous
mechanics laws, solved with the finite element
method.
Another requirement, particularly important in
the context of hadrontherapy, is the ability to predict
not only tumour motion but also motions,
deformations and density changes of any tissue
traversed by the beam.
Our group has been active in the biomechanical
modelling of the respiratory system (Villard et al,
2005, Didier et al, 2007, 2009) and the
transformation of biomechanical data into 4D-CT
data (Villard et al, 2006). Previously, we have
validated a chest wall model based on rib kinematics
that enables the computation of rib displacements
out of thorax outer-surface motion (Didier et al,
2009). In this paper, we develop a feasibility study
of a diaphragm model. First, we summarize previous
studies concerning the biomechanical modelling of
the respiratory system. Then we expose a complete
model of the respiratory system, using a "virtual
patient" data, and the preliminary results on the
diaphragm and lung motions.
2 ANATOMY OF THE
RESPIRATORY SYSTEM
Lungs are passive structures that inflate under
muscles action. The increase of thoracic volume, due
to inspiratory muscles action, induces lung
expansion, leading to internal negative pressure and
consequently to inspiration. Contact of the lungs
with the ribcage and the diaphragm is maintained by
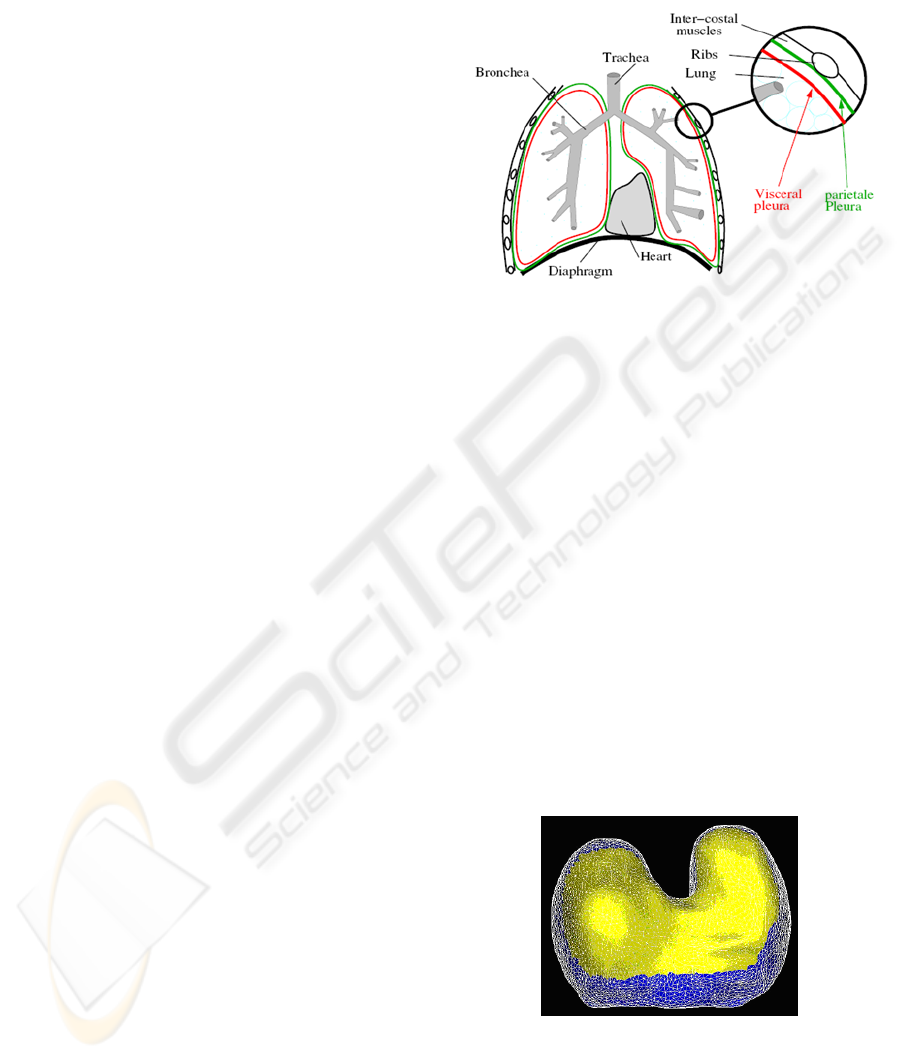
the pleura. The pleura is composed of two
membranes (figure 1): the first, referred to as
parietal, covers the chest wall, the mediastinum and
the diaphragm while the second, referred to as
visceral, covers the outer surface of the lungs.
The space in between the parietal and visceral
pleura, known as the pleural space, is filled with an
incompressible fluid which lubricates the pleural
space and allows the lungs to easily slide against the
chest wall and the diaphragm during their expansion.
Lungs mainly expand under the action of the
external intercostal muscles (EIM) and the
diaphragm. The role of the EIM is relatively
important in both quiet and forced respiration. They
are inserted between the ribs from the second to the
twelfth rib and they are responsible for the rib
elevation during inspiration.
Figure 1: Anatomy of the respiratory system.
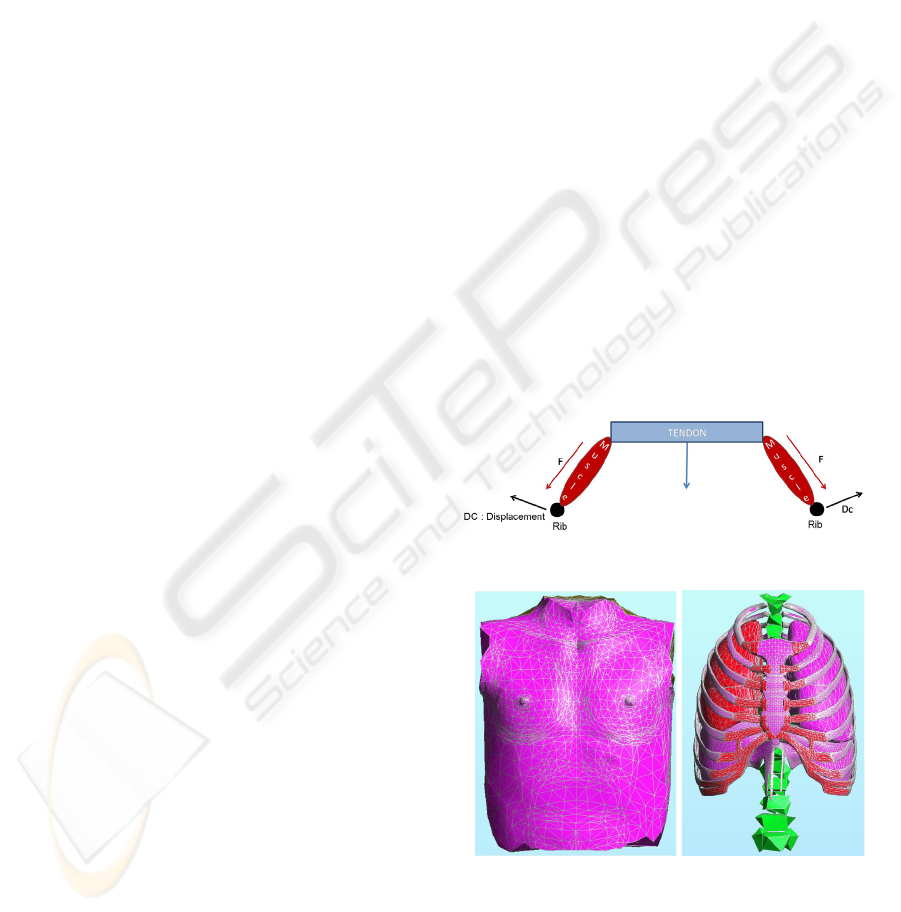
The diaphragm is a digastric muscle which
separates the thoracic and abdominal cavity. It is
composed of two domes (figure 2): the right dome
comes up to the fourth intercostal space whereas the
left dome remains below the fifth rib. The
diaphragm is constituted of a peripheral part
(muscular fibre) and a central tendon (figure 2). The
peripheral part is linked to the lower thoracic cavity
perimeter and has three major insertions: lumbar,
sternum and ribs. During inspiration, the muscular
contraction fibres bring down the central tendon.
This lowering increases the vertical diameter of the
thorax. As for the lungs, EIM action induces posto-
anterior and transversal inflation while the
diaphragm action causes vertical motion. The EIM
and the diaphragm may act independently, making
respiration a non-reproducible and an unpredictable
movement. Thereby, in general, lung motion cannot
be simply predicted by a correlation with one single
parameter.
Figure 2: A mesh representation of the diaphragm (upper
view). The central tendon is represented in yellow whereas
the peripheral part is in blue.
VISAPP 2010 - International Conference on Computer Vision Theory and Applications
510
3 BIOMECHANICAL
MODELLING OF THE
RESPIRATORY SYSTEM
In the past, several studies were achieved to model
the lung environment. A description of these studies
can be found in (Baudet et al. 2003), Villard et al.
(2005) and (Al-Mayah et al. 2007). Thus, we focus
on the more recent studies. (Villard et al. 2005) used
a patient's CT scan images to build the geometry of a
finite element lung model. They also studied lung
motion sensitivity to Poisson’s ratio, elastic modulus
(Young modulus) and contact conditions at the
pleura. It appeared that Poisson's ratio has an effect
on the amplitude and the orientation of the
displacements while Young modulus should be
carefully chosen because a change in its value may
either induce a faulty implementation of contact
conditions or increase the computing time needs.
(Brock et al. 2005) developed a platform to perform
multi-organ deformable image registration using
finite element modelling. The model was developed
using images from magnetic resonance (MR)
scanning. The lungs were included in this model and
good agreement was found between the finite
element simulation using orthogonal displacement
(OD) and the MR data. (Didier et al. 2007) showed
the significant role of the pleura and the necessity to
include its effect in the model. The role of the pleura
is simulated by applying contact conditions that
allow sliding on the lungs surface (contact without
friction). The results of this model were compared to
those of the OD model and showed an improvement
in predicting the position of the lungs while the
computing time requirement was higher. (Al-Mayah
et al. 2007) included the role of the pleura and two
other nonlinearities to the model (hyperelastic
nonlinear materials and nonlinear geometry due to
large displacements). They also added the chest wall
and the tumour to the model and achieved a good
precision on lung and tumour position. An
inconvenience of adding the nonlinearities was the
increase in the computation time needed to complete
the simulation. All the models mentioned above,
focused on deformable registration of soft tissues in
the thorax and did not invest in the bone tissues of
the rib cage. Going from the fact that the bones of
the rib cage can relatively be considered as rigid
bodies, (Didier et al. 2007) introduced a rigid
transformation that simulates the kinematic
behaviour of the rib cage intead of simulating the
action of each intercostal muscle. The
transformation is based on the Finite Helical Axis
(FHA) method. (Didier et al 2009) developped this
method in order to build a model of the chest wall.
This model proposed a correlation between ribs
motion and thorax-outer surface motion and
achieved a good precision on lungs position in the
upper thorax. This model is essential to enable
monitoring of lung motion out of thorax motion.
Thus, to be able to build a complete model of the
respiratory system and to include a second parameter
to the monitoring process of the lungs, we introduce
in this paper a biomechanical study of the diaphragm
and some preliminary results concerning a finite
element simulation of its motion.
4 DIAPHRAGM
BIOMECHANICAL MODEL
In order to build a complete model of the respiratory
system, the diaphragm is modeled and added to the
thorax and the lung models. As mentioned in the
anatomy part, the diaphragm is composed of a
peripheral part (muscular fibre) and a central tendon.
During inspiration, muscular fibres contract under
the action of a force F and the ribs undergo a
displacement Dc. Both actions cause the lowering of
the central tendon (figure 3).
Figure 3: An illustration of the diaphragm motion.
Figure 4: Anatomic elements of the model.
Since most thoracic medical imaging data cover
only the lungs and big parts of the diaphragm are not
included in the imaging protocol, we chose to carry
out our study on a “virtual model” data. We chose
A PRELIMINARY STUDY FOR A BIOMECHANICAL MODEL OF THE RESPIRATORY SYSTEM
511
the data of a virtual patient that include surface
meshes of the skin, the ribcage, the lungs and the
diaphragm. Figure 4 shows the different mesh data.
We apply on this geometrical model the
mechanical laws and boundary conditions and
material properties as follow.
4.1 Mechanical Behaviour Laws
We use continuous mechanics laws to compute the
deformations with a non-linear behaviour law that
allows large displacements. We considered elastic
materials. Calculations were made in the static mode
which means that only the initial and final states of
deformations are computed after the application of
boundary conditions.
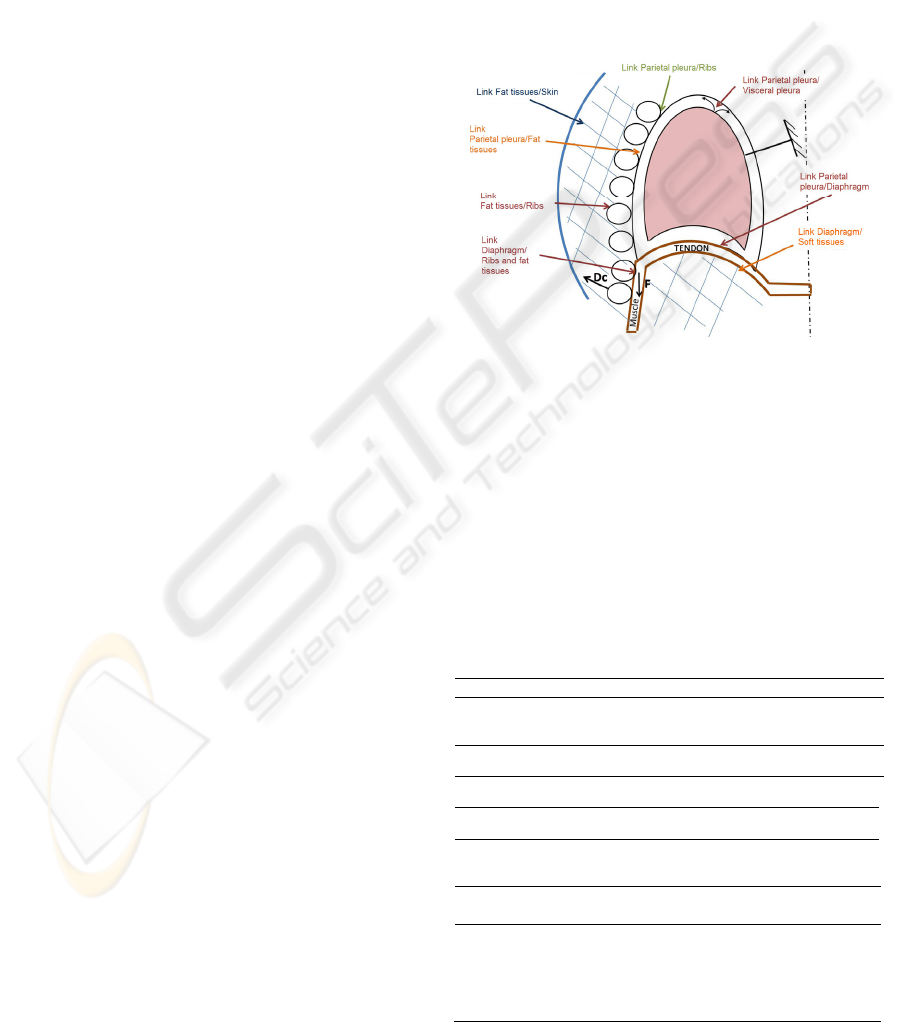
4.2 Boundary Conditions
The boundary conditions of our model are illustrated
in figure 5. They are the same as described in Didier
et al (2009), but we add the boundary conditions at
the diaphragm. Lungs are fixed near the trachea and
the pleura behaviour is simulated by applying
contact conditions allowing lungs surface to slide
against the chest wall (parietal pleura). These
contact conditions permit us to model the negative
intra-pleural pressure, and the sliding surface
represents the pleural fluid. According to reality,
parietal pleura is directly linked to the ribs or fat
tissue. A particular rigid transformation (Dc)
computed with the finite helical axis method is
applied to each rib. Ribs are directly linked to the fat
tissues which are also directly linked to the skin. The
diaphragm boundary conditions are as follow:
4.2.1 Diaphragm / Ribcage
As mentioned in the anatomy part, the diaphragm is
attached to the ribcage. In our simulation, we made
sure, in the attached region, that the corresponding
nodes were linked together.
4.2.2 Diaphragm / Fat tissues, Diaphragm /
Parietal Pleura
The diaphragm is directly linked to the fat tissues
and to the parietal pleura. This is an approximation
because normally the fat tissues can slide against the
diaphragm. The soft tissues that lie under the
diaphragm represent a resistance to the force that
tends to lower the diaphragm. They are simply
modelled like the fat tissues and they are affected the
same biomechanical parameters.
4.2.3 Contraction of the Muscular Fibres
To mimic the contraction, we apply the force F
illustrated on figure 5. This force should be parallel
to muscle orientation. In a first approximation, we
apply vertical (cranio-caudal) forces that are
oriented downwards. These forces are applied on
each node of the muscular part of the diaphragm.
This choice was motivated by the goal of this work,
which aims at demonstrating that it is possible to
propose a complete model of the respiratory system
as soon as a diaphragm model is available.
Figure 5: Boundary conditions.
4.3 Material Properties
Table 1 illustrates the biomechanical parameters
(Young modulus and Poisson’s ratio) of the lungs,
ribs, fat tissues, skin and diaphragm. The diaphragm
has two different parts (muscle and tendon) and each
part has different mechanical properties. All
parameters are taken from the bibliography
(Handriks, 2001; Promayon and Baconnier, 2008).
Table 1: The biomechanical properties of the different
organs.
Lungs Ribs & vertebrae
Young Modulus (MPa) 700*10
-6
5000
Poisson’s ratio 0.3 0.3
Fat tissues Skin
Young Modulus (MPa) 3 3
Poisson’s ratio 0.4 0.4
Diaphragm
Muscle)
Diaphragm
(Tendon)
Young Modulus (MPa) 5.32 10
Poisson’s ratio 0.3 0.3
VISAPP 2010 - International Conference on Computer Vision Theory and Applications
512
5 RESULTS
The “virtual patient” data are available for only one
respiratory state (we consider it arbitrarily as the
exhalation state). Because we need at least two
respiratory states to be able to compute rib
kinematics parameters (Didier et al, 2009), we apply
the rib parameters computed for a real patient in a
previous study (Didier et al, 2009). We apply the
force F as explained in 4.2.3, then we compare the
diaphragm at the initial state with the diaphragm at
the computed state to deduce its deformation and the
displacement fields. All calculations are made using
Code-Aster finite element software
(http://www.code-aster.org). The results
(deformations and displacement fields) are
visualised using GMSH software
(http://www.geuz.org/gmsh) and MESH (Aspert et
al, 2002).
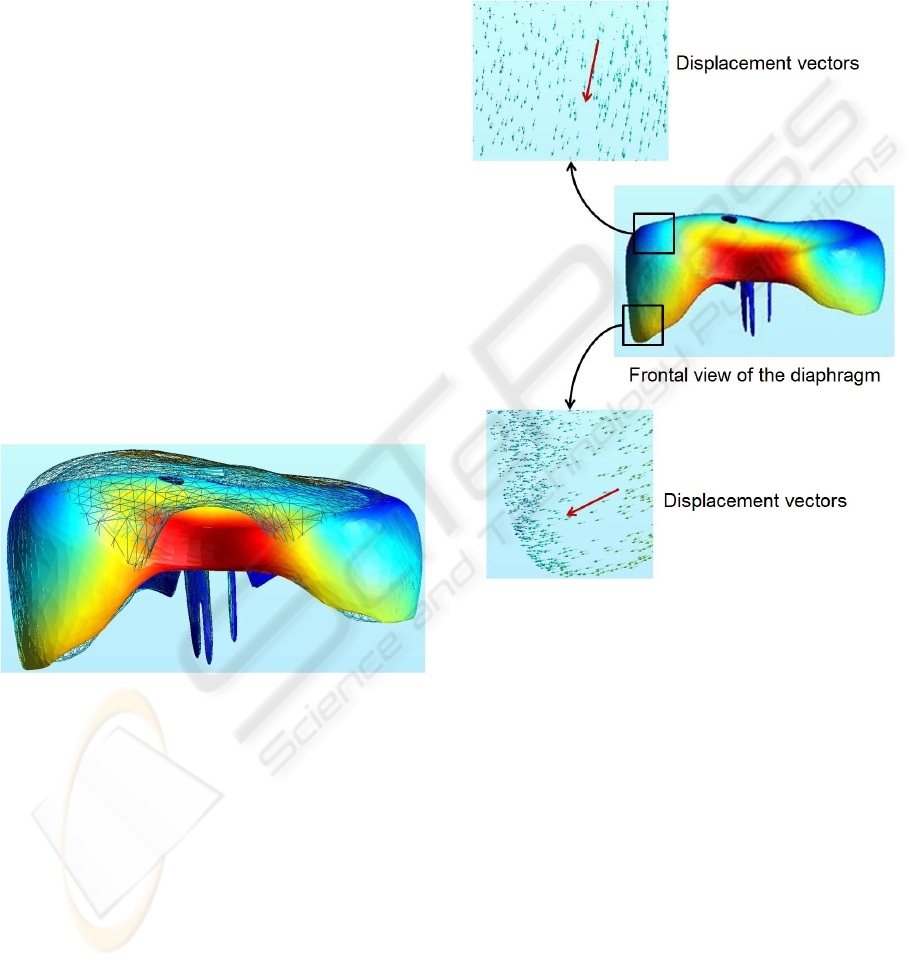
Figure 6 shows the diaphragm deformations
between the initial state (wireframe mesh) and the
computed final state (colored mesh). We can
observe that the central tendon goes down due to the
action of the force applied to the muscular part. We
observe also a lateral augmentation of the diaphragm
diameter due to the rib motion.
Figure 6: Frontal view of the diaphragm motion between
exhalation (wireframe mesh) and computed inhalation
state (coloured mesh). The deformations are illustrated in
colours on the computed mesh with red representing the
highest deformation value and blue its lowest value. The
colour scale is proportional to the motion amplitude.
Figure 7 represents the displacement vectors at
different locations on the diaphragm. The two red
vectors represent the mean orientation of the
displacement vectors at the level of the central
tendon (upper view) and at the level of the lower
muscular part (lower view). On the muscular part,
the displacement is lateral, oriented downwards
while the displacement on the level of the central
tendon tends to be more vertical. Globally, these
results are in accordance with the anatomy. Indeed,
the central tendon is relatively rigid, and therefore
less influenced by the ribs motion. However, after
the contraction of the muscular part, the central
tendon goes down while preserving the form of its
domes. This result is in accordance with the
bibliography and the observations made by Boriek
and Rodarte (1997).
Figure 7: Motion of the diaphragm.
We also present the results of our model
concerning lungs motion. Figure 8 represents the
displacement vectors at different locations on the
lungs. The two red vectors represent the mean
orientation of the displacement vectors at a high
level of the lungs (upper view) and at a low level of
the lung near the diaphragm (lower view). On the
upper level, the displacement is lateral, oriented
upwards while the displacement on the lower level
tends to be more vertical and is oriented downwards.
These results are in accordance with the anatomy.
Indeed, the higher parts of the lungs are influenced
by the ribs motion (lateral motion with elevation)
and the lower parts are more influenced by the
motion of the diaphragm central part (downwards).
A PRELIMINARY STUDY FOR A BIOMECHANICAL MODEL OF THE RESPIRATORY SYSTEM
513

Figure 8: Lungs motion.
6 CONCLUSIONS
We have developed a complete model of the
respiratory system built from “virtual patient” data.
A simple model of the diaphragm, which was
missing in our previous studies, has been introduced.
We showed preliminary results, which are in
accordance with the anatomical reality. The central
part of the diaphragm tends to move downwards,
while the muscular part motion tends to be lateral
oriented downwards due to rib motions. In future
works, the model should be applied on a real
patient’s data to enable quantitative comparisons of
the results. The applied nodal forces should be
replaced by more appropriated formulations. In
particular, the forces could be parallel to muscular
fibres in agreement with anatomy and derived from
biomechanical considerations. Last, the forces
should be correlated to thoracic motion and air flow
to the lungs.
ACKNOWLEDGMENTS
We thank the French League against Cancer and
PRRH ETOILE for their financial support.
REFERENCES
A. Al-Mayah, J. Moseley, and KK. Brock. Contact surface
and material nonlinearity modeling of human lungs.
Physics in medicine and biology, 53 : 305-317, 2008.
N. Aspert, D. Santa-Cruz, and T. Ebrahimi. Mesh :
measuring errors between surfaces using the hausdorff
distance. IEEE conference in multimedia and expo
(ICME), pages 705-708, 2002.
A. M. Boriek and J.R. Rodarte. Effects of transverse
stiffness and central tendon on displacement and shape
of a simple diaphragm model. Journal of applied
physiology, 82(5) : 1626-1636, 1997.
KK. Brock, MB. Sharpe, LA. Dawson, SM. Kim, and DA.
Jaffray. Accuracy of a finite element model-based
multi-organ deformable image registration. Medical
Physics, 32(6) : 1647-1659, 2005.
A. L. Didier, P.F. Villard, J.Y. Bayle, M. Beuve, and B.
Shariat. Breathing thorax simulation based on pleura
behaviour and rib kinematics. Information
Visualisation, IEEE Computer Society, pages 35-40,
2007.
A. L. Didier, P.F. Villard, J. Saadé, J.M. Moreau, M.
Beuve, and B. Shariat. A chest wall model based on
rib kinematics. Information Visualisation, IEEE
Computer Society, pages 159-164, 2009.
B. Gagel, C. Demirel, A. Kientopf, M. Pinkawa, M.
Piroth, S. Stanzel, C. Breuer, B. Asadpour, T. Jansen,
R. Holy, J.E. Wildberger, and M.J. Eble. Active
breathing control (abc): determination and reduction of
breathing-induced organ motion in the chest. Int. J.
Radiation Oncology Biol. Phys., 67(3) : 742-749,
2007.
P. Giraud, E. Yorke, S. Jiang, L. Simon, K. Rosenzweig,
and G. Mageras. Reduction of organ motion effects in
IMRT and conformal 3d radiation delivery by using
gating and tracking techniques. Cancer radiothérapie,
10 : 269-282, 2006.
F. M. Hendriks. Mechanical behaviour of human skin in
vivo - a literature review. In Nat.Lab. Unclassified
Report 820. Philips Research Laboratories, 2001.
S. B. Jiang. Radiotherapy of mobile tumors. Seminars in
Radiology Oncology, 16 : 239-248, 2006.
S. Mori, M. Endo, S. Komatsu, T. Yashiro, S. Kandatsu,
and M. Baba. Four-dimensional measurement of lung
tumor displacement using 256-multi-slice ctscanner.
Lung Cancer, 56 : 59-67, 2007.
C. Ozhasoglu and M.J. Murphy. Issues in respiratory
motion compensation during external-beam
radiotherapy. Int. J. Radiation Oncology Biol. Phys.,
52(5) : 1389-1399, 2002.
E. Promayon and P. Baconnier. A 3D discrete model of
the diaphragm and human trunk. ESAIM Proceedings,
23 : 66-77, 2008.
Y. Seppenwoolde, H. Shirato, K. Kitamura, S. Shimizu,
M. Van Herk, J.V. Lebesque, and K. Miyasaka.
VISAPP 2010 - International Conference on Computer Vision Theory and Applications
514

Precise and real-time measurement of 3d tumor
motion in lung due to breathing and heartbeat,
measured during radiotherapy. Int. J. Radiation
Oncology Biol. Phys., 53(4) : 822-834, 2002.
H. Shirato, K. Suzuki, GC. Sharp, K. Fujita, R. Onimaru,
M. Fujino, N. Kato, Y. Osaka, R. Kinoshita, H.
Taguchi, S. Onodera, K. Miyazaka. Speed and
amplitude of lung tumor motion precisely detected in
four-dimensional setup and in real-time tumor-
tracking radiotherapy. Int. J. Radiation Oncology Biol.
Phys., 64(4) : 1229-1236, 2006.
P. F. Villard, M. Beuve, and B. Shariat, V. Baudet, and F.
Jaillet. Simulation of lung behavior with finite
elements : influence of bio-mechanical parameters.
Information Visualisation, IEEE Computer Society,
pages 65-70, 2005.
P. F. Villard, M. Beuve, and B. Shariat : An Approach to
Convert 4D Geometry into a 4D CT Scan. WSCG
(Winter School of Computer Graphics), UNION
Agency ed. Plzen (Czech Republic). pp. 163-170.
ISBN 80-86943-05. 2006.
J. W. Wong, M.B. Sharpe, D.A. Ja_ray, V.R. Kini, J.M.
Robertson, J.S. Stromberg, and A.A. Martinez. The
use of active breathing control (ABC) to reduce
margin for breathing motion. Int. J. Radiation
Oncology Biol. Phys., 44(4) : 911-919, 1999.
A PRELIMINARY STUDY FOR A BIOMECHANICAL MODEL OF THE RESPIRATORY SYSTEM
515
