
I-CARE
A Health Promotion System for Active Ageing
Maria Lúcia Kroeff Barbosa
1
, Valter Roesler
2
, Alexandro Bordignon
2
,
Johannes Doll
1
and Eliseo Berni Reategui
1
1
PPGEDU, UFRGS, Av. Paulo Gama, 110, Porto Alegre - RS, Brazil
2
PPGC, UFRGS, Av. Bento Gonçalves, 9500, Porto Alegre - RS, Brazil
Keywords: Telemedicine, Telehealth, Health Promotion, Active Ageing, Education.
Abstract: I-Care is a health promotion system designed to: a) monitor vital signs of patients in real time; b) improve
the patients’ knowledge of the disease, aiming to increase their motivation to develop healthy habits; c)
motivate the patients through their interaction with doctors, friends and other patients with the same disease.
The system works through the web, being suitable for many platforms. A group of three people was
monitored during four weeks, generating some interesting conclusions about different ways to motivate
people to get older in a more active and healthy way. The test subjects were from 56 to 67 years, both male
and female, with hypertension, overweight and diabetes. The adopted methodology was both quantitative
and qualitative. Results showed that the proposed system can improve significantly the health of the
monitored patients, developing in the participants a better understanding about their health situation.
1 INTRODUCTION
This paper presents i-Care, a web-based system
which aims to provide autonomy to active elder
people through three basic approaches: Monitoring
of their health through the use of vital sign sensors
and communication with a Health Center;
Awareness of their health state and physical and
nourishment re-education; More social interaction
with doctors, friends, family and people with the
same disease, in order to exchange information.
One difference between i-Care and other health
monitoring systems is that i-Care aims to re-educate
the patients besides monitoring them.
The ageing of the world population brings more
and more attention to new health care tools and
technologies enabling an approximation between
elder people and the environment around them,
aiming to keep them in the center of the process.
This extra attention creates involvement and
motivation in the pursuit of health promotion and
disease prevention, enabling a re-education for
healthy lifestyles and better life quality.
The World Health Organization states that a big
share of the supervision or care that people actually
need may be provided by themselves (WHO, 1986).
Nakatani (2009) also emphasizes that most elders
are able to take care of themselves in their homes.
This is a much more comfortable solution, which
may also be more economic and a good alternative
for their health care. To make the treatment of
chronic conditions more effective and efficient, it is
important to envolve the patients and to educate
them to participate in the decision making process.
Motivating the elderly in the development of an
active attitude and making them more aware about
their health can lead to a path in which knowledge
contributes to the improvement of their lives. It is
important to reinforce that, to keep a good quality of
life, it is necessary to control chronic-degenerative
diseases such as hypertension, diabetes, arthritis,
osteoporosis, dementia, among others (Pavarini,
2005). One way to minimize age effects is to have a
healthy nutrition and regular exercise habits.
All of the above aspects were taken into
consideration when developing the i-Care interface
and an investigation was carried out with 11 elders
in order to validate it (Jantsch, 2011).
This paper is organized as follows: section 2
presents other works related to this research. Section
3 presents the system details, while section 4
presents the experiment methodology. Section 5
presents the results, and section 6 the conclusions.
331
Lúcia Kroeff Barbosa M., Roesler V., Bordignon A., Doll J. and Berni Reategui E..
I-CARE - A Health Promotion System for Active Ageing.
DOI: 10.5220/0003917703310336
In Proceedings of the 4th International Conference on Computer Supported Education (CSEDU-2012), pages 331-336
ISBN: 978-989-8565-07-5
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

2 RELATED WORKS
The IAMSPE (Institute of Medical Assistance for
the Public Server, 2011) created a monitoring
system for diabetics. Nowadays they are monitoring
about 300 patients, and they have resources to reach
800 people. They provide insulin, test strips and a
glucometer with memory to perform 3 exams each
day at home. Each 7 or 15 days, the patients upload
their data to a health center, and the doctors analyze
the data to decide if the patient needs orientation. In
that case, there is a team of instructors giving the
patients the necessary orientation.
I-Care has many differences in relation to
IAMSPE’s system. First of all, in i-Care the exams
are sent in real time, using an internet or a 3G
connection, through computers or mobile devices.
Another difference is that i-Care has many sensors,
and not only the glucometer. Another one is that the
system provides a lot of educational material in
order to improve the patients’ understanding about
their health issues.
Another related work is Angius’s research which
has the goal of developing of a low-cost system for
telemedicine based on the DVB-T (Digital Video
Broadcasting – Terrestrial) technology (Angius et al,
2008). The diffusion of DVB-T standard and the low
cost of DVB-T set-top boxes bring the vision of a
broad distribution of tele homecare monitoring
systems with an easy-to-use patient’s interface. The
proposed system, based on a currently widespread
infrastructure, enables patients to monitor their
health from home, without the need of any
installation procedure. Even untrained people (or the
elderly) can easily use such system due to their
familiarity with basic DVB-T home-entertainment
equipment.
The problem with a digital TV health care is that
a broadcaster must send the application through its
Transport Stream (TS). However, a health
application rarely is a priority for a broadcaster.
Besides, the user must have a conventional return
channel for sending the results. In practice, what
happens is that the patient, having the application in
a pendrive, runs it through a set-top box USB port.
The application presented in this paper was
initially implemented in NCL (Nested Context
Language) and Lua, which are digital TV
middleware standards (ITU, 2001). However,
evolved to the use of other languages and platforms
because of the need to create videoconferencing and
social network facilities, among others. Such
functionalities are very difficult to implement using
digital TV middleware languages.
The platform selected for this version of i-Care is
web based, as we observe a convergence towards
web. Today handhelds, tablets, connected televisions
and computers are all “talking” web.
3 SYSTEM DETAILS
The general idea of the system proposed here is
depicted in Figure 1. The patients stay at home, and
update their vital signs in a rate defined in their
profile (e.g. daily, weekly). According to their
chronic diseases, they receive a number of sensors to
monitor their data. The most common are
Glucometer (for diabetes), Blood pressure (for
hypertension) and Scale (for weight control). All of
them receive a Pedometer, which is a step meter,
used to monitor the amount of physical exercises
that they have been doing.
The system interface is projected to work also on
a television (as a monitor) connected to a computer,
because it is the most friendly equipment for the
target public. Some of the interface screens are
presented in Figure 1, and will be detailed hereafter.
The system has also an interface for mobile devices,
as it will be discussed later.
The system runs through a web browser,
eliminating the need of installing any software in the
patients’ home. The patient vital signs are sent to a
web server, and the data is immediately available to
anyone with access rights and the server’s URL.
Figure 1: System overview.
The system is composed of two main entities:
“User Portal” and “Health Care Center”, described
CSEDU2012-4thInternationalConferenceonComputerSupportedEducation
332

in the next sections. Besides, the system has the
patients’ configuration module, enabling the setting
up of their profile, the recording of the medicines
which they are taking, the registration of contact
persons, telephones, Body Mass Index (BMI), body
fat percentage, Waist to Hip Ratio (WHR), among
other information.
3.1 User Portal
The user portal is the interface where the patients
interact. The first screen is presented in Figure 2,
showing their possible choices, which are:
Figure 2: User portal.
a. Exams: allows the insertion of vital signs data;
b. Performance Graphics: allows the
visualization of the vital signs throughout time;
c. Communication: interactive functions related
to social networks and videoconferencing;
d. Bits of Health: educational videos about
diseases and benefits of physical exercises and
healthy eating.
The system compares the vital signs filled by the
patient with his/hers profile to see if there is any that
is out of the normal range. If so, it presents an alert
to the user, and suggests him/her to watch some
educational videos specifically about the problem.
For example, Figure 3 shows two parameters out of
range: Glucose and number of steps. The system will
suggest some videos with information on diabetes,
healthy food for patients with diabetes, and the
importance of physical activity.
Figure 3: Vital signs out of range.
At the same time, these data are sent to the
Health Care Center and, as there are vital signs out
of range, there will be an alarm also in the central.
This can be used for decision making, as for
example to call the patient and offer help. In extreme
cases, it is possible to use these data to send
immediately an ambulance to the patients’ home.
Related to the “Communication” option, the
interface allows the patient to access a social
network and interact with other people with similar
diseases, aiming to minimize the elderly isolation
and to be a forum for the exchange of ideas.
3.2 Health Care Center
The Health Care Center Module is responsible for
the monitoring of patients. If there is an alarm on a
patient, his/her data appear in the beginning of the
list, and a sound is generated, followed by a yellow
message.
The Health Care Center has also all the
information about the patients, as their performance
bar charts, telephone, name and telephone of close
people, name of doctors, medicines that the person is
taking, visit records, measurements, among other.
4 METODOLOGY OF TESTING
An experiment with i-Care has been carried out for
the period of 4 weeks, involving a group of 3 people:
• Patient 1: 56 years old, male, overweight and
acquired diabetes type 2.
• Patient 2: 67 years old, male, overweight and
Parkinson.
• Patient 3: 60 years old, female, overweight and
hypertension.
The test subjects were registered in the system,
and they were asked to fill out a web form informing
their vital signs on a daily basis. They were advised
to take these measurements at the same time every
day to avoid pressure or glucose levels variation.
Three profiles were created:
• Hypertension: for subjects with high pressure
levels. The system asks for daily exams of
Pressure (systolic and diastolic) and Resting
heart rate. Besides that, the system asks for the
Number of steps performed during the day.
Weekly, the system asks for the weight of the
subject.
• Diabetes: for subjects with diabetes mellitus.
The vital signs are exactly the same as
Hypertension profile, with an additional exam,
which is the measurement of glucose levels.
I-CARE-AHealthPromotionSystemforActiveAgeing
333

• Obesity: it is exactly the same as Hypertension
profile, with the difference that the weight is
asked daily, and not weekly.
During the first visit to the patient, a care taker
explained the system and also took some
measurements. This allowed the professional to get
some indexes of the patients, like Body Mass Index
(BMI), body fat percentage, Waist to Hip Ratio
(WHR), and so on.
During the first visit, we also made an interview
about their eating habits and physical activities
during the last 4 weeks, in order to better understand
how much the system could influence them.
During the experiment, we contacted the subjects
through some phone calls when needed due to the
exam results.
The patients were informed that, if they did not
fill the forms one day or if one of their vital signs
were out of the accepted range, an alarm would be
sent to the health center. They were also informed
that all their vital signs would be monitored daily by
a professional.
From an educational perspective, besides
participating in the process of making the users more
aware about their conditions, the system has about
160 videos related to each one of their profiles. The
users can watch the videos freely navigating through
the interface, or they can be directed to a specific
ones in the case one of their vital signs is out of the
accepted range. In that case, an alarm is also
generated to the health center dashboard.
After 4 weeks, the initial measurements were
repeated, and a final interview was made.
5 RESULTS
The experiment was performed during the month of
October, 2011. During the initial interview, we
discovered that two patients were trying to lose
weight and were fairly active, walking around 6 km
twice a week during the previous month. One of
them was not so active, and did not perform
activities at all.
The monitored tests proceeded for four weeks
beginning the day after the interview. It was clear
that only the fact of being participating in a health
program motivated the subjects. They now had to
walk at least 5,000 steps daily and they had to fill
the web form, otherwise the system would show an
alarm to the user and to the health center.
Figure 4 presents the 4 week result for one of the
patients. It is clear the motivation increase due to the
program. He began to walk about 10,000 steps every
day, without having anyone asking him to do so.
Figure 4: Patient 1 – number of steps when monitored.
Patient 2 presented similar results. Patient 3
increased slightly the number of steps at the
beginning but, when she discovered that she was
losing weight, the daily number of steps increased
impressively.
Figure 5 presents the number of steps for all test
subjects during the monitoring period. It is clear that
all of them tried to fulfil their duties with the system,
and were compromised with the program success.
Figure 5: Number of steps during the monitoring phase.
Figure 6 depicts the glucose and pressure
variation of patient 1. The glucose levels were high
at the beginning of the experiments, and decreased
to normal levels, while the pressure, which was
normal, continued normal.
Figure 6: Glucose levels of patient 1.
CSEDU2012-4thInternationalConferenceonComputerSupportedEducation
334
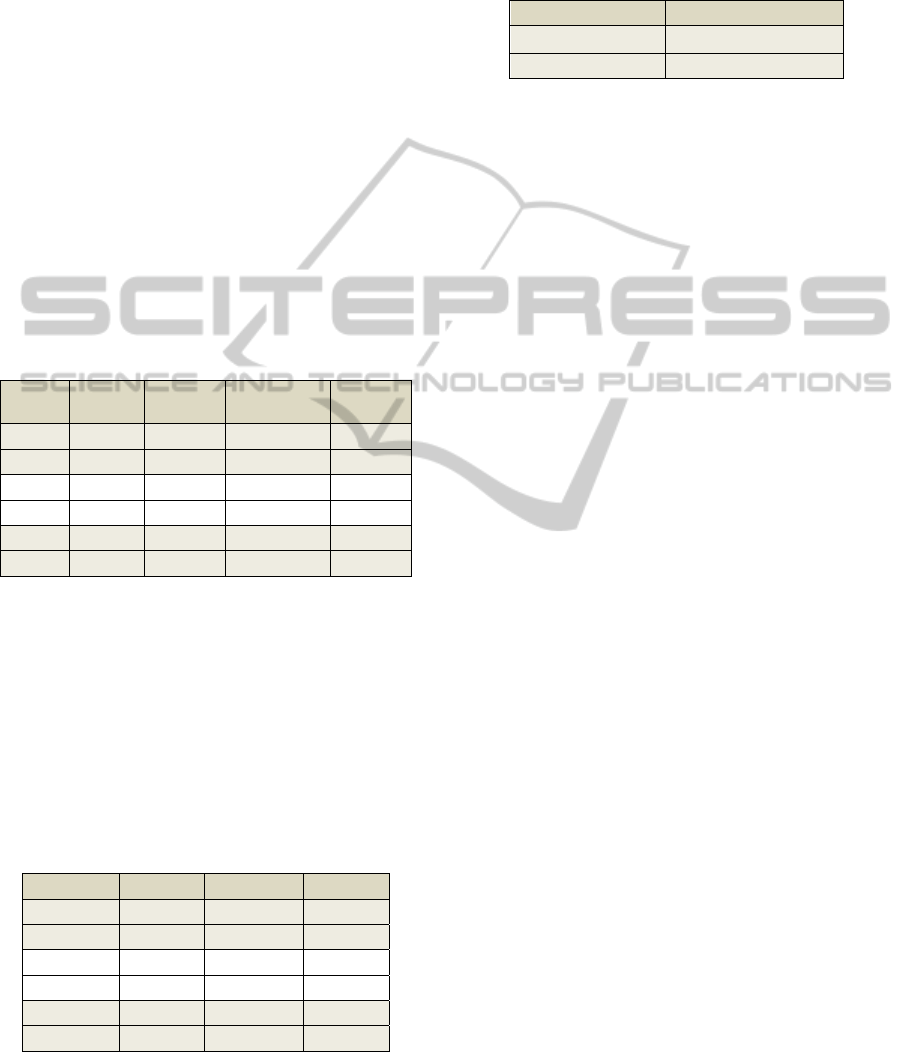
With the end of the experiment, the set of
measurements was repeated, and the results for the
patients’ weight are presented in Table 1.
All patients reduced the total weight (first
column), and additionally some of them increased
the lean weight (third column), reducing even more
their percentage of body fat (fourth column).
Patient 1 reduced 2.3 kg, 1.44 kg of fat and 0.86
kg of lean body mass.
Patient 2 reduced 1.5 kg, losing 4.29 kg of fat
and increasing 2.79 kg of lean body mass.
Patient 3 reduced 2 kg, losing 3.98 kg of fat and
increasing 1.98 kg of lean body mass.
The fat weight and lean weight are valuable
information because they showed that the system
was producing significant results for the patients.
Many times a person wants to lose weight and enters
a diet; however, often diets result in loss of lean
body tissue and water, which is not beneficial for the
person’s health.
Table 1: Weight results.
Total
weight
Fat weight Lean body
weight
Body Fat
(%)
P1_ini 85.00 16.14 68.86 18,99
P1_final 82.70 14.70 68.00 17.72
P2_ini 83.50 20.79 62.71 24.90
P2_final 82.00 16.50 65.50 20.12
P3_ini 73.10 25.56 47.54 34.96
P3_final 71.10 21.58 49.52 30.35
Other monitored results were the main corporal
indexes, shown in Table 2: BMI (Body Mass Index),
WHR (Waist to Hip Ratio) and BAI (Body adiposity
Index).
The results showed a reduction of all indexes for
all patients. However, it is important to note that all
participants still need to keep lowering most of their
indexes in order to reach the international health
standards (WHO, 1995, 2000, 2004, 2008)
(Bergman et al, 2011).
Table 2: Main corporal indexes.
Exam BMI WHR BAI
P1_ini 30.11 1.04 27.46
P1_final 29.30 1.01 26.54
P2_ini 29.94 1.00 29.72
P2_final 29.40 0.96 29.63
P3_ini 27.17 0.74 34.37
P3_final 26.43 0.74 33.51
In relation to glucose levels, the only patient
with diabetes was patient 1, and his results, shown in
Table 3, presented an average reduction of more
than 20%, which made him very happy indeed. One
comment was “I have never seen my glucose levels
so low as they are now”.
Table 3: Average glucose levels.
Exam Average glucose levels
P1_first two weeks 120.64
P1_final two weeks 100.64
Related to the patients’ awareness about their
own health, the results were just as exciting as the
quantitative ones. The patients had a form to fill out
with their impressions about the system, and the
interviews also clarified their feelings and learning.
Some selected statements from this form and from
the interviews are presented below:
“My goal is to reach the ideal weight. I will have
to reduce food and increase physical activity to see
if I succeed, but it is not easy, because it seems the
scale is stuck in 71.1 kg. Oh, God!!!”
“Today I watched some videos and I was very
pleased. They have a short duration, I can pause
them if I want, if I do not like one I can cancel and
choose another. Very good. I loved it.”
“The use of the Pedometer is very important. If I
do not reach the number of steps at the end of the
day, I walk around my building as many times as
needed to complete the minimum.”
“I was having some difficulties with my arms
flexibility, and then I saw a video explaining a series
of exercises to improve that. I tried and it worked,
and I am repeating them regularly since then.”
There are a lot of other interesting statements, but
these ones synthesize most of them. The fact is that
the patients are improving their life style, their
health, their autonomy and their knowledge about
their own condition.
6 CONCLUSIONS
This paper presented a new system for health
promotion, called i-Care. The system works on any
browser, so, it is suitable to many platforms, like
computers, tablets, mobile devices and also
television.
The main differences between i-Care and other
related health promotion systems are:
• The educational characteristic of i-Care, where
the patient has the option to effectively learn
about his disease, exercises and nutrition using
the videos;
• The indication of exercises (daily number of
steps) to set goals to the patients;
I-CARE-AHealthPromotionSystemforActiveAgeing
335

• The social component, which was slightly
explored in this paper.
The system is composed of three main modules:
patient configuration; health center dashboard; and
user portal. Each of these was explained in section
3.The interface usability was validated for
television, computers, tablets and mobile devices, as
also detailed in section 3.
We performed a four week experiment with
three real users to validate the system in relation to
its ability to increase the patients’ autonomy and
awareness about their health condition. The users
belonged to three different groups: diabetes,
hypertension and obesity, and they had to fill out
information about their vital signs every day using a
web browser. They also had to walk a number of
steps daily. They knew that they were being
monitored by a health center on a daily basis.
From the first moment it was clear that the
motivation of being constantly monitored was much
bigger than in a situation where the person only has
to count on him/herself to reduce weight without any
follow up. The system changed the routine of these
people, and they worked out much more when
compared to the time without monitoring, mainly
because they now had goals to reach, and someone
to help with their doubts and questions.
The results showed that a monitoring and
educational system can improve the health of the
monitored people, creating an “obligation” of
exercising and following some healthy rules.
Besides that, the results showed a real improvement
in the knowledge of the patients about their health
situation and what to do in order to grow old in a
healthy way.
The system is beginning to be applied to 8 new
users only with the diabetes profile, being monitored
with an enterprise specialized in homecare, in order
to confirm (or not) the data presented in this paper.
ACKNOWLEDGEMENTS
We would like to thank “Hospitalar Home Care”, for
their valuable suggestions on the system operation,
“I9access Technology ltda” for developing the
system based on our suggestions and FINEP
(Financial Supporter of Studies and Projects), which
helped to buy some sensors.
REFERENCES
Angius, G. Pani, D., Raffo, L., Randaccio, P., Seruis, S.
2008. A Tele-home Care System Exploiting the DVB-
T Technology and MHP. Methods Inf Med 3/2008. p.
223 – 228. At: http://www.orcatech.org/papers/home_
monitoring/08_Angius_telehome_care.pdf . Access:
October, 2011.
Bergman, R. N., Stefanovski, D., Buchanan, T., Sumner,
A. E., Reynolds, J. C., Sebring, N. G., Xiang, A. H.,
Watanabe, R. M. A better Index of Body Adiposity. In
Obesity 19, 1083 – 1089, May 2011. At: http://www.
nature.com/oby/journal/v19/n5/full/oby201138a.html.
Access: November, 2011.
ETSI Standard: EN 300 744 V1.5.1. 2004. Digital Video
Broadcasting (DVB). Framing structure, channel
coding and modulation for digital terrestrial television.
Iamspe. 2011. Iamspe selects diabetics for remote
monitoring. At: http://www.iamspe.sp.gov.br/index.
php?option=com_content&view=article&id=350:tele
medicina-diabeticos&catid=119:campanhas-e-eventos
-imprensa&Itemid=196. Access: October, 2011.
ITU-T J.200 (03/2001). 2001. Worldwide Common Core –
Application Environment for Digital Interactive
Television Services.
Jantsch, A., Barbosa, M. L. K., Reategui, E. B., Roesler,
V. 2011. Proposal of a simplified interface for TV-
Care: homecare through digital TV. In CITA 2011: VI
Ibero-american Congress of Telematics. Gramado,
Brazil.
Nakatani, A. Y. K., Silva, L. B., Bachion, M. M., Nunes,
D. P. 2011. Functional capacity in elderly in the
community and interventions proposed in the team
health. In Rev. Eletr. Enf. 2009; 11(1):144-50. At:
http://www.fen.ufg.br/revista/v11/n1/v11n1a18.htm.
Access: Febuary, 2011.
Pavarini, C. S. I. 2005. The art of taking care of the elder:
gerontology as profession? In Text & Context, v. 14,
n. 3, p. 398-402.
WHO. World Health Organization. 1995, 2000, 2004.
BMI Classification. At: http://apps.who.int/bmi/index.
jsp?introPage=intro_3.html. Access: November, 2011.
WHO. World Health Organization. 1986. The Ottawa
Charter for Health Promotion. In First International
Conference on Health Promotion, Ottawa, 21
November 1986. At: http://www.who.int/healthprom
otion/conferences/previous/ottawa/en/. Access: Octo-
ber, 2011.
WHO. World Health Organization. 2011. Waist
Circumference and Waist–Hip Ratio. At: http://whq
libdoc.who.int/publications/2011/9789241501491_eng
.pdf. Access: November, 2011.
CSEDU2012-4thInternationalConferenceonComputerSupportedEducation
336
