
Development of an Integrated Virtual Group Training
System for COPD Patients
Jonathan B. J. Dikken
1
, Bert-Jan F. van Beijnum
1
, Dennis H. W. Hofs
1
, Mike P. L. Botman
1
,
Miriam M. Vollenbroek-Hutten
1,2
and Hermie J. Hermens
1,2
1
Institute for Biomedical Technology and Technical Medicine (MIRA), University of Twente,
P.O. Box 217, 7500AE Enschede, The Netherlands
2
Roessingh Research and Development, Roessinghsbleekweg 33b, 7522AH Enschede, The Netherlands
Keywords: Physical Condition, Virtual Group Training, Chronic Obstructive Pulmonary Disease, Home-based Exercise
Training, Integrated Training System, Design, Evaluation, Exergaming.
Abstract: COPD patients experience a downward spiral of fear for breathlessness, inactivity and social isolation which
leads to a bad physical condition. Motivation to keep patients compliant to their training scheme is a key
factor in home-based exercise training. This paper presents the Integrated Training System for COPD
patients; a home based virtual group exercise system to facilitate improvement of the exercise capacity
safely at home using a virtual group environment. The four components of the system are the Home Trainer,
the Virtual Exercise Environment, the Web Portal and the Controller. These components are implemented
in a prototype. An in-training evaluation was performed to evaluate the subsystems used during a training
exercise. All subsystems are working correctly during the evaluation. In this paper the focus for the
Integrated Training System is on COPD patients, but the system might be used for other groups such as
Chronic Heart Failure patients or elderly people in general.
1 INTRODUCTION
Chronic Obstructive Pulmonary Disease, a common
disease characterized by persistent airflow
limitation, is one of the leading diseases in many
countries which will grow to the 4
th
largest cause of
death in 2030 (Global Initiative for Chronic
Obstructive Lung Disease, 2013; Mathers & Loncar,
2006). In 2007 in the Netherlands 323.600 people,
about 2% of the population, were diagnosed with
COPD. These figures are comparable to the
surrounding countries (Rijksinstituut voor
Volksgezondheid en Milieu, 2010).
The downward spiral of breathlessness fear,
inactivity and social isolation leads to a bad physical
condition (Global Initiative for Chronic Obstructive
Lung Disease, 2013). To overcome this downward
spiral patients can be enrolled in a pulmonary
rehabilitation program (PRP) which improve the
exercise capacity (Croitoru et al., 2013; Nici et al.,
2006; Shahin, Germain, Pastene, Viallet, & Annat,
2008). However, most benefits deteriorate after the
rehabilitation program is finished (Egan et al., 2012;
Gosselink, 2002; Karapolat et al., 2007; Nici et al.,
2006; Spruit, Troosters, Trappenburg, Decramer, &
Gosselink, 2004).
Maintenance strategies can retain the effects of a
pulmonary rehabilitation program. Du Moulin et al.
shows that home-based exercise training is effective
as maintenance of the exercise capacity (Du Moulin,
Taube, Wegscheider, Behnke, & Van Den Bussche,
2009). Also Beauchamp et al. showed a significant
improvement of the exercise capacity with a
community based maintenance exercise program
(Beauchamp, Francella, Romano, Goldstein, &
Brooks, 2013). Motivation to keep patients
compliant to their training scheme is a key factor in
home-based exercise training.
This paper presents a home-based virtual group
exercise system to facilitate improvement and
maintenance of the physical condition of COPD
patients. In this paper we focus on the technical
design of the system and the medical case it should
cover. The system should cover all important aspects
of home-based exercise training: means to do the
training, motivational support and professional
guidance. Therefore we call it the integrated training
101
B. J. Dikken J., F. van Beijnum B., H. W. Hofs D., P. L. Botman M., M. Vollenbroek-Hutten M. and J. Hermens H..
Development of an Integrated Virtual Group Training System for COPD Patients.
DOI: 10.5220/0004801601010108
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2014), pages 101-108
ISBN: 978-989-758-010-9
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

system (ITS). The goal of the system is to facilitate
improvement and maintenance of the physical
condition of COPD patients safely at home using a
(virtual) group environment. This will reduce
disabilities in activities of daily living (Garcia-
Aymerich et al., 2003; Tak, Kuiper, Chorus, &
Hopman-Rock, 2013).
In Backgrounds relevant training aspects,
motivation aspects, adherence aspects and existing
exergames will be given. After the Design
Considerations are explained, the Architecture of the
ITS will be drawn. The Implementation will be
tested in the Evaluation. With Discussion and
Conclusion this paper will be finalized.
2 BACKGROUNDS
2.1 Training
Different opinions exist about the use of either
power training or endurance training as the most
suitable method to improve the physical capacity
(Puhan, Schünemann, Scharplatz, & Bachmann,
2005). Studies have conflicting outcomes on which
training intensity and method gain the best results,
however all studies suggest an improvement of the
physical capacity by physical training (Global
Initiative for Chronic Obstructive Lung Disease,
2013; Gosselink, 2002; Korczak, Huber,
Steinhauser, & Dietl, 2010; Puente-Maestu et al.,
2000; Rijksinstituut voor Volksgezondheid en
Milieu, 2010). The type of exercise should
correspond as much as possible with the activities of
daily living. Cycling, walking and walking stairs are
the most suitable exercise forms.
To be effective, a training session should be
intense enough. The optimal heart rate is between 60
and 80 percent of the maximal heart rate (Global
Initiative for Chronic Obstructive Lung Disease,
2013; Janssen, 2001). With 60-80% of the maximal
heart rate a patient will train in the aerobic zone.
Staying in the aerobic zone for the whole training is
not mandatory, but the total amount of time in the
aerobic zone determines the efficiency of the
training.
2.2 Adherence and Motivation
The above results regarding physical training for
COPD patients have been used by the KNGF, the
Dutch physical therapist association, to develop the
therapeutic guideline for COPD patients (Gosselink
et al., 2008).
The lack of therapy adherence of COPD patients is a
known problem with physical exercises (Nici et al.,
2006). Therapy adherence can be increased by
enjoyment and social interaction (Ryan, Frederick,
Lepes, Rubio, & Sheldon, 1997). Burke et al
conducted a meta-analysis of 44 studies to qualify
the effect of the setting of the training (Burke,
Carron, Eys, Ntoumanis, & Estabrooks, 2006). Four
categories where defined: home-based training
without involvement of third parties, home based
training with consultation (e.g. by phone), center-
based training and center based training with
additional attention for group dynamics. A superior
result was found in groups with a high social
cohesion among the participants in comparison to
normal center-based training and home-based
training with consultation. The latter two had a
superior result in regard to individual training
without involvement of third parties. One can
conclude that both good group dynamics as
professional consultation result in a better therapy
outcome.
Social motivation theories can help in increasing
therapy adherence. One social motivation theory is
social support, which is associated with how
networking helps people cope with stressful events
and enhance psychological well-being and can be
categorized in appraisal, companionship, emotional,
instrumental and informational support (House,
1981; Sonderen, 1991). Another theory is the social
comparison theory which includes competition,
cooperation and normative comparison between
members of a groups (Janssen, 2001). These theories
will be used in the implementation of the Integrated
Training System.
2.3 Existing Exergaming
Several professional and consumer exergames are
used for improving the physical condition of
patients. Professional products include the Cybex
Trazer, LightSpace, and Sportwall. Consumer
products include the Sony PlayStation (with Dance
Dance Revolution), Nintendo Wii and Xavix (with
J-Mat). The energy expenditure with these 6 systems
are comparable with the energy expenditure of
walking (Bailey & McInnis, 2011). The Cybex
Trazer, LightSpace, Sony PlayStation with DDR and
Xavix are based on moving to specific positions.
These four systems require non-continuous dynamic
movements. Such movements are unsuitable for
COPD patients because injuries can occur.
Measuring and controlling the intensity of the non-
continuous dynamic movements is difficult. The
HEALTHINF2014-InternationalConferenceonHealthInformatics
102
Sony PlayStation with DDR supports multiplayer
sessions at distinct locations. The other systems
don’t support virtual groups where users play at
distinct locations and can see each other. Social
interaction is limited when players are at distinct
locations.
With Sportwall a player should hit specific
positions on a wall with the hand or a ball. This
system requires non-continuous dynamic
movements as well. Because it is a professional
product it is unsuitable to put at patients’ homes.
This system lacks the possibility to train in virtual
groups and thus the possibility for social interaction.
Wii Sports include five simulation games which
can be controlled by arm movements: baseball,
boxing, bowling, golf and tennis. A precise motor
system is important to use the described systems.
Also this system has the disadvantages of non-
continuous dynamic movements.
A system more tailored to the need of elderly
people is the Espresso Bike in combination with the
NetAthlon riding software. This system was used in
a randomized clinical trial in older adult cognition
(Anderson-Hanley et al., 2012). It has a simple user
interface and doesn’t require very fast responses
from the users. The training intensity is accurately
controllable by changing the resistance of the bike.
The intensity can be measured accurately. The
system focus on cognition aspects and the
improvement of the physical condition is a side
issue.
For COPD patients a system is needed that is
safe, has a low risk for injuries, can measure and
control the intensity accurately and support social
interaction.
None of these systems are built for – and suitable
for accessible physical exercises at home for elderly
people. None of the systems use a virtual group
environment to support social interaction for the
enhancement of therapy adherence.
3 DESIGN CONSIDERATIONS
Cycling on a home trainer was chosen, because a
home trainer is well known for COPD patient from
rehabilitation programs and can measure and set the
training intensity. Using the home trainer at home
increases the accessibility of the system. The ability
to control the power by changing the resistance
contributes to the safety of the system.
A virtual environment will be used to be able
to have a group setting at home. In the virtual
environment patient can train and interact with
each other.
The oxygen saturation level should be above
90% during training sessions to prevent
desaturations.
Requirements were elicitated from a literature
review, observations of PRPs and interviews with
physiotherapists and movement therapists using a
scenario and the People-Activity-Context-
Technology (PACT) framework (Huis in't Veld et
al., 2010). A detailed description of the design
process is given by Dikken et al. (Dikken, 2012;
Dikken, van Beijnum, & Hermens, 2013).
4 ARCHITECTURE
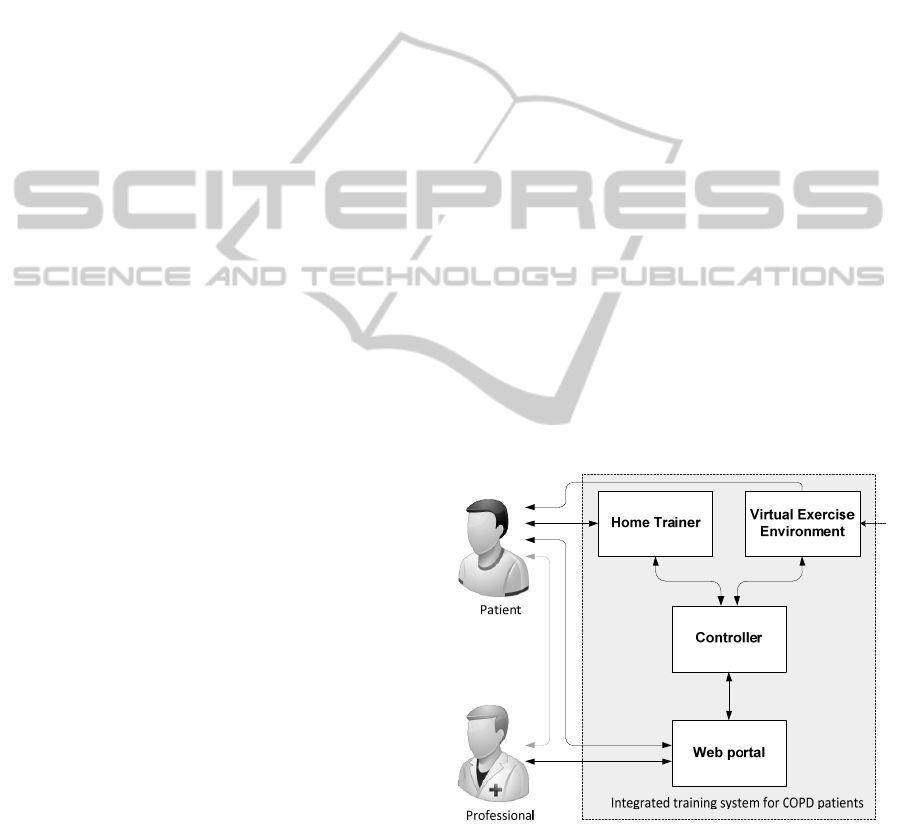
The ITS (Integrated Training System) is divided into
four components: the home trainer (HT), the virtual
exercise environment (VEE), the controller (C) and
the web portal (WP). The home trainer is an ergo
bike with some additional sensors, the virtual
exercise environment is a computer game in which a
patient can cycle together with other patients and the
controller ensure a safe and efficient training by
collecting and analyzing data from the home trainer
and giving feedback. The controller sends the
physiological and exercise data to the web portal. On
the web portal this data is shown. The overview of
the architecture is shown in figure 1.
Figure 1: High level architecture of the Integrated Training
System.
Users of the ITS are COPD patients and their
supervisors, the physiotherapist. Patients use the
whole system, while the physiotherapists only use
the web portal component.
DevelopmentofanIntegratedVirtualGroupTrainingSystemforCOPDPatients
103

4.1 Home Trainer
With the home trainer patient can perform physical
activities. On the home trainer the training intensity
can be controlled and patient data is acquired.
Patients will experience force feedback from the
home trainer.
The home trainer component contains all sensors
and actuators of the system. Quantities that need to
be measured are power, cadence, heart rate and
oxygen saturation level. This component consists of
a home trainer, a heart rate belt and a pulse
oximeter.
4.2 Virtual Exercise Environment
The virtual exercise environment (VEE), showed in
figure 2, provides motivation during a physical
training. The VEE is essentially a computer game in
which multiple players can cycle in the same virtual
environment. The avatar of a patient cycles with a
speed that reflects the performance of the patient in
the virtual environment, but the users are kept close
to each other to up keep the group spirit during the
whole training.
Several motivation theories are implemented,
which is explained in the next section. Each session
is a game in which the patient who cycles with the
best performance will win the game (social
comparison – competition). The performance is
calculated by how close a patient cycles to his
individual goal. Players are motivated when they
cycle together in the virtual environment and can see
each other (social support – companionship). When
a patient fails to cycle with a similar performance of
the other group members, he will slow down a get in
the back. To prevent a player to drop out because he
is too far behind, that player will get a boost to keep
up with the other group members. The boost will
stop when the player gets close to the other group
members to prevent disturbance of the competition.
Figure 2: Virtual Exercise Environment.
During training all interaction with the user is
provided by the VEE, except for the force feedback
by the home trainer. The interaction of the VEE
includes a user interface with an overview of the
important measured values, such as power and heart
rate and an overview with the current performance.
4.3 Web Portal
The web portal (WP) provides after-exercise
motivation: patient can retrieve their progress, set
and monitor personal and group goals and give
feedback on training results of group mates. Also the
portal is used to give the physiotherapist insight in
the training progress and configure the system.
After a training session both the patient and the
professional can see a summary of training on the
web portal. This includes a good indication of the
performance with a mark and important events such
as overperformance, underperformance and possible
desaturation events during the training. A screenshot
is shown in figure 3. Patients can review each
other’s performance (figure 4; social comparison –
competition and cooperation) and give feedback
through messages to motivate each other (social
support – companionship and emotional support).
The professional will use the training summary to
give advices.
A group of patients has the goal to reach each
individual goal (social comparison – cooperation).
The patients can compare themselves to a patient
who is performing well (social comparison –
normative comparison). Informational support
(social support) is given by sharing patient stories
with how they cope with the disease.
A detailed description of the web portal
including design rationale and the design process is
given by M. Botman (Botman, 2013).
4.4 Controller
The controller monitors and guides the safety and
performance during a training session and facilitates
data exchange between all components. For the
safety and performance three control modules are
used: the performance loop, the safety loop and the
positioning system. The controller has several
interface modules to connect to the other
components. A design overview is shown in figure
5.
Important measured data, such as power, heart
rate, oxygen saturation level and performance, is
send to the web portal by the controller.
All modules, both interface modules as control
HEALTHINF2014-InternationalConferenceonHealthInformatics
104
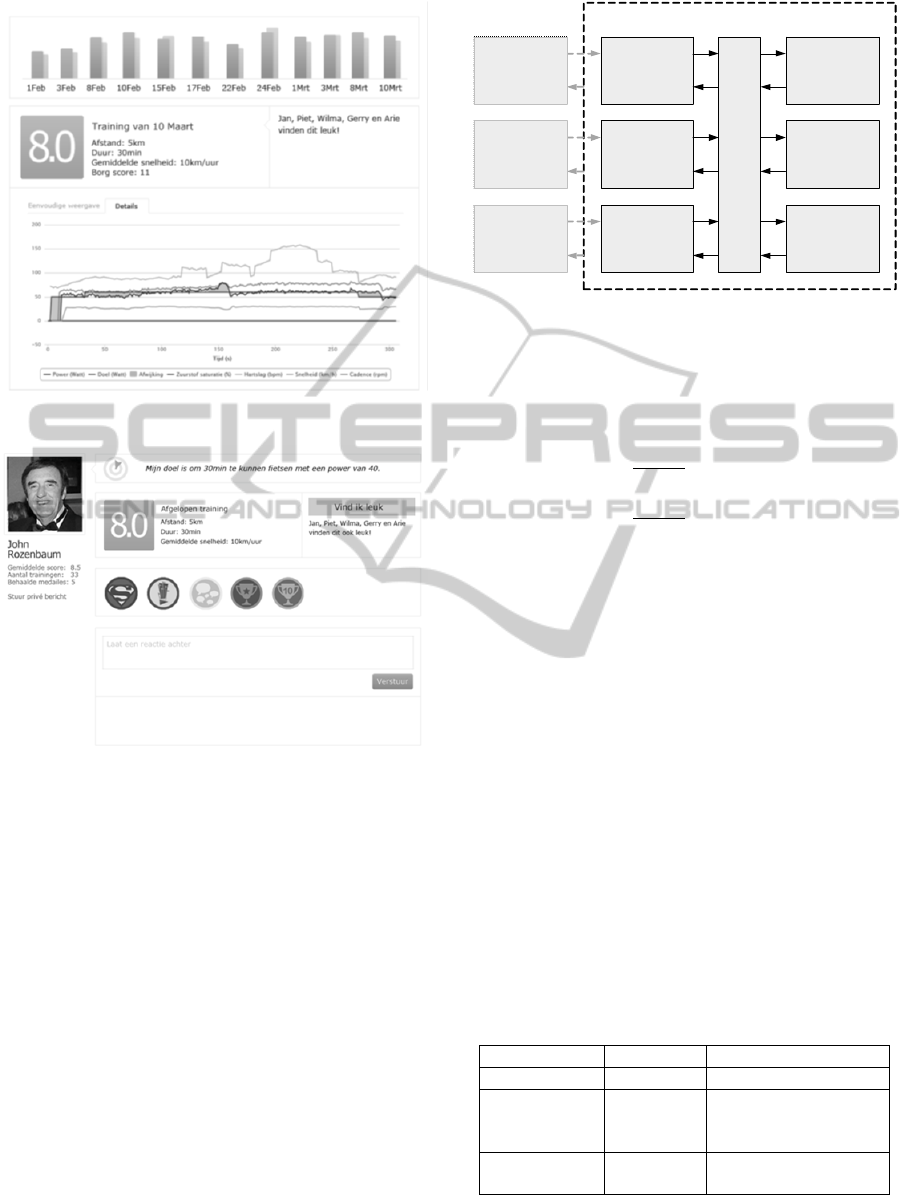
Figure 3: Web Portal - Training result page.
Figure 4: Web Portal - Patient profile page.
modules, use a data bus to exchange real-time data.
With a data bus the controller is highly flexible.
Modules are not aware of each other’s existence and
can be added, removed, updated and replaced easily.
Different execution frequencies are possible,
enabling usage of sensors with different sample.
4.4.1 Performance Loop
To facilitate improvement of the physical condition
a training session needs to be effective. This is
handled by the performance module. The
performance is calculated to be able to give visual
feedback on the performance and to adapt the
resistance of the home trainer.
Based on the current power (P
c
) and the target
power (P
target
), which is set in the web portal, the
performance is calculated as shown in equation (1).
The result is a dimensionless value between 0 and 1,
Data
Bus
HT
Interface
VEE
Interface
WP
Interface
Safetyloop
Performance
loop
Positioning
system
Controllercomponent
HT
component
VEE
component
WP
component
Figure 5: Modules of the Controller component.
HT: Home Trainer, VEE: Virtual Exercise Environment,
WP: Web Portal.
where 1 indicates the best possible performance and
0 the worst possible performance.
(1)
The speed for the VEE is calculated based on the
performance and the configured maximal speed
constant (v
max
) as shown in equation (2).
∗
(2)
4.4.2 Safety Loop
The safety is handled by the safety module. The
safety module has three different states based on the
measured oxygen saturation level (SpO
2
). The SpO
2
is compared with a desaturation threshold as shown
in equation (3). The desaturation threshold is set in
the web portal. The status is stored for the
configured interval, for example 60 seconds. Based
on the status values the saturation state is determined
and the corresponding feedback is executed, as
shown in table 1.
Status SpO
DesaturationThreshold
(3)
Table 1: Saturation state in safety module based on
saturation status shown in equation (3).
Status values State Feedback
All true Good Continue normally
Some true Warning
Patient is urged to
slow down and
intensity is decreased
All false Bad
Training session is
terminated
The target power is decreased in case of the
warning state. As a result the performance loop will
DevelopmentofanIntegratedVirtualGroupTrainingSystemforCOPDPatients
105
lower the training intensity by lowering the
resistance of the home trainer.
4.4.3 Positioning System
Part of the motivational support is handled by the
positioning module. As mentioned above patient are
kept together in the virtual exercise environment.
When a patient gets too far behind the player in front
he will get a boost to prevent the patient from
getting farther behind. For this equation (2) is
extended with the speed correction factor (SCF).
The new formula is shown in equation (4). The SCF
is a value between 1 and 20. The farther a patient
gets behind, the larger the SCF value.
∗∗
(4)
5 IMPLEMENTATION
The four components described architecture is
implemented in a prototype:
HT: Bremshey BE5i home trainer with a polar
T31 heart rate belt.
VEE: WebAthletics cycling game running on an
Asus ME301T Android tablet with a 22” LG
22EA53VQ monitor placed in front of the
home trainer.
C: Developed in Java and is running on the same
tablet as the VEE.
WP: Developed on top of the Liferay Portal,
running on a dedicated server.
The Bremshey BE5i has a 32-step servo motor to
control the resistance, the gear. To support patients
with cycling at the right performance a controller
module is built to set the gear based on the
performance. When P
c
/P
target
< 0.6 for 5 seconds the
gear is shifted up. When P
c
/P
target
> 1.25 for 5
seconds the gear is shifted down.
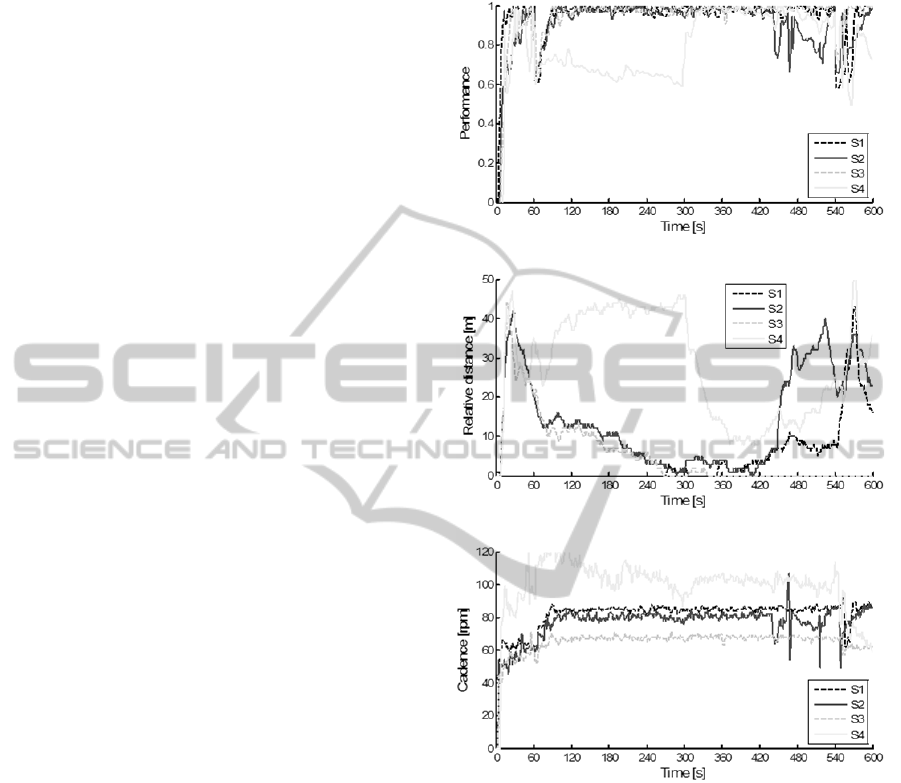
6 EVALUATION
The evaluation was performed with 4 healthy
subjects, cycling in separated rooms in the same
multiplayer session. Each subject was instructed to
cycle as close as possible to the given target power.
During the training session all relevant parameters
were recorded (time, power, cadence, heart rate,
speed in VEE, gear, distance, relative distance,
target power, performance and SCF). The relative
distance for each player is the distance between the
player and player in front. Performance, relative
distance and cadence are shown in figure 6. After
the training session subjects were asked to fill in a
short questionnaire.
Figure 6: Performance, Relative Distance and Cadence of
the four subjects during the exercise.
Results from the evaluation are shown in table 2.
The distance between all players is small (min: 0.0
m, mean: 13.1 m, max: 51.0 m), while the
performance for subject 4 was suboptimal. The
performance was calculated from the recorded
power and target power. This is compared with the
recorded performance. The average deviation is less
than 0.1%.
6.1 Control Modules
With a suboptimal performance of one of the
subjects the distance control module managed to
keep all subjects close to each other in the virtual
HEALTHINF2014-InternationalConferenceonHealthInformatics
106

Table 2: Evaluation results.
Subject S1 S2 S3 S4 All
Relative distance (m)
Min 0 0 0 0 0
Mean 4,3 14,2 5,4 28,3 13,1
Max 43 42 44 51 51
Performance
Mean 0,95 0,91 0,95 0,80 0,90
Performance deviation
Mean 0,003 0,000 0,002 -0,001 0,001
Standard
deviation
0,058 0,064 0,050 0,068 0,060
environment. The distance control module worked
correctly during the training. Also the performance
control module worked correctly. A small deviation
exists between real-time calculated performance and
the calculation afterwards. This might be caused by
a small delay in the power value used in the real-
time calculation.
6.2 Other Issues
The subjects reported some issues about the
automatic gear control, feedback on the performance
and feedback on the position of other users. The
automatic gear control caused the suboptimal
performance of one of the subjects. The subject was
cycling with a low power and high cadence, but the
gear didn’t shift up. Manual gear control can be
added to prevent this situation and give the users
more control. Feedback about the performance is
currently given by displaying the current power and
the target power in the virtual exercise environment.
Users have to compare these numbers themselves to
get an indication about their performance, while the
performance is an important parameter during the
training session. Suggested is to use a graphical
performance indicator.
Finally remarks were given about the position of
other users in the virtual environment. A user can
see other players in front of him with a limited
range. Players who are too far in front or behind the
user are not visible. A rear view or a third person
view, a map of the environment with indicators of
the other players, will overcome this problem.
7 DISCUSSION AND
CONCLUSIONS
The goal of the Integrated Training System is to
facilitate improvement and maintenance of the
physical condition of COPD patients safely at home
using a (virtual) group environment. The current
prototype satisfies to the goal of the system, but
leaves room for improvement. Further evaluation is
recommended.
The algorithms used in controller modules need
to be validated. For each algorithm several aspects
of the algorithm can be varied. For example with the
performance module the performance increases
linear with an increasing power, when the power is
lower than the target power. When the power is
higher than the target power the performance
decreases hyperbolic. This could be replaced by a
linear function as well. Further evaluation will
determine which alternative is the best indicator for
the performance. The gear algorithm can be
improved when the cadence is taken into account.
With a high cadence the threshold to shift up can be
decreased, while with a low cadence the threshold to
shift down can be decreased.
In this paper the technical design of the
Integrated Training System is described. Further
research into the economic and legal aspects is
needed. A sound business case should be created.
Motivation theories are implemented in the system.
The next step is to evaluate the system in a clinical
trial with the objective to evaluate the system
functionality with respect to the motivational
strength and to investigate the effectiveness of the
system with respect to improvements of adherence
to the therapy.
The focus is on COPD patients in this study.
However the Integrated Training System can be used
for other groups with no or only limited adaptations
to the system. It can be used for Chronic Heart
Failure patients or even elderly people in common to
facilitate improvement of the physical condition to
improve the quality of life.
REFERENCES
Anderson-Hanley, C., Arciero, P. J., Brickman, A. M.,
Nimon, J. P., Okuma, N., Westen, S. C., Zimmerman,
E. A. (2012). Exergaming and older adult cognition: A
cluster randomized clinical trial. American Journal of
Preventive Medicine, 42(2), 109-119.
Bailey, B. W., & McInnis, K. (2011). Energy cost of
exergaming: A comparison of the energy cost of 6
forms of exergaming. Archives of Pediatrics and
Adolescent Medicine, 165(7), 597-602.
Beauchamp, M. K., Francella, S., Romano, J. M.,
Goldstein, R. S., & Brooks, D. (2013). A novel
approach to long-term respiratory care: Results of a
community-based post-rehabilitation maintenance
DevelopmentofanIntegratedVirtualGroupTrainingSystemforCOPDPatients
107

program in COPD. Respiratory Medicine, 107(8),
1210-1216.
Botman, M.P.L. (2013). Design and evaluate a webportal
for physiotherapists and COPD patients for virtual
group training at home. (MSc Master Thesis),
University of Twente, Enschede. (BSS 13-21).
Burke, Shauna M, Carron, Albert V, Eys, Mark A,
Ntoumanis, Nikos, & Estabrooks, Paul A. (2006).
Group versus individual approach? A meta-analysis of
the effectiveness of interventions to promote physical
activity. Sport and Exercise Psychology Review, 2(1),
19-35.
Croitoru, A., Ioniţǎ, D., Stroescu, C., Pele, I., Gologanu,
D., Dumitrescu, A., Bogdan, M. A. (2013). Benefits of
a 7-week outpatient pulmonary rehabilitation program
in COPD patients. Pneumologia, 62(2), 94-101.
Dikken, J. B. J. (2012). Design and evaluation of an
Integrated Training System for COPD patients. (MSc
Master Thesis), University of Twente, Enschede.
(BSS 12-04).
Dikken, J. B. J., van Beijnum, B. J. F., & Hermens, H. J.
(2013). Integrated Training System for the
improvement of the physical condition of COPD
patients. Paper presented at the Fourth Dutch
Conference on Bio-Medical Engineering, Egmond aan
Zee, the Netherlands.
Du Moulin, M., Taube, K., Wegscheider, K., Behnke, M.,
& Van Den Bussche, H. (2009). Home-based exercise
training as maintenance after outpatient pulmonary
rehabilitation. Respiration, 77(2), 139-145.
Egan, C., Deering, B. M., Blake, C., Fullen, B. M.,
McCormack, N. M., Spruit, M. A., & Costello, R. W.
(2012). Short term and long term effects of pulmonary
rehabilitation on physical activity in COPD.
Respiratory Medicine, 106(12), 1671-1679.
Garcia-Aymerich, J., Farrero, E., Félez, M. A., Izquierdo,
J., Marrades, R. M., & Antó, J. M. (2003). Risk factors
of readmission to hospital for a COPD exacerbation: A
prospective study. Thorax, 58(2), 100-105.
Global Initiative for Chronic Obstructive Lung Disease.
(2013). Global Strategy for the Diagnosis,
Management, and Prevention of Chronic Obstructive
Pulmonary Disease.
Gosselink, R. (2002). Respiratory rehabilitation:
improvement of short- and long-term outcome. Eur
Respir J, 20(1), 4-5.
Gosselink, R., Langer, D., Burtin, C., Probst, V.,
Hendriks, H.J.M., van der Schans, C.P., Muris, J.
(2008). KNGF-richtlijn Chronisch obstructieve
longziekten: Koninklijk Nederlands Genootschap voor
Fysiotherapie.
House, James S. (1981). Work stress and social support.
Reading, Mass.: Addison-Wesley Pub. Co.
Huis in't Veld, R. M. H. A., Widya, I. A., Bults, R. G. A.,
Sandsjo, L., Hermens, H. J., & Vollenbroek-Hutten,
M. M. R. (2010). A scenario guideline for designing
new teletreatments: A multidisciplinary approach.
Journal of Telemedicine and Telecare, 16(6), 302-307.
Janssen, Peter. (2001). Lactate Threshold Training:
Human Kinetics Publishers.
Karapolat, H., Atasever, A., Atamaz, F., Kirazli, Y.,
Elmas, F., & Erdinç, E. (2007). Do the benefits gained
using a short-term pulmonary rehabilitation program
remain in COPD patients after participation? Lung,
185(4), 221-225.
Korczak, D., Huber, B., Steinhauser, G., & Dietl, M.
(2010). Outpatient pulmonary rehabilitation -
rehabilitation models and shortcomings in outpatient
aftercare. GMS Health Technol Assess, 6, Doc11. doi:
10.3205/hta000089.
Mathers, C. D., & Loncar, D. (2006). Projections of global
mortality and burden of disease from 2002 to 2030.
PLoS Medicine, 3(11), 2011-2030.
Nici, L., Donner, C., Wouters, E., Zuwallack, R.,
Ambrosino, N., Bourbeau, J., Troosters, T. (2006).
American thoracic society/European respiratory
society statement on pulmonary rehabilitation.
American Journal of Respiratory and Critical Care
Medicine, 173(12), 1390-1413.
Puente-Maestu, L., Sánz, M. L., Sánz, P., Cubillo, J.M.,
Mayol, J., & Casaburi, R. (2000). Comparison of
effects of supervised versus self-monitored training
programmes in patients with chronic obstructive
pulmonary disease. 15.
Puhan, M. A., Schünemann, H. J., Scharplatz, M, &
Bachmann, L. M. (2005). How should COPD patients
exercise during respiratory rehabilitation? Comparison
of exercise modalities and intensities to treat skeletal
muscle dysfunction. 60(367-375).
Rijksinstituut voor Volksgezondheid en Milieu. (2010).
Gezondheid en determinanten - Deelrapport van de
VTV 2010 Van gezond naar beter (N. Hoeymans, J. M.
Melse & C. G. Schoemaker Eds.). Houten: Bohn
Stafleu Van Loghum.
Ryan, R. M., Frederick, C. M., Lepes, D., Rubio, N., &
Sheldon, K. M. (1997). Intrinsic motivation and
exercise adherence. International Journal of Sport
Psychology, 28(4), 335-354.
Shahin, B., Germain, M., Pastene, G., Viallet, N., &
Annat, G. (2008). Outpatient pulmonary rehabilitation
in patients with chronic obstructive pulmonary
disease. International Journal of COPD, 3(1), 155-
162.
Sonderen, L. P. (1991). Het meten van sociale steun.
Groningen: University Library Groningen.
Spruit, M. A., Troosters, T., Trappenburg, J. C., Decramer,
M., & Gosselink, R. (2004). Exercise training during
rehabilitation of patients with COPD: a current
perspective. Patient Educ Couns, 52(3), 243-248. doi:
10.1016/S0738-3991(03)00098-3.
Tak, E., Kuiper, R., Chorus, A., & Hopman-Rock, M.
(2013). Prevention of onset and progression of basic
ADL disability by physical activity in community
dwelling older adults: A meta-analysis. Ageing
Research Reviews, 12(1), 329-338.
HEALTHINF2014-InternationalConferenceonHealthInformatics
108
