
Maintaining the Consistency of Electronic Health Record’s
Medication List
Juha Puustjärvi
1
and Leena Puustjärvi
2
1
Department of Computer Science, University of Helsinki, P.O. Box 68, Helsinki, Finland
2
The Pharmacy of Kaivopuisto, Neitsytpolku 10, Helsinki, Finland
Keywords: Electronic Health Record, HL7 RIM, CCD Standard, Medication List.
Abstract: An electronic health record (EHR) is a systematic collection of health information about an individual
patient. It includes a variety of types of observations entered over time by health care professionals,
recording observations and administrations of drugs and therapies, orders for the administration of drugs
and therapies, and test results. A well known problem is the consistency of EHR’s medication list: often
some of the prescribed drugs are missing, or some information is no more valid, e.g., some prescribed drugs
may be replaced by new drugs, or the dosage may be changed. In this paper we have focused on this
problem. We have restricted on EHRs and on prescriptions that are applications of the HL7 Reference
Information Model (RIM). Further, we have used the Refined Message Information Model (RMIM) to
specify the components that are extracted from prescriptions and transmitted into EHR. We have also
specified the criteria for medication list’s consistency, and the way it can be maintained. In addition, we
have studied the ways the RIM can be used in linking patient’s prescriptions among themselves such that
the name of the link indicates its semantics. By viewing patient’s prescriptions as a linked data structure we
can improve the effectiveness of prescriptions’ retrieval as well as provide expressive queries on patient’s
health documentation.
1 INTRODUCTION
An electronic health record (EHR) describes the
systematic documentation of a single patient's
medical history (Hartley and Jones, 2005). The main
goal of an EHR is to provide a complete and
accurate summary of the health and medical history
of a patient (NEHTA, 2006). It includes a variety of
types of observations entered over time by health
care professionals, recording observations and
administrations of drugs (Angst et al., 2008).
A well known problem is that EHRs’ medication
history is often out of date in the sense that some of
the prescribed drugs are missing, or some
information is no more valid, e.g., some prescribed
drugs may be replaced by new drugs, or the dosage
may be changed (Puustjärvi and Puustjärvi, 2011).
So, there is a risk for physician’s wrong diagnosis or
treatment decision.
In this paper we have focused on this problem.
We have studied how relevant medication data can
be extracted from prescriptions and transmitted to
the EHR such that the sender and receiver can
unambiguously interpret the semantics of the
exchanged messages.
It is not necessary to store the whole prescription
into an EHR as it is just a summary of the health and
medical history of a patient. For example, we have
omitted the context information of a prescription
such as who created it, when, where and for what
purpose. Yet the physician can retrieve such
information by following the link from the EHR to
the original prescription that is stored in a
prescription holding store. Anyway, storing the
information of prescribed drugs and dosages into
EHRs is of prime importance. Then a physician may
present data centric queries such as the average
blood pressure and/or cholesterol level during the
time periods the patient was using Emconcor (a drug
for blood pressure).
There are many standards, such as HL7 CDA
(HL7, 2004), EN 13606 (prEN13606, 2006) and
openEHR (openEHR, 2013) developed to digitally
represent clinical data. Nowadays EHR systems
increasingly use CDA’s CCD standard (CCD, 2009)
although it original purpose was to deliver clinical
330
Puustjärvi J. and Puustjärvi L..
Maintaining the Consistency of Electronic Health Record’s Medication List.
DOI: 10.5220/0005199203300335
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 330-335
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

summaries between healthcare organizations
(Benson, 2010).
With respect to the standards, we have restricted
on EHRs and on prescriptions that are applications
of the HL7 Reference Information Model (RIM),
i.e., they are based on the same terminology.
Further, we restricted on EHRs based on the CCD
standard as it is nowadays increasingly used for
storing medical summaries.
In order to achieve semantic interoperability
between the prescription holding store and the EHR
system we have to specify the semantics of the
exchanged message. In specifying the data elements
that are extracted from prescriptions and transmitted
to EHR we constrained the conceptual model of the
prescription, i.e., we constrained the Refined
Message Information Model (RMIM) of the
prescription.
Defining messages by RMIMs is a central idea of
the HL7 V3 approach (HL7, 2007). Each RMIM
diagram is derived from the RIM by limiting its
optionality in the sense that the designer can take
only the needed classes and attributes. Such
constrained specifications are called profiles. Hence,
EHRs based on CCD-standard, prescriptions as well
as the messages transmitted to EHR have profiles.
We have also studied the ways the RIM provides
for linking EHRs to prescriptions as well as linking
prescriptions among themselves such that the name
of the link (e.g., replaces) indicates the meaning of
the link. By viewing patient’s prescriptions as a
linked data structure we can improve the
effectiveness of prescriptions’ retrieval as well as
provide expressive queries on patient’s health
documentation.
The rest of the paper is organized as follows. In
Section 2, we first give a scenario of an electronic
prescription process, and then we give our
interpretations of the prescription concept. In
Section 3, we describe the prescription process from
communication architecture point of view, i.e., we
present the systems that are involved in prescription
process. In Section 4, we first give an overview of
the RIM, and then we illustrate how it is constrained
in modelling prescriptions as well as the messages
transmitted to the EHR.
In Section 5, we first present the structure of the
CCD documents, and then we describe how its
medication list can be linked into prescriptions
according to the modelling primitives of the RIM.
We also present our introduced notions of
medication list’s consistency and the ways it can be
maintained. In addition, we discuss the suitability of
our ideas for maintaining the consistency of personal
health records. Finally, Section 6 concludes the
paper by shortly discussing our future research.
2 PRESCRIPTION
Unfortunately there is no commonly used exact
interpretation of prescription concept. For example,
if the dosage of a prescription is changed or the
prescription is renewed whether we have modified
the existing prescription or whether we have
produced a new one?
We have adopted the interpretation that once the
prescription is stored in a prescription holding store
it cannot be changed. Yet, a prescription may be
invalidated and replaced by a new prescription.
Hence prescriptions may have mutual dependencies
which give rise for maintaining appropriate data
structures among patient’s prescriptions.
Our argument for not allowing prescriptions to
be changed is to avoid confusions. For example, if a
prescription is changed, then two physicians nay
have different views of the same prescription. In
addition, we only allow a prescription to be replaced
ones. However, the length of the replacement chain
is not restricted. The only requirement is that the
chain may not be cyclic as it indicates an error.
If a replaced prescription is retrieved, then the
whole replacement chain is presented for the user.
This ensures that the user can make the distinction
between valid and out date information in
prescriptions.
We have also made the distinction between
active and passive prescriptions: A prescription is
active, if all its prescribed drugs are not yet
dispensed or if the course of the drugs is not
finished; otherwise a prescription is passive.
Our argument is that passive prescriptions should
not be deleted from patient’s EHR. Otherwise,
queries such as “Give me the average blood pressure
during the time the patient was using drug A and
drug B” would require that both drugs are included
in active prescriptions.
3 THE ARCHITECTURE OF THE
SERVICE ORIENTED EPW
We now describe the architecture that can be used
for providing the services described in Section 2.
The architecture is based on the service oriented
computing paradigm (Singh and Huhns, 2005).
Basically, services are a means for building
MaintainingtheConsistencyofElectronicHealthRecord'sMedicationList
331
distributed applications more efficiently than with
previous software approaches. The main idea behind
services is that they are used for multiple purposes.
Services are also used by putting them together or
composing them. Therefore every aspect of services
is designed to help them to be composed.
In the health care sector service oriented
computing provides flexible methods for connecting
electronic prescription system to other relevant
health care systems (Puustjärvi and Puustjärvi,
2012). For example, electronic prescription writer
can interact through a Web service with the health
care system that supports patient records. There may
also be components that are used by different
healthcare systems. For example, medical database
may provide services for medical information
systems as well as for electronic prescription system.
The communication is based on Web services
and SOAP-protocol (SOAP, 2012). Originally they
provided a way for executing business transactions
in the Internet. Technically Web services are self-
describing modular applications that can be
published, located and invoked across the Web.
Once a service is deployed, other applications can
invoke the deployed service. In general, a Web
service can be anything from a simple request to
complicated business or eHealth processes.
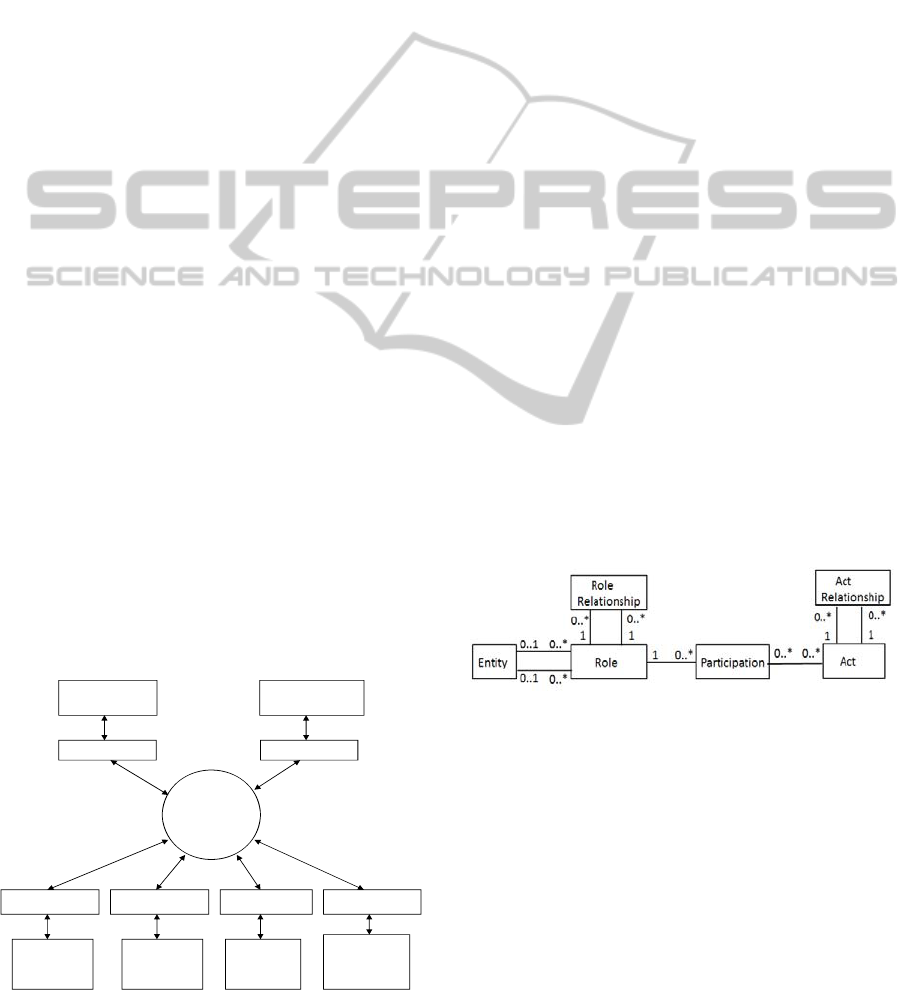
The components of the electronic prescription
system are presented in Figure 1. Each component
communicates through a Web service interface (WS-
interface). Further, each message is presented as an
XML-document, which is carried by the SOAP
protocol.
Although in this architecture EPW extracts
relevant data from prescription and transmits it to
the EHR system, we can also easily modify the
architecture such that the prescription holding store
carries out this function, i.e., transmits the extracted
data into the EHR. This functionality may also be
EPW
Expert
database
system
Medical
database
system
Prescription
holding store
Prescription
pricing
authority
Health care
system
WS-interface WS-interface
WS-interface WS-interface WS-interface
EHR
system
WS-interface
Figure 1: The Communication Architecture of the EPW.
EPW specific, i.e., depending on the EPW either it
or the prescription holding store transmits the
extracted data into the EHR. The analysis presented
in forthcoming sections is valid for all these
architectural choices.
4 MODELLING PRESCRIPTIONS
AND EXCHANGED MESSAGES
BY RMIMS
4.1 Reference Information Model Rim
The Reference Information Model RIM is the
cornerstone of the HL7 Version 3 development
process (Boone, 2011). It is the root of all
information models and structures developed as part
of the V3 development process.
The RIM is based on two key ideas (Benson,
2010). The first idea is based on the consideration
that most healthcare documentation is concerned
with “happenings” and things (human or other) that
participate in these happenings in various ways.
The second idea is the observation that the same
people or things can perform different roles when
participating in different types of happening, e.g., a
person may be a care provider such a physician or
the subject of care such as patient.
As a result of these ideas the RIM is based on a
simple backbone structure, involving three main
classes, Act, Role, and Entity, linked together using
three association classes Act-Relationship,
Participation, and Role-Relationship (Figure 2).
Figure 2: The RIM backbone structure.
The classes in the RIM have structured attributes
which specify what each RIM class means when
used in a message (exchanged document). The idea
behind structured attributes is to reduce the original
RIM from over 100 classes to a simple backbone of
six main classes.
Each happening, such as prescribing medication
or any CDA document is an Act, and it may have
any number of Participations, which are Roles,
played by Entities. An ACT may also be related to
other Acts via Act Relationships, i.e., it links Acts
together. Further, every ActRelationship has a
HEALTHINF2015-InternationalConferenceonHealthInformatics
332
source and target to which it points, and each Act
may have any number of AcRelationships. Its
typeCode, which is a structural attribute, describes
the type of association between Acts. These are
Composition (COMP), Documents (DOC), Fulfils
(FLFS), Refers (REF), and Replaces (REP).
The typeCodes REF and REP play a central role
in our solution: We use typeCode REF in linking the
medication list of an EHR to prescriptions, and
typeCode REP in linking prescriptions among
themselves.
4.2 Refined Message Information
Model RMIM
The RIM is not a model of healthcare, nor is it a
model of any message, although it is used in
messages. The structures of messages are defined by
constrained information models. The most
commonly used constrained information model is
the Refined Message Information Model (RMIM).
Each RMIM is a diagram that specifies the structure
of an exchanged message.
Each RMIM diagram is derived from the RIM by
limiting its optionality by omission and cloning
(Benson, 2010). Omission means that the RIM
classes or attributes can be left out. Note that all
classes and attributed that are not structural
attributes in the RIM are optional, and so the
designer can take only the needed classes and
attributes. Cloning means that the same RIM class
can be used many times in different ways in a
profile. For example, Patient and Employee are
specializations of Role, and so they may both appear
in the same diagram.
The multiplicities of associations and attributes
in the diagram are constrained in terms of
repeatability and optionality. Further, code binding
is used for specifying the allowable values of the
used attributes.
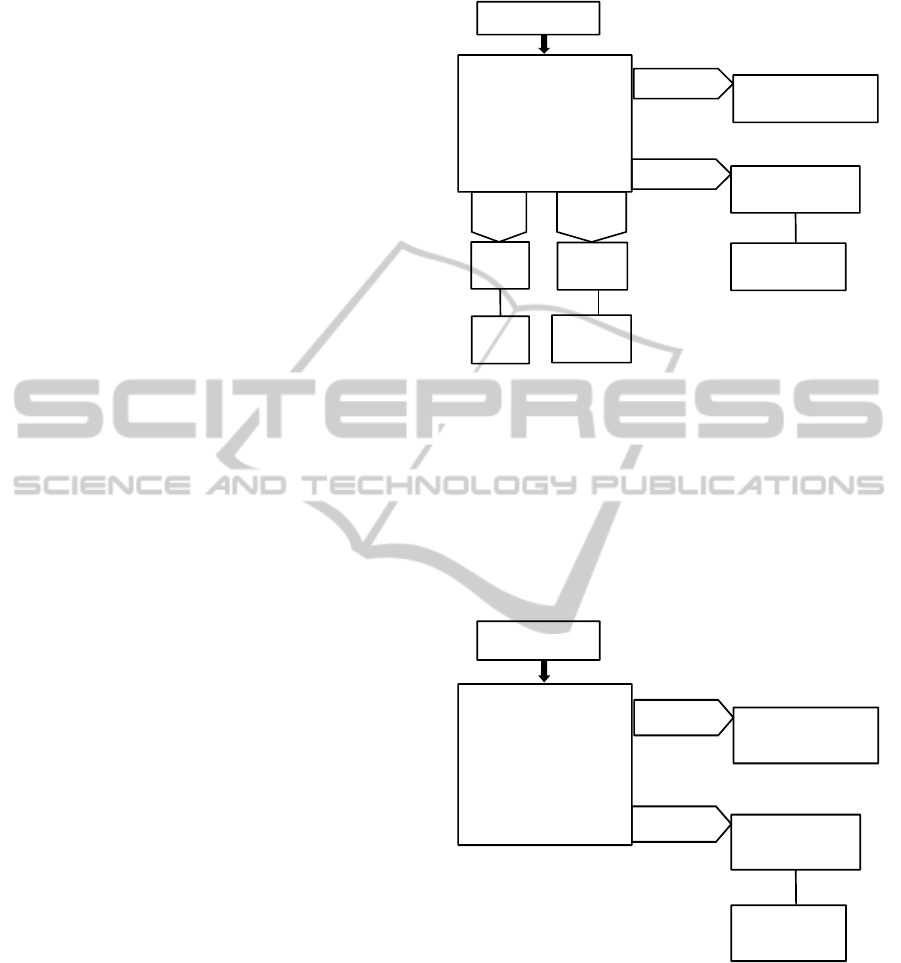
To illustrate the relationships of the RIM and
RMIM consider the RMIM diagram of Figure 3.
Note that HL7 uses its own representation of
UML in RMIM diagrams: each class has its own
color and shape to represent the stereotypes of these
classes, and they only connect in certain ways.
The entry point of this diagram (Prescription) is
SubstanceAdministration, which is a specialization
of the RIM class Act. Replaces is a specializations
of the association class ActRelationship. Patient and
Employee are specializations (subclasses) of the
RIM class Role. Person and Organization are
specializations of the RIM class Entity. Subject and
Performer are specializations of the association class
SubstanceAdministration
Subject Performer
Patient
Employee
Person
Organization
ManufacturedProduct
Consumable
1..1patientPerson
1..1employeeOrganization
1..*manufacturedProduct
Prescription
LabeledDrug
1..*manufacturedDrug
Replaces
0..*vitalSignsEvent
SubstanceAdministration
Figure 3: The RMIM of a simplified prescription.
Participation.
The diagram (drugsInPrescription) in Figure 4
specifies the RMIM for the message that the
prescription holding store (or EPW) transmits to the
EHR system. It is specified by constraining the
RMIM of the prescription by omission. In particular
the context information is left out from the
prescription.
SubstanceAdministration
ManufacturedProduct
Consumable
1..*manufacturedProduct
DrugsInPrescription
LabeledDrug
1..*manufacturedDrug
Replaces
0..*vitalSignsEvent
SubstanceAdministration
Figure 4: The RMIM of the message transmitted to EHR.
The XML-schemas of the exchanged messages are
derived from the RMIM such that the class and
attribute names of the diagram are the names of the
elements of the XML-schemas. So, the RMIM
diagram gives the semantics for the tags (elements)
of the exchanged messages.
MaintainingtheConsistencyofElectronicHealthRecord'sMedicationList
333

5 CONTINUITY OF CARE
DOCUMENT
5.1 CDA and CCD Standards
The HL7 Clinical Document Architecture (CDA) is
an XML-based markup standard intended to specify
the encoding, structure and semantics of clinical
documents for exchange (Boone, 2011). It is based
on the HL7 RIM, meaning that we can interpret the
semantics of its tags of the XML-documents by the
RIM.
Each CDA document has one primary purpose
(which is the reason for the generation of the
document), such as patient admission, transfer, or
inpatient discharge. The CCD specification is a
constraint on the HL7 CDA standard. The CCD
standard has been endorsed by HIMSS (Healthcare
Information and Management Systems Society
Though) (HIMSS, 2013) and HITSP (Healthcare
Information Technology Standards Panel) (HITSP,
2013) as the recommend standard for exchange of
electronic exchange of components of health
information.
Although the original purpose of the CCD
documents was to deliver clinical summaries
between healthcare organizations, nowadays it
increasingly used for other types of messages: it is
considered as set of templates because all its parts
are optional, and it is practical to mix and match the
sections that are needed (Benson, 2010). Hence,
there is a RMIM behind each CCD document.
5.2 The Structure of a CDA Document
A CCD document, as well as any CDA document, is
comprised of the Header and the Body (Benson,
2010). A simplified Level 3 CCD document
including the Header and the Medications section is
presented in Figure 5. The simple element REF in
the complex element Medication provides the link to
the original prescription. Note that there is only one
Medication element in the Medications element, and
so there is only one link (REF-element) in the
document.
<SimplifiedCCDfile>
<DocumentID>DOC_123</DocumentID>
<Patient>
<PatientID>AB-12345></PatientID>
<PatientName>Tim Jones></PatientName>
</Patient>
<Medications>
<Medication>
<REF>Prescription-123</REF>
<MedicationID>Medication.567</MedicationID>
<DateTime>
<ExactDateTime>
2012-03-01TO12:00
</ExactDateTime>
</DateTime>
<Source>
<Actor>
<ActorID>Pharmacy of Kaivopuisto</ActorID>
<ActorRole>Pharmacy</ActorRole>
</Actor>
</Source>
<Description>
<Text>One tablet three times a day</Text>
</Description>
<Product>
<ProductName>Voltaren</ProductName>
<BrandName>Diclofenac</BrandName>
</Product>
<Strenght>
<Value>50</Value>
<Unit>milligram</Unit>
</Strenght>
<Quantity>
<Value>30</Value>
<Unit>Tabs</Unit>
</Quantity>
</Medication>
</Medications>
</SimplifiedCCDfile>
Figure 5: A simplified example of a CCD document.
5.3 The Consistency of CCD’s
Medication List
We say that CCD document’s medication list
(Medications element) is well-formed, if each
Medication elements includes a link (i.e., REF-
element) to a prescription. It is exhaustive, if
patient’s all prescriptions are linked into the EHR.
Further if, the medication list is well-formed and
exhaustive, we say that it is consistent.
Whether the medication list is well formed can
be easily checked from patient’s EHR. Instead
whether it is exhaustive requires also accessing
patient’s prescriptions from prescription holding
store. However, assuming that the prescription
holding store follows the practise of linking its
prescriptions into EHRs, then there is no need for
such a checking.
6 CONCLUSIONS
As a patient may live in many places and use many
healthcare specialities, patient’s clinical documents
are often stored in several systems and locations.
However, patient’s all relevant documents should be
easily accessible for the physicians treating the
patient. Hence the EHRs, which provide a complete
HEALTHINF2015-InternationalConferenceonHealthInformatics
334

and accurate health and medical history of a patient
is of prime importance.
EHR systems usually organize clinical
documents into hierarchical structures that simplify
the search of documents, e.g., grouping together the
documents by episode, clinical specialty or time
period. Further, each clinical document is stored as a
stand-alone artefact, meaning that each document is
complete and whole in itself, including context
information such as who created it, when and where
and for what purposes. Without such contextual
information in some cases it may be a risk to
interpret some values of the data included on a
document.
On the other hand, considering each document
only as a complete and a whole in itself also has its
drawback. The problem here is that the efficient
usage of patients’ health documentation often is data
centric, meaning that data should be extracted from
various documents and then integrated according to
specific criteria. For example, a physician may be
interested to know the average blood pressure and/or
cholesterol level during the time periods the patient
was using a drug for blood pressure. Hence the
medical summaries such as the CCD documents are
of prime importance. However, maintaining the
consistency of the CCD documents is not an easy
task as it requires the interoperation of several
systems.
The key point in our presented solution for
achieving the consistency of CCD documents’
medication list is the semantic interoperability
between the prescription holding store and the EHR
system. Yet medication list is just a component of an
EHR. Ensuring the consistency of the other
components of the EHR is equally important. This
suggests that the semantic interoperability of the
EHR system and other systems that produce clinical
documents for the EHR is also of prime importance.
In our future research we will focus on this topic.
REFERENCES
Agarwal R, Angst C.M., 2006. Technology-enabled
transformations in U.S. health care: early findings on
personal health records and individual use, In Galletta
G, Zhang P, (Eds.), Human-Computer Interaction and
Management Information Systems: Applications (Vol.
5). Armonk, NY: M.E. Sharpe, Inc., pp. 357-378.
Angst, C.M., Agarwal, R, Downing, J., 2008. An
empirical examination of the importance of defining
the PHR for research and for practice, Proceedings of
the 41st Annual Hawaii International Conference on
System Sciences.
Benson, T., 2010. Principles of Health Interoperability
HL7 and SNOMED. Springer.
Boone, K., 2011. The CDA Book. Springer.
CCD, 2009. What Is the HL7 Continuity of Care
Document? Available at:
http://www.neotool.com/blog/2007/02/15/what-is-hl7-
continuity-of-care-document/
CCR, 2011. Continuity of Care Record (CCR) Standard.
Available at: http://www.ccrstandard.com/
Hartley, C., Jones, E., 2005. EHR Implementation. AMA
Press.
HIMSS, 2013. Healthcare Information and Management
Systems Society, Available at: http://himss.org/
HITSP, 2013. Healthcare Information Technology
Standards Panel, Available at: http://hitsp.org/
HL7, 2004. EHR System Functional Model and Standard
Draft Standard for Trial Use (DSTU).
HL7, 2007. What is the HL7 Continuity of Care
Document? Available at:
http://www.neotool.com/blog/2007/02/15/what-is-hl7-
continuity-of-care-document/
NEHTA. 2006. Review of shared electronic health record
standards. Version 1.0. National e- Health Transition
Authority, Available at:
http://www.nehta.gov.au/component/option,com_docman/
task,cat_view/gid,130/Itemid,139/
prEN13606, 2006.Health informatics – Electronic
healthcare record communication – Parts 1-5.
Committee European Normalisation, CEN/TC 251
Health Informatics Technical Committee. Available
at: http://www.centc251.org/
Puustjärvi, J. and Puustjärvi, L., Personal Health Book: A
Novel Tool for Patient Centered Healthcare. In the
Proc of the International Conference on Health
Informatics (HEALTHINF 2011). Pages 386-393.
2011.
Puustjärvi, J. and Puustjärvi, L.,. Moving from Remote
Patient Monitors to Cloud-Based Personal Health
Information Systems: a Way to Practicing Patient-
Centered Chronic Care Model. . In the Proc of the
International Conference on Health Informatics
(HEALTHINF 2012). Pages 37-45. 2012.
openEHR Foundation. Available at: http:
//www.openehr.org.
Singh, M., Huhns, M., Service Oriented Computing:
Semantics Proceses Agents. John Wiley & Sons, 2005.
SOAP, 2012. Simple Object Access Protocol. Available
at: http://www.w3.org/TR/SOAP/
MaintainingtheConsistencyofElectronicHealthRecord'sMedicationList
335
