On the Validation of Computerised Lung Auscultation
Guilherme Campos
1,2
and João Quintas
3
1
Departmento de Electrónica, Telecomunicações e Informática (DETI) – Universidade de Aveiro (UA),
Campus de Santiago, 3810-193 Aveiro, Portugal
2
Instituto de Engenharia Electrónica e Informática de Aveiro (IEETA) – Universidade de Aveiro (UA),
Campus de Santiago, 3810-193 Aveiro, Portugal
3
Instituto de Sistemas e Robótica (ISR) – Instituto Superior Técnico (IST),
Avenida Rovisco Pais 1, 1049-001 Lisboa, Portugal
Keywords: Adventitious Lung Sounds, Automatic Detection Algorithms, Annotation, Agreement, Performance Metrics,
Validation.
Abstract: The development of computerised diagnosis tools based on lung auscultation necessitates appropriate
validation. So far, this work front has received insufficient attention from researchers; validation studies found
in the literature are largely flawed. We believe that building open-access crowd-sourced information systems
based on large-scale repositories of respiratory sound files is an essential task and should be urgently
addressed. Most diagnosis tools are based on automatic adventitious lung sound (ALS) detection algorithms.
The gold standards required to assess their performance can only be obtained by human expert annotation of
a statistically significant set of respiratory sound files; given the inevitable subjectivity of the process,
statistical agreement criteria must be applied to multiple independent annotations obtained for each file. For
these reasons, the information systems we propose should provide simple, efficient annotation tools; facilitate
the formation of credible annotation panels; apply appropriate agreement criteria and metrics to generate gold-
standard ALS annotation files and, based on them, allow easy quantitative assessment of detection algorithm
performance.
1 INTRODUCTION
Easy, inexpensive and non-invasive, auscultation is
an age-old medical diagnosis method. The
stethoscope is a tribute to its paramount importance:
invented by Laënnec in 1816, it has become the most
universal symbol of the medical profession.
Diagnosing respiratory conditions through lung
auscultation is a skill healthcare practitioners acquire
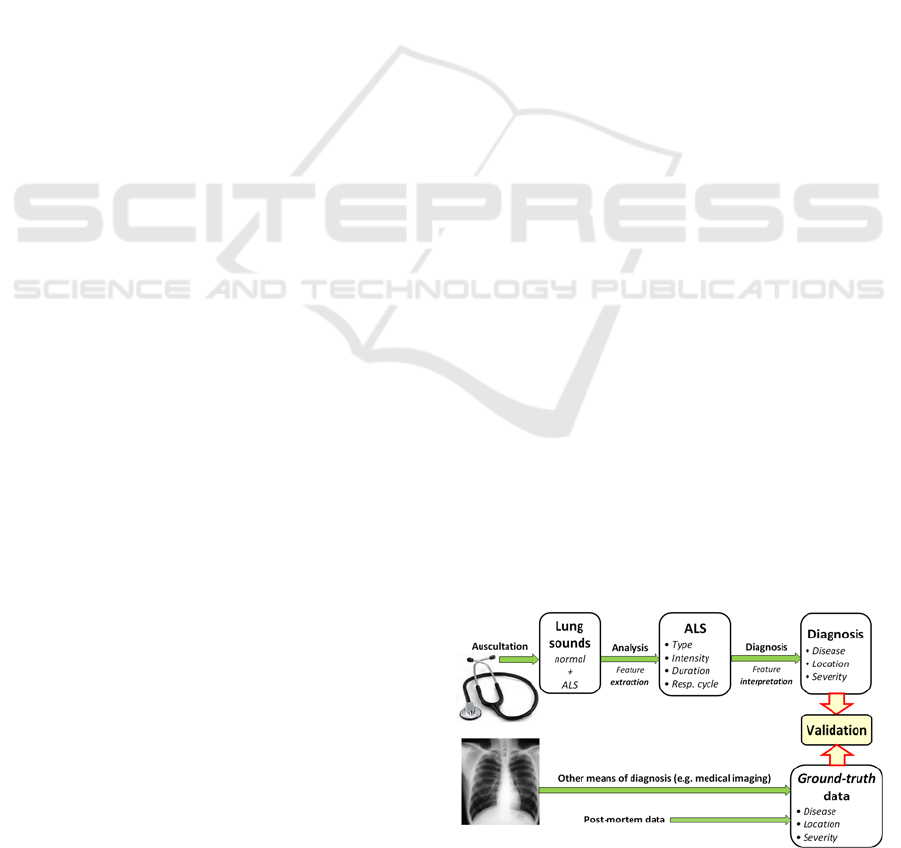
by training. As shown in the diagram of Figure 1, the
process can be decomposed into two steps.
The first is a sound analysis stage, based on the
notion of normal respiratory sounds and the ability to
identify abnormal features superimposed on them,
also called adventitious lung sounds (ALS). ALSs are
classified into various types according to their
acoustic characteristics. Classification criteria and
nomenclatures adopted in the literature may differ
slightly, as there is no universal standardisation; for
instance, Bohadana et al. (2014) list stridors,
wheezes, rhonchi, fine crackles, coarse crackles,
pleural friction rubs and squawks. Different sets of
clinical correlations have been established for each
ALS type.
Figure 1: Lung disease diagnosis based on auscultation.
Based on this accumulated knowledge, the second
step – diagnosis proper – consists in interpreting the
characteristics (type, intensity, duration, instant of
occurrence within the respiratory cycle…) of the ALS
observed in different auscultation points in order to
654
Campos G. and Quintas J..
On the Validation of Computerised Lung Auscultation.
DOI: 10.5220/0005293406540658
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 654-658
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)
establish the disease, its severity and area affected. As
Figure 1 suggests, the results can only be validated
against ground-truth data obtained through more
reliable diagnosis means (e.g. medical imaging) or
post-mortem examination.
2 AUTOMATIC ALS DETECTION
Carried out in the traditional guise (i.e. by humans),
and despite constant progress towards standardisation
and sophistication of auscultation training methods
and technology (see, for instance, Ward and Wattier’s
2011 review), the signal analysis process depicted in
Figure 1 is rather subjective; obviously, it is also
restricted to the human audible frequency range.
Computer-aided auscultation is potentially much
more objective, reliable and efficient. With the advent
of digital stethoscopy, its development became a real
prospect (reflected, for example, in the 1997 review
by Pasterkamp et al.). The EU-funded project
Computerised Respiratory Sound Analysis (CORSA),
involving a multinational task force of the European
Respiratory Society (Sovijärvi et al. 2000), marked a
research boom in this area. Naturally inspired by the
human auscultation process, depicted in Figure 1,
research efforts were primarily directed at automating
its first step – ALS detection.
The literature evidences intense work on the
development of algorithms applying pattern
recognition techniques to detect and classify the
various ALS types. Taking the example of crackle
detection (arguably the most important and certainly
one of the most challenging, given the discontinuous,
non-stationary nature of crackles), a wide variety of
signal processing techniques have been proposed,
including digital filters (Ono et al. 1989), spectrogram
analysis (Kaisla et al. 1991), auto-regressive models
(Hadjileontiadis 1996), time-domain analysis
(Vannuccini et al. 1998), fuzzy filters (Mastorocostas
et al. 2000), wavelet and wavelet-packet transform
methods (Kahya et al. 2001; Hadjileontiadis 2005; Lu
and Bahoura 2006; Lu and Bahoura 2008), fractal
dimension (FD) filtering (Hadjileontiadis and
Rekanos 2003), Hilbert transform analysis (Li and Du
2005) and empirical mode decomposition (EMD)
(Charleston-Villalobos et al. 2007; Hadjileontiadis
2007). This list is by no means exhaustive and similar
efforts have gone into the development of detection
algorithms for other ALS types, especially wheezes.
However, by and large, research publications in
this area reveal serious imbalance between
development and validation work, with insufficient
attention paid to the latter. To better characterise this
problem and support the practical solution proposed
for it in section 4, the next section discusses ALS
detection algorithm validation and its specific
requirements.
3 VA L I D AT I O N I S S U E S
ALS waveforms can be characterised qualitatively,
but establishing completely objective definitions is
not possible (if it were, developing an algorithm with
100% detection accuracy would be a simple task).
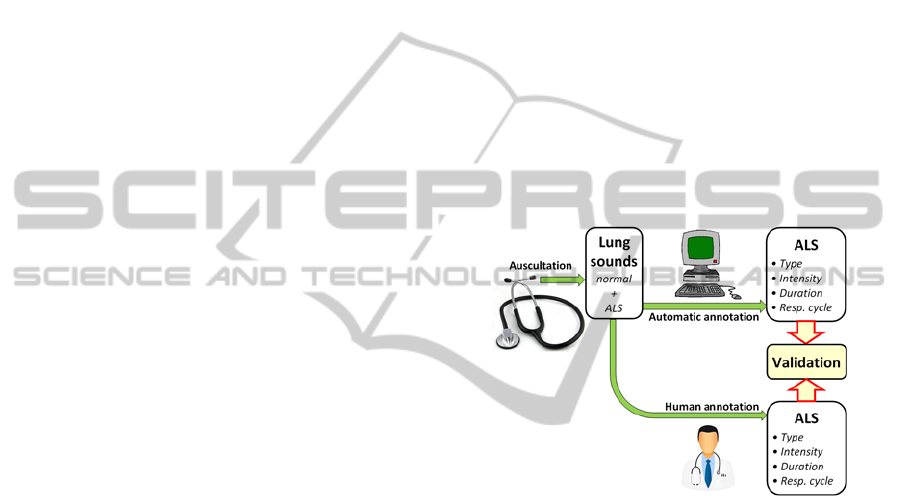
The performance of automatic ALS detection
algorithms can thus only be assessed by comparing
the annotations they generate with human expert
annotations of the same sound files, as illustrated in
Figure 2. In this context, the term annotation refers to
a complete record of the ALS of a given type
occurring in the sound file under analysis.
Figure 2: Validation of automatic ALS detection algorithm.
Given the subjectivity of human annotation, pointed
out in the previous section, it is essential to take
measures to minimise bias. For this reason, validation
references should be obtained by combining multiple
annotations of the same sound file, each carried out
independently by a different human expert, into a
single gold-standard annotation. The criteria
governing this combination or agreement process
must be explicit. For instance, the pilot study by
Quintas et al. (2013) used agreement by majority, but
other approaches can and should be explored.
Performance tests reported in the literature are
very often based on annotations by a single expert,
thus lacking credibility. In the rare instances of multi-
annotation, the criteria used for generating gold
standards are normally not clarified.
For statistical significance, both the panels of
expert annotators and the sets of annotated sound files
should be as large and diverse as possible. The
development of pattern recognition algorithms often
OntheValidationofComputerisedLungAuscultation
655
relies on training; obviously, training and test sets
must be separate i.e. performance tests cannot be
based on the same files used for training. This
constitutes an additional argument in favour of
building large, diverse repositories of sound files and
corresponding gold-standard annotations, but the
repositories actually used in practice tend to be very
small and relatively homogeneous.
It is clear from the previous discussion that the
availability of complete, reliable and user-friendly
computational tools for respiratory sound annotation
is essential. The use of open annotation file formats is
desirable. The crackle, wheeze and respiratory cycle
annotation application RSAS (Dinis et al., 2012) was
an effort in this direction. Regrettably, making this
kind of tools publicly available is not yet the rule.
In general, replicating the detection algorithm
tests described in the literature is virtually impossible,
as there is no easy access to the relevant data (sound
files and reference annotations). Any performance
claims under these circumstances would lack
credibility. Since absolute agreement between the
annotations used to build a gold standard is extremely
unlikely (the small pilot study on multi-annotation
presented in Dinis et al. (2012) strongly supports this
idea), some extreme performance claims found in the
literature may be signs of methodological flaws
related to the use of single-annotator data, artificially
homogeneous sound repositories (Quintas et al. 2013)
or even performance indices measured on training set
files.
The creation of a Web-based open information
system to stimulate the development and sharing of
respiratory sound data and annotation repositories,
annotation tools, gold standards, agreement metrics
and criteria, as well as detection algorithms, is
essential to solve the difficulties discussed and
advance research in this area.
4 ALS INFORMATION SYSTEM
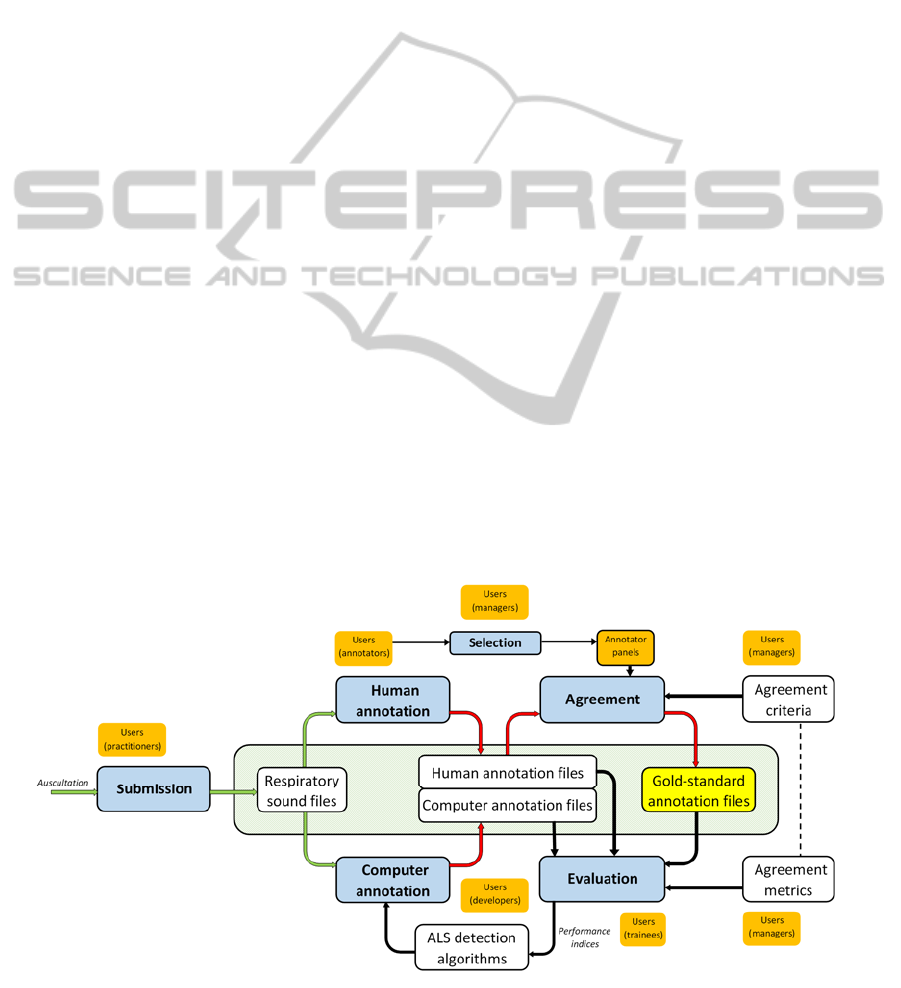
The information system we propose is outlined in
Figure 3. The idea is to base it on an Internet platform
and feed it through crowdsourcing i.e. by attracting
contributions from the respiratory healthcare
community worldwide. This point is emphasised in
the figure by the association of the various functional
modules with user classes, loosely labelled managers,
practitioners, annotators, developers and trainees.
At the core of this information system lies a
repository of lung auscultation sound files obtained
through digital stethoscopy. The aim is to make it as
expanded and diversified as possible. The online
sound file submission module must therefore be
versatile and user-friendly. It must accommodate
multi-channel stethoscopy data.
The records associated with the submitted sound
files should be as complete as possible (without
compromising patient anonymity), since successful
data-mining using the system will depend crucially on
access to data on the patient (age, gender, ethnicity,
weight, clinical antecedents,…), auscultation
conditions (location, equipment, procedures,…) and
results from other means of diagnosis (e.g. medical
imaging).
Academic research projects may be particularly
valuable in building a repository of this kind,
inasmuch as they can contribute large-scale data-sets
Figure 3: Web-based respiratory sound information system.
HEALTHINF2015-InternationalConferenceonHealthInformatics
656
obtained under controlled conditions.
It must be possible to define and label sets of
sound files within the repository, for the purposes of
generating gold standards, training detection
algorithms and testing their performance.
An essential tool of this system is the human
annotation module: a graphical user interface (GUI)
along the lines of RSAS (Dinis et al. 2012). It should
allow simple, intuitive annotation of any respiratory
sound file stored in the repository, the result being a
new file (annotation file) tagged to the corresponding
sound file/annotator pair and stored in a repository of
annotation files. Dinis et al. (2012) propose formats
for crackle, wheeze and respiratory cycle annotation
files.
Annotating files may be of interest to users of very
different levels. For example, the system can assist
non-experts (trainees) practice and assess their
performance. For the purpose of generating gold-
standards, however, it is important to select expert
annotator panels from the pool of annotators. As seen
in the previous section, the gold standards, generated
by the agreement module, combine multiple
annotations of the same sound file (one per panel
member) according to explicit agreement criteria.
The system must, of course, support computer
annotation through an interface to automatic ALS
detection algorithms; these must be able to collect
sound files (from test sets or training sets) and submit
their corresponding annotations, which must be
tagged accordingly and stored in the repository as any
other annotation.
The evaluation module applies appropriate
agreement metrics, consistent with the criteria used
for generating the gold standard annotations, to
compute detection performance indices. This can be
used both on computer annotations (to assist the
process of ALS detection algorithm training and
validation) and human annotations (to assist the
training and assessment of healthcare practitioners).
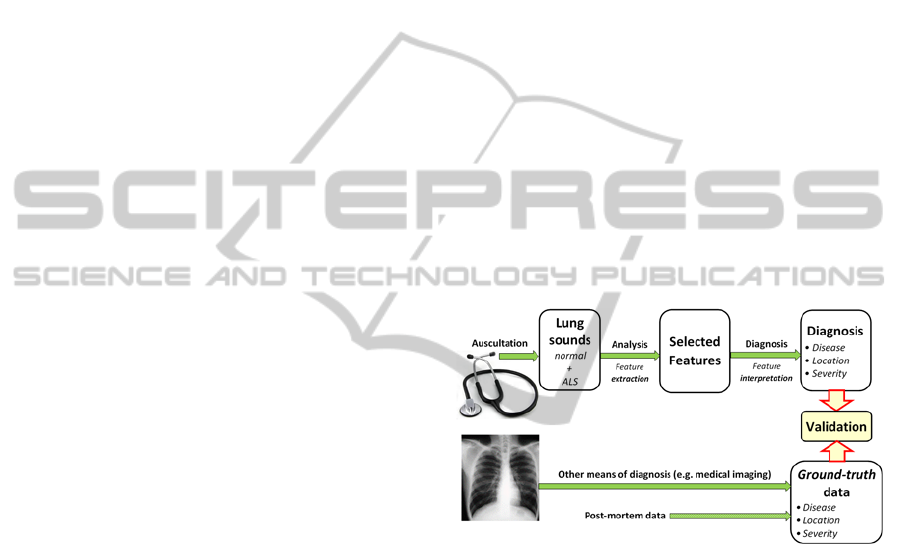
5 MACHINE LEARNING
ALS detection algorithms are intended to automate
the first step of the process outlined in Figure 1,
assuming that diagnosis proper will remain a human
task. However, with the unceasing progress of
computing, signal processing and communication
technologies, it is possible to envisage fully
automated respiratory disease diagnosis and
monitoring systems. This involves automating both
the feature extraction and the interpretation steps.
In this scenario, adventitious lung sounds lose
importance. Pattern recognition can be applied with
no a priori restrictions on which features to be
considered. This may prove a significant advantage
with machine learning techniques such as genetic
algorithms, support vector machines or neural
networks, as different features (for example in the
ultrasound frequency range, completely disregarded
by ALS) may contribute to more accurate diagnosis
results. In this regard, an analogy may be drawn with
music genre classification algorithms, whose
performance has improved significantly with the
increasing use of machine-selected low-level features
with no obvious musical meaning and seemingly
unrelated to the human process of musical style
identification.
The difficulty of this approach, in this case, is the
long validation loop. The intermediate validation of
the feature extraction step (see Figure 2) is no longer
applicable; the performance of automatic diagnosis
algorithms must be directly compared with ground-
truth results from other means of diagnosis, as shown
in Figure 4.
Figure 4: Automatic respiratory disease diagnosis.
This makes it even more indispensable to create an
information system with an extensive lung sound
repository fed by crowd-sourcing, as described in the
previous section; naturally, the modules related to
ALS annotation would not be necessary in this
approach.
REFERENCES
Bohadana A, Izbicki G, Kraman SS (2014) “Fundamentals
of lung auscultation.” The New England Journal of
Medicine, 370(8): 744-751.
Charleston-Villalobos S, González-Camarena R, Chi-Lem
G, Aljama-Corrales T (2007) "Crackle sounds analysis
by empirical mode decomposition. Nonlinear and
nonstationary signal analysis for distinction of crackles
OntheValidationofComputerisedLungAuscultation
657

in lung sounds." IEEE Engineering in Med. and
Biology Magazine 26(1): 40-47.
Dinis J, Campos G, Rodrigues J, Marques, A (2012)
“Respiratory sound annotation software.” Int. Conf. on
Health Informatics (HEALTHINF’12), 183-188.
Vilamoura, Portugal, February 1-4.
Hadjileontiadis LJ (1996) "Nonlinear separation of crackles
and squawks from vesicular sounds using third-order
statistics." 18
th
Annual Int. Conf. of the IEEE
Engineering in Medicine and Biology Society 5: 2217-
2219.
Hadjileontiadis LJ (2005) "Wavelet-based enhancement of
lung and bowel sounds using fractal dimension
thresholding-part I: methodology.” IEEE Trans. on
Biomedical Engineering 52(6): 1143-1148.
Hadjileontiadis LJ (2007) "Empirical mode decomposition
and fractal dimension filter. A novel technique for
denoising explosive lung sounds." IEEE Engineering in
Med. and Biology Magazine 26(1): 30-39.
Hadjileontiadis LJ, Rekanos T (2003) "Detection of
explosive lung and bowel sounds by means of fractal
dimension." IEEE Signal Processing Letters 10(10):
311-14.
Kahya YP, Yerer S, Cerid O (2001) “A wavelet-based
instrument for detection of crackles in pulmonary
sounds.” 23
rd
Annual Int. Conf. of the IEEE
Engineering in Med. and Biology Society, 2001. 4:
3175-3178.
Kaisla T, Sovijärvi ARA, Piirilä P, Rajala HM, Haltsonen
S, Rosqvist T (1991) "Validated method for automatic
detection of lung sound crackles." Medical & biological
engineering & computing 29(5): 517-521.
Li Z, Du M (2005) “HHT based lung sound crackle
detection and classification.” 2005 Int. Symposium on
Intelligent Signal Processing and Communication
Systems 385-388.
Lu X, Bahoura M (2006) "Separation of crackles form
vesicular sounds using wavelet packet transform." Int.
Conf. on Acoustics, Speech and Signal Processing
(ICASSP 2006).
Lu X, Bahoura M (2008) "An integrated automated system
for crackles extraction and classification." Biomedical
Signal Processing and Control 3(3): 244-254.
Mastorocostas PA, Tolias YA, Theocaris JB,
Hadjileontiadis LJ, Panas SM (2000). "An orthogonal
least squares-based fuzzy filter for real-time analysis of
lung sounds." IEEE Transactions on Bio-medical
Engineering 47(9): 1165-76.
Ono M, Arakawa K, Mori M, Sugimoto T, Harashima H
(1989). "Separation of fine crackles from vesicular
sounds by a nonlinear digital filter." IEEE transactions
on bio-medical engineering 36(2): 286-291.
Pasterkamp H, Kraman SS, Wodicka G (1997) "Respiratory
Sounds. Advances Beyond the Stethoscope." American
Journal of Respiratory and Critical Care Medicine
156(3): 974-87.
Quintas J, Campos G, Marques A (2013) “Multi-algorithm
respiratory crackle detection.” Int. Conf. on Health
Informatics (HEALTHINF’13), 239-244. Barcelona,
Spain, February 11-14.
Sovijärvi ARA, Vanderschoot J, Earis J E (2000)
“Standardization of computerized respiratory sound
analysis”. European Respiratory Review 10:77, 585.
Vannuccini L, Rossi M, Pasquali G (1998) "A new method
to detect crackles in respiratory sounds." Technology
and Health Care 6(1): 75-79.
Ward JJ, Wattier BA (2011) “Technology for enhancing
chest auscultation in clinical simulation”. Respiratory
Care 56(6): 834-845.
HEALTHINF2015-InternationalConferenceonHealthInformatics
658
