Hand Reach Star Excursion Balance Test as a Measure of
Joint Mobility
O. Eriksrud
1
, J. Cabri
1
and P. Federolf
2
1
Department of Physical Performance, Norwegian School of Sport Sciences, Oslo, Norway
2
Faculty of Psychology and Sport Science, University of Innsbruck, Innsbruck, Austria
1 OBJECTIVES
Joint range of motion (ROM) is commonly
measured using goniometry with accepted reference
values such as American Academy of Orthopedic
Surgeons (AAOS) (Greene and Heckman, 1994).
The procedures of obtaining these measures are
based on unidirectional and uniplanar passive testing
of isolated joint motions in supine, prone or seated
positions.
The relationship of such ROM measures to
performance have been found to be variable (Craib
et al., 1996; Menz et al., 2006). Utilizing tests of the
full kinematic chain from an upright standing
position that involve the concurrent use of multiple
joints, directions and planes of motion might be one
solution to the shortcomings of the traditional ROM
testing procedures. Full kinematic chain tests have
the advantage of greater specificity to most human
movements such as athletic performance.
The Star Excursion Balance Test (SEBT) is a
widely accepted test of dynamic postural control and
balance (Gribble et al., 2012) that challenges
coordination, mobility, and strength (Hubbard et al.,
2007). However it does not challenge all joint
movements at and above the hip (Delahunt et al.,
2013), but it offers a platform from which a whole-
body mobility and balance test can be created. In the
current study we propose a Hand Reach Star
Excursion Balance Test (HSEBT), which combines
a systematic use of unilateral and bilateral hand
reaches, thus also challenging mobility in hip and
upper body joints.
The purposes of this study were to (1) provide
joint movement reference data for HSEBT; and (2)
compare the 22 elicited joint movements of the
ankle, knee, hip and spine elicited by HSEBT to
ROM reference values and joint movements elicited
by SEBT.
2 METHODS
Twenty-eight healthy male subjects without
musculoskeletal dysfunction in the past 6 months
volunteered for the study. HSEBT was performed on
a testing grid that featured nine concentric circles at
10 cm intervals with eight vectors projecting from
the centre of the mat at 45° intervals and marked at
one centimetre intervals. The vectors were used as
reference for the horizontal reach tests (HR) and
named as follows: 1) Anterior (A0). 2) Left 45
(L45). 3) Right 45 (R45). 4) Left 90 (L90). 5)
Right 90 (R90). 6) Left 135 (L135). 7) Right 135
(R135) and 8) Posterior (P180). All HR are
measured in centimetres (cm). The rotational reaches
(RR) were measured in degrees () using the outer
concentric circle with degrees identified at 5
intervals. When performing overhead or rotational
reaches a plumbline was used to project reach
distance to the mat. All subjects performed 20 hand
reaches, 10 on each leg, in the same order without
warming up.
Movements of the participants were captured
using 58 reflective markers and fifteen Oqus
cameras (ProReflex®, Qualisys Inc., Gothenburg,
Sweden) recording at 480 Hz to create the foot, leg,
thigh, pelvis, thorax and upper arm segment. Data
analysis was performed using Visual 3D® (C-
Motion Inc., Rockwille MD, USA).
Three-dimensional joint movements of the foot,
knee, hip and trunk (=
max
-
start
) triggered by
different hand reach tests were calculated from
starting (
start
= mean
frames 5-100
) and maximum reach
position (
max
) of the fifth metacarpal marker of the
reaching hand(s). The maximum reach position was
defined to reflect the maximum HR and RR scores.
Descriptive statistics were then calculated for all
joint movements and hand reach performance.
Eriksrud, O., Cabri, J. and Federolf, P..
Hand Reach Star Excursion Balance Test as a Measure of Joint Mobility.
Copyright
c
2015 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
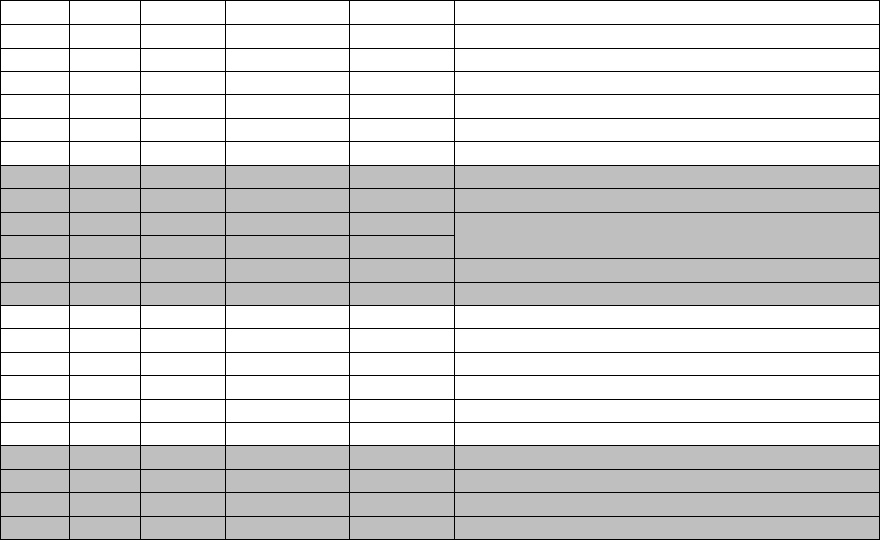
Table 1: HSEBT joint movement comparison to selected ROM reference values.
Joint Plane Motion Test
Result () ROM reference values ()
Foot Sag DF R45 29.2±6.0
2
11-27 (Lindsjo et al., 1985; Mudge et al., 2013)
Sag PF LROT 0.4±4.6 36-56 (Boone and Azen, 1979; Lindsjo et al., 1985)
Front Ev R90 18.1±3.2
2
13-34 Schwarz, 2011 #1564;Macedo, 2009 #1567}
Front Inv L90 7.8±4.4 21-43 (Macedo and Magee, 2009; Schwarz et al., 2011)
Trans Abd RROT 14.2±3.5 NR
Trans Add LROT 16.9±5.1 NR
Knee Sag Flex A0 94.3±22.4 132-149 (Macedo and Magee, 2009; Roach and Miles, 1991)
Sag Ext RROT 7.9±12.8 -2 -4 (Boone and Azen, 1979; Mudge et al., 2013)
Front Abd LROT 5.5±2.4
2
frontal plane movement arch of 13° at 20° of knee flexion
(Levangie and Norkin, 2011).
Front Add R45 18.2±6.9
2
Trans IR LROT 15.7±3.7
2
15 (Almquist et al., 2002)
Trans ER RROT 24.4±5.2
2
20 (Almquist et al., 2002)
Hip Sag Flex R45 109.0±8.2 113-133 (Macedo and Magee, 2009; Sankar et al., 2012)
Sag Ext L135 30.5±6.9
2
3-19 (Moreside and McGill, 2011; Roach and Miles, 1991)
Front Abd L90 18.2±7.4 34-60 (Macedo and Magee, 2009; Sankar et al., 2012)
Front Add R90 28.3±5.3
2
14-31 (Roaas and Andersson, 1982; Sankar et al., 2012)
Trans IR LROT 27.2±5.3
2
27-58 (Moreside and McGill, 2011; Mudge et al., 2013)
Trans ER RROT 32.2 ±5.4
2
32-48 (Mudge et al., 2013; Roach and Miles, 1991)
Trunk Sag Flex A0 58.1±9.0 Lumbar: 40-60 Thoracic: 20-45 (Magee, 2006)
Sag Ext P180 35.1±7.8 Lumbar: 20-35 Thoracic: 25-40
(Magee, 2006)
Front Lat Flex L90/R90 38.1±6.7
1, 2
Lumbar: 15-20 Thoracic: 20-40
(Magee, 2006)
Trans Rot LROT/RROT 33.1±4.3
1
Lumbar: Rot: 3-18 Thoracic: 35-50
(Magee, 2006)
1
= kinematic average of two tests
2
= within or greater than range of ROM reference values
Abbreviations: NR=None Reported; L=Left; R=Right; B=Bilateral; DF=Dorsiflexion; PF=Plantarflexion; Ev=Eversion; Inv=Inversion;
Abd=Abduction; Add=Adduction; Flex=Flexion; Ext=Extension; IR=Internal Rotation; ER=External Rotation; Lat Flexion= Lateral
flexion; Rot=Rotation
3 RESULTS
Twenty-eight healthy male subjects (age 23.8 2.2
years; height 181 6.0 cm; weight = 78.3 9.2 kg)
completed all 20 tests. The HSEBT test that elicited
the greatest joint movement, plane and direction, of
the ankle, knee, hip and spine is identified in Table
1. HSEBT elicited eleven out of twenty-two joint
movements within or greater than goniometric ROM
reference values.
4 DISCUSSION
Dorsiflexion (29.2±6.0°) is greater than ROM
reference values. However, more appropriate
comparisons can be made to the weight bearing
modified lunge test (38,2) (Menz et al., 2003). Foot
eversion (18.1±3.2°) is within ROM reference
values and similar to the test found to elicit
maximum ankle eversion in the SEBT (16.41.9°)
(Doherty et al., 2015). Inversion (7.8±4.4°) is not
within range of ROM reference values, however,
similar to what has been found for SEBT (7.11.9)
(Kang et al., 2015). To the authors’ knowledge no
goniometric ROM for abduction and adduction exist,
however the joint movements obtained is similar to
stance phase of running (Freedman et al., 2015).
Maximum knee flexion (94.3±22.4) is below
ROM reference values, but greater than in the SEBT
(66.3°-68.9°) (Doherty et al., 2015; Kang et al.,
2015). Knee internal rotation is within the range
while external rotation is greater, (7.8°-26.6°) and
(5.3±14.7°) respectively, when compared to SEBT
(Doherty et al., 2015; Kang et al., 2015). The frontal
plane arch (23°) obtained in this study is greater than
the ROM reference values (Table 1), but similar to a
functional task such as a jump-stop unanticipated cut
(27) (Ford et al., 2005)
HSEBT is eliciting more hip flexion than the
SEBT (72.0°-77.0°) (Doherty et al., 2015; Kang et
al., 2015). Hip extension is greater than ROM
reference values, but closer to what have been
observed in activities thought to require hip
extension such as sprint running (22°) (Kivi et al.,
2002) and football kick (25°) (Smith and Gilleard,
2015). In comparison, SEBT does not challenge hip
extension. Both hip internal and external rotation are
at the lower end of ROM reference values. The
rotational values are greater than the internal (4.3°-
8.0°) and external rotation (5.2°-23.5°) values
reported for the SEBT (Doherty et al., 2015; Kang et
al., 2015; Robinson and Gribble, 2008). Hip
adduction is within ROM reference values and
greater than what has been found with the SEBT
(15) (Doherty et al., 2015). Hip abduction is less
than ROM reference values, but similar to SEBT
(15) (Robinson and Gribble, 2008).
Spine movements elicited by the HSEBT are
representative of both lumbar and thoracic spine
movement. The HSEBT is able to elicit flexion and
lateral flexion within, and extension, and rotation
just outside range of ROM reference values (Magee,
2006). SEBT do not elicit spine movements within
ROM reference values. However, selected
movements do predict reach distance (Kang et al.,
2015), which might indicate their importance in
balance and postural adjustments.
HSEBT elicits unique combinations of
movements in ankle joint complex, knee, hip and
spine. Observed joint movements, nine of twenty-
two possible, were within the ranges of goniometric
ROM reference values, while two (ankle
dorsiflexion and hip extension) where greater. In
comparison to the SEBT, the HSEBT elicits similar
or lower values for the ankle, but greater values for
the knee, hip and spine. In addition, hip extension
and spine movements are elicited by the HSEBT and
not SEBT. HSEBT offers a new and promising
approach to functional mobility testing that
integrates the full kinematic chain.
REFERENCES
Almquist, P. O., Arnbjornsson, A., Zatterstrom, R., Ryd,
L., Ekdahl, C., & Friden, T. (2002). Evaluation of an
external device measuring knee joint rotation: an in
vivo study with simultaneous Roentgen stereometric
analysis. Journal of orthopaedic research : official
publication of the Orthopaedic Research Society,
20(3), 427-432. doi:10.1016/S0736-0266(01)00148-6
Boone, D. C., & Azen, S. P. (1979). Normal range of
motion of joints in male subjects. J.Bone Joint
Surg.Am., 61(5), 756-759. Retrieved from PM:457719
Craib, M. W., Mitchell, V. A., Fields, K. B., Cooper, T.
R., Hopewell, R., & Morgan, D. W. (1996). The
association between flexibility and running economy
in sub-elite male distance runners. Med.Sci.Sports
Exerc., 28(6), 737-743. Retrieved from PM:8784761
Delahunt, E., Chawke, M., Kelleher, J., Murphy, K.,
Prendiville, A., Sweeny, L., & Patterson, M. (2013).
Lower limb kinematics and dynamic postural stability
in anterior cruciate ligament-reconstructed female
athletes. Journal of athletic training, 48(2), 172-185.
doi:10.4085/1062-6050-48.2.05
Doherty, C., Bleakley, C. M., Hertel, J., Caulfield, B.,
Ryan, J., & Delahunt, E. (2015). Laboratory Measures
of Postural Control During the Star Excursion Balance
Test After Acute First-Time Lateral Ankle Sprain.
Journal of athletic training, 50(6), 651-664.
doi:10.4085/1062-6050-50.1.09
Ford, K. R., Myer, G. D., Toms, H. E., & Hewett, T. E.
(2005). Gender differences in the kinematics of
unanticipated cutting in young athletes. Med Sci
Sports Exerc, 37(1), 124-129. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/15632678
Freedman Silvernail, J., Boyer, K., Rohr, E., Bruggemann,
G. P., & Hamill, J. (2015). Running Mechanics and
Variability with Aging. Med Sci Sports Exerc.
doi:10.1249/MSS.0000000000000633
Greene, W., & Heckman, J. D. (1994). The clinical
measurement of joint motion. Rosemont, IL: American
Academy of Orthopedic Surgeons.
Gribble, P. A., Hertel, J., & Plisky, P. (2012). Using the
Star Excursion Balance Test to assess dynamic
postural-control deficits and outcomes in lower
extremity injury: a literature and systematic review.
Journal of athletic training, 47(3), 339-357.
doi:10.4085/1062-6050-47.3.08
Hubbard, T. J., Kramer, L. C., Denegar, C. R., & Hertel, J.
(2007). Contributing factors to chronic ankle
instability. Foot Ankle Int, 28(3), 343-354.
doi:10.3113/FAI.2007.0343
Kang, M. H., Kim, G. M., Kwon, O. Y., Weon, J. H., Oh,
J. S., & An, D. H. (2015). Relationship Between the
Kinematics of the Trunk and Lower Extremity and
Performance on the Y-Balance Test. PM & R : the
journal of injury, function, and rehabilitation.
doi:10.1016/j.pmrj.2015.05.004
Kivi, D. M., Maraj, B. K., & Gervais, P. (2002). A
kinematic analysis of high-speed treadmill sprinting
over a range of velocities. Med Sci Sports Exerc,
34(4), 662-666. Retrieved from http://
www.ncbi.nlm.nih.gov/pubmed/11932576
Levangie, P. K., & Norkin, C. C. (2011). Joint Structure
and function a comprehensive analysis, 5th Ed.
Philadelphia, PA: F. A. Davis Company.
Lindsjo, U., Danckwardt-Lilliestrom, G., & Sahlstedt, B.
(1985). Measurement of the motion range in the
loaded ankle. Clinical orthopaedics and related
research
(199), 68-71. Retrieved from http://
www.ncbi.nlm.nih.gov/pubmed/4042498
Macedo, L. G., & Magee, D. J. (2009). Effects of age on
passive range of motion of selected peripheral joints in
healthy adult females. Physiother Theory Pract, 25(2),
145-164. doi:10.1080/09593980802686870
Magee, D. J. (2006). Orthopedic physical assessment, 4th
Ed: Saunder, Philadelphia, PA. (Reprinted from: NOT
IN FILE).
Menz, H. B., Morris, M. E., & Lord, S. R. (2006). Foot
and ankle risk factors for falls in older people: a
prospective study. J Gerontol A Biol Sci Med Sci,
61(8), 866-870. Retrieved from http://
www.ncbi.nlm.nih.gov/pubmed/16912106
Menz, H. B., Tiedemann, A., Kwan, M. M., Latt, M. D.,
Sherrington, C., & Lord, S. R. (2003). Reliability of
clinical tests of foot and ankle characteristics in older
people. J Am Podiatr Med Assoc, 93(5), 380-387.
Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/13130085
Moreside, J. M., & McGill, S. M. (2011). Quantifying
normal 3D hip ROM in healthy young adult males
with clinical and laboratory tools: hip mobility
restrictions appear to be plane-specific. Clinical
biomechanics, 26(8), 824-829.
doi:10.1016/j.clinbiomech.2011.03.015
Mudge, A. J., Bau, K. V., Purcell, L. N., Wu, J. C., Axt,
M., J., Selber, P., & Burns, J. (2013). Normative
reference values of lower limb joint range, bone
torsion, and alignment in children aged 4-16 years. J
Pediatr Orthop, 23, 15-25.
Roaas, A., & Andersson, G. B. (1982). Normal range of
motion of the hip, knee and ankle joints in male
subjects, 30-40 years of age. Acta Orthop Scand,
53(2), 205-208. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/7136564
Roach, K. E., & Miles, T. P. (1991). Normal hip and knee
active range of motion: the relationship to age.
Phys.Ther., 71(9), 656-665. Retrieved from
PM:1881956
Robinson, R., & Gribble, P. (2008). Kinematic predictors
of performance on the Star Excursion Balance Test.
Journal of sport rehabilitation, 17(4), 347-357.
Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/19160909
Sankar, W. N., Laird, C. T., & Baldwin, K. D. (2012). Hip
range of motion in children: what is the norm? J
Pediatr Orthop, 32(4), 399-405.
doi:10.1097/BPO.0b013e3182519683
Schwarz, N. A., Kovaleski, J. E., Heitman, R. J.,
Gurchiek, L. R., & Gubler-Hanna, C. (2011).
Arthrometric measurement of ankle-complex motion:
normative values. Journal of athletic training, 46(2),
126-132. doi:10.4085/1062-6050-46.2.126
Smith, T., & Gilleard, W. (2015). Three-dimensional
analysis of a lofted instep kick by male and female
footballers. Eur J Sport Sci, 1-8.
doi:10.1080/17461391.2014.992477
