
Design of a Mobile Application for Eye Signs Screening
A. R. Silva
1
, P. Gomes
2
, D. Pereira
3
, S. Guimar˜aes
4
and A. Castro
5
1
Instituto Superior de Engenharia do Porto, Porto, Portugal
2
Instituto de Telecomunicac¸˜oes, Universidade do Porto, Porto, Portugal
3
Faculdade de Medicina da Universidade do Porto and Instituto de Telecomunicac¸˜oes, Porto, Portugal
4
Hospital de Braga, Braga, Portugal
5
Faculdade de Engenharia da Universidade do Porto, Porto, Portugal
Keywords:
Eye Pathologies, Mobile Application, Protocol, Red Reflex.
Abstract:
Advances in technology make mobile phones very attractive to everyone, specially smartphones, with a large
number of applications. In this paper we describe the necessary features of a mobile application for eye
signs screening, describing some of the ocular pathologies that can be detected with a photograph using a
smartphone, and the data collection protocol necessary to obtain this data and later process it. A first version
of the developed application and some results are also presented. This application is simple to use, since the
main target are the parents, who can use it at home as a tool to trace the visual health of their children, given
that an ophthalmologist follow-up is scarce or nonexistent in many places.
1 INTRODUCTION
Currently, the use of mobile applications has expe-
rienced a substantial growth, becoming part of day-
to-day life of many people. With the increasing use
of smartphones several applications in different ar-
eas are being developed, including the medical field
(J. Chhablani, 2012), (Bethke, 2010). This can make
the difference achieving an early diagnosis and, con-
sequently, a higher probability that the disease does
not progress to an advanced stage, also in remote
places, or with lack of experts (Gallagher, 2013), (To-
day, 2011). Ophthalmic and optometric organizations
recommend a visit to an eye care professional every 1-
2 years to have a comprehensiveeye exam (Vela et al.,
2012). In this paper we propose to develop a mobile
application for certain ocular pathologies detection
with adequate image collection protocol. The ”Red
Reflex Test” (RRT), also named ”Br¨uckner Test’, was
considered as an effective form of blindness preven-
tion and early diagnosis of serious diseases such as
retinoblastoma, Coats’ disease, anisometropia or stra-
bismus (P.J. Magalhes, 2009), (AAOP et al., 2008),
(Amitava et al., 2010).
The motivation for this work arose from several news
around the world about parents who post photos of
their children on social networks, with some friends
noticing that something may be wrong with their vi-
sion (Mail, 2007), (Tvi24, 2014), (Stampler, 2014),
(JornalNot´ıcias, 2014), (Anne, 2013). A correct diag-
nosis was made when parents went to an ophthalmol-
ogist, who actually detected an eye problem/disease,
what led us to the development of an application,
which will be presented next.
2 EYE PATHOLOGIES AND
OPHTHAMOLOGIC TESTS
In order to design a tool for eye signs screening in a
smartphone, it is important to understand the differ-
ent clinical tests and eye pathologies, since we need
to clarify the technological needs, and define an ad-
equate data collection protocol. After reviewing this
information, a clinical test feasible for the application
in a smartphone was designed. The test and corre-
sponding most common pathologies will be presented
in the following sections. This application is meant to
be used in detecting common eye pathologies of chil-
dren, and therefore the data collection protocol must
be simple to be practical in this context.
519
R. Silva A., Gomes P., Pereira D., Guimarães S. and Castro A..
Design of a Mobile Application for Eye Signs Screening.
DOI: 10.5220/0005256405190524
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 519-524
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

2.1 Eye Pathologies
A brief overview of the pathologies detectable using
the camera of a smartphone will be given in this sec-
tion. The features that may be useful in the detection
of these pathologies will also be described.
2.1.1 Retinoblastoma
Retinoblastoma is a tumor that originates from im-
mature retinoblasts in the neural retina and it is the
most frequent intraocular tumor in children, being re-
sponsible for 11% of cancer cases in the first year of
life. The most common signs of retinoblastoma are:
leukocoria, strabismus and inflammatory signs (Ra-
masubramanian and Shields, 2012). Leukocoria is
an abnormal (white) reflex when a direct light source
reaches the eye. Because retina is highly vascular-
ized and has red-orange color the light reflected to-
ward the eye must have a reddish appearance, but in
this disease there is a change in some internal struc-
ture of the eyeball so this reflex is absent, and there
is usually a whitish reflection. An algorithm may be
envisioned to detect the white spot in the eye of the
children, by taking a series of photos. The specialists
recommend parents to take photos once a month, in
a room with soft light and without red-eye reduction,
to check for a normal red-eye reflex in children under
six years of age (Fund, 2010). Coats’ disease, as well
as leukocoria, may be detected in photographs taken
with flash, but in this case the eye presents a yellowish
color (J. Liebmann-Smith, 2010).
2.1.2 Amblyopia
Amblyopia is another visual impairment that may be
detected with the RRT or Br¨uckner test, which is very
helpful to detect amblyogenic disorders (Gr¨af, 2010).
This disease is normally called ”lazy eye” because
the major symptom is a decrease in visual acuity in
a normal eye (Miller et al., 1995). Causes of ambly-
opia, which is a major cause of vision loss in chil-
dren and even adults, include strabismus, refractive
errors and ocular misalignment (Miller et al., 1995),
(Alhammouri et al., 2011), that is why it is very im-
portant to detect amblyogenic factors as early as pos-
sible. Like strabismus, amblyopia may be detected
in a photo with flash light, if there is a change in red
reflex symmetry.
2.1.3 Strabismus
Strabismus is an ocular misalignment (TheRoyalCol-
legeofOphthalmologists, 2012), where one eye is ei-
ther constantly or intermittently not directed towards
the same point as the other eye when the patient at-
tempts to fixate an object. It usually develops during
childhood but can occur at any age. Most cases be-
gin before 6 years of age, being the peak age of onset
around 3 years (Rutstein et al., 2011). The exams that
are made by an ophthalmologist usually include the
”Hirschberg test”, the ”Cross-over”, and the ”Cover-
uncover” test, which reveal latent strabismus (Angart,
2014). The Hirschberg test may be used to determine
the type and degree of strabismus using a small pen-
light and directing it toward the eyes. When the pa-
tient is looking at the light, a reflection can be seen
on the front surface of the pupil. The reflected point
of light will reveal the type and degree of strabismus
(Medical, 2011). The cover-uncover test may reveal
latent strabismus, ”heterophoria”. A cover (occluder)
is placed briefly before the eye that appears to fixate
while the patient looks at a small object (E.C. Cam-
pos, 2002). Finally, the Cross-over test may reveal
latent as well as manifest strabismus. As the name
suggests in this test, an occluder is transferred from
one eye to the other without interval (E.C. Campos,
2002). This brings the idea to develop features in the
application that can be helpful in the diagnosis of stra-
bismus. Such as the other disorders referred before,
the application will take a photograph with flash, and
then, with an algorithm automatically process the im-
age to detect and evaluate the local of the reflex in the
pupil, like in the Hirschberg test. After the tests are
done, an algorithm may read and calculate the devia-
tion of the eye relatively to the center of the image.
2.2 Red Reflex Test
The RRT is a screening exam for detecting ocular
abnormalities using an ophthalmoscope, that emits
light with the appropriate intensity over the pupil of
the newborn, even without the use of previous drops
(P.J. Magalhes, 2009). This test is performed to eva-
lute the eye condition, helping in the diagnosis of the
described pathologies, because the reflection of the
incident light produces a reddish and continuous color
on healthy eyes, meaning that the main internal struc-
tures of the eye (cornea, iris, pupil, lens and retina)
are transparent, allowing the light normally to reach
the retina. In the presence of an abnormality that
obstructs the arrival of light to the retina and its re-
flection, the light reflex undergoes changes that inter-
fere with their coloration, homogeneity and binocu-
lar symmetry (Aguiar et al., 2007). The test should
be done early in a child’s development, given that
it is when the vision progresses, and if the diagno-
sis is reached later, the likelihood of full recovery is
smaller. This test is very important, because how it
HEALTHINF2015-InternationalConferenceonHealthInformatics
520
was seen, allows the detection of a huge part of dis-
eases with high incidence in childhood. Thus, this test
was chosen to be reproduced in our application.
3 PROTOCOL DESIGNED FOR
DATA COLLECTION
After reviewing the most common pathologies and the
clinical tests, determining which clinical signs may
be detected using technology available in a smart-
phone, a protocol for data collection needs to be de-
fined within the application. The protocol is a guide-
line which encompass all the steps that are made by
the user, when handling with the mobile application
for data collection. For the development of this proto-
col we had to take into account the light environment,
which must be low in order not to allow the pupil to
close; the positioning of the person from the subject
to not obfuscate their vision; and all the necessary in-
formation shown in the screen, so the person fulfill
the minimum requirements for the photographs to be-
come perceptibles. The material necessary to do it is a
mobile phone with the application installed. The data
collection protocol was designed as follows:
1. Create a soft light environment: turning the lights
down and ensuring that any light sources - such as
table lamps or television - are behind the person
(so they dont reflect in the eyes).
2. Position yourself about 3 meters from the
child/person and use the zoom to capture the sub-
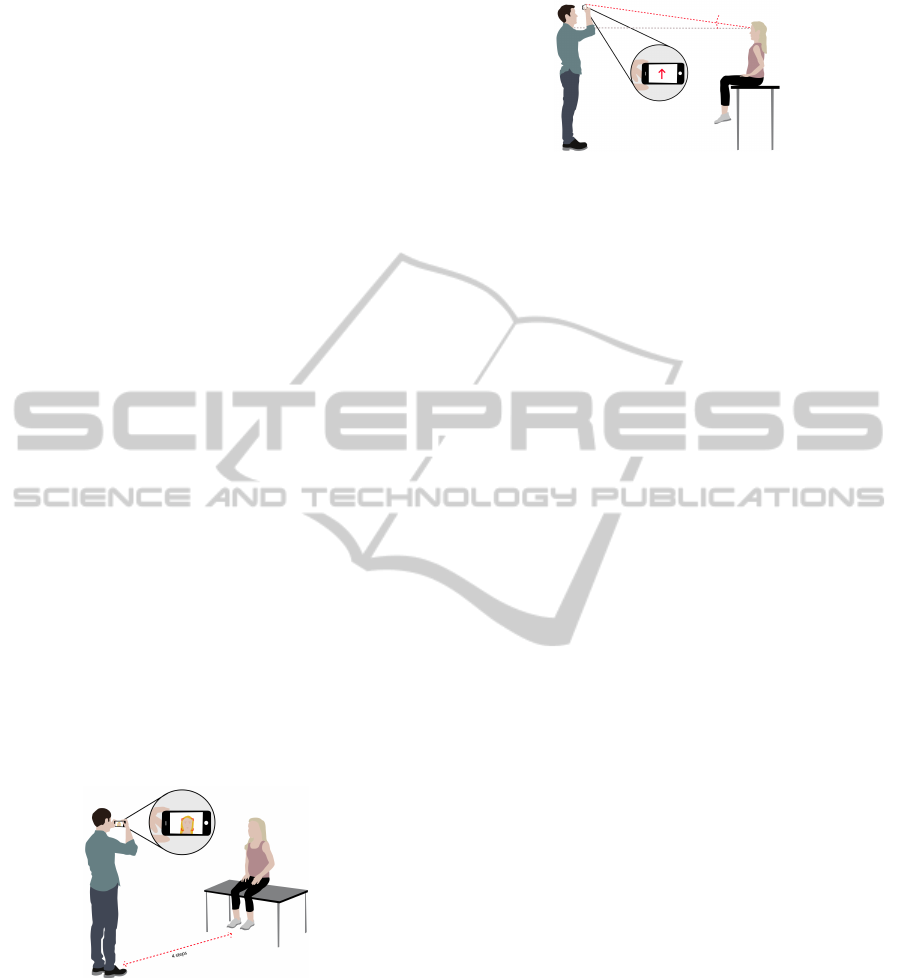
ject’s entire head (Figure 1).
Figure 1: Sketch ilustrating the positioning of the person.
3. Press the button when ready to initiate the collec-
tion.
(a) The head, eyes and pupil will be detected on the
screen.
4. When all is properly aligned the first of 5 photos
will be taken automatically.
5. Follow the arrows to tilt your phone to where they
indicate: 1st upwards (Figure 2).
Figure 2: Drawing exemplifying the indications on the
phone.
(a) Repeat step 5 to down, left and right.
6. A menu will show up asking to send the data col-
lected now or later.
(a) Now: link your mobile phone to the internet (to
your computer by wifi).
(b) Later: When you want, enter in ”Records” - se-
lect the folder with the collection you want to
send to analysis in a central server.
This protocol was included in the mobile applica-
tion developed by us, which will be described in more
detail in the section below.
4 DESIGN OF THE MOBILE
APLLICATION
The information previously referred was used to de-
sign an application for eye signs screening. It was
established that the user of the mobile application is
going to be a non medical person who wants to col-
lect data and receive a report on the eye health status,
preferably from a child. When opening the applica-
tion one disclaimer will appear, and the user may only
can continue after agreeing with the conditions: the
application does not replace a regularly ophthalmolo-
gist appointment. The reports act only as an alarm in
case of some abnormality detection, for further eval-
uation from a clinician, nonetheless it does not sub-
stitute a regular visit to the ophtalmologist. Then the
user will have three options: one for ”Collect”, other
for ”Alert”, and one for ”Records”. But, as in Fig-
ure 3, all will be disabled because the user has to reg-
ister a person in the application to start using it.
In a dropbox he can click on ”New”, and then will
be forwarded to a new window. In this window (Fig-
ure 4) the user can write the name and the age of the
child who he/she wants to screen and upload a photo
for ID.
After he/she saves it, the application returns to
the initial menu and the button ”Collect” will be now
available, to initiate the collection with the respective
person/child registered. After the first data collection
DesignofaMobileApplicationforEyeSignsScreening
521
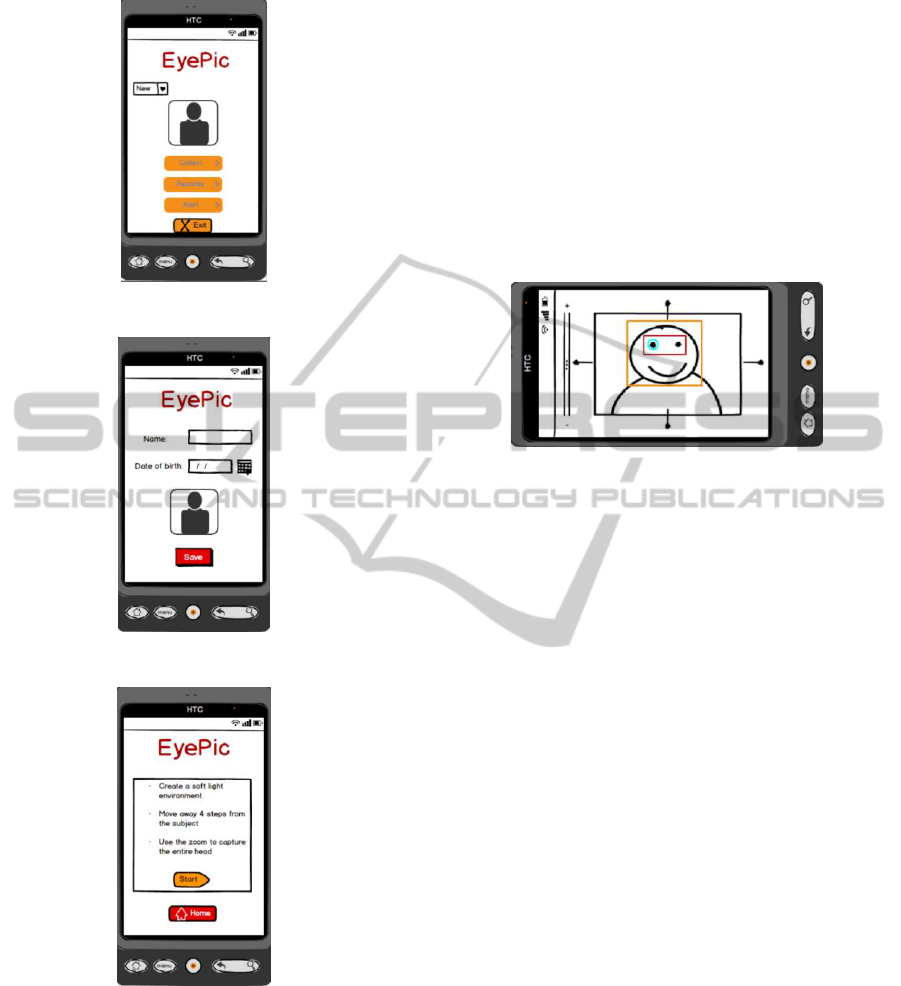
Figure 3: Mockup of the start menu.
Figure 4: Mockup of the user registration.
Figure 5: Mockup illustrating the pop-up guide to the user.
made, the user may have access to the remaining but-
tons. For the option ”Collect” some instructions to
this feature will pop-up to guide the user through data
collection: to turn the lights down, to step away 4
steps from the person who he wants to trace (which
will be in front of him/camera), and to use the zoom
to capture the entire head (Figure 5). This way the
user can apply the defined protocol and obtain useful
data for processing/screening.
When the user finishes reading the instructions
he/she can click the button to start collection. The
camera will initiate, and the algorithm for face recog-
nition will pop-up. When the detection of the eyes
and pupil is reached, the phone shoots the first of 5
photos with flash. Afterwards, arrows will appear on
the screen, indicating where to tilt the camera, and the
process of detection of the face, eyes and pupil will
repeat for right, left, up and down. When everything
is in the right position, the photo is taken automati-
cally, without requiring the user to press the ”shutter”
button, like in 6.
Figure 6: Mockup exemplifying one procedure of the trac-
ing method.
At the end, the user is prompted to choosebetween
sending the collection now or later to the server. If
he chooses now, this data will be sent to the server.
Choosing to send it later, he returns to the start menu
and may send it later in the ”Records” feature. In
option ”Alert” of the front menu, the user will have
indications to set an alarm of thirty days between col-
lections. After this, the calendar of his phone will
appear, where he can see other events that have been
scheduled. Clicking on the desired day, and setting
the time will set the alarm. Then, on the selected date,
he will receive a notification to remind him of the col-
lection. Nonetheless the application is available for
data collection whenever the user decides to use it,
regardless of the alarm set. Finally, when the user
clicks on the button ”Records” (History), the applica-
tion will redirect him to the gallery where he can see
the different folders of previous data collection ses-
sions. In each screening, one folder will be created to
store all the information collected and corresponding
reports. When the user opens the selected folder, he
will have access to the photos recorded, getting 3 dif-
ferent options: ”Properties”, ”Delete” or ”Send”. In
”Properties” the non medical user can see the name,
date and hour of the photo, and also the age of the per-
son/child, in months, at the time of the collection. In
”Delete” he can erase it, and, in the ”Send” option he
can send the chosen session to the server, if it has not
been done before or if he wants to repeat it, receiving
a new report.
HEALTHINF2015-InternationalConferenceonHealthInformatics
522
4.1 Test Beds
The camera of the mobile phone needs to be con-
trolled in such a way that face, eyes, and pupils are au-
tomatically detected, and then the necessary controls
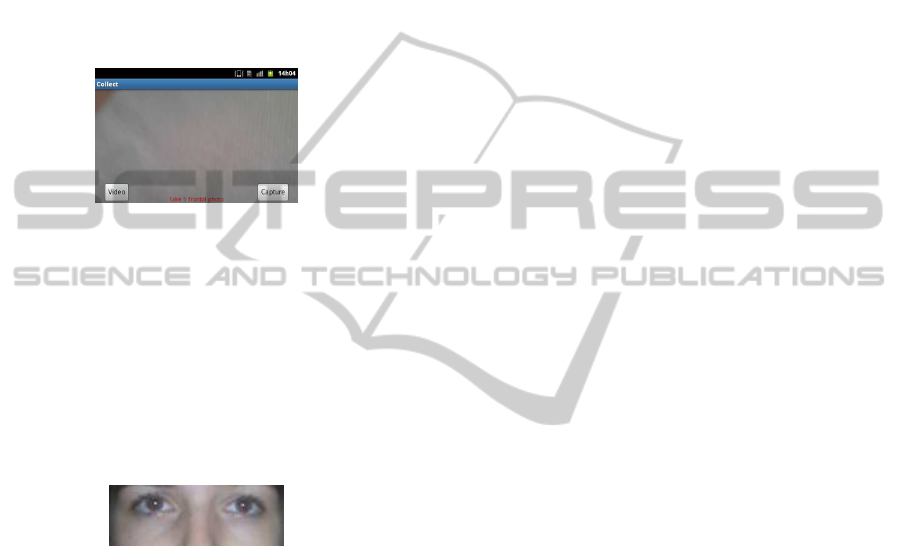
and instructions for the user are presented. Figure 7
is referent to the final aspect of the camera preview.
Implementation of different sensors, like accelerom-
eter, to detect motion when the user needs to follow
the instructions, and light sensor to measure the il-
lumination of the room, would be very useful in the
application.
Figure 7: Camera’s preview of the mobile application.
The developed mobile application (”EyePic”) was
then tested following the required protocol and with-
out the use of any external hardware. Figure 8 shows
the result of the application with the proposed proto-
col and the white reflex necessary to evaluate the de-
gree of strabismus (”Hirschberg test”). The dual flash
of the mobile phone leads pupil closure, not allow-
ing the presence of a red reflex, being this an issue to
evaluate in further tests.
Figure 8: Binocular photograph taken with ”EyePic” mo-
bile application.
This application was shown to some profession-
als of the area who express their opinion about the
designed protocol, respective mobile application and
early results. They agree that this kind of mobile ap-
plication is very useful for variousreasons, mainly be-
cause it is low-cost, but also because most parents are
not informed or do not even have knowledge on the
subject, the majority thinks they can not take a baby
to an appointment, that he will not cooperate. So, be-
cause nowadays everybody adhere to mobile applica-
tions quite well, this new one, easy to access, allow-
ing to perform a data collection at home and trans-
mitting important information, becomes very usefull
for an early ophthalmologist appointment. This is an
important tool to battle with a delayed diagnosis, hav-
ing, consequently, huge impact in the medical field.
In fact, Br¨uckner test plays an important role in de-
tection of these eye pathologies, that must be detected
as soon as possible.The main concern is the quality of
the camera phone, which may not have the required
conditions for a complete assessment of lunar reflec-
tions like in the Br¨uckner test.
Relatively to the defined protocol, the lighting in
the room should be low (as we noted when starting
the data collection) in order to allow scotopic vision
(vision produced by the eye in low light conditions)
and frontal photos will be the ideal, since taken from
another perspective may mislead.
A ”beta” version of this application will be tested
at Hospital de Braga in a screening project named
”Pimpolho”, aiming to make an evaluation of the eye
health of children aged 3 to 4 years, with special focus
on amblyopia or some amblyogenic risk factors.
5 DISCUSSION AND
CONCLUSIONS
In this paper, we propose the framework for eye
pathology screening using a mobile application, with
special emphasis in children and fast degrading eye
pathologies. The most common diseases that ben-
efit from early detection, and respective signs were
described. This allowed for the design of a novel
data collection protocol for a range of eye pathology
screening, specially designed for non-medical users,
and with only the technology available on a smart-
phone: camera and flash. In this application there is
no need for external devices. Besides the features pre-
sented before, in the future we intend to make avail-
able a video recording what could add more value to
the application, covering more eye pathologies, like
nystagmus or other evaluation for strabismus (Train-
ing, 2014). But there are some important issues to be
considered like the child’s attention during the record-
ing, and the accuracy required to implement it.
Given the importance of the eye diseases covered
in this work, early detection is essential to a timely
and effective treatment, making this mobile applica-
tion quite advantageous, due to its practical and easy
to use aspects for a regular monitoring, something
extremely important for this diseases with high inci-
dence during childhood.
In conclusion we can say that one of the strengths
of this application is its accessibility: it can reage ev-
eryone, since low income countries where medical in-
struments are scarce (this can become an alternative);
and mainly because allows a first screening, collect-
ing usefull images to the detection of serious diseases.
Its great advantage is the ability to store all collec-
tions made by date (records / history), and thus can be
viewed by a medical expert. As parents with young
DesignofaMobileApplicationforEyeSignsScreening
523

children usually attend a pediatrician, and he only per-
forms any non routine eye exam in case of alarm, it
will be a great asset to have a visual history of the
development of eye disease (if that manifest) for an
accurate diagnosis. Also, a image repository can be
achievedwith this collection, not only for doctor eval-
uation, but for science research as well.
Besides all of that this is a very innovative mo-
bile application, there are no currently similar appli-
cations, to our knowledge, including the same fea-
tures an without the use of additional hardware to ob-
tain the imagens for the analysis (Gallagher, 2013).
ACKNOWLEDGEMENTS
The authors would like to acknowledge B´arbara Mota
(Faculty of Fine Arts of the University of Porto) and
the Ophthalmology Service of the Hospital de Braga.
This work was partially funded by Project I-CITY
- ICT for Future Health/Faculdade de Engenharia
da Universidade do Porto, NORTE-07-0124-FEDER-
000068, funded by the Fundo Europeu de Desen-
volvimento Regional (FEDER) through the Programa
Operacional do Norte (ON2) and by national funds
through FCT/MEC (PIDDAC).
REFERENCES
AAOP et al. (2008). Section on ophthalmology; american
association for pediatric ophthalmology and strabis-
mus, et al. red reflex examination in neonates, infants,
and children. Pediatrics, 122:1401–4.
Aguiar, A. S. C., Cardoso, M. V. L. M. L., and L´ucio, I.
M. L. (2007). Teste do reflexo vermelho: forma de
prevenc¸˜ao `a cegueira na infˆancia. Revista Brasileira
de Enfermagem, 60(5):541–545.
Alhammouri, Q., Gr¨af, M., and Lorenz, B. (2011).
Br¨uckner test sensitivity to detect foveal dimming.
JRMS, 18(3):10–15.
Amitava, A. K., Kewlani, D., Khan, Z., and Raz-
zak, A. (2010). Assessment of a modification
of br¨uckner’s test as a screening modality for ani-
sometropia and strabismus. Oman journal of ophthal-
mology, 3(3):131.
Angart, L. (2014). Strabismus test. Vision Testing.
Anne (2013). How a photo can save a childs life.
Bethke, W. (2010). Review of ophthalmology. vision test-
ing? there’s an app for that.
E.C. Campos, G. V. N. (2002). Binocular Vision and Ocu-
lar Motility: Theory and Management of Strabismus,
volume 2, chapter 12 - Examination of the Patient - II:
Motor Signs in Heterophoria and Heterotropia, pages
174–176. Mosby, 6 edition.
Fund, D. E. C. (2010). Life and sight for every child. Daisys
Eye Cancer Fund - PhotoRED Technique.
Gallagher, J. (2013). Optician’s clinic that fits a pocket -
peek. BBC News Health.
Gr¨af, M. (2010). The br¨uckner test revisited. In Pedi-
atric Ophthalmology, Neuro-Ophthalmology, Genet-
ics, pages 113–124. Springer.
J. Chhablani, S.Kaja, V. A. S. (2012). Smartphones
in ophthalmology. Smartphones in ophthalmology,
60(2):127–131.
J. Liebmann-Smith, E. J. (2010). Baby photos can reflect
serious eye disorders. Huffpost Healthy Living.
JornalNot´ıcias (2014). Menina salva de ficar cega grac¸as a
uma foto no facebook.
Mail, D. (2007). The ’strange white light’ that nearly killed
baby grace.
Medical, N. (2011). Strabismus diagnosis.
Miller, J. M., Hall, H. L., Greivenkamp, J. E., and Guyton,
D. L. (1995). Quantification of the br¨uckner test for
strabismus. Investigative ophthalmology & visual sci-
ence, 36(5):897–905.
P.J. Magalhes, I. M. V. (2009). Divulgac¸˜ao e treinamento
do teste do reflexo vermelho em rec´em-nascidos como
estrat´egia pol´ıtica em defesa da sa´ude ocular infan-
til no cear´a. Minist´erio da Sa´ude - Departamento de
Ciencia e Tecnologia.
Ramasubramanian, A. and Shields, C. L. (2012).
Retinoblastoma. JP Medical Ltd.
Rutstein, R. P., Cogen, M. S., Cotter, S. A., Daum, O.
K. M., Amos, J. F., Barry Barresi, O., Beebe, K. L.,
and Cavallerano, O. J. (2011). Optometric clinical
practice guideline care of the patient with strabismus:
Esotropia and exotropia. Lindbergh Blvd. St. Louis:
American Optometric Association.
Stampler, L. (2014). How posting a facebook picture saved
a 3 year olds sight.
TheRoyalCollegeofOphthalmologists (2012). Guidelines
for the management of strabismus in childhood. Tech-
nical report, The Royal College of Ophthalmologists -
Scientific Department.
Today, M. N. (2011). Remote diagnosis via camera phones.
Medical Devices and Diagnostics.
Training, V. (2014). Test for strabismus. Cover and Cross
Over tests.
Tvi24 (2014). Facebook salva visao de menina de trˆes anos.
Vela, C., Samson, E., Zunzunegui, M. V., Haddad, S.,
Aubin, M.-J., and Freeman, E. E. (2012). Eye care
utilization by older adults in low, middle, and high in-
come countries. BMC ophthalmology, 12(1):5.
HEALTHINF2015-InternationalConferenceonHealthInformatics
524
