
Design of a Remote Treatment Monitoring and Seizure Warning
System Framework for Epilepsy Patients
C. L. Martínez-González
1
, J. Mendizabal Navarro
2
and N. I. Plascencia Álvarez
3
1
Programa de Posgrado en Ingeniería de Sistemas, Instituto Politécnico Nacional, Zacatenco, Av. IPN S/N,
Del. Gustavo A. Madero, México, D.F., México
2
Escuela Superior de Cómputo, Av. Juan de Dios Bátiz esq. Av. Miguel Othón de Mendizábal, Col. Lindavista.
Del. Gustavo A. Madero. México, D.F., México
3
Centro Médico Nacional 20 de Noviembre, Av. Felix Cuevas 540, Col. Del Valle,
Del. Benito Juarez, México D.F., México
Keywords: Remote Treatment Monitoring System, Epilepsy, Mobile Technology, Seizure Warning, Patient Location.
Abstract: Personal health care technologies in chronic diseases face the challenge to design holistic approaches where
health care involves not only the medical specialist for treatment and monitoring, but the patient and the
family. Epilepsy is a term used for a group of chronic disorders with diverse etiology characterized by
recurrent seizures, caused by an abnormal electrical activity in the brain. Treatment monitoring requires
continuous collaboration of the patient and the family to register manually a diary of activities, seizures,
seizures triggers and symptoms associated to medication in order to reach optimal therapy. Patients with
non-controlled seizures and their families have to deal with a restricted quality of life: the patient is exposed
to physical risks when seizures appear under any circumstance and place. In this paper a remote patient
treatment monitoring and warning system framework design based on mobile technology is proposed, with
multiple input, seizure detection with a smartphone accelerometer, automatic and manual seizure warning
and location of the patient through GPS and a social support network. This design approach is patient-and
family-centred, as they are the source of individual information in a particular environment, condition and
treatment response. It also represents a first proposal of a potential ubiquitous health care system through a
wearable device.
1 INTRODUCTION
A challenge in health care technology involves the
non-integrated approach of specialists records of
patients information, the large volume of data and
the difficulties with appropriate information retrieval
that have resulted in a lack of use of available
electronic health records (EHR) and personalized
health records (PHR) while adherence of patients to
these systems need to take to account motivation and
self-care (Wang & Huang, 2012). In the near future,
ubiquitous technology for health care will be a
common environment in everyday life with
monitoring and prevention purposes (Omary et al.,
2011), however, actual technology provides useful
and powerful frameworks to design integrative
systems where data volume and information
actualization should not be an important issue.
Patient-centred integrative systems based on
individual modules from different sources
(ubiquitous or not) with independent updating, still
have to be designed. When health has become the
following target in personal technology, even more
with Apple HealthKit potential, health and well-
being smartphone applications represent the 40% of
current development (Furht and Agarwal, 2013) with
a growing trend.
Several mobile applications are available to aid
different chronic diseases like diabetes, obesity,
heart diseases, bipolar disorder and epilepsy, for
instance. In epilepsy, functionalities like seizure and
symptoms diary; medical and emergency
information; record of medications; seizure tracking,
videotaping and even detection have been widely
used for treatment monitoring and diagnosis support
(Epilepsy Foundation; National Society for
Epilepsy; The National Centre for Young People
with Epilepsy, among others). These applications are
546
Martínez-González C., Mendizabal Navarro J. and Plascencia Álvarez N..
Design of a Remote Treatment Monitoring and Seizure Warning System Framework for Epilepsy Patients.
DOI: 10.5220/0005274405460552
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 546-552
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

not linked to an integrated system, do not solve the
main problems of the medical specialist, do not
update the patient’s record, cannot be used for
emergency situations and more important, not all of
them involve family intervention, therefore losing
important information and feedback.
In many chronic diseases, a holistic approach for
treatment is mandatory. The patient cannot be the
only source of data for monitoring, for inherent
reasons of the disease or insufficient information
acquired by this mean. A common way to face this
challenge is a combination of interventions as
mechanisms to enhance adherence of the patient’s
behavior on taking medication, modifying habits and
attending clinics, according to medical advice and
including family participation (McDonald et al.,
2002) or using a patient-centered approach. Yet this
kind of combined interventions do not make use of
an integrative technology support system.
Consequently, treatment monitoring of chronic
diseases requires models that consider the
participation of all the roles involved in the disease:
the patient as the focus, the medical specialist and
the family, e.g. in a real patient-and family-centered
approach.
The system framework that we propose for
epilepsy is intended to accomplish the three main
issues in m-health (Furht & Agarwal, 2013) i) access
from anywhere and anytime, ii) quality since is
designed as an integrated system and iii) value for
the target to provide health care in a efficient and
effective way. It is divided in three parts.
The first part is a mobile medical device
designed for the patient with a small personal health
system, with an informative module, medication
alerts, social network, automatic seizure detection
and manual or automatic seizure warning –that takes
advantage of the smartphone accelerometer– and
physical location of the patient with GPS data. The
second part is mobile medical app for the caregiver
use, which contains symptoms observation diary,
seizure warning, seizure recording, social network
and first aid emergency programmed calls. The third
part is the monitoring system by a web system for
the medical specialist use; it involves the patient
record (personal data, treatment and seizure
monitoring, seizure records, EEG data), seizure
warnings and emergency services contact. All of
these modules linked by a cloud-computing service.
Current mobile apps or systems are designed
only for the one final user, as independent medical
information systems, without integration of the
information from all the input sources; this is the
principal innovative scheme of the present work. It
takes into account all the stakeholders that must be
involved, is user-centered (UCD) in each module,
but patient-and family-centered as an integrative
system: the context must be defined on the particular
environment and condition of each patient, thus, the
profile and use is personalized, the benefit is
pretended for the patient, the family and the
specialist. Furthermore, an important consequence is
the potential use for data generated by the system,
for statistical research in epilepsy patients’ habits
and seizure occurrence. This model also represents a
first proposal to be part of a potential ubiquitous
health care system.
2 HEALTH CARE
REQUIREMENTS IN EPILEPSY
Epilepsy is a term used for a group of disorders with
diverse etiology (infections, birth problems, tumors,
trauma and in many cases, origin is unknown),
characterized by recurrent seizures, caused by an
abnormal electrical activity in the brain. In the
world, around 50 million people have epilepsy
(World Health Organization 2012). Any person,
without previous symptoms or circumstances, is
susceptible to epilepsy. Diagnosis is achieved in a
precise way by seizures description and different
medical studies as electromagnetic resonance,
tomography and particularly electroencephalograms.
The specialists for this diagnosis are a neurologist
and an epileptologist. The most known and shocking
kind of seizure is a generalized tonic-clonic, where
the patient loses consciousness and the entire body
convulsions.
Available treatment of a diagnosed patient
depends upon the classification of the epilepsy and
the seizures; it consists on stopping seizures by
medication with anti-epileptic drugs (AEDs),
securing appropriate habits, specific diet and in
determined cases, surgery is indicated, besides
alternative treatments. Treatment monitoring
requires continuous collaboration of the patient and
his family to register a diary of activities, seizures,
seizures triggers and associated symptoms to update
the specialist and analyse medication efficacy and
tolerability to reach the optimal therapy with the
exact combination of AEDs in certain doses.
In some patients, seizures are announced by a
certain perception called “aura”, a sensory signal
like visual, auditory, gustatory, olfactory
hallucination or the awareness that something is
wrong that indicates an imminent seizure. Then the
patient is able to warn someone or to avoid risks by
DesignofaRemoteTreatmentMonitoringandSeizureWarningSystemFrameworkforEpilepsyPatients
547

himself. The patients that do not perceive this aura
and are in a vulnerable physical location suffer the
risk of accidents, falls and injuries.
Speaking about quality of life, the first of its
possible indicators, defined by Cribb (1985) is the
quality of lifestyle, associated to the patient’s
capacities and restrictions in their work, social and
home life; the second possible indicator is mental
health, where emotional well-being in all levels
takes into account. Therefore, patients with non-
controlled epileptic seizures and their families have
to deal with a restricted quality of life due to the
inherent risks of the disease: the patient is exposed
to physical risks when seizures appear under any
circumstance at any place. Also, per se, epilepsy is
involved in underlying discrimination and stigma
(Forsgren et al., 2013) and still risks prevention in
uncontrolled seizures is limited to the self-exile,
affecting family, relatives or caregivers.
Records of seizures observation and medication
achieve actual treatment monitoring.
Accordingly, current technology can be
extraordinary to support some of the intrinsic
mechanisms of the disease with an appropriate
holistic design approach, a patient-and-family
centred design.
3 PATIENT-AND-FAMILY
CENTRED DESIGN
As a starting point for the design approach of this
system framework, the patient-centred design basis
was proposed —defined by Baecker as the design
with users or patients in a participatory design—
implicating the sense of person-centred care, as
McCormack et al. (2011) established: an approach
that involves care providers, patients, and others
significant to them; thenceforth converting our
overall design approach in a patient-and-family
centred design.
The Institute of Patient-and-Family-Centered
Care defines the core concepts in patient-and-family
centred care as 1) the dignity and respect of patient
and family perspectives and choices, 2) the
information sharing, 3) the participation and 4) the
collaboration of them in care and decision-making.
In ambulatory care specifically, the patient and the
family are conveyed to be integral part of the health
care team, while self-management of the chronic
condition is desirable, getting all them involved in
the planning, implementation and evaluation of
chronic care strategies (Johnson et al. 2008).
3.1 Design Considerations for Epilepsy
Usability and accessibility are the main features in
user-centred design, directly related with a integral
approach.
In this remote treatment monitoring and warning
system framework for epilepsy, a particular profile
of patient must be stated. The specific users of the
patient app are persons already diagnosed with
epilepsy to achieve treatment monitoring by
observing medication effects on seizures recurrence,
principally patients with uncontrolled seizures that
need to be supervised by a caregiver, commonly
someone in the family. Seizure detection
functionality is defined for tonic-clonic seizures;
thenceforth other kind of seizures may not be
detected.
A patient with uncontrolled epilepsy seizures
suffers of anxiety due to the unpredictability of the
seizures, he or she does not have normal activities
and the daily routine needs to contemplate the
possibility of falls or injuries.
It is comprehensible that the patient and the
family must be considered as the principal role for
the design, since the prevalence of use of the system
depends on the participation of both users.
The central topics concerning the whole system
are:
Personal Health Record. Patient is able to
upload personal information related to general
data, emergency contact data and health data:
medical history, allergies, actual diagnosis and
medication. The specialist can upload strategic
results of primary neurologic diagnostic
technics like magnetic resonance and
tomography and principal laboratory tests
results like blood test and urine test, if they are
able.
Treatment monitoring. Appropriate medication
adherence is required in a patient that suffers
epilepsy; monitoring effects and tolerability is
overriding (Campos and Kanner, 2004),
especially with a new anti-epileptic drug, a new
combination of them or a different dose. Side
effects of medication are important to watch.
This monitoring is proposed for the specialist
use.
Habits, mood and daily activities. Missing
medication, emotional stress, sleep deprivation,
fatigue, missing meals, fever and smoking are
the most common —but not all— triggering
factors of seizures. Identification and
recognition of individual seizure triggers and
may be beneficial for the treatment; registering
HEALTHINF2015-InternationalConferenceonHealthInformatics
548

daily habits, mood and specific activities will
help to identify the most common for each
patient (Balamurugana et al. 2013). Selection
of symptoms, moods and daily activities will
be available.
Seizure records. A daily registration of seizures
in a detailed form is useful to determine the
medication efficacy. Time, duration and
detailed description are information needed for
a correct monitoring. A video recording of the
seizure is very valuable, since a patient does
not always exhibit seizures during a medical
examination.
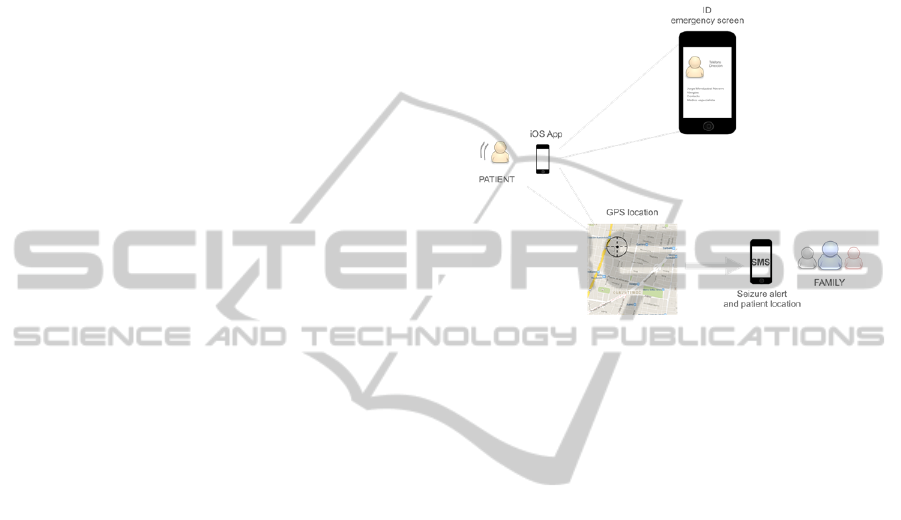
Seizure detection, seizure warnings and patient
location. Paroxysm will be detected by the
accelerometer of the smartphone running the
patient’s app, when seizure is detected, a
message will appear to confirm a false
detection. If this is discarded, an automatic
warning will be sent to the caregiver with the
physic location of the patient. If the patient has
an “aura”, he or she will be able to send a
manual warning of an imminent seizure. In
both cases, an urgency ID screen will be
displayed in the smartphone.
Support social network. A collaborative
network is a valuable element in this
framework. Epilepsy patients and families live
in a constant worry, anxiety and fear. This
network could be a platform to share
experiences and give emotional support.
3.1.1 Usability and Accessibility
In user-centred design (UCD), a specific iterative
cycle is outlined in ISO 9241-210 (Goldberg et al.,
2011), where the context of the system use is the
starting point –in this framework, for each module,
the patient, the caregiver or relative and the
specialist–, the requirements specification is the
following consideration, to produce, afterwards, the
design solutions and evaluate them to update the
design until usability is achieved. For the three user
profiles of this system, the cycle of UCD needs to be
completed.
Usability is considered from the design to the
final use of the system; each module must be
designed to be effective, efficient and satisfactory in
the specified context of use for each user profile
(ISO/IEC, 1998). Usability also has to take into
account training for the patient, the caregiver or
relative and the specialist of the whole system
framework in order to understand the main objective
and the particular goals for each profile.
Epilepsy is a chronic disease that may or not disable
the patient; in either way accessibility will delimit
the use of the mobile device by the patient. If the
patient is not able to operate the mobile device or
use the mobile app, he or she may not use all the
potential of the system, but the treatment monitoring
with the module of the caregiver can be a supporting
data source.
Like any other healthcare system, in epilepsy,
confidentiality of the information is a significant
subject, correspondingly to the trust of the patient on
the security of the data. Confidentiality must be
guaranteed as a primary expectation of the users,
principally, of the patient. Signed consent must be
considered for each patient and the caregiver
(family), focusing on confidentiality and use of the
data.
4 SYSTEM FRAMEWORK
M-Health or mobile health is the evolution of e-
health, with the use of mobile devices and wireless
network technologies for healthcare services
(Istepanian et al., 2006). The most common mobile
health systems are mobile health monitoring
systems, designed to store monitor patient status and
have been proposed for different purposes,
In the international standardization ISO/TC 215,
the proposed module for the caregiver is classified in
the category of Mobile Medical App, with the
intended use to support the treatment and monitoring
of the disease. The particular utilization of the
accelerometer as a sensor to detect seizures, gives
this patients module a function as a mobile medical
device (Kim & Song, 2013) with a Personal Health
Record (PHR).
Figure 1: System framework architecture.
DesignofaRemoteTreatmentMonitoringandSeizureWarningSystemFrameworkforEpilepsyPatients
549
The patient and the family modules of the system
can be also considered home use devices, since their
use is proposed for an environment outside a
professional healthcare facility (FDA, 2014).
Figure 1 shows the system framework
architecture, defined by three layers and two levels,
the first level is the backend and the second level,
the controller and interface.
4.1 Architecture
The first layer is data layer or backend, the second is
business layer or controller and the third is
presentation layer or interface. The level one is the
backend and the second level is formed by the other
two layers, business layer and interface.
In backend, patients and specialist data will be in
stored in a cloud database, allowing to be retrieved
from any business layer to be shown by the
interface.
For the controller, the patient and caregiver apps
were proposed to be developed for iOS and the
specialist module for web browser visualization.
Required data are obtained by requests to the data
layer.
Mobile apps need an intuitive interface,
according to the visual design of components from
Apple guides. Data obtained by the requests must be
correctly showed in this layer.
4.1.1 Specifications
For backend, web services were proposed on Ruby
programming language and the database system
manager, PosgreSQL. Cloud storage achieved by
Parse backend platform for iOS.
For the controller or business layer, the
programming language is SWIFT for iOS platform
for mobile apps and Ruby on Rails for web access.
As for the interface, for mobile apps, the native
of iOS was proposed and for web access interface,
JavaScript, CSS and HTML5.
4.1.2 Notifications, Warnings and Seizure
Detection
Push notifications are used to send seizures warnings
to the app for the relative or caregiver. The patient or
the caregiver must program drug administration
schedules in the specific app for each profile user.
To detect seizures, the accelerometer of the iOS
device (iPhone) is used. Continuous shaking is
considered as the paroxysm of a seizure, then a
warning message will appear on the screen to
discard a false alarm and in a positive case, seizure
detection warning will be send to the caregiver app.
GPS data will be attached to indicate the current
location of the patient.
Patient’s app will show an urgency ID screen
with emergency contact data and aid information
when a seizure is detected or manually warned
(Figure 2).
Figure 2: Seizure detection and alert with patient location.
4.2 Accuracy and Specificity
In-situ and in-depth trials must be planned and
achieved as a main part of the methodology of
development to determine reliability of the system.
The defined user’s profile of the patient and the
or caregiver or family modules is an epilepsy patient
with tonic-clonic seizures and a caregiver that is in
charge of the health care and support, the patient
could be a child, an adolescent or adult, as long as
the caregiver is engaged with the treatment
monitoring and updating of the data. A typical use of
the system depends on the participation of the
patient, the caregiver and the specialist.
4.3 Development Methodology
Rational Unified Process is a conventionally used
software engineering methodology. Roles, activities
and artefacts delineate it and use cases and iterative
processes are the main features. In the present work,
RUP was proposed implementing UCD through an
explicit role of usability designer, as Svanæs &
Gulliksen (2008) recommended. There have been
some experiences with this methodology for systems
development in industry without desirable success
(Vukelja et al., 2010) in the case of healthcare
information systems, the participation of particular
stakeholders in usability design is crucial and final
users must share this role in the development team.
HEALTHINF2015-InternationalConferenceonHealthInformatics
550

5 CONCLUSIONS
The system framework design presented here is a
hybrid approach to a remote treatment monitoring
with a module of a cloud Personal Health Record for
the patient and the family (both functioning as home
use medical devices) and a module of an Electronic
Health Record for the specialist, based on an
integrative holistic approach of patient-and-family
centred, that could be linked to other medical
systems.
The main use requirement for the patient and the
family is active participation; for the patient to carry
the mobile device, especially in environments out of
home, to fulfil information of habits and perceptions
and for the family or caregiver and to fulfil
observation data of the patient’ habits and seizures.
Information collected in this way gives the
patient the possibility to share his or her health
history when an emergency occurs.
This framework is intended to be an holistic
approach design, considering all roles involved in a
remote treatment monitoring, the design
methodology could be used to design for other
chronic diseases.
Patient’s module could serve as a basic approach
to a pervasive system as well, reminding the patient
to keep an appropriate lifestyle and determining real
criteria for detecting personal seizure triggers (lack
of sleep, certain food or activities, personal
conditions or sensibility and stress), when a large
amount data is collected and analysed to determine
personal tendencies that even offers an interesting
potential use of collected data for research purposes,
taking into account confidentiality and security of
the information.
After current development, the accelerometer of
the smartphone for seizure detection will be
substituted by a very sensitive sensor kit in a
wearable device to detect other kind of seizures with
minimum clinic symptoms like tremors and
temperature and cardiac rhythm changes.
ACKNOWLEDGEMENTS
Authors acknowledge the Instituto Politécnico
Nacional, CONACYT, COFAA and EDI for
financial support of this work.
REFERENCES
Baecker, J., A taxonomy of technology for cognition -
product and process, Available at: http://ron.taglab.
ca/papers/D60.pdf.
Balamurugana, E. et al., 2013. Perceived trigger factors of
seizures in persons with epilepsy. Seizure, vol. 22, no.
9, pp.743–747.
Campos, M.G. & Kanner, A.M. eds., 2004. Epilepsias.
Diagnóstico y tratamiento, Santiago de Chile:
Mediterráneo.
Cribb, A., 1985. Quality of life- a response to K. C.
Calman. Journal of Medical Ethics, vol. 11, pp.142–
145.
Epilepsy Foundation, My Epilepsy Diary.
FDA Federal Drug Administration, 2014. Design
Considerations for Devices Intended for Home Use.
Guidance for Industry and Food and Drug
Administration Staff, Available at: http://www.
fda.gov/downloads/MedicalDevices/DeviceRegulation
andGuidance/GuidanceDocuments/UCM331681.pdf.
Forsgren, L. et al., 2013. On the experience of stigma by
persons with epilepsy in Sweden and Iran—A
comparative study. Seizure, vol. 22, pp.748–751.
Furht, B. & Agarwal, A. eds., 2013. Handbook of Medical
and Healthcare Technologies, Springer New York.
Goldberg, L. et al., 2011. Usability and accessibility in
consumer health informatics current trends and future
challenges. American journal of preventive medicine,
vol. 40, no. 5 Suppl 2, pp.S187–97. Available at:
http://www.ncbi.nlm.nih.gov/pubmed/21521594
[Accessed July 11, 2014].
ISO/IEC, 1998. ISO/IEC. International standard 9241-
151: ergonomic requirements for offıce work with
visual display terminals (VDTs), Part 11: Guidance on
usability.,
Istepanian, R., Laxminarayan, S. & Pattichis, C.S., 2006.
Ubiquitous M-Health Systems and the Convergence
Towards 4G Mobile Technologies. In E. Mechelli-
Tzanakow, ed. M-Health: Emerging Mobile Health
Systems (Topics in Biomedical Engineering.
International Book Series). Springer, pp. 3–14.
Johnson, B. et al., 2008. Partnering with Patients and
Families to design a Patient- and Family-Centered
health Care system, Available at: http://www.
ipfcc.org/pdf/PartneringwithPatientsandFamilies.pdf.
Kim, I.K. & Song, J.H., 2013. Mobile Health reference
architectures. In International Conference on
Information Society (i-Society). IEEE, pp. 158–164.
Available at: http://ieeexplore.ieee.org/articleDetails.
jsp?arnumber=6636363 [Accessed September 9,
2014].
McCormack, B., Dewing, J. & McCance, T., 2011.
Developing Person-Centred Care: Addressing
Contextual Challenges Through Practice
Development. OJIN: The Online Journal of Issues in
Nursing, vol. 16, no. 2. Available at: http://nursing
world.org/MainMenuCategories/ANAMarketplace/A
NAPeriodicals/OJIN/TableofContents/Vol-16-
2011/No2-May-2011/Developing-Person-Centred-
Care.html?css=print.
McDonald, H.P., Garg, A.X. & Haynes, R.B., 2002.
Interventions to Enhance Patient Adherence to
DesignofaRemoteTreatmentMonitoringandSeizureWarningSystemFrameworkforEpilepsyPatients
551

Medication Prescriptions. JAMA, vol. 288, no. 22,
p.2868. Available at: http://jama.jamanetwork.com/
article.aspx?articleid=195605 [Accessed May 26,
2014].
National Society for Epilepsy, Epilepsy Society. Available
at: http://www.epilepsysociety.org.uk/free-epilepsy-
smartphone-app#.U7d8bxbvFqo [Accessed April 1,
2014].
Omary, Z. et al., 2011. Ubiquitous Healthcare Information
System: Assessment of its Impacts to Patient’s
Information. International Journal for Information
Security Research (IJISR), vol. 1, no. 1/2, pp.71–77.
Svanæs, D. & Gulliksen, J., 2008. Understanding the
context of design: towards tactical user centered
design. In NordiCHI. Lund, Sweden.
The National Centre for Young People with Epilepsy,
Young Epilepsy. Available at: http://youngepilepsy.
org.uk/all-about-epilepsy/epilepsy-app [Accessed June
10, 2014].
Vukelja, L., Opwis, K. & Müller, L., 2010. A Case Study
of User-Centred Design in Four Swiss RUP Projects.
Advances in Human-Computer Interaction, vol. 2010.
Wang, C.J. & Huang, A.T., 2012. Integrating Technology
Into Health Care. What will it take? American Medical
Association, vol. 307, no. 6, pp.569–570.
World Health Organization, 2012. Epilepsy. Fact Sheet N
o
999. Available at: http://www.who.int/mediacentre/
factsheets/fs999/en/ [Accessed September 1, 2014].
HEALTHINF2015-InternationalConferenceonHealthInformatics
552
