
Comparison of Recognition Accuracy of ADL with Sensor Wearing
Positions using 3-Axis Accelerometer
D. I. Shin
1
, S. K. Joo
2
and S. J. Huh
2
1
Department of Biomedical Engineering, Asan Medical Center, Seoul, Korea
2
Department of Biomedical Engineering, University of Ulsan College of Medicine, Seoul, Korea
Keywords: Accuracy, Activity, Daily Life, Sensor, Position, Accelerometer.
Abstract: The monitoring of single elderly is being more important due to rapid transition to aging society. There are
many bio-signals to monitor the emergent state of elderly. In this paper we propose new criteria to classify
daily life activities using accelerometer and pulse oximeter. We categorized activities with the motility of
real action. The upper most criteria are normal and abnormal activity. The lower criteria are ‘small or large
movement’, ‘periodic or random movement’, ‘no movement or shock’. Then we derive some parameters to
get thresholds to classify these activities according to our new criteria. The main parameters are entropy,
energy and autocorrelation. Some experiments were carried out to determine classifying thresholds. Finally
we got results of classified activities such as ‘no movements’, ‘small movements’, ‘large movements’,
‘periodic movements’ and ‘falls’. We got nearly 100% of classifying result for falls and no movements. In
this case of ‘quasi-emergency state’ our developing device investigates further status of elderly by
measuring of heart rate and oxygen saturation (SpO
2
) using pulse oximeter. Finally the device decides in
emergency, it sends a short message to server and then connects to the u-Healthcare centre or emergency
centre and one’s family.
1 INTRODUCTION
According to the data from Statistics Korea, the
aging index will increase rapidly from 9.5% (2006)
to 14.3% (2018) and 20.8% (2026). With this trend,
the number of single elderly increases too. Knowing
the emergency status of these single elderly is a
critical issue in the emergency monitoring system.
So we have been developing a monitoring device,
which can be easily worn on an elders’ body. The
wearing position is very important because it must
be very convenient for the elderly. And in the case
of an emergency, the reaction of elderly is also
important for the decision whether he or she is
serious. There were many researches for monitoring
devices(Boo-Ho Yang, Sokwoo Rhee, 2000, P.
Mendoza, P. Gonzalez, B. Villanueva, E.
Haltiwanger, H. Nazeran, 2004, Giuseppe Anastasi,
Marco Conti, Mario Di Francesco, Andrea Passarell,
2009, Francis E.H. Tay, D.G. Guo, L. Xu, M.N.
Nyan, K.L. Yap, 2009, Prajakta Kulkarni, Yusuf
Ozlurk, 2010, Amr Amin Hafez, Mohamed Amin
Dessouky, Hani Fikri Ragai, 2011). In these
researches, there are many considerations about
monitoring devices and systems with respect to u-
Healthcare Monitoring. After all, we conclude that
the ideal wearing position is wrist for now. With the
progress of technology, the device may be the shape
of hearing aid in the future.
In this research, we classified the activity type of
elderly in daily life. Recent researches classified the
activity type with the real action such as walking,
standing, sitting, lying etc.(Arunkumar Pennathur,
Rohini Magham, Luis Rene Contreras, Winifred
Dowling, 2003, A. Mannini, A.M. Sabatini, 2009,
G.M. Lyons, K.M. Culhane, D. Hilton, P.A. Grace,
D. Lyons, 2005, Marcia Finlayson, Trudy Mallinson,
Vanessa M. Barbosa, 2005, Angela L. Jefferson,
Robert H. Paul, Al Ozonoff, Ronald A. Cohen, 2006,
A. Godfrey, A.K. Bourke, G.M. Ólaighin, P. van de
Ven, J. Nelson, 2011). But in fact this kind of
classification is not helpful for the decision of
emergency status of an elderly. So we suggest new
concept of classification criteria. We categorized
activities with the motility of real action. The upper
most criteria will be normal and abnormal activity.
The lower criteria may be ‘small or large movement’,
‘periodic or random movement’, ‘no movement or
180
Shin D., Joo S. and Huh S..
Comparison of Recognition Accuracy of ADL with Sensor Wearing Positions using 3-Axis Accelerometer.
DOI: 10.5220/0005279901800184
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2015), pages 180-184
ISBN: 978-989-758-071-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)
shock’.
Once we classify the elderly activity to abnormal
we can further investigate the accurate status with
the reaction button or pulse oximeter, which will be
adopted by our monitoring device. The clinical
importance of oxygen saturation of blood (SpO
2
) is
mentioned on many articles (Barker SJ, Morgan S.,
2004, Anna Letterstål, Fredrik Larsson, 2007,
Gülendam Hakverdioğlu Yönt, Esra Akin Korhan,
Leyla Khorshid, 2010, Elif Derya Ubeyli, Dean
Cvetkovic, Irena Cosic, 2010)
If we can classify a person’s status by normal or
abnormal, we can make more concrete speculation
in case of abnormal status. As a result, we may
reduce processing resource, power and finally
physical size of the sensor. The more compact size
and reduced processing power will be more
convenient in wearing it.
2 MATERIALS AND METHODS
2.1 System Overview
We extracted acceleration data and oxygen
saturation data from our monitoring device in
developing. Data was moved from the memory of
monitoring device to PC via USB port. Sampling
rate is 10ms/sample and converted by 12bits depth.
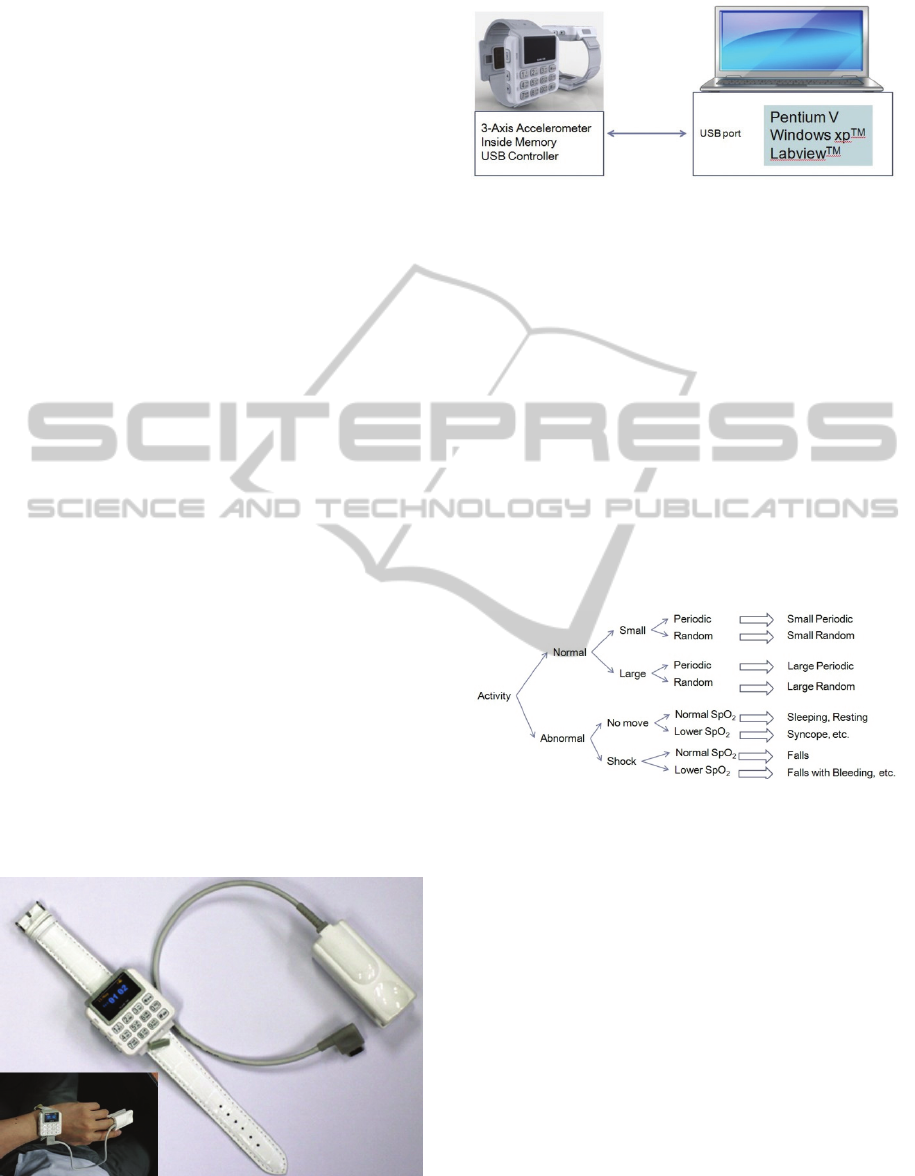
Fig. 1 shows the illustration of our monitoring
device. Figure 2 illustrates our processing system.
Personal computer (Pentium V) is used to process
and analyse activities. The LabView
TM
software
from National Instruments is used to acquire and
display the acceleration data from monitoring device.
The Matlab
TM
software is used to process and
analyse the acceleration data.
Figure 1: The illustration of our monitoring device.
Figure 2: The overall processing system.
2.2 Activity Classification
In this research, we classified the activity type of
elderly in daily life. Recent researches classified the
activity type with the real action such as walking,
standing, sitting, lying etc. But in fact this kind of
classification is not helpful for the decision of
emergency status of an elderly. So we suggest new
concept of classification criteria. We categorized
activities with the motility of real action. The upper
most criteria will be normal and abnormal activity.
The lower criteria may be ‘small or large movement’,
‘periodic or random movement’, ‘no movement or
shock’. Figure 3 shows the classification criteria of
our new concept.
Figure 3: Classification criteria of activities.
The 3-axis acceleration data were pre-processed like
below.
A
o
= sqrt(a
x
2
+ a
y
2
+ a
z
2
) (1)
A
os
= LPF(A
o
) (2)
A
o
is root-mean-square of original 3-axis
acceleration data and A
os
is low pass filtered data
with 5Hz cutoff frequency.
To classify activities, we calculate some
parameters and define threshold of classification.
First, the entropy is measured like below,
Entropy = ∇a/∇t (3)
Entropy is the ratio of acceleration change per
unit time. And the energy is defined like this,
Energy = ∑a (4)
ComparisonofRecognitionAccuracyofADLwithSensorWearingPositionsusing3-AxisAccelerometer
181
It can be interpreted as speed. The autocorrelation is
calculated for the grade of periodicity.
Autocorrelation = Periodicity (a) (5)
2.2.1 Normal Activity Classification
Normal activity is classified with two categories.
The first is the magnitude of movements. This is
judged by the threshold of entropy and energy. The
judge function is described like this.
J
mov
= a*Entropy + b*Energy (6)
The second category is periodicity and judge
function for this is,
J
per
= c*Entropy + d*Autocorrelation (7)
2.2.2 Abnormal Activity Classification
Abnormal state is categorized into two classes. One
is ‘no movements’, the other is ‘falls’. When in ‘no
movements’ there might be two situation which are
“in sleep” and “in emergency”. In these situations
our monitoring device will check heart rate and O2
saturation in blood using pulse oximeter.
To determine whether falls or not, we use the
entropy for the threshold function.
J
fall
= e*Entropy (8)
To determine whether no movements or not, we
use the entropy and the energy for the threshold
function.
J
nmov
= f*Entropy + g*Energy (9)
2.3 Classifying Algorithm
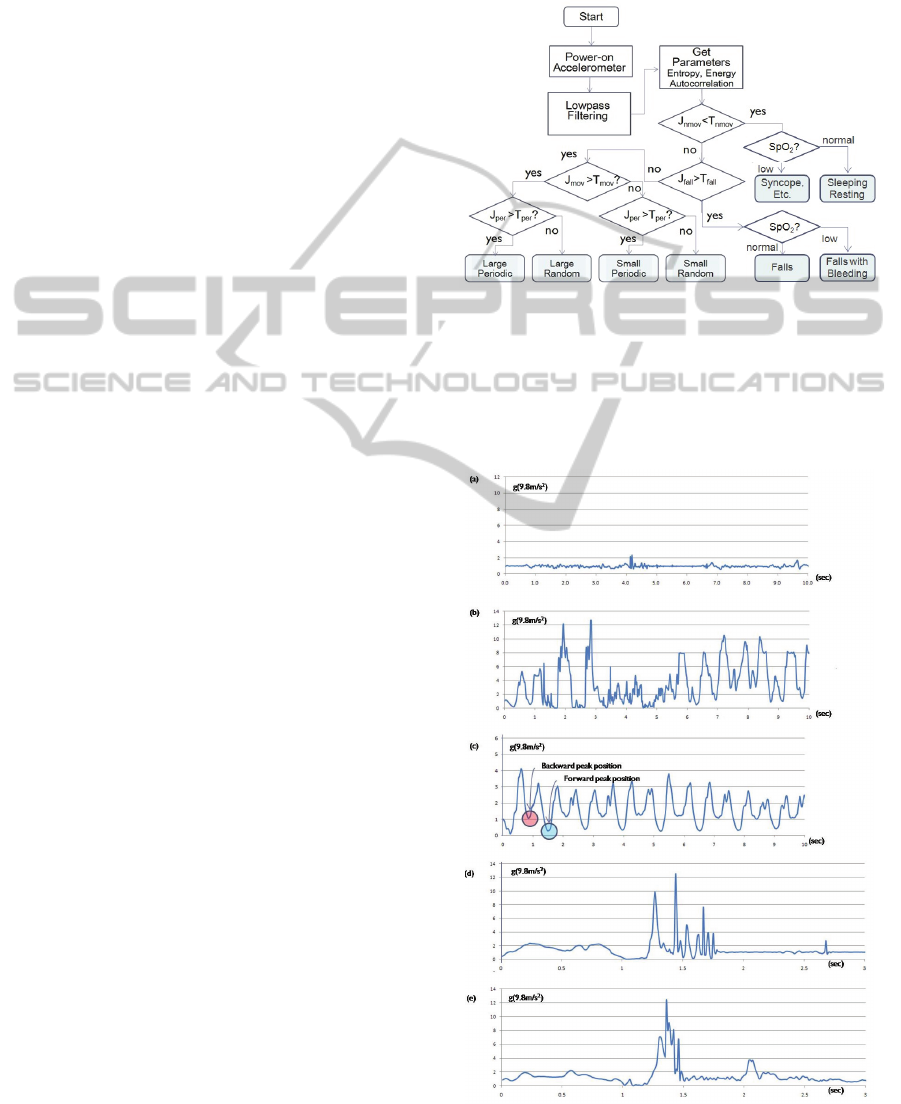
Figure 4 shows the flowchart of activity classifying
algorithm. Once we start the algorithm, the
accelerometer in the device is powered on. The
acceleration data is acquired with the speed of 100
samples/sec. And then the acceleration data is low-
pass filtered with the 5Hz cut-off frequency. We call
these procedures ‘Pre-processing’ and equation (1)
and (2) show these procedures. Next, we calculate
parameters on equations (3) to (5). Using the entropy
and energy we can calculate the parameter J
nmov
. If
J
nmov
is less than the threshold T
nmov
, we can judge
there are no movements such as resting or sleeping
state. If J
nmov
is great than the threshold T
nmov
, we
can judge that there are some movements that
include some kind of falls.
The next stage we investigate the parameter J
fall
according to the equation (8). If this is greater than
T
fall
, a kind of fall must have happened. Once the
state is classified to normal movement, we can
classify to lower categories as shown in figure 3.
In real world, situations are more complex and
ambiguous. So, the classification algorithm is
difficult. But as we refine the algorithm more
accurately, the result will be more realistic.
Figure 4: Flowchart of activity classifying algorithm.
3 RESULT
Figure 5 shows the low-pass filtered acceleration
data. It includes various activities. Small movements
Figure 5: Acceleration data from various activities.
BIODEVICES2015-InternationalConferenceonBiomedicalElectronicsandDevices
182

Figure 6: Classified results for successive various activities.
can be showed in Figure 5(a). These movements
include gripping a pen, writing, moving a paper,
scratching one’s skin, removing glasses etc. In small
movements, it shows small accelerations under 2g
(1g=9.8m/s
2
). On the other hand, Figure 5(b) shows
large movements such as stretching, doing
gymnastics, standing up suddenly etc. It shows large
acceleration of 5g or more. Sometimes it exceeds
10g but its slope is rather than gradual. Figure 5(c)
shows a typical periodic movement which is walking.
There are two levels of valley, the upper valley
represents backward peak position of hand and the
lower valley represents forward peak position of
hand.
Figure 6 shows classified results for successive
various activities according to our algorithm. The
color bar denotes the class of activity. Data from
monitoring device is transmitted to personal
computer and are processed with Labview
TM
and
Matlab
TM
software to verify our algorithm.
4 CONCLUSIONS
Knowing the emergency status of these single
elderly is a critical issue in the emergency
monitoring system. So we have been developing a
monitoring device, which can be easily worn on an
elders’ body. The wearing position is very important
because it must be very convenient for the elderly.
And in the case of emergency, the reaction of the
elderly is also important for the decision whether he
or she is serious. After all, we conclude that the ideal
wearing position is wrist for now. With the progress
of technology, the device may be the shape of
hearing aid in the future.
In this research, we classified the activity type of
an elderly in daily life. Recent researches classified
the activity type with the real action such as walking,
standing, sitting, lying etc. But actually this kind of
classification is not helpful for the decision of
emergency status of an elderly. So we suggest new
concept of classification criteria. We categorized
activities with the motility of real action. The upper
most criteria will be normal and abnormal activity.
The lower criteria may be ‘small or large movement’,
‘periodic or random movement’, ‘no movement or
shock’. Once we classify the elders’ activity to
abnormal we further investigate the accurate status
with the reaction button or pulse oximeter, which is
already adopted, in our monitoring device. If we can
classify a person’s status to normal or abnormal, we
can make more concrete speculation in case of
abnormal status. As a result, we may reduce
processing resource, power and finally physical size
of the sensor. The more compact size and reduced
processing power will be more convenient in
wearing it.
REFERENCES
Boo-Ho Yang, Sokwoo Rhee, Development of the ring
sensor for healthcare automation, Robotics and
Autonomous Systems 30 (2000) 273–281
P. Mendoza, P. Gonzalez, B. Villanueva, E. Haltiwanger,
H. Nazeran, A Web-based Vital Sign Telemonitor and
Recorder for Telemedicine Applications, in
Proceedings of the 26th Annual International
Conference of the IEEE EMBS San Francisco, CA, USA,
September 1-5, 2004, pp. 2196-2199.
No Movements
Small Movements Large Movements
Small Movements
Periodic Movements
Falls
No Movements
ComparisonofRecognitionAccuracyofADLwithSensorWearingPositionsusing3-AxisAccelerometer
183

Giuseppe Anastasi, Marco Conti, Mario Di Francesco,
Andrea Passarell, Energy conservation in wireless
sensor networks: A survey, Ad Hoc Networks 7 (2009)
537-568
Francis E.H. Tay, D.G. Guo, L. Xu, M.N. Nyan, K.L. Yap,
MEMSWear-biomonitoring system for remote vital
signs monitoring, Journal of the Franklin Institute 346
(2009) 531–542
Prajakta Kulkarni, Yusuf Ozlurk, mPHASiS: Mobile
patient healthcare and sensor information system,
Journal of Network and Computer Applications, 2010
Amr Amin Hafez, Mohamed Amin Dessouky, Hani Fikri
Ragai, Design of a low-power ZigBee receiver front-
end for wireless sensors, Micro Electronics Journal 40
(2011) 1561-1568
Arunkumar Pennathur, Rohini Magham, Luis Rene
Contreras, Winifred Dowling, Daily living activities in
older adults:Part II—effect of age on physical activity
patterns in older Mexican American adults,
International Journal of Industrial Ergonomics 32
(2003) 405–418
G.M. Lyons, K.M. Culhane, D. Hilton, P.A. Grace, D.
Lyons, A description of an accelerometer-based
mobility monitoring technique, Medical Engineering &
Physics 27 (2005) 497–504
Marcia Finlayson, Trudy Mallinson, Vanessa M. Barbosa,
Activities of daily living (ADL) and instrumental
activities of daily living (IADL) items were stable over
time in a longitudinal study on aging, Journal of
Clinical Epidemiology 58 (2005) 338–349
A. Mannini, A.M. Sabatini, Computational methods for
the automatic classification of postures and movements
from acceleration data, Gait & Posture 30S (2009) S26–
S74
A. Godfrey, A.K. Bourke, G.M. Ólaighin, P. van de Ven,
J. Nelson, Activity classification using a single chest
mounted tri-axial accelerometer, Medical Engineering
& Physics, in Press (2011)
Angela L. Jefferson, Robert H. Paul, Al Ozonoff, Ronald
A. Cohen, Evaluating elements of executive functioning
as predictors of instrumental activities of daily living
(IADLs), Archives of Clinical Neuropsychology 21
(2006) 311–320
Thessa I.M. Hilgenkamp, Ruud van Wijck, Heleen M.
Evenhuis, (Instrumental) activities of daily living in
older adults with intellectual disabilities, Research in
Developmental Disabilities 32 (2011) 1977–1987
Barker SJ, Morgan S., A Laboratory Comparison of the
Newest “Motion-Resistant” Pulse Oximeters During
Motion and Hypoxemia, Anesthesia and Analgesia
2004;98(55),S2:A6
Anna Letterstål, Fredrik Larsson, Assessment of vital
signs on admission to short time emergency wards
improves patient safety and cost-effectiveness,
Australasian Emergency Nursing Journal, Volume 10,
Issue 4, November 2007, Page 191
Gülendam Hakverdioğlu Yönt, Esra Akin Korhan, Leyla
Khorshid, Comparison of oxygen saturation values and
measurement times by pulse oximetry in various parts
of the body, Applied Nursing Research, 2010
Elif Derya Ubeyli, Dean Cvetkovic, Irena Cosic, Analysis
of human PPG, ECG and EEG signals by eigenvector
methods, Digital Signal Processing 20 (2010) 956–963
BIODEVICES2015-InternationalConferenceonBiomedicalElectronicsandDevices
184
