
Activity Theory as a Lens to Identify Challenges in Surgical Skills
Training at Hospital Work Environment
Minna Silvennoinen
1
and Maritta Pirhonen
2
1
Agora Center, University of Jyvaskyla, Mattilanniemi 2, Jyvaskyla, Finland
2
Department of Computer Science and Information Systems, University of Jyvaskyla, Mattilanniemi 2, Jyvaskyla, Finland
Keywords: Surgical Skills Training, Activity Theory, Surgical Simulator, Expertise Development.
Abstract: In this paper the concepts from activity theory (AT) are applied for identifying the challenges and
contradictions emerging in surgical resident’s curriculum based training at hospital. AT is utilised as a lens
to identify contradictions that cause disturbances, problems, ruptures, breakdowns, and clashes which
emerge while surgical skills training is implemented in a new way at hospital. We especially aim at finding
solutions for contradictions which emerge while the new and old working culture are confronted and the
workers are required to balance themselves between the patient care demands and workplace learning
requirements. We are using the conceptual theoretical approach to describe the phenomenon of surgical
working.
1 INTRODUCTION
Surgical traditions are facing the need for radical
changes. Throughout the history, the method of
teaching and learning surgery has been the
apprentice model in which surgical residents follow
specialist surgeons at work and develop their skills
with the “see-one, do–one” method while gradually
progressing to become as independent physicians.
The learning opportunities and method are
extremely workplace dependent and situationally
affected by each hospital’s working culture and the
supervising senior’s guidance and work duties. Now,
the new development of computer based simulators
and skill requirements of video-assisted surgery
have challenged this traditional way of mentoring
residents learning (Gallagher and O'Sullivan 2012,
Reznick 2006). The arguments favourable to
operating skills curriculum which utilises newest
technology, surgical simulators, have forced also the
hospitals to consider their learning and teaching
traditions in a new way (Aggarwal et al. 2006).
Simulators have already proven to significantly
increase the efficiency of skills learning, they are a
good investment into error-preventive actions and
cost reduction relating highly expensive surgical
complications and should be used as mandatory part
in training from patient safety reasons (Reznick
2006). However, there are various views on how
resident education at hospitals should be arranged
(Hammoud et al. 2008). Even though the
development of surgical computer-based simulators
has been rapid, these learning tools are still not
utilized systematically in surgical training in
Finland, why? Previous research has found that
implementation of a curriculum based training at
hospital is not without problems (Silvennoinen et al.
2011 and 2012, van Dongen 2008). Hospitals are not
designed for learning; instead they are built for
taking care of patients. The problems in
implementation process might be caused by the fact
that even though the need for making workplaces
effective learning environments exists, it requires a
clear vision about the best possible learning structure
within each workplace (Billett 2000). In order to
implement new training models which will bring
possible rather radical change to the old traditional
training culture, we should form clear vision of both
the context and the phenomenon.
Alan Bleakley (2011) suggests models of socio-
cultural learning theories to be used in explaining
surgical learning at work. This activity partially is
seen through the model of communities of practice
by Lave and Wenger (1991), as participation in a
highly context-situated and dependent work-based
activity. Bleakley (2011) also sees that the actor-
network theory by Latour (1996) and activity theory
by Engeström (1987) can be used for competence
455
Silvennoinen M. and Pirhonen M..
Activity Theory as a Lens to Identify Challenges in Surgical Skills Training at Hospital Work Environment.
DOI: 10.5220/0005497204550462
In Proceedings of the 7th International Conference on Computer Supported Education (CSEDU-2015), pages 455-462
ISBN: 978-989-758-108-3
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

development discussion. The advantages of AT in
the role of explaining the phenomenon is the
dynamic nature of learning activities, an activity
system (surgical residents training at hospital),
which is focused on achieving the same goal but still
conflicts can be produced (Bleakley 2011). The
social theories of learning are important in observing
activities where the impact of the team in the
learning process is highly important (Fry 2011). The
strength of AT is that it allows for breaking down
the structure of an activity into smaller categorical
elements (Basharina, 2007), and to identify
contradictions and structural tensions of the activity
(Engeström, 1995; Engeström, 2001). Contradictions
are not simply conflicts or problems but they are
structural tensions that have been historically
accumulated within and between activity systems
(Engeström 2001, 137). The identication of
contradictions in an activity system helps focusing
the efforts on the root causes of problems. When
contradictions arise, or when they are observed, they
expose dynamics, inefficiencies, and importantly,
opportunities for a change (Helle 2000).
In this article, surgical training as a workplace
learning activity at hospital is explored. We utilise
AT (Engeström 1987, 2001) as a lens to identify and
explore the challenges which emerge while surgical
skills training is implemented in a new way at
hospital. We especially aim at finding solutions for
contradictions which emerge while the new and old
working culture are confronted and the workers are
required to balance themselves between the patient
care demands and workplace learning requirements.
This paper is organized as follows. First, we
present the background on the requirements needed
for surgical work. Then requirements for enhancing
surgical learning at work are presented. This is
followed by the brief description of activity theory
and the description of the surgical training program
in a hospital context as an activity in AT. Finally,
identified contradictions and solutions are presented.
2 SURGEONS PROFESSIONAL
REQUIREMENTS AT
HOSPITAL IN THE CONTEXT
OF LAPAROSCOPY
Surgical work requires considerable psychomotor
skills, critical thinking abilities and decision-making
skills, a great deal of medical knowledge to recall
and apply as well as situational awareness to be able
to react rapidly to changing situations (Norman et al.
2006). Technical skills and dexterity are seen as
important for safe surgery, but from a patient safety
perspective, in order to maintain surgical expertise,
great deal of non-technical proficiency is also
needed (Yule et al. 2008, Yule and Patterson-Brown
2012). Surgeons are leaders of an operation team
which requires also responsibilities and social
abilities, so besides the technical skills, also the
cognitive and interpersonal abilities like team
working and decision making skills are needed
(Yule et al. 2008, Yule and Patterson-Brown 2012).
While skills and learning demands in modern
healthcare tends to increase, at the same time the
surgical residency time at hospitals has been
shortened as a result of new European Working
Time Directive (Bleakley 2011). Many surgeons and
senior residents have therefore concerns that
graduating residents are not anymore fully prepared
for independent work immediately after graduation
(Britt et al. 2009). In Finland the residency period
also contains a nine-month period of training in
general medicine, which does not enhance surgical
skills and surgical residents have around five years’
time to develop their specialised expertise.
The awareness of the surgical skill challenges
especially relating abdominal area video-assisted
procedures, laparoscopies has made it topical target
for research and curriculum implementation. The
technique is very popular, it needs a very short sick
leave, 7-10 days, and most of the patients are able to
go home on the operation day (Satava 2011). There
is however concerns relating increased training
requirements since the complication rates of these
procedures remain relatively high compared to open
surgeries due to various skill demands (Subramonian
et al. 2004). In video-assisted operation, surgeons
have limited visual and haptic information compared
to the open surgical technique where the incision is
larger and the visual field is normal, not transmitted
by camera and surgeons can touch the tissues with
hands, not only with long thin instruments (Van
Veelen et al. 2003).
3 IDENTIFIED REQUIREMENTS
FOR ENHANCING SURGICAL
WORKPLACE LEARNING
Surgical residents learn most of the operating skills
during their residency time while working in
hospitals. It is notable from the point of view of
education and learning that this obviously very
important period includes no structured curriculum.
CSEDU2015-7thInternationalConferenceonComputerSupportedEducation
456

Therefore a great deal of attention needs to be paid
on how resident’s education during hospital work
should be implemented in a successful way.
Making workplaces effective learning
environments is an interest in many fields today
including healthcare, which means creating
meaningful opportunities to facilitate skills and
knowledge development at work (Van De Wiel et al.
2011). Learning at work is not obvious or automatic,
but workplaces should actually be designed to
promote learning (Ellström et al. 2008). Workplaces
vary a lot in how they enable, support or constrain
learning, which effects on learning opportunities and
execution (Tynjälä 2008). The ‘expansive learning
environments’ provide the best possibilities for both
organisational and individual development as well as
their integration (Fuller et al. 2004). The list of the
issues identified on organisations that are fostering
an expansive workplace learning approach to
workforce development can be shortly listed as
follows according to Fuller et al. 2004, Fuller and
Unvin 2010:
• Workforce development is used as a vehicle for
aligning the goals of developing the individual and
organisational capability
• Organisational recognition of and support for workers
as learners - given time to become full members of
the community through gradual transition, having a
vision of workplace learning such as providing
chances to learn new skills/jobs and access to range of
qualifications.
• Managers given time (and resources) to support
workforce development and facilitate workplace
learning and individual development
• Skills and knowledge widely distributed through
workplace—multi-dimensional view of expertise;
valuing expertise, high trust
• Workers given discretion to make judgments and
contribute to decision-making
• Participation in different communities of practice
inside and outside the workplace is encouraged—
job/team boundaries can be crossed, cross-boundary
communication encouraged and identity extended
• Planned time off-the-job for reflection and deeper
learning beyond immediate job requirements.
In a context of this study, fostering surgical
expertise development at a hospital would require a
vision and development of both organisation and
individuals through workplace learning. As an
example, this would mean a curriculum developed
for the surgical residents. It would also mean
hospital organisations and managers recognition of
and support for surgeons as learners not just as a
workforce, making commitments to chances and
organising time for skills development and reflection
both on- and off-the-job during the courses, high
appreciation towards expert laparoscopists, but still
fostering cross-boundary communication within
surgical teams.
There is still a shortage of research on how the
medical experience and learning at work should be
structured to enhance skills and knowledge
development optimally (Norman et al. 2006, Van De
Wiel et al. 2011) Employees should be provided
opportunities to acknowledge and utilize the
learning situations at work, and the managers should
be provided with adequate competences to organise
and lead workplace learning (Ellström et al. 2008).
Learning task or curriculum-based learning
assignment within hospital alongside the resident’s
normal work, is similar that Tynjälä calls on-the-job
learning (Tynjälä 2008), when conducting
successfully as a learning activity, at least the
following elements should be taken account: First,
theory and practice should be meaningfully
connected, second learners need to be provided
conceptual and pedagogical tools to enable the
integration of theory and practice when solving
problems, for example, simulated contexts, and third
participating in real-life situations is not solely
sufficient for the development of high-level
expertise. In professional expertise, theoretical-,
practical-, and self-regulative knowledge are closely
integrated (Tynjälä 2008) and the education of
surgical residents shall therefore also be structured
and combine all three.
The current research on continuing education of
health professionals tends to promote research-based
pedagogical self-assessment in professional
development, to help physicians become better
informed about self-assessment and more skilled
monitors of their own practice (Eva and Regehr
2011, Moulton and Epstein 2011). Self-monitoring
is one aspect of self-assessment, a metacognitive
process that is necessary to manage in order to
sustain adequate situational awareness, an important
feature of expert performance (Eva and Regehr
2011, Moulton and Epstein 2011). Moment-to-
moment self-monitoring is an important aspect of
healthcare professionalism that seems to form the
basis of the early recognition of cognitive biases,
technical errors and facilitating self-correction and
self-questioning (Epstein et al. 2008).
Simulators are suggested to be used as training
tools within formal residency curricula, which would
integrate SBT into surgical residents’ other daily
work routines (Kneebone 2003, Van Dongen et al.
2008). Practicing opportunities should be organised
systematically and periodically within longer
ActivityTheoryasaLenstoIdentifyChallengesinSurgicalSkillsTrainingatHospitalWorkEnvironment
457
interval periods in order for the requirements for
expertise development in complex skills like
laparoscopy to be fulfilled (Ericsson 2004). It would
also be important to get the senior surgeons involved
in training, although simulator practise should
always contain tutoring, assessment and corrective
feedback for enhancing learners’ evaluative
reflection processes (Kneebone 2003, Epstein et
al.2008).
Based on the knowledge gathered on former
literature relating surgical skills training as well as
the empirical findings gathered from the surgical
procedures performed by the residents under senior
guidance, the curriculum of laparoscopy skills
learning was launched in 2008 which contained both
instructive sessions with supervisor and independent
training as well as lectures (Silvennoinen 2011).
Simulator training took place in a skill centre at
hospital, where residents could practice with the
simulator when actual patient care allowed. The
support during training was offered through
specialist instructions, feedback and assessment
tasks performed both residents themselves (self-
assessments) and seniors (evaluations/exams). Also
the simulator measurements were available
(performance parameters) for training feedback.
Training alongside real patient treatments was
considered as a connective link from the simulator to
real workplace learning. Also lectures and instructed
self-study was organized to enhance learning
(Silvennoinen 2011). However there emerged
challenges such as time allocation problems which
interfered both residents training and supervisor
surgeon’s guidance and some residents dropped out
the program or didn’t perform adequate amount of
simulator training to achieve the required skill level,
even though training was experienced both
important and useful (Silvennoinen 2011).
4 ACTIVITY THEORY IN THE
CONTEXT OF SURGICAL
LEARNING AT HOSPITAL
Activity theory (AT) offers a theoretical framework
to study both individual and collective activities.
The basic unit of analysis in activity theory is human
activity which ties individual actions in context. An
activity has in particular situation it also means that
it is impossible to make general classification of
what is an activity (Kuutti 1991). It provides an
analytical framework within which to study human
activity in general. An activity system (AS) includes
two types of constituents: core components, such as
subject, object/outcome, and community; and
mediatory components, such as instruments/tools,
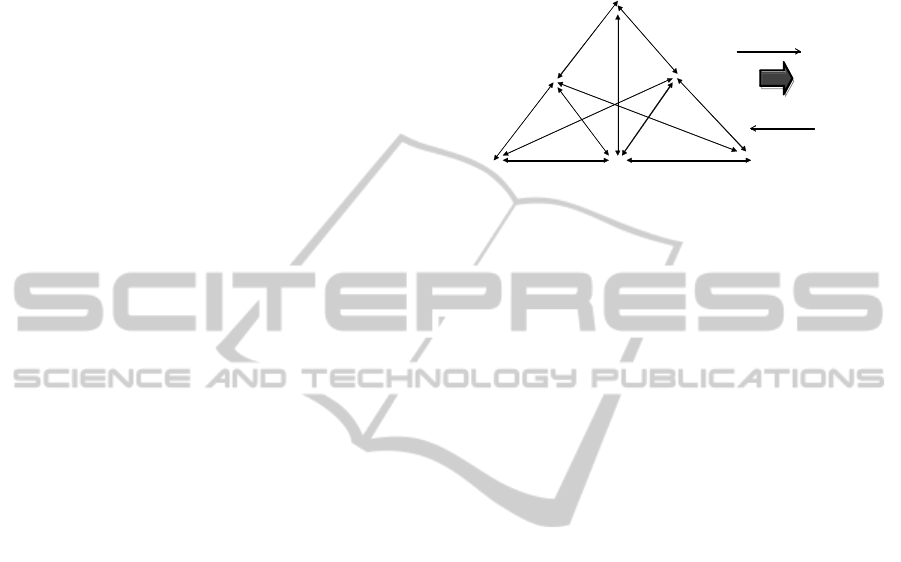
rules, and division of labor (see Figure 1).
Figure 1: The structure of a human activity (adapted from
Engeström, 1987, p. 78).
Engeström added the concept of contradiction onto
Vygotsky´s (1978) thinking. Contradictions
constitute a key principle in AT and shape an
activity (Engeström, 2001). Kuutti (1996, p. 34)
describes contradictions as “a misfit within
elements, between them, between different
activities, or between different development phases
of a single activity”. They generate “disturbances
and conflicts, but also innovative attempts to change
the activity” (Engeström, 2001, p. 134).
Contradictions are significant for development
and they exist in the form of resistance to achieving
goals of the intended activity. They also exist as
emerging dilemmas, disturbances, and
discoordinations. In spite of the potential of
contradictions to result in development in an activity
system, the development does not always occur.
Often contradictions may not be easily recognized or
acknowledged, visible, or even openly discussed by
those experiencing them (Engeström 2000 2001). On
the other hand, contradictions that are not discussed
may be embarrassing, or uncomfortable in nature.
They may also be culturally difficult to confront,
such as personal habits, bad behaviour, or an
incompetence of the leader.
An activity is always associated with long-term
purposes and strong motives. All members of the
community share the object (and the motive) of the
activity. Tools mediate between a subject and the
object, which is transformed into the outcome. The
object is seen and manipulated within the limitations
set by the tools. Rules mediate the relationship
between the community and the subject, while the
division of labor mediates the relationship between
the community and the object. Rules cover both
implicit and explicit norms, conventions, and social
Inst
r
uments
Object
Rules
Subject
Communit
y
Division of
l
a
bour
Outcome
Transformation
Motivation
CSEDU2015-7thInternationalConferenceonComputerSupportedEducation
458
relations in a community as related to the
transformation process of the object into an
outcome. The responsibilities of the members of the
community are coordinated by some division of
labor (e.g., the division of tasks and roles among
members of the community and the divisions of
power and status), yet guided by rules. These rules
regulate, as well as constrain, their actions and
relationships in the activity system (Engeström
1990, Kuutti, 1996). A weakness of the AT and also
strength to some extend is its generality. The
definition being totally dependent on what the
subject, object etc. is in particular situation it also
means that it is impossible to make general
classification of what is an activity (Kuutti 1991).
To summarize, subjects, who are motivated by
an object, carry out activities. A subject transforms
the object into an outcome. An object may be shared
by a community of people, working together to
achieve a desired outcome. Tools, rules, and a
division of labor mediate the relationship between
the subjects, community, and the object.
Contradictions are a key principle in AT and they
are driving force of change.
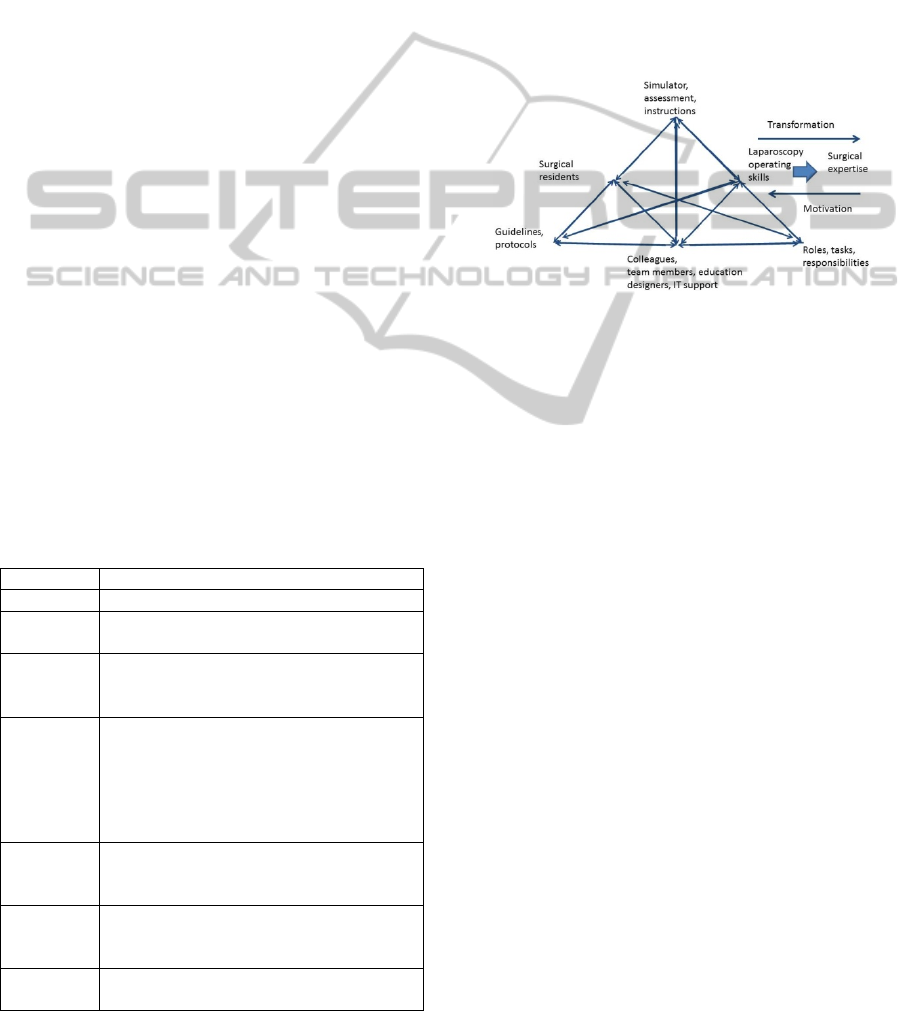
In the depiction of surgical residents training at
hospital as an activity, the resident surgeons are
chosen to be a subject. A subject plays a key role
when analysing other elements of an activity. In this
case we are interested in how the hospital working
culture promotes or restricts workplace learning –
how for example the tools support residents learning
and achieving the learning objectives or how the
Table 1: Surgical residents training at hospital.
Component Description
Subject Resident surgeons
Object To learn skills needed in operating
laparoscopic procedures
Outcome Resident surgeons with adequate
professional skills to perform surgical
operations
Instruments
(tools)
Virtual reality simulator for practicing
p
sychomotor skills, ergonomics, procedures
etc., guidelines and instructions (written,
online videos, lectures, seminars), senior
surgeons guidance during simulator training,
pedagogic methods
Community Surgical residents, senior surgeons, surgical
team members, education designers, IT
support
Division of
labour
Roles, tasks, responsibilities divided among
a community such as teaching, skills
practising, guidance, support
Rules Patient treatment policies guidelines,
treatment protocols
community supports the usage of the tools. From the
residents’ and supervisors’ as well as hospital points
of view, the main object is to produce skilled
professional surgeons for the hospital work to
maintain and further enhance patient safety, working
efficiency and resources. The activity “surgical
residents training at hospital” is presented in the
terms of activity theory (AT) in Table 1.
The instruments (tools) include simulation
environment for practising skills, assessment tools
such as self-assessment forms and instructions for
training and conducting independent learning, senior
guidance sessions, lectures etc. (see Figure 2).
Figure 2: Surgical residents training at hospital as an
activity.
The mediating tools in the surgical education context
in hospitals could be seen as enhancing
metacognitive and reflective skills, such as creating
possibilities for supervisor-learner discussions and
self-assessments. For improving workplace learning,
Kyndt et al. (2009) sees as the most crucial
contribution to support the condition of “feedback
and knowledge acquisition”. This means creating
situations for receiving feedback, such as enhancing
teamwork practices, debriefings or peer feedback
possibilities (Kyndt et al. 2009).
5 CHALLENGES IN SURGICAL
TRAINING AT HOSPITAL
WORK
The empirical evidences presented in this chapter are
based on Silvennoinen´s study (2011). The study
was conducted in a Finnish hospital in which
resident training was studied with variable methods,
such as observations, and data was also gathered via
interviews and questionnaires and analysed with
both qualitative and quantitative approaches.
However, in this paper we present several
contradictions in AT system of surgical residents
training applying new simulation-based learning
ActivityTheoryasaLenstoIdentifyChallengesinSurgicalSkillsTrainingatHospitalWorkEnvironment
459

approach at hospital work environment. Many of the
contradictions are in connection to the elements of
expansive workplace learning and emerge when
organisations are not fostering an expansive
workplace learning approach.
The problematic issues or contradictions within
AT system can be listed as the elements affecting to
training program implementation and the realisation
fluency of this new type of workplace learning.
1) Workplace culture, such as hospital’s
recognition and support for employees as
learners can be compromised by the fact that
there is not enough planned time off-the-job for
simulation-based training (SBT). This creates a
contradiction between the Rules and Subject.
2) Second contradiction relates to senior surgeons,
since hospital’s recognition of, and support for
employees as teachers/instructors is sometimes
also compromised by the same fact that they
also have other tasks and not enough planned
time off-the-job for instructors of (SBT) for
facilitating learning and developing their own
competences. This creates a contradiction
between the Division of labour and
Community.
3) Lack of metaskills – (self-assessment is
experienced as difficult task). This
contradiction emerges when Instruments are
not supporting the Subject.
4) Learning requirements; the gap between the
surgical work task demands and existing skills
(too difficult tasks for example relating
psychomotor abilities). This creates another
contradiction between the Rules and
Instruments.
5) Special characteristics /constraints of the
simulation environment; usability and efficacy
problems: realism, interactivity, received
feedback, potential to enhance skill transfer.
This inner contradiction emerges within
Instrument.
Figure 3: Identified contradictions.
Contradictions have several consequences. The
contradiction between Rules and Subject creates
problems with motivation when residents are not
willing to come to practise skills with simulators
after normal working hours. Also the problems of
managing one’s working hours might cause
exhaustion which results in motivation decrease.
6 CONCLUSIONS
From the curriculum design viewpoint, we should be
able to define the activities that surgical residents
need to engage in. The two main tasks taking care of
patients and learning to become specialised
physicians seem sometimes contradictive.
Identifying contradictions within and between these
two different activities - effective learning at
workplace and taking care of patients should
enhance understanding on how the workplace
learning could be enhanced more efficiently.
In this paper we used the concepts from the
activity theory (Engeström 1987, 1999) to identify
contradictions within the surgical residents training
at hospital activity. The following contradictions
were identified: contradiction between the Rules and
Subject, contradiction between the Division of
labour and Community, contradiction between
Instruments and Subject, contradiction between the
Rules and Instruments, and inner contradiction
within Instruments.
There are several studies that support the
findings of this paper. It has been noticed that the
hospital routines and rules are not adequately
supportive of changes within resident education that
has remained unchanged for centuries. The study of
Van de Wiel et al. (2011) is supporting this
argument, which shows that learning opportunities
for expertise development are not utilized optimally
by the young physicians at clinics. The learning is
organized according to physician’s practical
experience and patient care procedures, and
opportunities for enhancing deliberate learning are
not actively sought (Van de Wiel et al. 2011).
In the study of Kyndt et al. (2001) there emerged
several prohibiting reasons for participation in
formal learning activities amongst public healthcare
employees. The residents were discouraged by the
‘required investments’ such as distance, costs, time,
or writing assignments relating to the learning
activity and they also more likely have children, who
might prohibit extra working or training hours
(Kyndt et al. 2011). On the other hand the older
generation, like senior surgeons might have
CSEDU2015-7thInternationalConferenceonComputerSupportedEducation
460

attitudinal issues towards learning with new
technology and might even experience that they are
not good at learning new things and “refuse going
back to school (Kyndt et al. 2011).
In a context of education, for example, a
contradiction in teachers’ practices might occur
when a new technology is introduced into their
activity system and clashes with an old element (see
e.g. Engeström 1995, Murphy and Manzanares
2008, and Turner and Turner 2001). The similar
features emerge at the surgical simulator training
while implemented in traditional working culture.
We present recommendations for dealing with
the contradictions that we presented in this paper.
First, the lack of hospital’s recognition and support
for employees as learners and fact that there is not
enough planned time off-the-job for simulation-
based training. The contradiction between the Rules
and Subject can be dealt with careful planning and
implementation of new workplace learning activities
which creates a culture in which better commitment
of the whole organisation and all workers is reached.
The potentiality for workplace learning depends here
on the extent that hospital is designed not only to
produce service of patient care, but to support
workers competency development (Ellström et al.
2008). The success for supporting workplace
learning would therefore require changes to
traditional training culture and whole hospital
organisation. Enhancing open discussions and
enabling high level decisions relating trainees and
trainers division of labor is needed. Better success
would be acquired by investing more human
resources and time allocated for instruction, training
and facilitating.
Second contradiction was the lack of instructors
time allocated to instructing residents since they also
has several other tasks relating patient treatment.
This contradiction between the Division of labour
and Community could be dealt with similar
proposals for action. Lack of metaskills of the
medical residents as well as specialist doctors has
also been found in other research (Silvennoinen
2011) which suggests that educating and practising
self-monitoring and self-assessment is needed.
The contradiction between Rules and
Instruments caused by too high demands in learning
should be solved by offering the residents gradual
progressive tasks with senior support and guidance.
At work the interaction between novices and experts
is very important (Billet 2000) and in surgery this
means that the residents needs to interact with
specialists and work under their guidance, taking
part in the job tasks together – in other words,
participating in the communities of practice (Lave
and Wenger 1991).
The special characteristics/constraints of the
inner contradiction emerging within instruments
need both the technical development and evaluation
of tools used for skills practising, such as surgical
simulators. Supportive actions for training
implementation at hospital environment could also
be co-creative planning and right placement of
training and defining the right training phase within
resident curriculum. Critical evaluation should be
used for guaranteeing continuity and quality
progress of the education design.
REFERENCES
Aggarwal, R., Grantcharov, T., Moorthy, K., Hance, J. and
Darzi, A. 2006. A competency-based virtual reality
training curriculum for the acquisition of laparoscopic
psychomotor skill. The American Journal of Surgery
191(1), 128-133.
Basharina, O. K. 2007. An activity theory perspective on
student-reported contradictions in international tele-
collaboration. Language Learning and Technology,
11(2), 82-103.
Billett, S. (2000). Guided Learning at Work. Journal of
Workplace Learning, 12(7), 272-285.
Bleakley, A. 2011. Learning and Identity Construction in
the Professional World of the Surgeon. In H. Fry and
R. Kneebone (Eds.) Surgical Education: Theorising
an Emerging Domain. Netherlands: Springer, 183-
197.
Britt, L. D., Sachdeva, A. K., Healy, G. B., Whalen, T. V.,
and Blair, P. G. (2009). Resident duty hours in surgery
for ensuring patient safety, providing optimum
resident education and training and promoting resident
well-being: a response from the American College of
Surgeons to the Report of the Institute of Medicine,
“Resident Duty Hours: Enhancing Sleep, Supervision,
and Safety”. Surgery, 146(3), 398-409.
Ellström, E., Ekholm, B. and Ellström, P. 2008. Two
Types of Learning Environment: Enabling and
Constraining a Study of Care Work, Journal of
Workplace Learning, 20(2), 84-97.
Engeström, Y. 1987. Learning by expanding: An activity-
theoretical approach to developmental research.
Helsinki: Orienta-konsultit.
Engeström, Y. 1995. Objects, contradictions and
collaboration in medical cognition: an activity-
theoretical perspective. Artificial Intelligence in
Medicine, 7(5), 395-412.
Engeström, Y. 1999. Expansive Visibilization of Work: an
Activity Theoretic Perspective. Computer Supported
Cooperative Work (CSCW), 8(1-2), 63-93.
Engeström, Y. 2000. Activity theory as a framework for
analyzing and redesigning work. Ergonomics, 43(7),
960-974.
ActivityTheoryasaLenstoIdentifyChallengesinSurgicalSkillsTrainingatHospitalWorkEnvironment
461

Engeström, Y. 2001. Expansive Learning at Work:
towards an Activity Theoretical Reconceptualization.
Journal of Education and Work, 14(1), 133-156.
Epstein, R. M., Siegel, D. J. and Silberman, J. 2008. Self-
monitoring in Clinical Practice: A Challenge for
Medical Educators. Journal of Continuing Education
in the Health Professions, 28(1), 5-13.
Ericsson, K. A. (2004). Deliberate practice and the
acquisition and maintenance of expert performance in
medicine and related domains. Academic medicine,
79(10), S70-S81.
Eva, K. W. and Regehr, G. 2011. Exploring the
Divergence between self-assessment and Self-
monitoring. Advances in Health Sciences Education
16(3), 311-329.
Fry, H. 2011. Educational Ideas and Surgical Education.
In H. Fry and R. Kneebone (Eds.) Surgical Education:
Theorising an Emerging Domain. Springer, 19-36.
Fuller, A., Munro, A. and Rainbird, H. 2004. Workplace
learning in context. Routledge.
Fuller, A. and Unwin, L. 2010. ‘Knowledge workers’ as
the new apprentices: The Influence of Organisational
Autonomy, Goals and Values on the Nurturing of
Expertise. Vocations and Learning, 3(3), 203-222.
Gallagher, A. G. and O'Sullivan, G. C. 2012.
Fundamentals of Surgical Simulation: Principles and
Practice. London: Springer Verlag.
Helle, M. 2000. Disturbances and Contradictions as Tools
for Understanding Work in the Newsroom.
Scandinavian Journal of Information Systems, 12(1),
81-113.
Kneebone, R. (2003). Simulation in Surgical Training:
Educational Issues and Practical Implications. Medical
Education, 37(3), 267-277.
Kuutti, K. 1991. Activity Theory and Its Applications to
Information Systems Research and Development. In
H.-E. Nissen, H. Klein, R. Hirscheim (eds.).
Information Systems Research: Contemporary
Approaches and Emergent Traditions. North Holland:
Elsevier Science Publishers, 529-549.
Kuutti, K. 1996. Activity Theory as a Potential
Framework for Human-computer Interaction
Research. In B. Nardi (ed.) Context and
Consciousness: Activity Theory and Human Computer
Interaction, MIT Press, Cambridge, 17-44.
Kyndt, E., Dochy, F. and Nijs, H. 2009. Learning
Conditions for Non-formal and Informal Workplace
Learning. Journal of Workplace Learning, 21(5), 369-
383.
Latour, B. 1996. On actor-network theory: a few
clarifications. Soziale welt, 369-381.
Lave, J. and Wenger, E. 1991. Situated Learning:
Legitimate peripheral participation. Cambridge
University Press.
Moulton, C. and Epstein, R. 2011. Self-Monitoring in
Surgical Practice: Slowing Down When You Should.
In H. Fry and R. Kneebone (Eds.) Surgical Education:
Theorising an Emerging Domain. Springer, 169-182.
Murphy, E. and Manzanares, M. A. R. 2008.
Contradictions between the Virtual and Physical High
School Classroom: A Third-generation Activity
Theory Perspective. British Journal of Educational
Technology, 39(6), 1061-1072.
Norman, G., Eva, K., Brooks, L. and Hamstra, S. 2006.
Expertise in Medicine and Surgery. In K. Anders
Ericsson, N. Charness, P. J., Feltovich, R. R. Hoffman
(eds.) The Cambridge Handbook of Expertise and
Expert Performance, 339-354.
Reznick, R. K. 2006. Medical Education: Teaching
Surgical Skills - Changes in the Wind. New England
Journal of Medicine, 355(25), 2664-2669.
Satava, R. M. 2011. Moral and Ethical Issues in
Laparoscopy and Advanced Surgical Technologies. In
Minimally Invasive Surgical Oncology. Springer, 39-
45.
Silvennoinen, M. 2011. Learning Surgical Skills with
Simulator Training: Residents’ Experiences and
Perceptions. In Proceedings of Informing Science and
IT Education Conference (InSITE).
Silvennoinen, M., Helfenstein, S., Ruoranen, M. and
Saariluoma, P. 2012. Learning Basic Surgical Skills
through Simulator Training. Instructional Science,
40(5), 769-783.
Subramonian, K., DeSylva, S., Bishai, P., Thompson, P.
and Muir, G. 2004. Acquiring Surgical Skills: a
Comparative Study of Open versus Laparoscopic
Surgery. European urology, 45(3), 346-351.
Turner, P. and Turner, S. 2001. A Web of Contradictions.
Interacting with Computers, 14(1), 1-14.
Tynjälä, P. 2008. Perspectives into Learning at the
Workplace. Educational Research Review, 3(2), 130-
154.
Van de Wiel M., Van den Bossche P., Janssen, S. and
Jossberger, H. 2011. Exploring Deliberate Practice in
Medicine: How do Physicians Learn in the
Workplace? Advances in Health Sciences Education,
16(1), 81-95.
Van Dongen, K. W., Van der Wal, W. A., Rinkes, I. B.,
Schijven, M. P. and Broeders, I. A. M. J. 2008. Virtual
Reality Training for Endoscopic Surgery: Voluntary or
Obligatory? Surgical Endoscopy, 22(3), 664-667.
Van Veelen, M., Nederlof, E., Goossens, R., Schot, C. and
Jakimowicz, J. 2003. Ergonomic Problems
Encountered by the Medical Team Related to Products
Used for Minimally Invasive Surgery. Surgical
Endoscopy and Other Interventional Techniques,
17(7), 1077-1081.
Vygotsky, L. S. 1978. Mind in Society. The development
of Higher Psychological Processes. Harvard
University Press, Cambridge, MA.
Yule, S. 2008. Debriefing Surgeons on Non-technical
Skills (NOTSS). Cognition, Technology and Work,
10(4), 265-274.
Yule, S. and Paterson-Brown, S. 2012. Surgeons’ non-
technical skills. Surgical clinics of North America
92(1), 37-50.
CSEDU2015-7thInternationalConferenceonComputerSupportedEducation
462
