
Towards an Intelligent Triage Bracelet: A Conceptual Study of a
Semi-Automated Prehospital Triage Algorithm and the Integration of
Blood Pressure Measurement
Lorenz Gr
¨
unerbel
a
, Ferdinand Heinrich
b
, Oliver Zett
c
, Kristjan Axelsson
d
and Maximilian Schumann
e
Fraunhofer EMFT, Hansastr. 27d, Munich, Germany
Keywords:
First Responder, Automated Triage System, Mass-Casualty Incident, Blood Pressure Monitoring, AI, Machine
Learning.
Abstract:
First responders often reach their limit when they have to find and triage dozens of victims in a mass-casualty
incident. However, a delay in treatment directly affects the survival chances of seriously injured people. A
method to reduce the time for the prehospital triage could potentially save lives. Hence, this work outlines the
conceptual development of an intelligent bracelet that semi-automates the prehospital triage. This bracelet is
supposed to enable non-professional first responders to help with the triage, which maximises the utilisation
of man power at a mass-casualty incident. The bracelet should automate the part of the triage that is based
on vital, position and movement data and it should guide through the necessary patient interactions. As a step
towards this goal, this work proposes a semi-automated triage algorithm that is based on mSTaRT. One of the
challenges to implement this concept is to measure the blood pressure with a small and easy to attach system.
Therefore, this work presents a wrist worn oscillometric blood pressure measurement prototype. Furthermore,
we discuss the use of machine learning methods to forecast triage level changes.
1 INTRODUCTION
After a mass-casualty incident, such as a train crash or
an environmental disaster, a large number of victims
immediately need emergency treatment. However, of-
ten only a few first responders are quickly available.
Upon arrival, the first responders, with the necessary
training, perform a comprehensive prehospital triage
of all victims to categorize them depending on the
severity of their injuries and consequently define the
order of treatment. It is impossible to immediately
treat everyone. Furthermore, a simultaneous monitor-
ing of all patients is not realizable, hence a sudden
deterioration of a patient’s health can remain unde-
tected.
Innovative technical assistance could accelerate
the triage process, which saves time for victim treat-
a
https://orcid.org/0000-0002-1932-481X
b
https://orcid.org/0000-0002-4626-2394
c
https://orcid.org/0000-0002-4074-9310
d
https://orcid.org/0000-0002-5044-2152
e
https://orcid.org/0000-0002-2528-2492
ment. Additionally, it makes continuous victim mon-
itoring possible. We hypothesize that the right tech-
nical assistance enables first responders without dedi-
cated triage training to perform a semi-automated pre-
hospital triage. Consequently, this would maximize
the utilisation of man power at a mass-casualty inci-
dent.
To develop a semi-automated prehospital triage
concept we first analysed which part of the modified
Simple Triage and Rapid Treatment (mSTaRT) triage
algorithm, as it is shown in the work of Paul et al.
(Paul et al., 2009), can be automated. We believe that
all necessary vital data recordings and the embedded
guidance for first responders should be integrated in a
small, cost-efficient and easy to attach sensor system.
Hence, our proposed solution is an Intelligent Triage
(ITRI) bracelet to be worn at the wrist. The continu-
ous non-invasive acquisition of relevant vital data in
this scenario is difficult. This work focuses on the in-
tegration of wrist worn blood pressure measurement.
The acquired continuous vital data might not only be
used to semi-automate the triage decision, but it might
Grünerbel, L., Heinrich, F., Zett, O., Axelsson, K. and Schumann, M.
Towards an Intelligent Triage Bracelet: A Conceptual Study of a Semi-Automated Prehospital Triage Algorithm and the Integration of Blood Pressure Measurement.
DOI: 10.5220/0011746200003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 1: BIODEVICES, pages 169-176
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
169

be used to forecast deteriorating patient conditions.
2 CURRENT PREHOSPITAL
TRIAGE SYSTEMS
The procedure for a prehospital triage in the case of
a mass-casualty incident (MCI) is defined by national
regulations or laws. In this work we will focus on
the mSTaRT triage algorithm, as it is shown in the
work of Paul et al. (Paul et al., 2009), because the
Bavarian directive about MCIs incorporates a ”Bavar-
ian Model” of the mSTaRT algorithm (Schm
¨
oller and
Hagen, 2017).
The prehospital triage in the event of MCI is or-
ganised as follows: The first arriving paramedic au-
tomatically becomes the operational leader. To es-
timate the number and severity of casualties every
available first responder with dedicated triage train-
ing starts in a team of two with a first comprehensive
triage. Patients with a chance of survival are grouped
in 3 categories: SK 1 (red) - life threatening - imme-
diate care/transport, SK 2 (yellow) - seriously injured
- transport based on urgency, SK 3 (green) - slightly
injured - transport when available. Every patient that
is able to walk is categorised in SK3 (green). If a life
ending injury is present a physician needs to confirm
the death. Every patient that is not able to walk is
assumed to be SK 2 (yellow). If one condition from
a checklist of immediate life threatening conditions
is met the patient is classified as SK 1 (red). This
checklist includes checks for spontaneous breathing,
a reasonable breathing rate, spurting bleeding, radial
pulse and a check whether the patient can execute
simple commands. Patients are marked with paper
triage cards and barrier tape according to their triage
level. Classically the situation overview has to be ag-
gregated manually (Schm
¨
oller and Hagen, 2017; Paul
et al., 2009).
Ideas for how to improve the prehospital triage
with technical aid were already published. In the fol-
lowing the use of vital sensors and the triage automa-
tion incorporated in these systems is recapitulated.
The commercially available system RescueWave
is an electronic replacement for the triage card that is
coupled with an application that tracks and visualizes
severity and position of each patient and also supports
transport organization. No vital data is recorded (Res-
cueWave, 2022).
In the literature multiple advanced electronic
triage tags that enable victim tracking, continuous vi-
tal data monitoring and medical data exchange over
information networks have been presented. The Wire-
less Internet Information System for Medical Re-
sponse in Disasters (WIISARD) limits the use of vi-
tal data to a pulse oximeter (Lenert et al., 2011). The
CodeBlue project focused on the sensor network for
emergency responses and demonstrates vital data ag-
gregation with an exemplary pulse oximeter and a
two-lead electrocardiogram (ECG). The authors ex-
pect that more vital data sensors will be available in
the future (Lorincz et al., 2004). For the Advanced
Health and Disaster Aid Network (AID-N) an elec-
tronic triage tag that integrates a pulse oximeter, blood
pressure arm cuffs and a two-lead ECG was devel-
oped. Vital data is continuously monitored and an
alarm is raised on patient specific thresholds (Gao
et al., 2007). The authors of the AID-N network point
out that an arm cuff to measure non-invasive blood
pressure has to be attached properly to deliver accu-
rate sensor reading which might be challenging with
clothed patients. Furthermore, the cuff adds extra ma-
terial cost and makes the system much larger (Gao
et al., 2006).
Automation of the triage decision based on elec-
tronic triage tags has also been studied in the litera-
ture. The eTriage tag comes in a version that mea-
sures blood oxygen saturation (SpO2) and heart rate
with a pulse oximeter and an extended version that
additionally measures the breath rate via a nasal can-
nula. The triage category can either be manually set
by the triage officer or in a simple triage mode the
priority is deduced from heart rate and SpO2 thresh-
old values (Sakanushi et al., 2013). A Korean elec-
tronic triage system measures the heart rate, the SpO2
and the respiratory rate with a pulse oximeter. Ad-
ditional information including the body temperature,
the blood pressure, the consciousness of the patient
and the walking ability can be set by a first responder
via a mobile app. The triage category is automatically
determined based on a checklist of combined patient
conditions (Park, 2021). One German triage tag in-
troduced the concept of pre triage levels as a general
and simple reference. To determine these pre triage
levels accelerometer-based activity classification dif-
ferentiates walking patients, i.e. minor affected, and
lying or sitting patients, i.e. major effected. Addition-
ally, a pulse oximeter records the SpO2 as well as the
heart rate and thresholds for triage levels are defined.
During real emergencies it was found that especially
minor affected patients tend to temporally stop mov-
ing without clinical relevant reasons, which hindered
the detection of minor affected patients based on ac-
tivity classification. The vital data based triage clas-
sification was better at identifying the minor affected
patients but struggled to clearly identify the major af-
fected ones (Rodriguez et al., 2014).
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
170
3 PROPOSED PREHOSPITAL
TRIAGE SYSTEM
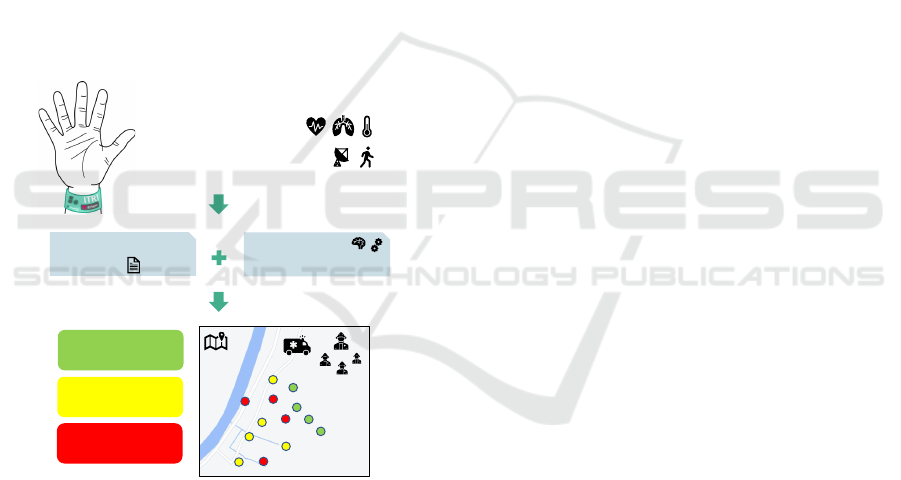
We envision an intelligent triage system that utilizes
the available man power at a mass-casualty incident
by enabling first responders without explicit triage
training to perform the prehospital triage. Therefore,
we introduce the concept of an easily attachable Intel-
ligent Triage (ITRI) bracelet that records vital, posi-
tion as well as movement data and features embedded
triage guidance. With this system patients could be
monitored continuously to detect condition changes.
Additionally, machine learning methods could fore-
cast triage category changes. The location of all pa-
tients could be shown on a central device with an
overview map to give the operations manager a clear
situation picture. Figure 1 displays a schematic rep-
resentation of this system. It would allow the first
responders to monitor the whole mass-casualty event
well-arranged and continuously over the total first aid
intervention period.
AI methods:
condition forecasting
vital data
slightly injured
SK III
seriously injured
SK II
life-threatening
SK I
semi automated triage:
ITRI mSTaRT
position and movement
Figure 1: ITRI-system vision: The ITRI bracelet records
vital data as well as position and movement data. Based
on this data the triage levels are determined with a semi-
automated algorithm, which is based on mSTaRT. AI meth-
ods are used to forecast condition changes. On a central
device the health state of all patients during a mass-casualty
incident can be monitored.
3.1 Prehospital Triage Algorithm
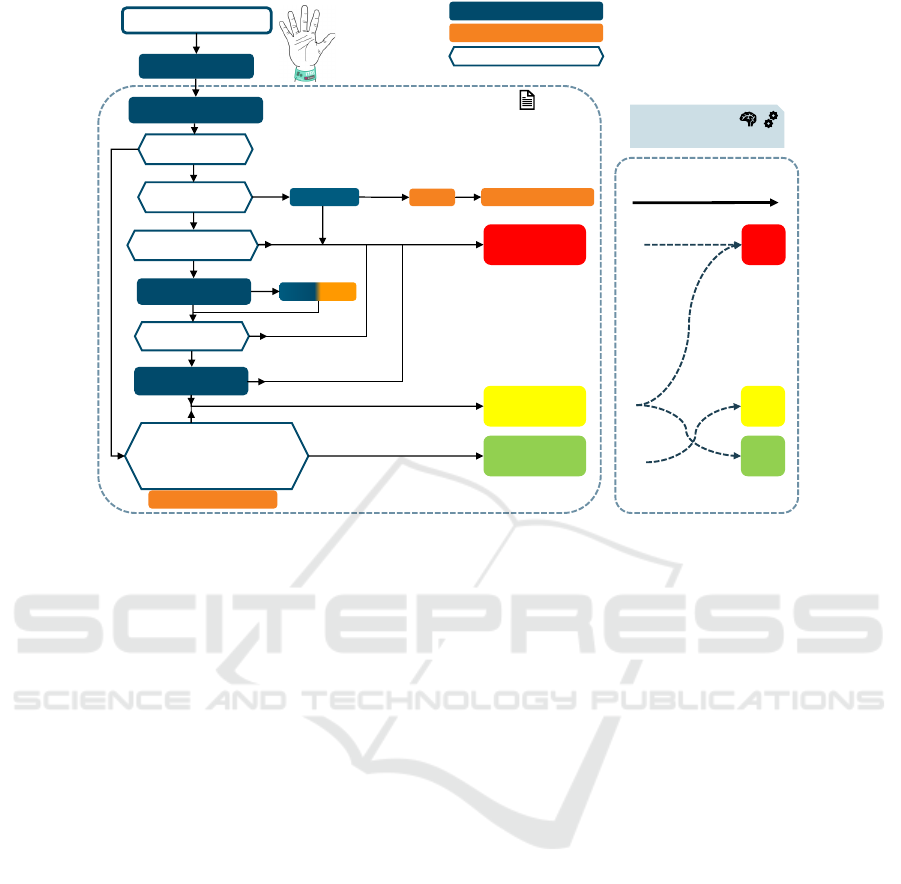
As argued before, the semi-automated prehospital
triage algorithm of the ITRI bracelet will be based on
the mSTaRT algorithm (Paul et al., 2009). We iden-
tified the parts of the mSTaRT scheme which might
be automated with vital sensor or position and move-
ment data and show the resulting triage classification
scheme in Figure 2. After attaching the ITRI bracelet,
the first triage decision depends on the patient’s abil-
ity to walk to a collection point. This can be su-
pervised by GPS in combination with accelerometer-
based movement detection. At the collection point a
critical finding checklist is assessed. Besides checks
that have to be conducted by a medical expert, the
list also includes threshold values for the respiratory
rate, the SpO2 and the systolic blood pressure. Pa-
tients that are not able to walk are tested for sponta-
neous breathing. The check for spontaneous breath-
ing as well as the respiratory rate can be deduced from
a pulse oximeter. If no spontaneous breathing is de-
tected, the first responder should clear the airways.
When the life-saving measure is not successful a med-
ical expert has to be called to the site to determine the
chances of survival with the help of an electrocardio-
gram. Next, the respiratory rate is checked. Detec-
tion of squirting bleeding is not recognizable with vi-
tal sensor data. Thus, the ITRI system needs a user
interface, which asks the first responder to check for
squirting bleeding and an option to send for a med-
ical expert if necessary. Next the presence of radial
pulse is assessed. Lastly the system needs to inter-
act with the first responder to test the consciousness
of the patient, for example with a simple movement
instruction.
The necessary user interface between the first re-
sponder and the ITRI system, which might be a com-
bination of speech commands and buttons for user
feedback, is outside the scope of this work. As dis-
cussed in section 2 the necessary hard- and software
for victim tracking has been addressed in the liter-
ature. Furthermore, the feasibility to use a pulse
oximeter to obtain SpO2, the heart rate as well as
the respiratory rate have been shown. A two-lead
electrocardiogram has also been integrated in elec-
tronic triage tags already. In the classic mSTaRT the
use of an electrocardiogram is limited to the deter-
mination of death. ECG readings might be helpful
for continuous patient monitoring, but the attachment
of an ECG also takes a relatively long time. The
systolic blood pressure is a vital parameter used in
the critical finding check list, but an automated mea-
surement with an arm cuff has practical limitations.
Therefore, this work focuses on a concept for a wrist
worn non-invasive intermittent blood pressure mea-
surement. Additionally, such a system would also be
able to detect and quantify the radial pulse.
3.1.1 Potential Triage Forecasting
As outlined on the right side of Figure 2 the con-
tinuous recording of vital sensor data in combination
Towards an Intelligent Triage Bracelet: A Conceptual Study of a Semi-Automated Prehospital Triage Algorithm and the Integration of
Blood Pressure Measurement
171
AI methods:
condition forecasting
now
+10 min
ITRI mSTaRT
mass-casualty incident
attach ITRI bracelet
send to collection point
slightly injured
SK III
seriously injured
SK II
life-threatening
SK I
walks to
collection point
SK III
SK II
SK I
spontaneous
breathing
first responder interaction
legend:
ITRI automated decision
respiratory rate
RR > 30/min or <10/min
spurting bleeding
radial pulse
simple movement
instruction
clear airways
critical finding checklist
(vital data):
- RR > 30/min or <10/min
- SPo2 < 90%
- syst. blood pressure < 90mmHg
yes
no
no
yes
yes
no
yes
no
no
yes
medical expert interaction
stop bleeding
movement not recognized
movement recognized
spontaneous
breathing
no spontaneous
breathing
determination of death
Other critical findings
ECG
Figure 2: Proposed semi-automated prehospital triage scheme which is based on data from the ITRI-bracelet and is supposed
to be performed by non professional first responders.
with available static patient data could be used to fore-
cast the triage status with machine learning methods.
This can improve the continuous monitoring of pa-
tients, because the medical experts can focus on pa-
tients with worsening conditions. A challenge for the
development of machine learning algorithms is the
scarcity of available data: Data from mass-casualty
incidents is difficult to obtain, because these incidents
happen relatively rare and complete documentation is
not guaranteed. Additionally, no continuous monitor-
ing of vital signs is currently used.
In the literature, studies with static data from a
pre-hospital setting or clinical daily routine suggest
that the triage could be improved with machine learn-
ing models. One retrospective study with data from
two emergency departments took vital signs, the chief
medical complaint and active medical history to pre-
dict likelihood of acute outcomes. Compared with
the emergency severity index the proposed random
forest model showed superior results. (Levin et al.,
2018) Another study analysed data in two regions in
the Netherlands to improve pre-hospital triage. The
study identified eight significant predictors based on
clinical reasoning and built a regression model to pre-
dict whether a patient is severely injured and thus
needs to be transported to a higher level trauma cen-
ter. The authors also present a mobile app that advises
to which trauma center a patient should be transported
(van Rein et al., 2019).
When continuous vital data is available, machine
learning methods for times series data are applica-
ble. The PhysioNet/Computing in Cardiology Chal-
lenge 2012 challenged participants to predict the in-
hospital mortality of intensive care unit patients based
on five general static descriptors and 36 time series of
vital signs and laboratory results. Multiple methods
of competitors have shown to obtain significantly bet-
ter scores compared to a classic acuity score baseline
algorithm. Beside the conventional logistic regres-
sion other model architectures like support vector ma-
chines, neural networks, random forests and ensem-
ble learning methods were used by participants (Silva
et al., 2012). This challenge was based on the MIMIC
data set. This data set is recorded at critical care units
of the Beth Israel Deaconess Medical Center and the
newest version is organised in modules that reflect the
provenance of the data. For potential triage forecast-
ing algorithms the emergency department and inten-
sive care unit modules are the most relevant (MIMIC,
; Johnson et al., 2022).
To potentially integrate machine learning models
trained on clinical data into the ITRI bracelet one
has to use transfer learning techniques. For this use
case differences in vital data sensors and sample rates
as well as inhomogeneous patient populations pro-
pose challenges. Lastly, a validation with real mass-
casualty incident data is indispensable.
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
172

3.2 Blood Pressure Measurement
The blood pressure (BP) readings have to be non-
invasive and enable automated intermittent monitor-
ing during the whole duration of an emergency re-
sponse. The selected approach is the oscillometric
measurement method. This method is in widespread
clinical and ambulatory use for automated cuff based
BP measurement systems, that either measure at the
arm or at the wrist.
3.2.1 Oscillometric Measurement Principle
The automated oscillometric BP measurement with
electronic readout via a pressure sensor is based on
the work of Ramsey (Ramsey, 1979). The typical
measurement principle is well described by Sharman
et al. (Sharman et al., 2022) and consists of the fol-
lowing steps: A pneumatic cuff with an integrated
pressure sensor is placed around the arm and inflated
to a pressure greater than the systolic blood pres-
sure. Then the cuff is deflated and the pressure sensor
records the pressure decrease overlayed with a pul-
satile component, i.e. the pulse waves. These pulse
waves result from the pulsatile heartbeat and can be
analysed separately after high pass filtering. During
the cuff pressure decrease the pulse wave amplitudes
first increase sharply when the cuff pressure is near
the systolic BP, then the amplitudes reach a maximum
when the cuff pressure is equivalent to the mean arte-
rial BP and for even lower cuff pressure the amplitude
of the pressure waves decrease again. The recorded
pulse waves during the cuff pressure decrease is called
the oscillometric waveform and the approximation of
their amplitude change is called the oscillometric en-
velope. The cuff pressure at which the oscillometric
envelop is maximal is equivalent to the mean arte-
rial BP. The systolic BP is typically estimated to be
the cuff pressure at the rising site of the oscillometric
envelope at about 50% (range 45–73%) of the maxi-
mal amplitude. Equivalently the diastolic BP is typ-
ically estimated to be the cuff pressure at the falling
site of the oscillometric envelope at about 70% (range
69–83%) of the maximal amplitude (Sharman et al.,
2022).
The oscillometric measurement method has some
known drawbacks. The placement of the device rela-
tive to the heart can alter the BP measurement due to
hydrostatic pressure effects. During the measurement
the patients should not move. Conventional oscillo-
metric BP measurements are known to underestimate
systolic BP (Sharman et al., 2022). Differences of ar-
terial stiffness, which for example can be observed in
elderly or diabetic patients, also influence the accu-
racy of the measurements (van Montfrans, 2001). It
remains to be evaluated if these drawbacks prevent the
usage of the oscillometric method.
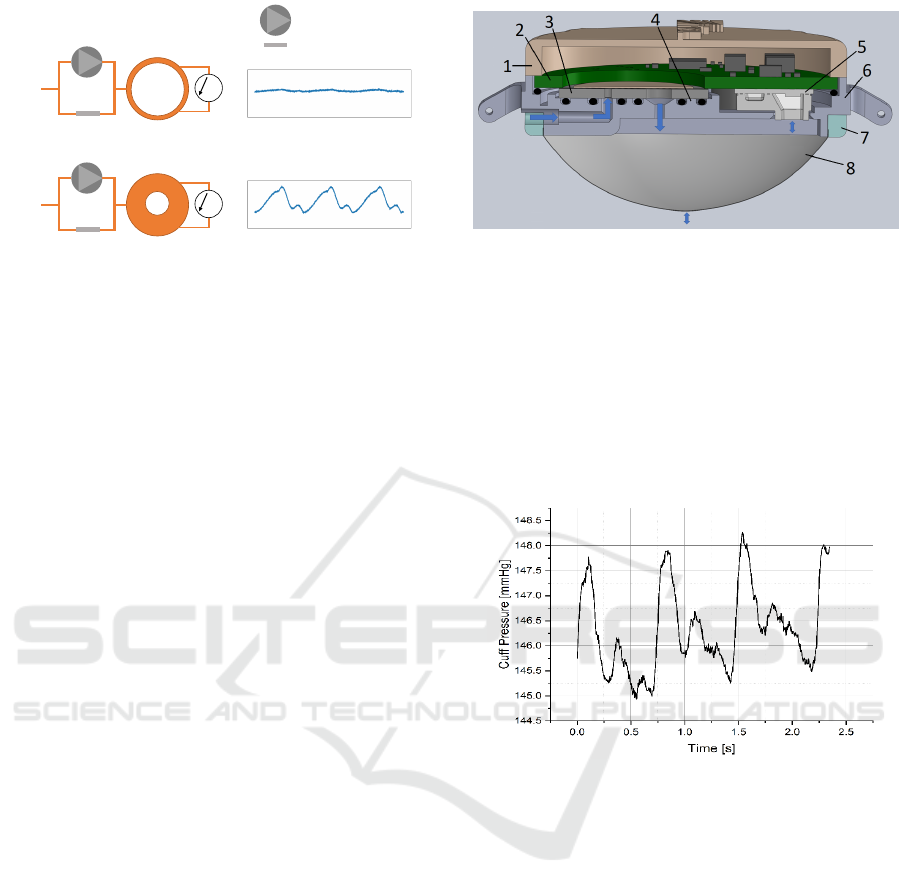
3.2.2 System Implementation
The BP measurement component should be a small
and lightweight system that is comfortable to wear
and easy to use.
Generating a varying cuff pressure with a pre-
cise resolution on a small footprint is a challenging
task that can be solved with micropumps. We pro-
pose the use of piezoelectric micropumps to combine
high pressure generation (25 kPa), large enough flow
rates (50 ml/ min), a relative low power consump-
tion (<300 mW) as well as a small system size (Ø
20 mm x 2.1 mm) (Bußmann et al., 2021b; EMFT
Steel Pumps, ). The operating principle is based on
the indirect piezoelectric effect that describes the me-
chanical deformation of a material due to an applied
electric field. The actuator is a piezoceramic, be-
cause this material exhibits a strong piezoelectric ef-
fect. An alternating voltage at the piezoceramic ac-
tuator leads to its extraction and contraction, which
bends the metal diaphragm it is glued on. The bending
displaces the volume inside the pump chamber and
moves the fluid according to the two integrated pas-
sive check valves (Bußmann et al., 2021a). Figure 3
presents the schematic layer-stack of a metal microp-
ump that can be used to generate the cuff pressure.
Figure 3: Diaphragm micropump consisting of four layers:
Body plate with holes, two valve sheets in the middle, and
an actuator with a piezoelectric element on top.
In Figure 4 a schematic representation of the com-
plete fluidic setup is shown. The piezoelectric mi-
cropump fills the cuff with environmental air to gen-
erate the required cuff pressure. An integrated pres-
sure sensor is used to measure the cuff pressure and
the pulse waves. A flow restriction with a high flu-
idic resistance in parallel to the micropump acts as
a over-pressure protection and pressure relief. Since
the cuff pressure is directly controlled by the actua-
tion frequency of the micropump the pressure build
up can be precisely controlled. This enables to mea-
sure the oscillometric waveform during the pressure
build up.
Towards an Intelligent Triage Bracelet: A Conceptual Study of a Semi-Automated Prehospital Triage Algorithm and the Integration of
Blood Pressure Measurement
173
2. pressure cuff inflated
flow restriction
1. pressure cuff deflated
environment
∆p
micropump
∆p
environment
pressure
time
pressure
time
Figure 4: Fluidic principle of proposed oscillometric blood
pressure measurement method (figure taken from (Gruener-
bel, 2022)).
Our design does not use a complete cuff, but
a pressurised area that is fixated to the wrist by a
bracelet. During system design a proper placement
of the pressurised area with its center above an artery
is ensured as suggested for the centre of an arm cuff
by Petrie et al. (Petrie et al., 1986). Furthermore,
we apply a pressurised area that is large enough to
ensure good signal quality but still comes with a rea-
sonable filling time. Figure 5 shows the current state
of the housing and the integrated electronics of the
BP measurement bracelet. The Housing consists of
three 3D-printed parts, which are manufactured us-
ing stereo lithography. The 100 µm thick thermoplas-
tic polyurethane foil at the bottom of the housing is
pressed against the housing base with a ring. Addi-
tionally the foil is glued to the housing base. The ring
fixating the elastic foil and the upper housing lid are
pulled together with four screws. The rubber seals be-
tween the micropump and the housing base are com-
pressed when the upper housing lid presses down on
the printed circuit board, pushing the micropump in
the housing base. To make silicon sealing easier, a
chamber is positioned at the pressure sensor opening.
The fluidic channels are printed directly into the hous-
ing base. The air inlet is positioned opposite the wrist
strap mounting arms so that it will be hidden behind
the wrist strap to prevent unintentional blocking of the
inlet. A rubber wrist strap that is commercially avail-
able is used.
3.2.3 Feasibility Study - Results
The introduced BP monitoring system is tested in
an early feasibility study. Therefore, a test person
wears the bracelet. As soon as the applied pressure
is high enough, the pulse waves become visible. An
exemplary pulse wave recording is shown in Figure
6. The y-axis represent the measured pressure inside
the pressurised area. The pressure pulses can be dis-
tinguished clearly. It should be feasible to calculate
Figure 5: Cross section of the blood pressure monitoring
bracelet with: 1) housing lid, 2) PCB with electronics, pres-
sure sensor and contact pad for micropump, 3) the metal
micropump, 4) rubber sealings, 5) a pressure sensor, 6) the
outer housing with integrated fluid channels, 7) a fixture for
the elastic foil, 8) the elastic foil, i.e. the pressurised area.
the mean arterial blood pressure and estimate the sys-
tolic and diastolic blood pressure using the algorithm
for the oscillometric method described in section 3.2.
Additionally, the sensor readings can be used to quan-
tify the radial pulse and the heart rate.
Figure 6: Exemplary measurement of blood pressure pulses
acquired with the presented demonstrator.
4 CONCLUSION
It was analysed which part of the mSTaRT algorithm
can be automated to potentially enable all first respon-
ders to perform a semi-automated prehospital triage.
As a step towards integrating all necessary vital data
sensors a small, cost-efficient and easy to attach pro-
totype of an oscillometric blood pressure monitoring
bracelet was designed and build. Measurements with
the demonstrator show promising raw sensor value
readings with clearly identifiable pressure pulses. The
exact algorithm to determine the oscillometric enve-
lope and the calculation of the systolic and diastolic
blood pressure values remains to be defined. The
blood pressure reading must than be verified with, ei-
ther an intra-arterial measurement or the classic aus-
cultatory method with a sphygmomanometer.
The integration of all other vital data sensors, the
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
174

position determination, the movement detection, the
embedded triage guidance together with the user in-
terface of the bracelet as well as the central situation
overview still have to be designed.
The integration of machine learning to forecast
possible triage status changes is an interesting re-
search topic. In both prehospital and clinical settings
data based triage models show promising results. A
prehospital triage forecasting model based on time
series data can only be developed after it was deter-
mined which vital data can be measured continuously
during a prehospital triage.
The effectiveness of an electronic triage system
can only be validated with emergency drills or even
better with real emergency situations. Especially
our assumption that first responders without spe-
cific triage training are enabled to perform a semi-
automated prehospital triage has to be verified this
way. Additionally, in the same manner, the validity
of the proposed blood pressure measurement method
must be confirmed.
REFERENCES
Bußmann, A. B., Durasiewicz, C. P., Kibler, S. H. A., and
Wald, C. K. (2021a). Piezoelectric titanium based
microfluidic pump and valves for implantable medi-
cal applications. Sensors and Actuators A: Physical,
323:112649.
Bußmann, A. B., Gr
¨
unerbel, L. M., Durasiewicz, C. P.,
Thalhofer, T. A., Wille, A., and Richter, M. (2021b).
Microdosing for drug delivery application—a review.
Sensors and Actuators A: Physical, 330:112820.
EMFT Steel Pumps. Stainless steel micropumps for
medical-, laboratory and analysis technology.
https://www.emft.fraunhofer.de/content/dam/emft/
emft-neu/deutsch/dokumente/infoblatt-stainless-
steel-micropumps-medical-laboratory-analysis-
technology-fraunhofer-emft.pdf. Accessed: 2023-01-
02.
Gao, T., Massey, T., Bishop, W., Bernstein, D., Selavo,
L., Alm, A., White, D., and Sarrafzadeh, M. (2006).
Integration of triage and biomedical devices for con-
tinuous, real-time, automated patient monitoring. In
2006 3rd IEEE/EMBS International Summer School
on Medical Devices and Biosensors, pages 34–39.
Gao, T., Massey, T., Selavo, L., Crawford, D., Chen, B.-
r., Lorincz, K., Shnayder, V., Hauenstein, L., Dabiri,
F., Jeng, J., Chanmugam, A., White, D., Sarrafzadeh,
M., and Welsh, M. (2007). The advanced health and
disaster aid network: A light-weight wireless medical
system for triage. IEEE Transactions on Biomedical
Circuits and Systems, 1(3):203–216.
Gruenerbel, L. (2022). Experimental and theoretical
methodologies for high-flow optimization of microp-
umps in medical applications. Dissertation (not pub-
lished yet), page 165.
Johnson, A., Bulgarelli, L., Pollard, T., Horng, S., Celi,
L. A., and Mark, R. (2022). Mimic-iv. https://
physionet.org/content/mimiciv/2.0/. Accessed: 2022-
11-16.
Lenert, L. A., Kirsh, D., Griswold, W. G., Buono, C., Lyon,
J., Rao, R., and Chan, T. C. (2011). Design and eval-
uation of a wireless electronic health records system
for field care in mass casualty settings. Journal of the
American Medical Informatics Association : JAMIA,
18(6):842–852.
Levin, S., Toerper, M., Hamrock, E., Hinson, J. S., Barnes,
S., Gardner, H., Dugas, A., Linton, B., Kirsch, T., and
Kelen, G. (2018). Machine-learning-based electronic
triage more accurately differentiates patients with re-
spect to clinical outcomes compared with the emer-
gency severity index. Annals of Emergency Medicine,
71(5):565–574.e2.
Lorincz, K., Malan, D. J., Fulford-Jones, T., Nawoj, A.,
Clavel, A., Shnayder, V., Mainland, G., Welsh, M.,
and Moulton, S. (2004). Sensor networks for emer-
gency response: Challenges and opportunities. IEEE
Pervasive Computing, 3(4):16–23.
MIMIC. The medical information mart for intensive care.
https://mimic.mit.edu/. Accessed: 2022-11-16.
Park, J. Y. (2021). Real-time monitoring electronic
triage tag system for improving survival rate in
disaster-induced mass casualty incidents. Healthcare,
9(7):877.
Paul, A. O., Kay, M. V., Huppertz, T., Mair, F., Dierking,
Y., Hornburger, P., Mutschler, W., and Kanz, K.-G.
(2009). Validierung der vorsichtung nach dem mstart-
algorithmus: Pilotstudie zur entwicklung einer multi-
zentrischen evaluation. Der Unfallchirurg, 112(1):23–
30, 32.
Petrie, J. C., O’Brien, E. T., Littler, W. A., and de Swiet,
M. (1986). Recommendations on blood pressure mea-
surement. Br Med J (Clin Res Ed), 293(6547):611–
615.
Ramsey, M. (1979). Noninvasive automatic determination
of mean arterial pressure. Medical & biological engi-
neering & computing, 17(1):11–18.
RescueWave (2022). Digitale sichtungskarte f
¨
ur manv.
https://rescuewave.de/. Accessed: 2022-06-29.
Rodriguez, D., Heuer, S., Guerra, A., Stork, W., Weber, B.,
and Eichler, M. (2014). Towards automatic sensor-
based triage for individual remote monitoring during
mass casualty incidents. undefined.
Sakanushi, K., Hieda, T., Shiraishi, T., Ode, Y., Takeuchi,
Y., Imai, M., Higashino, T., and Tanaka, H. (2013).
Electronic triage system for continuously monitoring
casualties at disaster scenes. Journal of Ambient Intel-
ligence and Humanized Computing, 4(5):547–558.
Schm
¨
oller, G. and Hagen, F. (2017). Sichtung und vorsich-
tung bei massenanfall von verletzten und erkrankten.
retten!, 6(05):372–381.
Sharman, J. E., Tan, I., Stergiou, G. S., Lombardi, C., Sala-
dini, F., Butlin, M., Padwal, R., Asayama, K., Avolio,
A., Brady, T. M., Murray, A., and Parati, G. (2022).
Automated ’oscillometric’ blood pressure measuring
Towards an Intelligent Triage Bracelet: A Conceptual Study of a Semi-Automated Prehospital Triage Algorithm and the Integration of
Blood Pressure Measurement
175

devices: how they work and what they measure. Jour-
nal of Human Hypertension, pages 1–8.
Silva, I., Moody, G., Scott, D. J., Celi, L. A., and Mark,
R. G. (2012). Predicting in-hospital mortality of icu
patients: The physionet/computing in cardiology chal-
lenge 2012. Computing in cardiology, 39:245–248.
van Montfrans, G. A. (2001). Oscillometric blood pressure
measurement: progress and problems. Blood pressure
monitoring, 6(6):287–290.
van Rein, E. A. J., van der Sluijs, R., Voskens, F. J., Lansink,
K. W. W., Houwert, R. M., Lichtveld, R. A., de Jongh,
M. A., Dijkgraaf, M. G. W., Champion, H. R., Beeres,
F. J. P., Leenen, L. P. H., and van Heijl, M. (2019).
Development and validation of a prediction model for
prehospital triage of trauma patients. JAMA Surgery,
154(5):421–429.
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
176
