
Implementing an Intersectoral Telemedicine Network in Rural Areas:
Evaluation from the Point of View of Telemedicine Users
Domenic Sommer
a
, Sebastian Wilhelm
b
, Diane Ahrens
c
and Florian Wahl
d
Deggendorf Institute of Technology, Technology Campus Grafenau, Hauptstrasse 3, 94566 Grafenau, Germany
{domenic.sommer, sebastian.wilhelm, diane.ahrens, florian.wahl}@th-deg.de
Keywords:
Telemedicine, Remote Medicine, Delivery of Healthcare, Ehealth, Rural Health, Germany.
Abstract:
Telemedicine (TMed) is becoming popular due to the growing number of elderly and the shortage of health-
care workers. In Germany, TMed is rarely part of rural healthcare, and the research state is limited. To
improve healthcare and to research the conditions under which TMed can be used in German rural areas, an
intersectoral, TMed network was set up from July 2018 to Oct. 2020 and evaluated with mixed methods, in-
cluding qualitative interviews and quantitative feedback forms. Seven Use-Cases (UCs) were implemented in
the dimensions: (i) home visits (n = 170), (ii) patient video consultation (n = 30), (iii) intensive care (n = 15),
(iv) mountain accident (n = 6), (v) wound management (n = 6), (vi) caregiver video consultation (n = 3) and
(vii) electronic health record (n = 10). Our study indicates that digitally supported general practitioner (GP)-
home visits and intensive care are the most frequent UCs. TMed is satisfactory and leads to advantages for
rural healthcare. However, vital data transmission and the electronic health record (eHR) were less in demand
due to high preparation efforts. Findings from previous studies can be confirmed. Facilitators for TMed who
should be considered and further researched are: training on digital literacy including awareness-rising, fi-
nancing, cross-institutional documentation, and suitable mobile network infrastructure.
1 INTRODUCTION
European Challenges. Increasing multi-morbidity
and treatments for chronic diseases in an aging soci-
ety in Western Europe are putting pressure on health
systems. In Germany, one in five people is over 65
years of age (Dudel, 2018, p. 5), and rising life ex-
pectancy leads to an increase in the number of elderly
requiring treatment in Europe (European Parliament,
2021). There are several challenges Health Service
Providers (HSPs) face: (i) disciplines become more
specialized, (ii) services get increasingly fragmented,
(iii) overall complexity is increasing and (iv) no inef-
ficiencies can be afforded due to the shortage health-
care workers (HCWs) (Valentijn et al., 2013; Hack-
mann and Moog, 2010; Tsiasioti et al., 2020).
Rural Challenges. Equal opportunities between ur-
ban and rural areas and the same access to health
services are a priority for many European countries
a
https://orcid.org/0000-0002-2581-513X
b
https://orcid.org/0000-0002-4370-9234
c
https://orcid.org/0000-0001-9905-7442
d
https://orcid.org/0000-0002-1163-1399
(Weingarten and Steinf
¨
uhrer, 2020). Many rural gen-
eral practitioner (GP) vacancies won’t be filled in
the future because there often is no succession plan-
ning (Kopetsch, 2010; Laschet, 2019). Another chal-
lenge is that young people are the backbone of rural
development, but due to urbanization, they are miss-
ing in rural healthcare jobs, and the role of informal
caregiver remains unfilled (Hennig, 2019). Therefore,
the rural elderly are increasingly dependent on profes-
sional health and care services in rural regions (Bay-
erisches Landesamt f
¨
ur Statistik, 2019b).
In rural areas, there is a shortage of rural
HCWs and conversely a high demand for health ser-
vices (Hackmann and Moog, 2010; Tsiasioti et al.,
2020). In addition, a large portion of work time
of HCWs is spent on not direct patient care tasks
(e.g., administration or travel). Some German re-
gions are sparsely populated with, e.g., 80 residents
per km
2
, and travel times for home visits or clinic ad-
missions take longer than in cities (Bayerisches Lan-
desamt f
¨
ur Statistik, 2019a, p. 14). The fact that ru-
ral HSPs travel long distances to visits or examina-
tions (e.g., vital parameter checks) is costly, ineffec-
tive and reduces the attractiveness of the health pro-
fession (Meyer, 2020). In addition, not only obtaining
Sommer, D., Wilhelm, S., Ahrens, D. and Wahl, F.
Implementing an Intersectoral Telemedicine Network in Rural Areas: Evaluation from the Point of View of Telemedicine Users.
DOI: 10.5220/0011755500003476
In Proceedings of the 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2023), pages 15-27
ISBN: 978-989-758-645-3; ISSN: 2184-4984
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
15

timely care is critical, even the time for patient care is
reduced as well as medical and paramedical staff are
burdened. The patient’s situation is similar because
mobility is reduced with increasing age and house
visits have capacity bottlenecks. Furthermore, they
often have to deal with a lack of specialist support
in close vicinity, which makes it difficult to get treat-
ment for complex conditions without traveling longer
distances (L
¨
offler et al., 2021). Treatment delays can
lead to worse health outcomes (Meyer, 2020).
TMed as a Solution. Telemedicine (TMed) is us-
ing medical data exchange from distinct locations via
electronic communication to improve patient’s health
and bridge distances (Schwab, 2020). Since COVID-
19, protecting vulnerable patients from infections has
become more important in rural areas, where the
loss of personnel becomes directly noticeable (Kn
¨
orr
et al., 2022). In rural areas, HSPs serve a remarkably
vital role in the care of their communities, and TMed
can contribute to infection protection. TMed even has
the potential to close the gap in healthcare access and
alleviate disparities between rural and urban health-
care delivery.
Research Focus. The main contribution is to show
how TMed in german rural areas can improve health
care. Contrary to prior studies, our applied study
presents a multisided picture of rural TMed, uncov-
ers barriers, and shows how individual TMed applica-
tions fit into a bigger intersectoral network.
The remaining paper is structured as follows: We re-
view the current literature on rural TMed in Section 2,
highlighting the existing barriers and research gaps.
In Section 3, we present how we established an in-
tersectoral TMed network (Subsection 3.1) and eval-
uated it (Subsection 3.2). The results are presented in
Section 4. The paper ends with a discussion in Sec-
tion 5, a conclusion, and an outlook in Section 6.
2 RELATED WORK
The scientific community dealt with TMed and tel-
erehabilitation, focusing on mental health, home care,
primary care, and emergencies (Butzner and Cuf-
fee, 2021; Speyer et al., 2018). Plenty of re-
search even focused on teleconsultation as a techni-
cal application for communication between profes-
sionals and patients (Yamano et al., 2022). Due to
COVID-19, the publication record has increased sig-
nificantly (Mbunge et al., 2022; S¸ahin et al., 2021).
2.1 International Perspective
Regarding international studies, much of the applied
science is being carried out in emerging, and develop-
ing countries since TMed usually represents the only
care option here. For example, in the Himalayan re-
gion, patients were provided with TMed (treatment
and health education) in their homes and rural care
centers because of a rural physician shortage (Amatya
et al., 2022; Ganapathy et al., 2019).
Outcomes and Effects. Most high-level TMed
evidence focus on clinical outcomes and cost-
effectiveness, with findings that TMed is at least as
effective as standard care and can reduce costs for pa-
tients as well as HSPs (Speyer et al., 2018; Zhang
et al., 2022b; Butzner and Cuffee, 2021). The cost-
benefit analysis is complex since TMed first requires
investments and pay off later (Goharinejad et al.,
2021). Eliminating the need for travel, TMed can help
reduce the cost of care for patients and HSP (Zhang
et al., 2022a). TMed is also convenient, and patients
often recommend it to others (Sekhon et al., 2021).
Furthermore, TMed advantage people with limited
mobility or social isolation (Banbury et al., 2018).
The outcome of TMed is greater than saving time
and costs in overall care. TMed offers versatile op-
portunities for elderly, multimorbid, and mobility-
impaired people and can compensate for dispari-
ties (Batsis et al., 2019). Teleconsultations can pre-
ventively avoid hospital admissions and thus a high
burden on patients due to a new environment and
starting treatment too late (Batsis et al., 2019). In
particular, the connection of medical devices, such as
an ECG or wearables, can monitor health status and
complement existing care (Yamano et al., 2022).
There are several advantages to TMed in rural ar-
eas, including the (i) ability to reach underserved pop-
ulations (better healthcare access), (ii) the provision
of care at a lower cost and (iii) the potential to im-
prove clinical outcomes (Haleem et al., 2021). The
most obvious TMed benefit is the reduction of infec-
tion risks and increased protection against COVID-19
in fragmented health care (Mbunge et al., 2022). Fur-
ther, patient satisfaction with TMed is good, and pa-
tients accept them (Sekhon et al., 2021; Batsis et al.,
2019). HCW also show overall satisfaction, accep-
tance and see opportunities for better relationships
with patients (Odendaal et al., 2020). TMed also
transforms the work of HCWs, creating flexibility and
better coordination in care so that resource utilization
can be improved (Butzner and Cuffee, 2021).
Outcomes depend on applications and clinical pic-
ture: In diabetes, an improvement in blood glucose
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
16

control and self-management of health can be ob-
served (Zhang et al., 2022a). TMed also has psy-
chological effects, reducing negative emotions and
enhancing medication adherence (Ma et al., 2022).
TMed also decreases hospital admissions and severe
adverse effects (Batsis et al., 2019). Many exist-
ing studies are biased and consider only one specific
disease (Batsis et al., 2019), although society gets
more multimorbid (The American Geriatrics Society,
2012). This raises the question about the transferabil-
ity of existing studies, shown in Table 1.
Table 1: International evidence on TMed in rural areas.
Findings of Reviews Source
Better or comparable
outcomes (TMed &
face-to-face)
(Goharinejad et al.,
2021; Batsis et al.,
2019; S¸ahin et al.,
2021; Speyer et al.,
2018)
Decreased direct and
indirect costs for pa-
tient & health service
(Butzner and Cuffee,
2021; Haleem et al.,
2021; Speyer et al.,
2018; Zhang et al.,
2022b)
Better resource alloca-
tion & staff relief
(Butzner and Cuffee,
2021)
Satisfaction and accep-
tance by patients &
healthcare workers
(Sekhon et al., 2021;
Butzner and Cuffee,
2021; Mbunge et al.,
2022)
Outcomes are limited
due to heterogeneity:
rural areas need further
research
(Butzner and Cuffee,
2021; Speyer et al.,
2018; Yamano et al.,
2022; Banbury et al.,
2018; Batsis et al.,
2019; S¸ahin et al.,
2021)
Barriers and Facilitating Factors. The main barri-
ers to implementing TMed in rural areas are: (i) lack
of infrastructure, (ii) limited resources and (iii) lack of
provider training. To provide remote access to medi-
cal care, TMed requires a reliable internet connection
in remote areas. While most of the population has ac-
cess to broadband internet, the picture is switching for
mobile applications in rural areas, where connectiv-
ity gaps exist (Baake and Mitusch, 2021). Insufficient
mobile connectivity makes it difficult to provide or re-
ceive care via TMed. In addition, emerging and devel-
oping countries struggle with affordable internet con-
nection and electricity isn’t always available (Oden-
daal et al., 2020). However, the reliability of solu-
tions is especially (esp.) important when consulting
emergencies (Yamano et al., 2022). In this context,
technical support is important. Furthermore, the in-
teroperability of TMed solutions, esp. a unified elec-
tronic health record (eHR), will determine the success
or failure of TMed (Haleem et al., 2021).
Time must be invested first to find and train the
resources needed for TMed deployment. Similarly,
the training of health workers is quite important in
this context, and the solutions must be user-friendly
and integrate with existing systems (Odendaal et al.,
2020). Accessibility can be essential because hear-
ing problems or sign language can be a problem for
current TMed (S¸ ahin et al., 2021).
The Chochrane Library revealed that concerns ex-
ist in the form of supervision, threatening one’s com-
petence, and fears of being overworked and deperson-
alized (Odendaal et al., 2020). These should be ad-
dressed to promote TMed. Digital literacy is limited
in some cases. For successful TMed deployment, user
training and guidance were needed (Banbury et al.,
2018). Also, concerns exist about the reliability of
TMed, and sometimes interventions can’t be deliv-
ered with TMed at all (Sekhon et al., 2021). Some in-
terventions even require additional people to perform
physical exams. Further research on barriers and fa-
cilitating factors are needed to accelerate the uptake
of TMed (Banbury et al., 2018; S¸ahin et al., 2021).
2.2 National Perspective
National Achievements. Germany’s TMed efforts
are focused on providing access to care for rural
and under-served populations, enhancing coordina-
tion, and lowering costs. One of the notable german
TMed efforts is the creation of legal foundations (e.g.,
e-health law and digital healthcare act) for imple-
menting, billing, and TMed delegation of medical ser-
vices. Even though the government wants to advance
TMed, some regulatory burdens, such as changing
professional codes, billing arrangements, and indica-
tion for TMed, still need to be changed (Peine et al.,
2020). The TMed efforts are slowly translating to
countrywide care, although COVID-19 leads to an in-
creased TMed demand (Peine et al., 2020). Much
TMed applications are piloted and focused on spe-
cific diseases, esp. cardiovascular disease or mental
health. Furthermore, most applications include cer-
tain regions or professions (Allner et al., 2019).
Further Needs. Various associations, such as the
German Society for TMed (DGTELEMED) and na-
tional alliances (e.g., Bavarian TMed Alliance), pro-
mote TMed. Regional networks or projects exist
within funding limits and have specific Use-Cases
Implementing an Intersectoral Telemedicine Network in Rural Areas: Evaluation from the Point of View of Telemedicine Users
17

(UCs), e.g., stroke care, mental health, and primary
care. Partly complex applications such as the diagno-
sis of dementia via videoconferencing or TMed sup-
ported stroke units have been well-tested (Barth et al.,
2018; Mathur et al., 2019). In addition, previously
applied science on TMed is often unsystematic, and
many results aren’t published (Allner et al., 2019).
Lack of Transferable Research. Table 2 shows
that experience is limited in the field of TMed in
Bavaria with promising effects, although further re-
search is required (Black et al., 2011). National stud-
ies have shown a broad acceptance of TMed by health
professionals and patients, but there is untapped po-
tential in the actual use (Muehlensiepen et al., 2021;
Kirchberg et al., 2020; Techniker Krankenkasse,
2022; van den Berg et al., 2009; von Solodkoff et al.,
2020). Many health professionals share the assess-
ment that TMed measures improve care and repre-
sent a solution strategy for current challenges (Beck-
ers and Stellmacher, 2021, p. 60).
The elaborated international outcomes seem sim-
ilar, but there isn’t enough research to derive a clear
conclusion for Germany (Kn
¨
orr et al., 2022). Most
studies have low evidence levels, and the effects are
unclear. Some studies attest to a potential positive
benefit of TMed in the form of a reduction in the
workload of GPs, although the increase in quality
of care and safety hasn’t yet been conclusively clari-
fied (Black et al., 2011; Grohs and Thiess, 1997). The
effects always depend on the application scenario.
esp. treating skin diseases and wounds is a time-
saving and effective TMed application field (Eber
et al., 2019; J
¨
unger et al., 2019). Furthermore, om-
nipresent economic benefits, such as saving time and
money by avoiding unnecessary clinic visits, reducing
travel time, and utilizing more GPs working time for
direct patient care, are fulfilled by TMed. Nonethe-
less, many studies can’t calculate exact savings (Gen-
sorowsky et al., 2021). Yet, it should be clear by
the nature of TMed that elderly with limited mobil-
ity benefit from positive effects in their quality of life
through telediagnostics (Bohnet-Joschko and Stahl,
2019; Partheym
¨
uller et al., 2019).
Explore Barriers Nationally. Nationally, barri-
ers reducing the use of TMed exist mainly struc-
turally (Peine et al., 2020). Barriers are related to fi-
nancing, technical infrastructure, fear of misdiagnos-
ing, lack of interfaces, and missing resources, e.g.,
GP shortage (Weißenfeld et al., 2021). The indica-
tions for TMed are also limited by the impossibility
of examining patients directly physically, i.e., either
self-tests or non-medical specialists are needed (von
Solodkoff et al., 2020). The digital literacy of HCWs
primarily needs improvement, esp. in the legal as-
pects and data safety of TMed (Kirchberg et al.,
2020). Privacy knowledge and ambiguity regarding
terminology, digital treatment concepts, and evalua-
tion or improvement of TMed measures are demand-
ing (K
¨
ohnen et al., 2019; von Solodkoff et al., 2020).
The barriers for TMed can reduce use and accep-
tance. The literature cited so far doesn’t explicitly
examine the barriers nationally, doesn’t communicate
transparently, and doesn’t compare effects between
rural and urban TMed. We are unaware of any study
examining barriers to TMed in rural areas. Further-
more, international experience can only be transferred
to Germany to a limited extent due to the country’s
special structure and form of government organiza-
tion (Kidholm et al., 2012). This is exactly why fur-
ther research in the field is important.
3 METHODOLOGY
From July 2018 to October 2020, we implemented an
intersectoral TMed network in a German rural region.
We focus on UCs that deliver diagnostics and therapy
to the patient or HCWs due to audio-visual commu-
nications, the transmission of vital data between GPs
and non-physician staff, and a commercial eHRs.
First, we describe the TMed network and the consid-
ered UCs in Subsection 3.1, followed by a description
of the evaluation approach with Subsection 3.2.
3.1 Framework, Setup, and Use-Cases
After analyzing the requirements and opportunities,
we implemented an intersectoral TMed network in
Lower Bavaria consisting of several HSPs: one GP,
two regular clinics, one special clinic, two nursing
homes, and one intensive care provider with residen-
tial care communities. Furthermore, a mountain shel-
ter without para-/medical professionals was added to
the network (see UC 4). The HSPs relations are
shown in Figure 1.
Applied Technology. Various HSPs were equipped
gradually with TMed gear available in 2018. We
chose the equipment after market research in which
we considered: security, interfaces, usability, and
training. Because prior studies showed that common
documentation is vital, a commercial eHR Vitabook
®1
was used. For audio-visual communication as well
as the mobile and stationary transmission of video,
1
www.vitabook.de, accessed on 2023-02-06
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
18
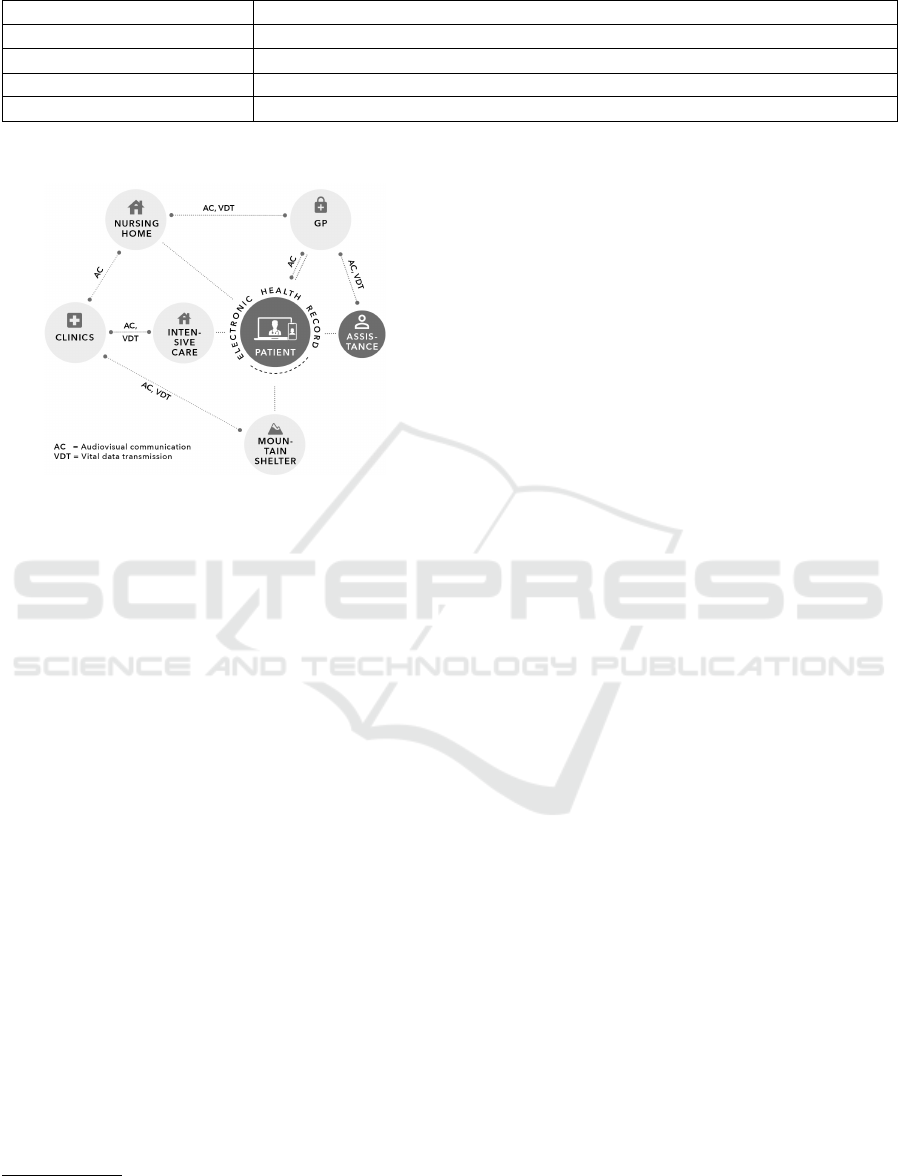
Table 2: Bavarian TMed projects, cf. (Jedamzik, 2022).
Project title content
eNurse
a
TMed network of specialists and GPs, established itself as an enterprise
SPeed
b
Cross-sector care record, TMed-network of GPs & geriatric-/ nursing homes
TEMPiS
c
TMed stroke care with special & regular clinics
Gesundheitsversorgung 4.0
d
GPs, pharmacy, nursing service & patients communicate via TMed
a
High Franconia
b
Ingolstadt Region
c
entire Bavaria
d
High Franconia
Figure 1: HSPs relationship within the TMed network.
images, and text, MEYDOC
®2
was used. For the
transmission of vital data, such as electrocardiogram
(ECG) data, Heart Rate Variability (HRV)rate, Blood
pressure (BP) and oxygen saturation, we used the mo-
bile medical product DynaVision
3
Use-Cases (UCs). With the described equipment,
we investigated seven TMed UCs as shown in Table 3.
In UC 1, we investigated TMed support of home
visits. Medical assistants could contact the GP audio-
visually during home visits, transmit vital data, and
carry out certain activities by delegation. The GP
also offered video consultations for patients (UC 2)
directly to reduce the risk of COVID-19 infections.
In UC 3, we connected an intensive care service
with a specialist clinic for respiratory diseases. The
TMed coordination and optimization of ventilation
parameters between the two HSPs were investigated
with online visits scheduled or organized ad hoc.
In UC 4, non-medical staff at the mountain shelter
were networked with the hospital to support rescue or
first aid in the event of mountain accidents.
During the project, it emerged that digital support
for wound management in nursing represents a useful
field of application (UC 5). Furthermore, we set up
digital consultation hours with the GP and the care
facility to discuss critical patients before the weekend.
2
www.meydoc.de, accessed on 2023-02-06
3
No longer available; supplier: www.eurovation.de
In all UCs, the eHR should be used as uniform
documentation and information basis (UC 7).
3.2 Evaluation Methodology
For evaluating the conditions of rural TMed and to an-
swer the research question on how TMed can improve
rural health care, a mixed-method approach was used
following Kuckartz (Kuckartz, 2014).
Quantitative Approach. Quantitatively the case
numbers, reasons for use, UCs as well as satisfaction
after each consultation were recorded using analog
feedback forms. Corresponding feedback forms were
filled out by GP, intensive care, and nursing home
staff. The data about the consultations were entered
and analyzed with IBM SPSS
®
Ver. 24.
Because of limited case numbers (see Table 4),
data analysis was only descriptive. The feedback
forms and the raw data will be provided as supple-
mentary material to this article.
Qualitative Approach. The qualitative approach
was intended to clarify the question of the feasibil-
ity and acceptance of TMed applications in practice,
as well as to record the challenges (i.e., the barri-
ers) and the subjectively perceived outcomes in care
multi-dimensionally. Therefore, seven guided inter-
views were conducted with non- and paramedical
staff (nursing home manager, nurse, medical assis-
tant, wound manager, critical care nurse) and the med-
ical profession (GP and specialist physician) from the
TMed network. For this purpose, we used a guide-
line with five main topics, including: (i) biographical
context (ii) understanding and acceptance of TMed
(iii) coordination and integration (iv) facilitating and
inhibiting factors (v) outcomes relevant to care
The interviews were transcribed and analyzed
using qualitative content analysis according to
Mayring (Mayring, 2010). MAXQDA Vers. 20 was
used to support the classification system, consisting of
six categories. The classification system is provided
as supplementary material to this article.
Implementing an Intersectoral Telemedicine Network in Rural Areas: Evaluation from the Point of View of Telemedicine Users
19

Table 3: Investigated UCs with involved HSPs and periods.
No. Use Cases Providers Duration
1 Home visits GP 11.2018 - 10.2020
2 Video consultation for patients GP 05.2020 - 10.2020
3 Intensive care care service, specialist clinic 03.2020 - 10.2020
4 Mountain accident regular hospital, mountain shelter 08.2019 - 11.2019
5 Wound management nursing home, regular hospital 07.2020 - 10.2020
6 Digital consultation for care nursing home, GP 09.2019 - 11.2019
7 eHR GP 02.2019 - 10.2020
4 RESULTS
The presentation of results follows the UCs and ends
structurally with contents of the qualitative analysis
on success factors and barriers of TMed.
4.1 Case Numbers and Applications
During the survey period, the audio-visual commu-
nication application was mainly used by GPs (170
cases) and intensive care units (15 cases). Further rel-
evant case numbers resulted from COVID-19 in video
consultation hours for patients (30 cases). Table 4
gives an overview about the investigated UCs.
Table 4: UC with case number.s
No. Use Case n
1 Home Visits 170
2 Video Consultation for Patients 30
3 Intensive Care 15
4 Mountain Accident
*
6
5 Wound Management 6
6 Digital Consultation Hour for Care
*
3
7 Electronic Health Record 10
∑
TMed applications, connections 240
*
only test runs, no real emergencies and live environment
Home Visits (GP ⇔ Medical Assistance). The
possibility for medical assistants to contact the GP
audio-visually during home visits was the most
common UC (n = 170). A total of 1.147 home visits
were carried out from Sept. 2018 to Oct. 2020. In
170 cases (14.8 % of all home visits), the medical
assistant needed to contact the GP via TMed. Of
these 170 cases, communication wasn’t possible in
44 cases (25.9 %). The results on (un)successful and
not required audio-visual communication between
medical assistants and GP during home visits in the
studied period are presented in Table 5.
Table 5: Audio-visual communication between medical as-
sistance and GP during a total of 1.147 home visits.
to all only to
home-visits tele-visits
Connection n % n %
successful 126 11.0 126 74.1
not successful 44 3.8 44 25.9
not required 978 85.2 - -
According to the feedback form, the reason for the
failed connections of 25.9 % (n = 44) is a lack of mo-
bile network coverage. On a query of satisfaction, a
sum of N = 345 responses was made, of which were
n = 273 (79.1 %) positive and n = 72 (20.9 %) neg-
ative. Overall the TMed users are pleased. With the
quantitative negative answers, 67 times (92.1 %) the
network connection, e.g., the transmission speed, was
criticized. Problems with the sound quality (3.2 %)
and picture quality (2.0 %) were marginal. The quali-
tative interviews confirm overall satisfaction and net-
work connection as a barrier 4.2.
Analyzing the successful connections shows that
clarification of wound care, with 38.3 % (n = 64), is
the most common reason for using audiovisual com-
munication, followed by medication management,
with 26.4 % (n = 44) and unforeseen symptoms in
the case of unexpected side effects or a deteriora-
tion in health with 4.6 % (n = 36). Even in 9.0 %
(n = 15), patients requested TMed actively an audio-
visual contact with the doctor. In 4.8 % (n = 8) of the
cases, audio-visual communication was used to clar-
ify queries regarding documents from other service
providers, such as prescriptions or discharge letters
from the hospital.
Video Consultation (GP ⇔ Patients). During the
COVID-19 pandemic, the GP established a video con-
sultation service for patients. 30 patients used this of-
fer at least once. During the interviews, the GP stated
that video consultation is an advantageous offer, al-
though older patients need guidance and a period of
acclimatization. Another interviewee, the Nursing
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
20
Home Manager (NH-Manager) (para. 13), who uses
video consultation privately to discuss laboratory re-
sults, emphasizes the savings in time for working peo-
ple and the protection against viruses: “TMed allows
me [. . . ] to discuss my medical needs with a doctor
at a controlled time. [. . . ] For me, waiting times in
the doctor’s office are wasted time and harbor risks of
infection.” Furthermore, indications of health benefits
are given by the same interviewee, the NH-Manager
(para. 13): “I would also go to the doctor more be-
cause of the elimination of waiting time and do less
self-therapy.”
4
Intensive Care (Nursing Service ⇔ Specialist
Clinic). Audiovisual visits (n = 15) between the
intensive care service and the specialist clinic were
used to coordinate ventilation parameters and discuss
saturation drops, blood gas analysis, secretion man-
agement, and patient mobilization with experts. For
organizing the audiovisual visits, pre-appointment
was revealed practicably. The visits were conducted
in the shared intensive care flats (n = 11) and also in
the mobile nursing service (n = 4). The case numbers
in this UC from March 2020 to October 2020 are
outlined in Table 6.
Table 6: Use and successful/not-successful application of
TMed for audio-visual communication in critical care, de-
pending on Care Flats (N = 51) and Home Visits (N = 24).
Care Flats Home Visits
Connection n % n %
successful 11 21.6 4 16.7
not successful 0 0.0 1 4.2
not required 40 78.4 19 79.2
The interviews with the intensive care specialist
indicate high satisfaction with the transmission and
image quality over the entire application period. The
feedback forms and the interviews HCWs mentioned
that using an electronic stethoscope would be useful.
Mountain Accident (Mountain Shelter ⇔ Clinic).
During our study, no emergencies or accidents oc-
curred during the test period, so there was no need for
actual operation. Therefore only test runs (n = 4) with
the audio-visual communication could be performed,
but they were successful with positive feedback. Non-
medical staff from the mountain shelter expressed that
user-friendliness was given.
No technical problems regarding connection es-
tablishment and transmission quality occurred, as
only General Packet Radio Service (GPRS) reception
4
All interview statements were translated from German
of the vital data transmission with DynaVision was re-
quired. In the parallel running video communication,
there were occasional dropouts because MEYDOC
®
required higher data rates, and network coverage was
limited to our mountain shelter.
For the medical staff of the regular clinic, our test
runs were an additional burden and a disruptive factor
in the daily clinic routine. Although the test runs with
the mountain shelter were assessed as useful in princi-
ple, the value added for the clinic wasn’t seen. In the
interview, the GP stated that he saw the advantage but
that this special UC would need to be implemented in
larger concepts with mountain rescue and the avail-
ability of much TMed-supported rescue points.
Wound Management (Nursing Home ⇔ Clinic).
We connected the nursing home to a regular clinic’s
wound specialist (special nurse education) and carried
out digital wound management (n = 6). Interviewing
the NH-Manager shows positive perceptions regard-
ing wound management: The networking with the
clinical wound manager showed above all that sim-
ple audio-visual applications, without special cam-
eras, with commercially available tablets, can lead to
an adequate assessment of the wound and thus support
the care. Interviewing the nurse showed a satisfactory
perception of nursing staff and home residents. From
the nursing staff’s perspective, the ward rounds with
a clinical wound manager enrich their work and con-
tribute to empowerment. Since, due to legal condi-
tions and a contract with a special wound care firm,
it was impossible to rely exclusively on wound visits
with the clinic, an analog on-site wound assessment
was carried out in parallel. The video visits and the
analog counterpart are comparable in outcomes, i.e.,
they lead to identical care proposals.
Digital Consultation Hour for Care (Nursing
Home ⇔ GP). In this UC, only successful tests (n =
3) in audio-visual communication for digital consul-
tations with the GP to avoid hospital admissions at
weekends were carried out. The digital consultations
weren’t extended to further live operations (n = 0) be-
cause of ”the good weekday doctor presence in the
nursing home” and ”unpredictability of emergencies,
e.g., falls”, as said by the NH-Manager. The GP inter-
view even showed that it makes more sense to imple-
ment a TMed network with the on-call medical ser-
vice to clarify emergencies that occur on weekends
and avoid unnecessary travel.
Electronic Health Record (GP). A limited number
of patients (n = 10) that used eHR at least once and
the interview with the GP show that there was less
Implementing an Intersectoral Telemedicine Network in Rural Areas: Evaluation from the Point of View of Telemedicine Users
21

eHR acceptance during the project period. However,
GPs and research associates created promotional fly-
ers and educated through citizen events. Only ten pa-
tients actively used the eHR. The GP states in inter-
views that benefits of the eHR weren’t always seen,
and HSPs, which actively use the eHR, were just a
few. High-aged patients aren’t ever already equipped
with mobile devices or weren’t digitally experienced
enough to use the eHR, which limits accessibility.
4.2 Qualitative Assessment
TMed-Perceptions. The interviews reveal that the
perception of TMed is largely positive among the sur-
veyed paramedical and medical staff (3.2). On the
HSP side, there were high expectations, and TMed
was seen as a chance to transfer expertise, save time,
and utilize resources (wound manager, para. 6; medi-
cal assistant, para. 4). The use of TMed “is fun” (criti-
cal care nurse (CC-Nurse), para. 16), “should be used
as often as possible” (CC-Nurse, para. 38), and “en-
riches skills on many levels” (nurse, para. 28).
But at some points, the interviews reveal fears
about liability, the anxiety of extra work for non-
physician staff, and fear of another physician’s status
and estrangement in patient relations (IP 5, para. 34).
The GP (para. 35) even remarked: “The fear of
making wrong decisions under time pressure is om-
nipresent. After all, even if TMed brings a lot of re-
lief, I am unsure if TMed has the same quality instead
of being on-site.” TMed was new for the HSPs, and
initially, there were some uncertainties.
Even though patients weren’t interviewed, the
HCW implied the satisfaction of patients. Similarly,
patients explicitly desired audio-visual contact with
the GP. The positive patient acceptance is evidenced
by an interview statement: “Patients have perceived
TMed positively and have been pleased with the new
opportunities. The uncomplicated way of consulting
experts via TMed was appreciated. [. . . ] An ambu-
lance ride and a visit to the hospital are, after all, not
pretty” (wound manager, para. 10). The positive per-
ception of TMed also seems to have increased fur-
ther during COVID-19 as a catalyst due to the in soci-
ety more widespread use of digital applications (spe-
cialist physician, para. 15) and “digitalization is now
more on the agenda” (specialist physician, para. 28).
The interviews even show that TMed is changing the
paramedical profession and empowering them due to
the possibility of delegating medical treatment to non-
physicians (wound manager, para. 35).
Outcomes. TMed has multiple outcomes, as evi-
denced by several interviews. It can be noted that the
use of TMed reduces the fear of contact with tech-
nology in general (nurse, para. 8). The introduction
of TMed has also eliminated General Data Protection
Regulation (GDPR) non-compliant solutions such as
using private devices with private messaging clients
for official purposes like the exchange of wound pic-
tures (NH-Manager, para. 2).
TMed even eliminates waiting and travel times
for vulnerable patients, which improves equality of
opportunity between healthier and multimorbid pa-
tients (NH-Manager, para. 31). According to the GP
(para. 30), efficiencies increase because travel times
are reduced, and physician work time can be bet-
ter used for patients through supportive delegation.
TMed complements current care and can alleviate
some challenges in rural healthcare. TMed allows
physicians to “reduce physician work time per patient
and helps the personal shortage in rural areas” (wound
manager, para. 35). But it is also a relief on the side of
the paramedical staff. In the interview with the medi-
cal assistant (para. 4), it emerged that queries are clar-
ified more quickly through TMed, thus speeding up
the treatment process and making paramedical staff
feel more confident or secure.
Intensive care (para. 31) also states that safety
for patients and caregivers increases because prob-
lems are discussed early, and there is a profes-
sional, uncomplicated possibility of contacting ex-
pertise through TMed. Early preventive interven-
tions, which are possible through TMed, can improve
healthiness: “The patient is fitter, more stable and
can also accept therapy recommendations. I can pre-
vent worsenings and therapists can work with more
resources” (CC-Nurse, para. 16).
Challenges and Barriers. Despite positive attribu-
tions, some barriers, like the mobile network during
home visits, resulted in, as noted by GP (para. 18),
“lost potential.” Participants wanted to use the appli-
cations as often as possible. Still frustratingly, po-
tential use was often seen for the applications, but
the technology couldn’t be used due to cellular cov-
erage. “As an employee, I assume that just works”
(medical assistant, para. 17). The TMed-ECG showed
a preparation effort due to the adhesive electrodes
and, if necessary, shaving of the corresponding ar-
eas, which wasn’t appropriate if the connection failed.
The TMed-ECG was also unwieldy, as shown by the
following testimonial: “Since we have so much med-
ical equipment to carry, the ECG is another suitcase
that has to be lugged” (medical assistance, para. 28).
Furthermore, structural difficulties are apparent,
as expressed in the interview of the NH-Manager and
the GP. The following quote from the NH-Manager
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
22

(para. 46) sums it up well: “The individual sectors are
rather brothers-in-law. Only with a few, I like to go
drinking, and with some others, I’m happy if I only
see them at Christmas, and then I’m allowed to leave
after two hours.” The relationship and design of the
cooperation are challenging because each HSP works
on TMed with its intentions, different revenues, di-
verse interests, and different efforts. This, in some
cases, leads to accusations between HSPs. Further-
more, intersectoral collaboration and process respon-
sibility are challenges. Building relationships takes
time because “everyone is cooking their soup and at
the beginning HSPs aren’t networked” (CC-Nurse,
para. 4). Also, not every HSP of the TMed-network
was able to prescribe. “Ultimately, it is the family
doctor who prescribes” (NH-Manager, para. 25).
Digital prescriptions can’t yet be mapped, and
many things, such as wound rounds, still have to be
done analogically for legal reasons. The interviewees
(GP, para. 43 and the special nurse from the clinic,
para. 18) also complain about the lack of financial in-
centives for TMed and poor billing modalities. In ad-
dition, the GP and the special nurse from the clinic
argue that TMed applications are often “just too ex-
pensive” (wound manager, para. 57) and that this is
“exploited economically, putting small HSPs at a dis-
advantage” (GP, para. 44).
Facilitators. The early integration of all rural HSPs
promotes TMed since treatments can be coordinated
better. TMed deployment is an intersectoral process
where it is important to recognize the motivators of
each HSP (GP, para. 46). TMed requires certain rules,
guidelines, statutes, and adequate privacy and secu-
rity (CC-Nurse, Abs. 18). Furthermore, it’s benefi-
cial if all HSP are “working on the same system with
the same things”, i.e., they have common information
and documentation base like an eHR (GP, para. 46).
In this context, “interfaces are desired” (wound man-
ager, para. 16). TMed solutions must be interopera-
ble, i.e., that TMed can be linked to HSP-software.
The need for TMed and digitalization training is
evident: “[As employee] there is uncertainty in han-
dling that you have to be guided first.” (NH-Manager,
para. 8) A high level of digital competence and aware-
ness is helpful, but, as stated by all interviewees,
many HSPs are less digitally aware. It is important
to sensitize all stakeholders for TMed and take away
their fears because if this doesn’t happen, then “the
TMed won’t be used” (nurse, para. 21). Sometimes
it also requires, as mentioned by the NH-Manager
(para. 30), a good interpersonal understanding, emo-
tional intelligence, and investment in relationships
(with employees, partners, and patients). Also, “a pe-
riod of acclimatization is necessary for everyone, in-
cluding the patients” (NH-Manager, para. 31).
Likewise, it is important to make TMed as handy
and user-friendly as possible. “There are definitely
older people who have little experience with digital
technology and are afraid to use it” (nurse, para. 35).
The interview with the GP and medical assistant
stated that TMed should be just easy to use, also the
effort required to use the ECG, for example, must
be reduced to a minimum TMed acceptance is re-
duced when problems quickly lead to frustration in
the stressful daily care routine (CC-Nurse, para. 38).
This was demonstrated by the disconnection of mo-
bile applications in rural areas. Therefore, technology
must always work, and regular funding is beneficial
for spreading TMed (wound manager, para. 16).
5 DISCUSSION
Subsection 5.1 discussed the methodology and Sub-
section 5.2 compares the findings with related work.
5.1 Method Discussion
We generated a variety of TMed-UCs with technol-
ogy that was state of the art (in 2018) when TMed
wasn’t widespread. The TMed-infrastructure, regu-
lations, and billing were just being introduced (Oden-
daal et al., 2020; Baake and Mitusch, 2021), so during
the project (2018 – 2020), it wasn’t possible to com-
pensate the HSP for their TMed-connections. The
UCs were carried out in rural Lower Bavaria. This
region was chosen due to the challenging HSP situa-
tion with a high average age and low population den-
sity. (Bayerisches Landesamt f
¨
ur Statistik, 2019b).
Furthermore, the number of cases is restricted in
each UC (N = 240 applications) because of limited
HSPs in rural areas. This doesn’t allow multivari-
ate analysis. Another shortcoming is that no teleme-
try data could be analyzed. To reduce limitations,
a mixed-method approach, consisting of quantitative
surveys and qualitative interviews, was used accord-
ing to (Kuckartz, 2014). It allowed exploring the sub-
jective perception of TMed users.
5.2 Results Discussion
Our study draws advantages from testing various UCs
with diverse HSPs rather than focusing on a specific
clinical picture, as is often the case in national stud-
ies (Allner et al., 2019; Barth et al., 2018). Overall
we present a multisided picture about TMed in a rural
german region, limiting our results generalization.
Implementing an Intersectoral Telemedicine Network in Rural Areas: Evaluation from the Point of View of Telemedicine Users
23

Table 7: Requirements for rural TMed.
Governance Technical HSP-setting
Legal TMed-framework Network coverage Training & Sensitization
Coordination centers Interoperability Wide implementation
Intersectoral incentives Usability & practicability numerous HSPs-variety
Further applied research Frustration- & fault-tolerance Process adaption(s)
In the project, audiovisual communication was
used extensively in the GPs and intensive care. In
the GP, digital support took place in 14.8% (n = 170)
of all 1.147 home visits. In our study, 20% (n = 15)
furthermore of all 75 intensive care treatments TMed
were successfully supported by digital tuning ventila-
tion parameters. This field completes the current re-
search, as no corresponding studies exist in rural ar-
eas with TMed-intensive care. The numbers would
be higher if there weren’t connection losses and more
project HSPs.
GP and intensive care rated TMed qualitatively
as valuable for rural areas. This HSPs may be over-
represented and at bias risk. Other applications, such
as vital data transmission and the eHR, were used
less (Table 4). The used TMed-vital data transmis-
sion needs preparation time (i.e., positioning the elec-
trodes), which doesn’t seem practical enough. In ad-
dition, the commercial eHR wasn’t used much de-
spite a lot of promotion and education. The interviews
show indications that the benefits aren’t seen and that,
at the time of the project, only a few HSPs could use
the eHR.
Some of our results are shown in previous stud-
ies, like the importance of interference-free applica-
tions and infrastructure, esp. mobile networks, as a
substantial barrier in rural Areas (Peine et al., 2020;
Odendaal et al., 2020). Usability, interoperability, re-
liable TMed, and training of HCWs for TMed are
confirmed as important for TMed-deployment (Ya-
mano et al., 2022; Haleem et al., 2021; S¸ ahin et al.,
2021). Some construction sites still exist, such as reg-
ulation and incentivizing funding of TMed, confirmed
by our study (von Solodkoff et al., 2020). In Comple-
menting the Cochrane review (Odendaal et al., 2020),
which argues that fears need to be reduced, our study
results go beyond this and call for awareness raising
and general training in digitization among HCWs and
the population at large. It should be considered that
the socio-cultural environment can play a role in the
TMed-deployment.
The perception of TMeds in our study was positive
in the sense of a high acceptance observed in related
work (Muehlensiepen et al., 2021; Kirchberg et al.,
2020). TMed-benefits can be transferred to rural ar-
eas (Hackmann and Moog, 2010). The avoidance of
travel time, the reduction of burden on the elderly, and
the immediate adjustment of care by TMed are appre-
ciated by HCWs and patients. GPs work time can be
better utilized due to reducing traveling. These bene-
fits and increased quality of life are supported by na-
tional studies (Black et al., 2011; Kn
¨
orr et al., 2022;
Beckers and Stellmacher, 2021). Promoting further
research about TMed in rural areas is necessary. The
study populations are mostly restricted.
6 CONCLUSION
This paper outlines the multidimensional benefits of
TMed in rural german healthcare. It shows the po-
tential of multisided TMed applications due to an in-
tersectoral TMed network with several HSPs. Due to
a mixed-method approach, we evaluated the barriers,
facilitators, and perspectives of TMed users.
Summary. Audio-visual communication was heav-
ily used in the GP (n = 203). Vital-data transmis-
sion was used less for the mountain accident (n = 6)
and also small in GP (n = 11), because of the needed
preparation effort. The eHR was used only in a few
cases (n = 10) as insufficient patients signed up. Al-
though the cases were limited in total (N = 240), qual-
itatively, we highlight that professional users are open
to TMed and satisfied with it. The empowerment of
the paramedical staff is increased, esp. with audio-
visual communication, and they feel more confident.
The elimination of travel time led to relief for GPs
and their staff and ease to the outpatient and inpatient
nursing services. TMed led to efficiency, as time-
consuming telephone arrangements or mailings were
avoided. In addition, delegation and TMed guidance
of medical tasks gave paramedical staff new compe-
tencies, which were perceived as enriching. Ambi-
guities could also be clarified more quickly, creating
security. TMed not only avoids unnecessary travel,
TMed also reduces the patient’s burden.
Recommendations. TMed is feasible and helps to
meet rural healthcare needs, as indicated by our study.
TMed has benefits in rural areas, particularly in terms
of time-saving for GP and intensive care. However,
some barriers must be overcome for wider TMed im-
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
24

plementation, such as better mobile network cover-
age in remote areas and financial incentives to collab-
orate intersectoral (Table 7). TMed must be mostly
fail-safe. Furthermore, someone should always be
available to act as a coordinating point and take care.
Coordination centers should be established, monetary
incentives for intersectoral cooperation and TMed
should be given, and a wide range of HSP should
be involved. Other considerations include coordina-
tion and adaptation of the treatment processes among
HSPs and digitalization training for TMed users.
Future research should focus on improving the us-
ability of TMed, exploring TMed barriers, and inte-
grating new technologies like Artificial intelligence
(AI) and augmented reality. More studies should also
conduct knowledge about rural TMed and use bigger
study populations and comparison groups.
ACKNOWLEDGEMENTS
This research was funded by the Bavarian State Min-
istry of Health and Care.
REFERENCES
Allner, R., Wilfling, D., Kidholm, K., and Steinh
¨
auser,
J. (2019). Telemedizinprojekte im l
¨
andlichen Raum
Deutschlands. Eine systematische Bewertung mit dem
”Modell zur Evaluation von telemedizinischen An-
wendungen”. Zeitschrift f
¨
ur Evidenz, Fortbildung und
Qualit
¨
at im Gesundheitswesen, 141-142:89–95.
Amatya, R., Mishra, K., Karki, K., Puri, I., Gautam, A.,
Thapa, S., Katwal, U., Veer, S., Zervos, J., Kaljee, L.,
Prentiss, T., Zenlea, K., Maki, G., Rayamajhi, P. J.,
Khanal, N. K., Thapa, P., Upadhyaya, M. K., and Ba-
jracharya, D. (2022). Post-implementation Review
of the Himalaya Home Care Project for Home Iso-
lated COVID-19 Patients in Nepal. Frontiers in public
health, 10:891611.
Baake, P. and Mitusch, K. (2021). Mobile Phone Net-
work Expansion in Sparsely Populated Regions in
Germany: Roaming Benefits Consumers.
Banbury, A., Nancarrow, S., Dart, J., Gray, L., and Parkin-
son, L. (2018). Telehealth Interventions Delivering
Home-based Support Group Videoconferencing: Sys-
tematic Review. Journal of Medical Internet Re-
search, 20(2):e25.
Barth, J., Nickel, F., and Kolominsky-Rabas, P. L. (2018).
Diagnosis of cognitive decline and dementia in rural
areas - A scoping review. International journal of
geriatric psychiatry, 33(3):459–474.
Batsis, J. A., DiMilia, P. R., Seo, L. M., Fortuna, K. L.,
Kennedy, M. A., Blunt, H. B., Bagley, P. J., Brooks,
J., Brooks, E., Kim, S. Y., Masutani, R. K., Bruce,
M. L., and Bartels, S. J. (2019). Effectiveness of Am-
bulatory Telemedicine Care in Older Adults: A Sys-
tematic Review. Journal of the American Geriatrics
Society, 67(8):1737–1749.
Bayerisches Landesamt f
¨
ur Statistik (2019a).
Demographie-Spiegel f
¨
ur Bayern: Berechnungen
bis 2031.
Bayerisches Landesamt f
¨
ur Statistik (2019b). Landkreis
Freyung-Grafenau: Eine Auswahl wichtiger statistis-
cher Daten.
Beckers, R. and Stellmacher, L. (2021). Qualit
¨
atssicherung
in der Telemedizin. In Telemedizin, pages 53–71.
Springer, Berlin, Heidelberg.
Black, A. D., Car, J., Pagliari, C., Anandan, C., Cresswell,
K., Bokun, T., McKinstry, B., Procter, R., Majeed,
A., and Sheikh, A. (2011). The impact of eHealth
on the quality and safety of health care: a systematic
overview. PLoS medicine, 8(1):e1000387.
Bohnet-Joschko, S. and Stahl, T. (2019). Telegeriatrische
Modelle: Einblick in die Zukunft der Versorgung.
Pflegezeitschrift, 72(1-2):50–53.
Butzner, M. and Cuffee, Y. (2021). Telehealth Interven-
tions and Outcomes Across Rural Communities in the
United States: Narrative Review. Journal of Medical
Internet Research, 23(8):e29575.
Dudel, C. (2018). Demografie. In Voigt, R., editor,
Handbuch Staat, Handbuch, pages 7–15. Springer VS,
Wiesbaden, Germany.
Eber, E. L., Arzberger, E., Michor, C., Hofmann-Wellenhof,
R., and Salmhofer, W. (2019). Mobile Teledermatolo-
gie in der Behandlung chronischer Ulzera. Der Hau-
tarzt; Zeitschrift fur Dermatologie, Venerologie, und
verwandte Gebiete, 70(5):346–353.
European Parliament (2021). Demographic outlook for the
European Unii 2021. Publications Office, Brussels.
Ganapathy, K., Alagappan, D., Rajakumar, H., Dhana-
pal, B., Rama Subbu, G., Nukala, L., Premanand,
S., Veerla, K. M., Kumar, S., and Thaploo, V.
(2019). Tele-Emergency Services in the Himalayas.
Telemedicine journal and e-health : the official
journal of the American Telemedicine Association,
25(5):380–390.
Gensorowsky, D., D
¨
orries, M., and Greiner, W. (2021).
Telemedizin – Bewertung des Nutzens. In Marx,
G., Rossaint, R., and Marx, N., editors, Telemedizin,
pages 483–496. Springer Berlin Heidelberg, Berlin,
Heidelberg.
Goharinejad, S., Hajesmaeel-Gohari, S., Jannati, N., Go-
harinejad, S., and Bahaadinbeigy, K. (2021). Review
of Systematic Reviews in the Field of Telemedicine.
Medical Journal of the Islamic Republic of Iran,
35:184.
Grohs, B. and Thiess, M. (1997). Telematik im Gesund-
heitswesen: Perspektiven der Telemedizin in Deutsch-
land.
Hackmann, T. and Moog, S. (2010). Pflege im Span-
nungsfeld von Angebot und Nachfrage. Zeitschrift f
¨
ur
Sozialreform, 56(1):113–138.
Haleem, A., Javaid, M., Singh, R. P., and Suman, R.
(2021). Telemedicine for healthcare: Capabilities,
Implementing an Intersectoral Telemedicine Network in Rural Areas: Evaluation from the Point of View of Telemedicine Users
25

features, barriers, and applications. Sensors interna-
tional, 2:100117.
Hennig, B. D. (2019). The growth and decline of urban ag-
glomerations in Germany. Environment and Planning
A: Economy and Space, 51(6):1209–1212.
Jedamzik, S. (2022). Bayerische Telemedizin Al-
lianz: Telemedizinische Projekte in Bayern.
https://www.telemedallianz.de/praxis/bayerische-
projekte/. Last checked on Sep 31, 2022.
J
¨
unger, M., Arnold, A., and Lutze, S. (2019). Tele-
dermatologie zur notfallmedizinischen Patientenver-
sorgung : Zweijahreserfahrungen mit teledermatolo-
gischer Notfallversorgung. Der Hautarzt, 70(5):324–
328.
Kidholm, K., Ekeland, A. G., Jensen, L. K., Rasmussen, J.,
Pedersen, C. D., Bowes, A., Flottorp, S. A., and Bech,
M. (2012). A model for assessment of telemedicine
applications: mast. International journal of technol-
ogy assessment in health care, 28(1):44–51.
Kirchberg, J., Fritzmann, J., Weitz, J., and Bork, U. (2020).
eHealth Literacy of German Physicians in the Pre-
COVID-19 Era: Questionnaire Study. JMIR mHealth
and uHealth, 8(10):e20099.
Kn
¨
orr, V., Dini, L., Gunkel, S., Hoffmann, J., Mause, L.,
Ohnh
¨
auser, T., St
¨
ocker, A., and Scholten, N. (2022).
Use of telemedicine in the outpatient sector during
the COVID-19 pandemic: a cross-sectional survey of
German physicians. BMC Primary Care, 23(1):92.
K
¨
ohnen, M., Dirmaier, J., and H
¨
arter, M. (2019).
Potenziale und Herausforderungen von E-Mental-
Health-Interventionen in der Versorgung psychischer
St
¨
orungen. Fortschritte der Neurologie-Psychiatrie,
87(3):160–164.
Kopetsch, T. (2010). Dem deutschen Gesundheitswe-
sen gehen die
¨
Arzte aus! Studie zur Altersstruktur-
und Arztzahlentwicklung. Bundes
¨
arztekammer und
Kassen
¨
arztliche Bundesvereinigung, Berlin, 5. aktu-
alisierte und komplett
¨
uberarb. aufl. edition.
Kuckartz, U. (2014). Mixed Methods: Methodologie,
Forschungsdesigns und Analyseverfahren. Springer
VS, Wiesbaden.
Laschet, H. (2019).
¨
Arztemangel bereitet weiter Sorgen.
Uro-News, 23(5):51.
L
¨
offler, A., Hoffmann, S., Fischer, S., and Spallek,
J. (2021). Ambulante Haus- und Facharztver-
sorgung im l
¨
andlichen Raum in Deutschland –
Wie stellt sich die Versorgungssituation aus Sicht
¨
alterer Einwohner im Landkreis Oberspreewald-
Lausitz dar? Gesundheitswesen (Bundesverband
der Arzte des Offentlichen Gesundheitsdienstes (Ger-
many)), 83(1):47–52.
Ma, Y., Zhao, C., Zhao, Y., Lu, J., Jiang, H., Cao, Y., and
Xu, Y. (2022). Telemedicine application in patients
with chronic disease: a systematic review and meta-
analysis. BMC medical informatics and decision mak-
ing, 22(1):105.
Mathur, S., Walter, S., Grunwald, I. Q., Helwig, S. A.,
Lesmeister, M., and Fassbender, K. (2019). Improving
Prehospital Stroke Services in Rural and Underserved
Settings With Mobile Stroke Units. Frontiers in neu-
rology, 10:159.
Mayring, P. (2010). Qualitative Inhaltsanalyse: Grundla-
gen und Techniken. Beltz P
¨
adagogik. Beltz, Wein-
heim, 11., aktualisierte und
¨
uberarb. aufl. edition.
Mbunge, E., Batani, J., Gaobotse, G., and Muchemwa,
B. (2022). Virtual healthcare services and digital
health technologies deployed during coronavirus dis-
ease 2019 (COVID-19) pandemic in South Africa: a
systematic review. Global health journal (Amsterdam,
Netherlands), 6(2):102–113.
Meyer, N. (2020). Sicherung der medizinischen Ver-
sorgung in l
¨
andlichen Regionen: Eine empirische
Untersuchung im rheinland-pf
¨
alzischen Gillenfeld
und Umgebung, volume Band 2 of Schriften zu
Gesundheits- und Pflegewissenschaften. LIT, Berlin
and M
¨
unster.
Muehlensiepen, F., Knitza, J., Marquardt, W., Engler, J.,
Hueber, A., and Welcker, M. (2021). Acceptance
of Telerheumatology by Rheumatologists and Gen-
eral Practitioners in Germany: Nationwide Cross-
sectional Survey Study. Journal of Medical Internet
Research, 23(3):e23742.
Odendaal, W. A., Anstey Watkins, J., Leon, N., Goudge,
J., Griffiths, F., Tomlinson, M., and Daniels, K.
(2020). Health workers’ perceptions and experi-
ences of using mHealth technologies to deliver pri-
mary healthcare services: a qualitative evidence syn-
thesis. The Cochrane database of systematic reviews,
3:CD011942.
Partheym
¨
uller, A., M
¨
uller, C., Schneider, V., and Rashid,
A. (2019). Effekte der telemedizinischen Assistenz
bei haus
¨
arztlichen Hausbesuchen im Projekt MONA.
Peine, A., Paffenholz, P., Martin, L., Dohmen, S., Marx, G.,
and Loosen, S. H. (2020). Telemedicine in Germany
During the COVID-19 Pandemic: Multi-Professional
National Survey. Journal of Medical Internet Re-
search, 22(8):e19745.
S¸ahin, E., Yavuz Veizi, B. G., and Naharci, M. I. (2021).
Telemedicine interventions for older adults: A sys-
tematic review. Journal of telemedicine and telecare,
page 1357633X211058340.
Schwab, T. (2020). Pilotprojekt Telearzt: Gesundheit-
stelematik. KVB Forum, pages 28–29.
Sekhon, H., Sekhon, K., Launay, C., Afililo, M., Inno-
cente, N., Vahia, I., Rej, S., and Beauchet, O. (2021).
Telemedicine and the rural dementia population: A
systematic review. Maturitas, 143:105–114.
Speyer, R., Denman, D., Wilkes-Gillan, S., Chen, Y.-W.,
Bogaardt, H., Kim, J.-H., Heckathorn, D.-E., and
Cordier, R. (2018). Effects of telehealth by allied
health professionals and nurses in rural and remote ar-
eas: A systematic review and meta-analysis. Journal
of rehabilitation medicine, 50(3):225–235.
Techniker Krankenkasse (2022). Forsa-Umfrage:
Digitalisierung im Gesundheitswesen gefordert.
https://www.tk.de/presse/themen/digitale-
gesundheit/elektronische-
patientenakte/digitalisierung-im-gesundheitswesen-
gefordert-2131956?tkcm=aaus. Last checked on
Sep 29, 2022.
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
26

The American Geriatrics Society (2012). Guiding princi-
ples for the care of older adults with multimorbidity:
an approach for clinicians: American Geriatrics So-
ciety Expert Panel on the Care of Older Adults with
Multimorbidity. Journal of the American Geriatrics
Society, 60(10):E1–E25.
Tsiasioti, C., Behrendt, S., J
¨
urchott, K., and Schwinger, A.
(2020). Pflegebed
¨
urftigkeit in Deutschland. In Ja-
cobs, K., Kuhlmey, A., and Greß, S., editors, Mehr
Personal in der Langzeitpflege - aber woher?, Pflege-
Report, pages 257–311. Springer Berlin Heidelberg,
Berlin, Heidelberg.
Valentijn, P. P., Schepman, S. M., Opheij, W., and Brui-
jnzeels, M. A. (2013). Understanding integrated care:
a comprehensive conceptual framework based on the
integrative functions of primary care. International
journal of integrated care, 13:e010.
van den Berg, N., Meinke, C., and Hoffmann, W.
(2009). M
¨
oglichkeiten und Grenzen der Telemedi-
zin in der Fl
¨
achenversorgung. Der Ophthalmologe
: Zeitschrift der Deutschen Ophthalmologischen
Gesellschaft, 106(9):788–794.
von Solodkoff, M., Strumann, C., and Steinh
¨
auser, J.
(2020). Akzeptanz von versorgungsangeboten zur
ausschließlichen fernbehandlung am beispiel des
telemedizinischen modellprojekts , , docdirekt“: ein
mixed-methods design. Das Gesundheitswesen,
83(03):186–194.
Weingarten, P. and Steinf
¨
uhrer, A. (2020). Daseinsvor-
sorge, gleichwertige Lebensverh
¨
altnisse und l
¨
andliche
R
¨
aume im 21. Jahrhundert. Zeitschrift f
¨
ur Politikwis-
senschaft, 30(4):653–665.
Weißenfeld, M. M., Goetz, K., and Steinh
¨
auser, J. (2021).
Facilitators and barriers for the implementation of
telemedicine from a local government point of view
- a cross-sectional survey in Germany. BMC Health
Services Research, 21(1):919.
Yamano, T., Kotani, K., Kitano, N., Morimoto, J., Emori,
H., Takahata, M., Fujita, S., Wada, T., Ota, S.,
Satogami, K., Kashiwagi, M., Shiono, Y., Kuroi, A.,
Tanimoto, T., and Tanaka, A. (2022). Telecardiology
in Rural Practice: Global Trends. International Jour-
nal of Environmental Research and Public Health,
19(7):4335.
Zhang, A., Wang, J., Wan, X., Zhang, Z., Zhao, S., Guo,
Z., and Wang, C. (2022a). A Meta-Analysis of the Ef-
fectiveness of Telemedicine in Glycemic Management
among Patients with Type 2 Diabetes in Primary Care.
International Journal of Environmental Research and
Public Health, 19(7).
Zhang, Y., Bai, W., Li, R., Du, Y., Sun, R., Li, T.,
Kang, H., Yang, Z., Tang, J., Wang, N., and Liu, H.
(2022b). Cost-Utility Analysis of Screening for Di-
abetic Retinopathy in China. Health Data Science,
2022:1–11.
Implementing an Intersectoral Telemedicine Network in Rural Areas: Evaluation from the Point of View of Telemedicine Users
27
