
SleepPal: A Sleep Monitoring System for Body Movement and Sleep
Posture Detection
Ali Ibrahim
1,2 a
, Kabalan Chaccour
1,2 b
, Amir Hajjam El Hassani
1 c
and Emmanuel Andres
3 d
1
Nanomedicine, Imagery and Therapeutic (NIT Lab.), University of Bourgogne Franche-Compt
´
e (UBFC), Belfort, France
2
TICKET Lab. Dept. of Computer and Communications Engineering, Antonine University (UA), Hadat-Baabda, Lebanon
3
Health Sciences Pedagogy Center, University of Strasbourg, Strasbourg, France
Keywords:
Sleep, Sleep Posture, Nocturnal Body Movements, Sleep Quality, Actigraphy.
Abstract:
Sleep posture is a clinical relevant parameter for it is associated with several pathologies and affects the
quality of sleep. In this paper, we propose SleepPal a sleep monitoring system for body movement and sleep
posture detection. It consists of a wearable device that extracts data from a 3-axis accelerometer and transmits
them to a remote monitoring station. A threshold-based algorithm is used to detect body movement and to
distinguish between transitions. The proposed system will also evaluate the sleep quality index. Experiments
were conducted on 10 subjects and results showed 88% of sensitivity and 82% of accuracy.
1 INTRODUCTION
Movements during sleep and body postures were re-
ported to be associated with different pathologies
(Horne et al., 2002) and decreased sleep quality
(De Koninck et al., 1983). For example, patients with
insomnia spend more time on their back (De Koninck
et al., 1983), whereas patients with heart failure pre-
fer to sleep on their side (Leung et al., 2003) (Hoff-
stein, 1996). Sleep apnea is also increased by certain
sleep positions such as supine position (Cartwright,
1984). Obviously, the number of pathologies that im-
plies sleep disorders has become of significance im-
portance that it became prime to evaluate the quality
of sleep. Accurate measurement of sleep quality is
performed normally by overnight polysomnography
(PSG) which includes several physiological measure-
ments such as Electrocardiogram (ECG), Electroen-
cephalogram (EEG), Electromyogram (EMG), res-
piration and body movement during sleep (Colman,
2006). PSG is a reliable method used in sleep diagno-
sis, but it is not without drawbacks. It involves high
costs associated with the utilisation of complex equip-
ment and require continuous monitoring from health-
care professionals. In addition, attaching many elec-
a
https://orcid.org/0000-0003-0092-7247
b
https://orcid.org/0000-0002-3731-7787
c
https://orcid.org/0000-0002-8470-806X
d
https://orcid.org/0000-0002-7914-7616
trodes to the patient’s body is considered intrusive,
which can disturb sleep. Thus, the measured data
may not accurately represent the sleep behavior of
the patients. These drawbacks make PSG impractical
to be implemented within a long-term sleep monitor-
ing system within homes. Alternately, actigraphy has
been recently adopted for continuous measurement of
sleep activity. The device is called an actigraph. It is
composed of motion sensors such as accelerometers.
It is capable of measuring and logging the movement.
The advantages of actigraphy over PSG are many, to
note the cost, the low number of sensors, the mini-
mum intrusiveness and and the continuous log over
long periods of time (i.e Weeks, Months).
In this paper, a complete monitoring system in-
cluding a wearable device for a long-term sleep mon-
itoring is proposed. The wearable device named
SleepPal is comfortable to wear with low intrusive-
ness for the patient and its deployment does not re-
quire any intervention from a trained expert. It ex-
tracts data from a 3-axis accelerometer and transmits
them to a remote monitoring station over a wireless
network connection. The body posture, the position,
and the movements can be determined based on mul-
tiple features extracted from the acceleration data. A
simple but accurate threshold-based algorithm is de-
veloped that detects the transitions between different
body postures that are defined in a state diagram. Fi-
nally, the sleep quality indicator will be determined
40
Ibrahim, A., Chaccour, K., El Hassani, A. and Andres, E.
SleepPal: A Sleep Monitoring System for Body Movement and Sleep Posture Detection.
DOI: 10.5220/0011840900003476
In Proceedings of the 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2023), pages 40-47
ISBN: 978-989-758-645-3; ISSN: 2184-4984
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)

considering the number of transitions between two
sleep postures over the period of the sleep.
The rest of this paper is divided as follows. Sec-
tion 2 surveys existing solutions related to bed move-
ments detection. Section 3 elaborates on the material
and methods followed in the development and imple-
mentation of the sleep monitoring system. Section 4
explains the experimental evaluation of the proposed
system and discusses the obtained results. Finally,
Section 5 presents the concluding remarks and the fu-
ture directions of this research.
2 RELATED WORK
Actigraphy has been used in various areas of medi-
cal research, typically for monitoring motion-related
sleep disorders. In fact, It has been used in many stud-
ies since 30 years ago. (Kupfer et al., 1972) reported
a correlation between EEG signals, wrist activity, and
wakefulness in 1972. (Sadeh et al., 1995) concluded
that normal subjects showed more than 90% correla-
tion when comparing actigraphy data with PSG. By
1995, sufficient experimentation had been carried out
to finally enable the Standards of Practice Committee
of the American Sleep Disorders Association (ASDA)
to support the use of actigraphy in evaluating cer-
tain aspects of sleep disorders, such as insomnia, cir-
cadian sleep–wake disturbances, and periodic limb
movements. On an higher level, a generic classifica-
tion of bed related systems was proposed by (Ibrahim
et al., 2021). The authors classified these systems
into Wearable Systems (WS), Non-Wearable Systems
(NWS), and Fusion Systems (FS).
• Wearable Systems (WS): Many studies have
been reported to use actigraphy in WS. For in-
stance, (Miwa et al., 2007) proposed a rollover
detection system using a SenseWear Pro2 Arm-
band. They used the maximum and the mean
acceleration in the x and y directions to identify
the posture differences using a threshold based
algorithm. The experiments showed that 82.4%
of rollovers were detected. Similarly, (Acharya,
2020) proposed a rollover detection system using
the ADXL335 accelerometer attached on socks
where acceleration row data was used in a thresh-
old based algorithm.
• Non-Wearable Systems (NWS): Other studies
reported the use of unobtrusive sensors used for
bed movement detection. These include load sen-
sors installed under bedposts. (Adami et al., 2008)
proposed a system for classification of movement
in bed using load cells. The experiments were
done on 15 participants and showed an accuracy
of 84.6%. (Beattie et al., 2011) also used load
cells under bedposts giving a total of 4 cells. The
classification of the sleeping posture was done us-
ing K-Means classifier of the bed’s Center of Pres-
sure (CoP) in the x and y directions. The exper-
iments showed an accuracy of 68%, 57%, 69%,
and 33% for the back, right, left, and stomach
postures respectively. The problem with this ap-
proach is that CoPy values for back and stom-
ach postures are the same so the classifier fails to
distinguish between them. An unrestrained sleep
monitoring system using cameras has been also
proposed to monitor sleep postures. (Lee et al.,
2015) proposed a system to monitor the sleep-
ing position using a Kinect sensor. They used
Kinect’s skeleton and Kinect’s infrared camera to
detect the body joints. The joint model given by
the Kinect has 25 points. The authors recorded the
x, y and z positions of those points and calculated
the sleep movement taking the Euclidean distance
between those points with respect to time. How-
ever, the procedure may still be considered as an
invasion of privacy for some patients which makes
its utilisation not suitable.
• Fusion Systems (FS): Fusion of sensors will form
a multi-channel source of data which can provide
more accurate analysis. For instance, (Nam et al.,
2016a) used a pressure sensor and an accelerom-
eter to extract data on motion, respiration, body
activity, and heart rate. These data were used to
measure sleep quality by estimating the depth of
sleep, the number of apneaic episodes and the pe-
riodicity. The experimental results demonstrated
that the proposed system is effective in measuring
the physiological factors of sleep quality.
In addition to proposing a low cost device used to
identify body posture and transitions, this paper seeks
to contribute in proposing a body transition matrix
that could be used in any threshold based algorithm.
3 MATERIALS AND METHODS
3.1 Wearable Sensor
Continuous sleep monitoring must be unobtrusive
and have minimal physical impacts on bed activi-
ties. For these reasons, we proposed our sleep mon-
itoring system SleepPal. SleepPal includes a small
device that could be attached to the center of the
chest and measures the body acceleration in the three
axes. The device transmits real-time accelerome-
SleepPal: A Sleep Monitoring System for Body Movement and Sleep Posture Detection
41
ter raw data over the Wi-Fi network to a monitor-
ing and visualization software installed on a remote
computer. The architecture of SleepPal is illustrated
in Figure 1. The system is composed of an Iner-
tial Measurement Unit (IMU) and a Microcontroller
Unit (MCU). To ensure the wireless communication,
ESP8266 NodeMCU is used with IMU MPU6050
which includes the ADXL345 triaxial accelerometer.
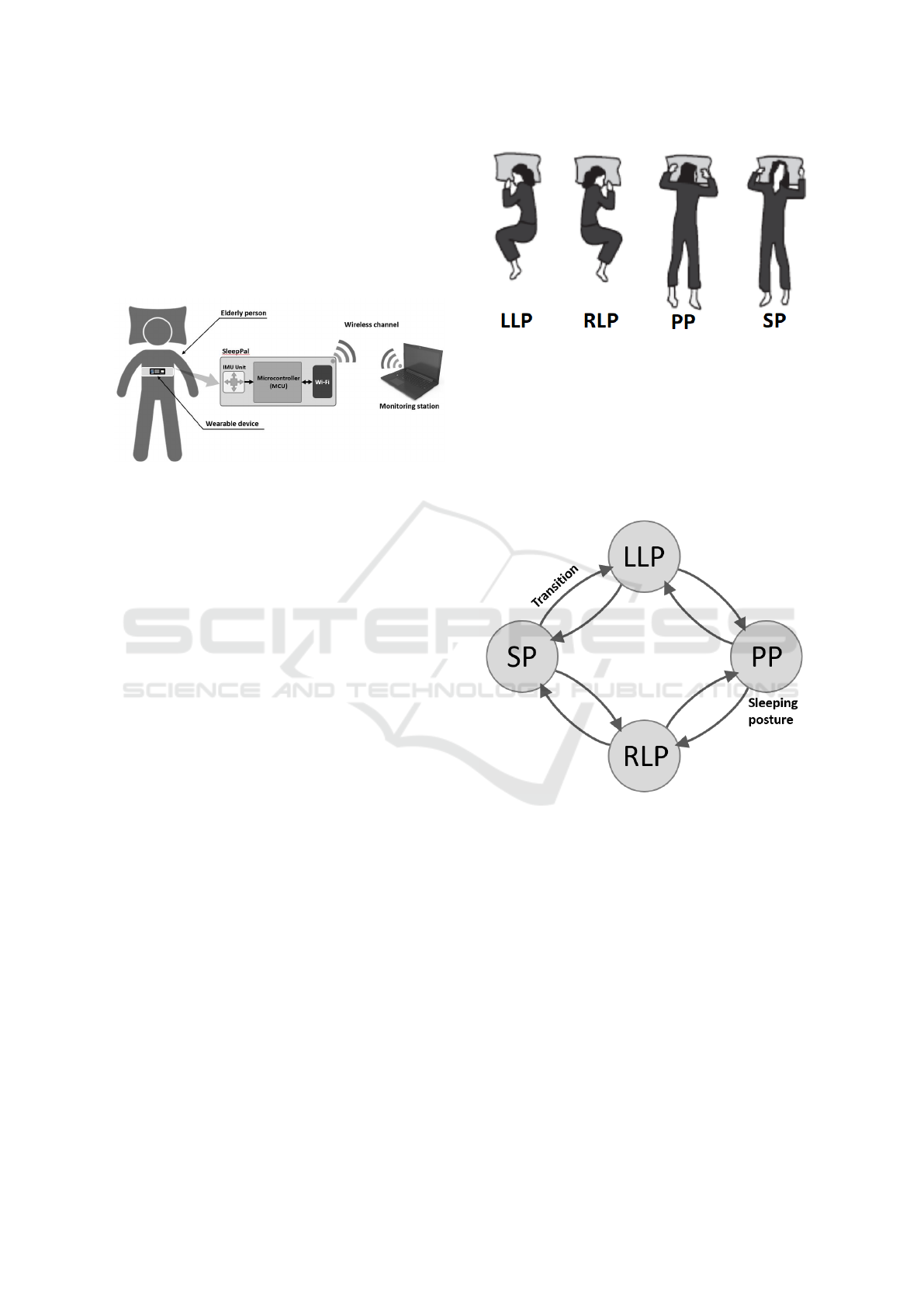
Figure 1: Architecture of SleepPal.
3.2 Sleep Postures and Bed Movements
The objective of SleepPal is to detect and record the
sleep posture and bed movements in order to build a
sleep monitoring database. The device will be able to
detect and store each posture and each movement in
the database for further analysis and evaluate the sleep
quality. Generally, sleep postures on the bed could be
classified into four categories namely, the front, the
back, the left, and the right (Nam et al., 2016b). The
same terminology is also adopted by (Hoque et al.,
2010). This terminology will be adopted for the rest
of this paper. These postures are as follows:
• Supine Posture (SP): The subject is lying on his
back (back posture);
• Prone Posture (PP): The subject is lying on his
stomach (front posture);
• Right Lateral Posture (RLP): The subject is lying
on his right side (right posture);
• Left Lateral Posture (LLP): The subject is lying
on his left side (left posture);
The sleeping posture is identified based on the
body movement detected and the raw data extracted
from the accelerometer. By knowing which move-
ment was performed, we can derive the position rela-
tively to the edges of the bed. The motion data is used
to validate the last performed posture.
A change in the sleeping posture also called
rollover is defined as a series of trunk movements
beginning from the current static posture to the next
static posture through rotational motions during sleep
(Miwa et al., 2007) (Acharya, 2020). Therefore, the
most adequate location to fix our device is on the
Figure 2: Common sleeping postures. From left to right:
Left Lateral Posture (LLP), Right Lateral Posture (RLP),
Prone Posture (PP) and Supine Posture (SP).
chest. Referring to this definition, each static posture
is defined as a state and each rollover is defined as a
transition. SleepPal will count the rollovers to deter-
mine the position and evaluate the sleep quality. We
identify four states and eight possible transitions as
illustrated in Figure 3.
Figure 3: Sleep postures and movement transition scheme.
On the side note, there can be other transitions
such that from RLP to LLP and vice versa or from
PP to SP and vice versa, however, such transitions are
a composition of two consecutive transitions.
3.3 Features Extraction
The data from the accelerometer is collected in raw
mode, which provides the acceleration data in actual
g-forces. The sampled data are stored and analysed in
epoch of an approximate length of 2s. The extracted
features are the Mean Acceleration (
¯
A
(T )
,
¯
A
(L)
), and
the Mean of Absolute Difference (MAD
(T )
, MAD
(L)
)
for both the transverse and longitudinal directions
as well as the Posture Difference (∆P) proposed by
(Miwa et al., 2007). Herein, MAD
(d)
is used as an
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
42

indicator of the movement intensity, the Mean Accel-
eration
¯
A
(d)
is used to identify the direction, and (∆P)
is used to identify the difference in postures. These
features are formulated below:
3.3.1 Mean of Acceleration ( ¯a)
It represents the average of acceleration in both trans-
verse and longitudinal directions (d) defined in g and
shown in Equation (1).
¯
A
(d)
=
1
n
n
∑
i=1
a
i
(1)
Where n is the number of samples in the epoch
and a
i
is the acceleration sample.
3.3.2 Mean of Absolute Difference (MAD)
It describes the mean distance of data points about the
mean in both transverse and longitudinal directions
(d) defined in g and shown in Equation (2).
MAD
(d)
=
1
n
n
∑
i=1
|r
i
− ¯r| (2)
Where n is the number of samples in the epoch, r
i
is the i
th
resultant sample within the epoch and ¯r is the
mean resultant value of the epoch.
3.3.3 Posture Difference (∆P)
It represents the difference in average acceleration
¯
A
(T )
and
¯
A
(L)
defined in g
2
as shown in Equation (3).
We designated ∆P as Posture Difference between time
t and t − 1.
∆P
t
= (
¯
A
(T )
t
−
¯
A
(T )
t−1
)
2
+ (
¯
A
(L)
t
−
¯
A
(L)
t−1
)
2
(3)
Where
¯
A
(T )
is the average acceleration in the
transverse direction, and
¯
A
(L)
is the average acceler-
ation in the longitudinal direction.
3.4 Detection Algorithm
According to the position of the accelerometer in-
stalled in the wearable device illustrated in Figure 4,
the y-axis will represent the transverse direction and
the z-axis will represent the longitudinal direction.
When stationary, the acceleration over the z-axis is
equal to the gravitational force (+1g), and it should
be (0g) on the y-axis. Thus, the value of the z-axis
should be positive in SP, and negative in PP. On the
other hand, the value of the y-axis should be posi-
tive when moving right and negative when moving
left. Ideally, when moving to the LLP, the acceler-
ation over the y-axis should be equal to (−1g) and
(0g) in the z-axis. Alternately, when moving to the
RLP, the acceleration over the z-axis should be equal
to (+1g) and (0g) in the y-axis.
Figure 4: Positioning of SleepPal wearbale device.
The signal of ∆P and MAD
(d)
in both directions
during a transition or a rollover corresponds to an in-
crease in both values since MAD
(d)
is influenced by
the movement intensity and ∆P expresses the differ-
ence in posture between time t and t − 1. Signals of
the above features were exploited experimentally in
order to define and derive the below threshold values:
• Upper Posture value (U
∆P
): corresponds to the
lowest upper peak value of ∆P recorded.
• Upper MAD
(T )
Transversal value (U
MAD
(T )
): cor-
responds to the lowest upper peak value of
MAD
(T )
recorded.
• Upper MAD
(L)
Longitudinal value (U
MAD
(L)
): cor-
responds to the lowest upper peak value of
MAD
(L)
recorded.
The perfect lateral position is hard to achieve
therefore we defined two additional thresholds:
• Upper
¯
A
(L)
in both lateral postures (U
¯
A
(L)
): corre-
sponds to the highest value of
¯
A
(L)
in the lateral
position.
• Lowest
¯
A
(L)
in both lateral postures (L
¯
A
(L)
): cor-
responds to the Lowest value of
¯
A
(L)
in the lateral
posture.
Thus, a transition is detected when ∆P, MAD
(T )
and MAD
(L)
are higher than the defined thresholds as
described in Equation (4):
∆P
t
> U
∆P
MAD
(T )
> U
MAD
(T )
MAD
(L)
> U
MAD
(L)
(4)
To classify the transition upon detecting a move-
ment, we used
¯
A
(T )
t
,
¯
A
(L)
t
, and
¯
A
(L)
t−1
. The pattern in
each transition is described in Table 1.
The proposed algorithm will use the peaks of the
posture difference ∆P, MAD
(T )
, and MAD
(L)
to de-
tect body transitions and rollovers. Upon detecting a
SleepPal: A Sleep Monitoring System for Body Movement and Sleep Posture Detection
43

Table 1: Body transition matrix.
↱
SP PP LLP RLP
SP
NA NA
¯
A
(L)
t
↘
¯
A
(T )
t
↘
¯
A
(L)
t−1
> U
¯
A
(L)
¯
A
(L)
t
↘
¯
A
(T )
t
↗
¯
A
(L)
t−1
> U
¯
A
(L)
PP
NA NA
¯
A
(L)
t
↗
¯
A
(T )
t
↘
¯
A
(L)
t−1
< L
¯
A
(L)
¯
A
(L)
t
↗
¯
A
(T )
t
↗
¯
A
(L)
t−1
< L
¯
A
(L)
LLP
¯
A
(L)
t
↗
¯
A
(T )
t
↗
L
¯
A
(L)
<
¯
A
(L)
t−1
< U
¯
A
(L)
¯
A
(L)
t
↘
¯
A
(T )
t
↗
L
¯
A
(L)
<
¯
A
(L)
t−1
< U
¯
A
(L)
NA NA
RLP
¯
A
(L)
t
↗
¯
A
(T )
t
↘
L
¯
A
(L)
<
¯
A
(L)
t−1
< U
¯
A
(L)
¯
A
(L)
t
↘
¯
A
(T )
t
↘
L
¯
A
(L)
<
¯
A
(L)
t−1
< U
¯
A
(L)
NA NA
body movement, the algorithm will compute the dif-
ference in signals for
¯
A
(T )
and
¯
A
(L)
in order to deter-
mine the signal behavior. Finally, the algorithm will
compare the signal patterns with the matrix of pattern
behaviors presented in Table 1 in order to identify the
transition type and the current sleep posture.
4 EXPERIMENTAL EVALUATION
The system was evaluated on data collected in labora-
tory. Experiments were conducted on 10 volunteering
subjects aging between 18 and 40 and weighting from
52 to 106kg. The device was attached to the center of
the chest. The volunteers didn’t report any discom-
fort in wearing the device. Each subject simulated all
sleep movements five times. Thus, each subject per-
formed 40 transitions and each posture transition is
performed 50 times. In order to confirm the volun-
teer’s posture, we installed a video camera above the
bed and recorded the body movements.
Figures 5, 6, 7, and 8 show the signals recorded
during body movements transitioning contrariwise
from SP to LLP, from SP to RLP, from PP to LLP, and
from PP to RLP respectively. As shown, during any
body movement, a peak of ∆P, MAD
(T )
, and MAD
(L)
are recorded simultaneously. The signals of
¯
A
(T )
and
¯
A
(L)
differ according to the transition.
The signals of the
¯
A
(L)
t
and
¯
A
(T )
t
directions cor-
respond to a decrease in both values during SP to
LLP and RLP to PP transitions. This decrease is due
to rotational motion to the left. In order to distin-
guish between these transitions, we used the
¯
A
(L)
t−1
to
identify the previous posture. Similarly, from the SP
to LLP transition, the
¯
A
(L)
t−1
value should be (+1g)
which is greater than U
¯
A
(L)
recorded in lateral pos-
tures, whereas in the RLP to PP transition, the
¯
A
(L)
t−1
should be between L
¯
A
(L)
and U
¯
A
(L)
. Contrarily, the sig-
nals observed in LLP to SP and PP to RLP correspond
to an increase in both values but in the first transition,
the
¯
A
(L)
t−1
should be between L
¯
A
(L)
and U
¯
A
(L)
and in
the second transition it should be less than L
¯
A
(L)
. An
increase in
¯
A
(L)
t
along with a decrease in
¯
A
(T )
t
are ob-
served in RLP to SP and PP to LLP transitions.
¯
A
(L)
t−1
should be between L
¯
A
(L)
and U
¯
A
(L)
in the first transition
and less than L
¯
A
(L)
in the second. Finally, a decrease
in
¯
A
(L)
t
with an increase in
¯
A
(T )
t
are observed in SP
to RLP and LLP to PP transitions.
¯
A
(L)
t−1
should be
greater than U
¯
A
(L)
in the first transition and between
L
¯
A
(L)
and U
¯
A
(L)
in the second.
Table 2 shows the detection results of the proposed
algorithm. Since we considered any body movement
is a rollover, the total number of rollovers is 400.
The proposed algorithm detected a 352 rollovers con-
firmed to be correct. Consequently, 48 rollovers were
undetected (false negative) and a total of 30 false pos-
itive detections were recorded. The efficacy and ro-
bustness of our algorithm are evaluated by measur-
ing both the sensitivity (i.e. Detected rollovers over
the total of number of rollovers) and the accuracy (i.e.
Ability of the system to detect the rollovers) which are
recorded to be equal to 88% and 82% respectively.
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
44
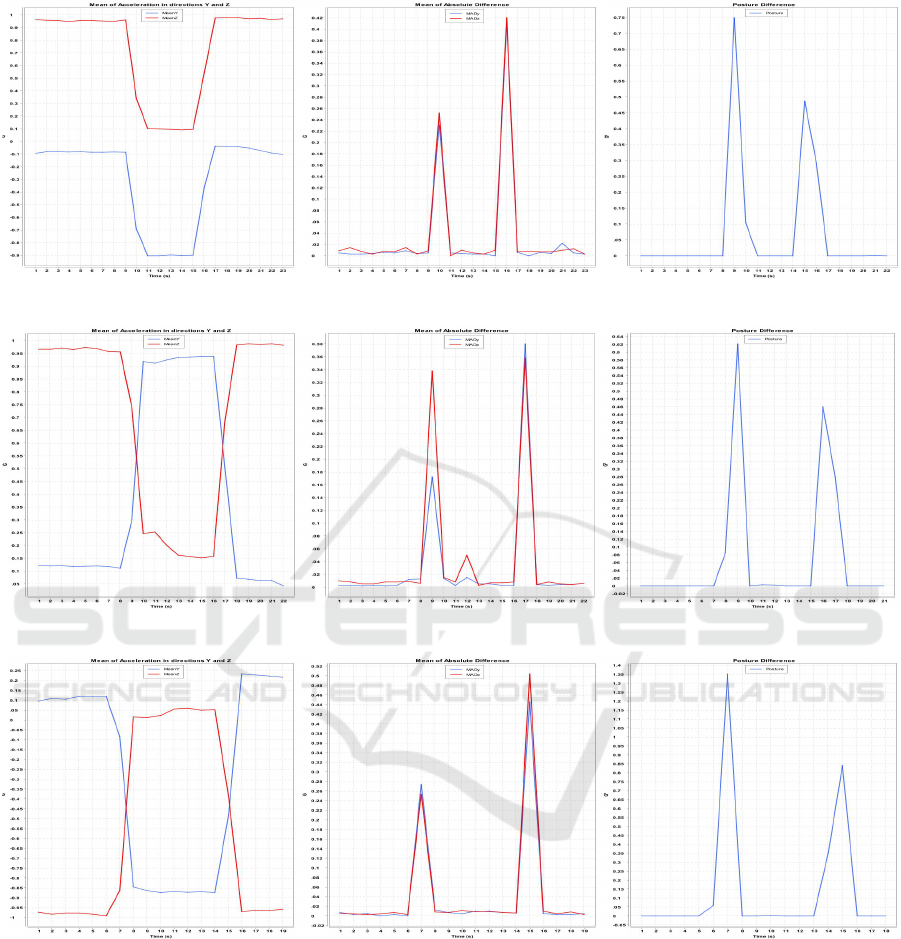
Figure 5: Signals during movement from SP to LLP and vice versa.
Figure 6: Signals during movement from SP to RLP and vice versa.
Figure 7: Signals during movement from PP to LLP and vice versa.
5 SLEEP QUALITY EVALUATION
Human sleep can be classified into Rapid Eye
Movement (REM) and Non-Rapid Eye Movement
(NREM). The latter is further divided into three
stages, N1-N3. Each stage of sleep includes varia-
tions in the brain wave pattern and eye movements.
The body cycles through all of these stages approxi-
mately 4 to 6 times each night, averaging 90 minutes
for each cycle (Memar and Faradji, 2017). REM and
N1 stages are the lightest sleep, while N3 stage is the
deepest sleep. In general, body movements increase
during light sleep and decrease during deep sleep.
Thus, the sleep can be classified into two stages, deep
sleep and light sleep based on the frequency of body
transitions detected. Hence, and upon detecting a
body transition, SleepPal will record the time and will
compare it to the time of the previously recorded body
transition. Consequently, the interval between body
transitions is computed and compared to a threshold
SleepPal: A Sleep Monitoring System for Body Movement and Sleep Posture Detection
45

Figure 8: Signals during movement from PP to RLP and vice versa.
Table 2: Results of the detection algorithm.
# Posture Transitions Detection
1 SP → LLP 46/50
2 SP → RLP 47/50
3 LLP → SP 45/50
4 RLP → SP 45/50
5 PP → LLP 43/50
6 PP → RLP 43/50
7 LLP → PP 42/50
8 RLP → PP 41/50
as shown in Equation (5).
DeepSleep = BM
t
− BM
t−1
≥ time
th
LightSleep = BM
t
− BM
t−1
< time
th
(5)
Where BM
t
and BM
t−1
are the body movements
at times t and t − 1 respectively. time
th
is the time
threshold equal to 20 minutes according to (Miwa
et al., 2007).
The time of each sleep stage will be recorded in
order to evaluate the sleep quality. The latter is de-
pending on several factors such as genetics, sleep
habits, medical problems, and essentially sleep depth
which is considered the most important in evaluating
sleep quality. Thus, we determined the sleep quality
in term of the sleep depth according to Equation (6)
as follows:
QI
SleepQuality
=
d
DeepSleep
d
Total
(6)
Where QI
SleepQuality
is the sleep Quality Index,
d
DeepSleep
is the duration of the deep sleep stage, and
d
Total
is the total sleep duration.
6 CONCLUSION
In this paper, we developed a body movement and
body posture classifier using an accelerometer device
attached to the center of the chest. The proposed sys-
tem is based on a simple threshold algorithm and uses
multiple features extracted from the raw acceleration
data. The efficacy and robustness of our algorithm are
evaluated by measuring both the sensitivity and the
accuracy which were recorded to be equal to 88% and
82% respectively. In order to evaluate the sleep qual-
ity, we distinguished between deep sleep and light
sleep using a simple threshold-based equation. Our
proposed sleep monitoring system can be used for
monitoring sleep quality in hospitals by interfacing it
with the existing nurse call system.
Further research will exploit the limitations of the
device in settings where sliding in bed remains un-
detected and motion noise caused by the fixation of
the sensor must be removed. We will also emphasize
the relationship between sleep quality, sleep disorders
and nocturnal falls.
REFERENCES
Acharya, J. (2020). Design and development of a method
for detecting sleep roll-over counts using accelerom-
eter adxl335. International Journal of Electrical and
Computer Engineering (IJECE), 10:477.
Adami, A., Singer, C., Hayes, T., and Pavel, M. (2008).
A system for unobtrusive monitoring of mobility in
bed. Proceedings of the 11th IEEE International Con-
ference on Computational Science and Engineering,
CSE Workshops 2008, pages 13 – 18.
Beattie, Z., Hagen, C., and Hayes, T. (2011). Classification
of lying position using load cells under the bed. Con-
ference proceedings : ... Annual International Confer-
ence of the IEEE Engineering in Medicine and Biol-
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
46

ogy Society. IEEE Engineering in Medicine and Biol-
ogy Society. Conference, 2011:474–7.
Cartwright, R. (1984). Effect of sleep position on sleep ap-
nea severity. Sleep, 7:110–4.
Colman, A. (2006). A Dictionary of Psychology. Oxford
University Press.
De Koninck, J., Gagnon, P., and Lallier, S. (1983). Sleep
positions in the young adult and their relationship with
the subjective quality of sleep. SLEEP, 6:52–59.
Hoffstein, V. (1996). Snoring. chest, 109:201–22.
Hoque, E., Dickerson, R., and Stankovic, J. (2010). Mon-
itoring body positions and movements during sleep
using wisps. Proceedings - Wireless Health 2010,
WH’10, pages 44–53.
Horne, R., Franco, P., Adamson, T., Groswasser, J., and
Kahn, A. (2002). Effects of body position on sleep
and arousal characteristics in infants. Early human
development, 69:25–33.
Ibrahim, A., Chaccour, K., Hassani, A. H. E., and An-
dres, E. (2021). Bed-fall detection and prediction:
A generic classification and review of bed-fall related
systems. IEEE Sensors Journal, 21(5):5678–5686.
Kupfer, D., Detre, T., Foster, G., Tucker, G., and Delgado,
J. (1972). The application of delgado’s telemetric mo-
bility recorder for human studies. Behavioral biology,
7:585–90.
Lee, J., Hong, M., and Ryu, S. (2015). Sleep monitoring
system using kinect sensor. International Journal of
Distributed Sensor Networks, 2015:1–9.
Leung, R., Bowman, M., Parker, J., Newton, G., and
Bradley, T. (2003). Avoidance of the left lateral decu-
bitus position during sleep in patients with heart fail-
ure: Relationship to cardiac size and function. Journal
of the American College of Cardiology, 41:227–30.
Memar, P. and Faradji, F. (2017). A novel multi-class eeg-
based sleep stage classification system. IEEE Trans-
actions on Neural Systems and Rehabilitation Engi-
neering, PP:1–1.
Miwa, H., Sasahara, S., and Matsui, T. (2007). Roll-
over detection and sleep quality measurement using
a wearable sensor. Conference proceedings : ... An-
nual International Conference of the IEEE Engineer-
ing in Medicine and Biology Society. IEEE Engi-
neering in Medicine and Biology Society. Conference,
2007:1507–10.
Nam, Y., Kim, Y., and Lee, J. (2016a). Sleep monitoring
based on a tri-axial accelerometer and a pressure sen-
sor. Sensors (Basel, Switzerland), 16.
Nam, Y., Kim, Y., and Lee, J. (2016b). Sleep monitoring
based on a tri-axial accelerometer and a pressure sen-
sor. Sensors, 16:750.
Sadeh, A., Hauri, P., Kripke, D., and Lavie, P. (1995). The
role of actigraphy in the evaluation of sleep disorders.
SLEEP, 18:288–302.
SleepPal: A Sleep Monitoring System for Body Movement and Sleep Posture Detection
47
