
Development of a Web-based Program for Personalized Physical
Exercise for Older Adults
Frederico Baptista
1a
, Bárbara Ursine
1b
, Ana Isabel Martins
2c
, Rosa Andias
1d
, Joana Pais
3e
,
Anabela G. Silva
2f
and Nelson Pacheco Rocha
1g
1
IEETA, Department of Medical Sciences, University of Aveiro, Aveiro, Portugal
2
Centesis.UA@RISE, Health Sciences School, University of Aveiro, Aveiro, Portugal
3
Neuroinova, EPIUnit, Institute of Public Health, University of Porto, Porto, Portugal
joanapais@neuroinova.com
Keywords: Older Adults, Web-based Application, Physical Activity, Physical Exercise.
Abstract: Information technologies support personalized strategies to promote the effectiveness of physical exercise
programs. The study reported by this paper developed a web-based program for personalised physical exercise
for community dwelling older adults. Considering the Medical Research Council framework for developing
and evaluating complex interventions, the paper reports the results of the development phase, which is the
first phase of this framework. The development phase included the identification of the existing evidence, the
identification of the developing theory, and the modelling of the intervention. The developed program and
respective web-based application integrate the inherent complexity of physical exercise programs and allow
the definition of personalized prescriptions considering a diverse range of factors (i.e., frequency, intensity,
time, type, volume, and progression) recommended by international guidelines.
1 BACKGROUND
Accidental falls and fall-related injuries are major
problems among older adults and put them at higher
risk of functional limitations, disabilities, and even
death (Kannus, Sievänen, Palvanen, Järvinen &
Parkkari, 2005). Specifically, in the European Union,
between 2010 and 2012, there were, approximately,
3,750,000 admissions to hospitals related to falls each
year (Turner, Kisser & Rogmans, 2015).
The risk of falls is related to the environment (e.g.,
architectural barriers, such as poor lighting or
slippery surfaces), behaviours (e.g., nutritional habits
or consumption of alcohol and tobacco), and
limitations of physical performance, such as poor
muscle strength and balance, or functional, cognitive,
and sensory impairment (Turner et al., 2015). Since
a
https://orcid.org/0000-0003-1842-6539
b
https://orcid.org/0000-0001-5308-8411
c
https://orcid.org/0000-0002-5220-0528
d
https://orcid.org/0000-0003-2419-5642
e
https://orcid.org/0000-0003-4663-8184
f
https://orcid.org/0000-0002-4386-5851
g
https://orcid.org/0000-0003-3801-7249
physical activity contributes to increase or maintain
physical performance, several guidelines (e.g.,
(Ferguson, 2014; Committee PAGA, 2018; US
Department of Health and Human Services, 2018;
World Health Organization, 2020; Izquierdo et al.,
2021)) establish recommendations for exercises that
increase endurance and flexibility, strengthen
muscles, and improve balance, aiming to prevent falls
and promote a healthy living (Vozzi et al., 2022).
The remote control offered by information
technologies, namely web-based or mobile
applications and ambient assisted living systems
(Queirós et al., 2015), constitute a potential facilitator
for the dissemination of physical exercise programs
(Vozzi et al., 2022).
Since the effectiveness of exercise programs at
distance for older adults requires further research, this
Baptista, F., Ursine, B., Martins, A., Andias, R., Pais, J., Silva, A. and Rocha, N.
Development of a Web-based Program for Personalized Physical Exercise for Older Adults.
DOI: 10.5220/0011982200003476
In Proceedings of the 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2023), pages 221-229
ISBN: 978-989-758-645-3; ISSN: 2184-4984
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
221

paper reports on the development of a web-based
program for personalized physical exercise for
community dwelling older adults. This development
was performed in the context of the project Built
Environments for an Active, Safe, and Healthy Life
(Ambientes Construídos para uma Vida Ativa, Segura
e Saudável - ACTIVAS).
2 METHODS
In 2000, the Medical Research Council (MRC)
introduced a framework to guide the development and
evaluation of complex interventions (Medical
Research Council, 2000), being complex
interventions defined as interventions with more than
one component (e.g., what practitioners and patients
should do).
The 2000 version of the MRC framework had
some limitations due to its similarity to those used to
guide the development of drugs. Consequently, a
revised version was published in 2008 (Craig et al.,
2008), which proposed four phases with no linear or
cyclic order:
Development – systematization of the
theoretical understanding of the intervention,
the outcomes that are expected, and the specific
approaches to achieve these outcomes
considering the current scientific evidence.
Feasibility and pilot – determination of
acceptability, compliance, delivery of the
intervention, recruitment, and retention, as well
as unexpected side effects not predicted during
the development phase.
Evaluation – assessment of the effectiveness of
the intervention, namely by conducting
randomized controlled trials.
Implementation – Dissemination of the
intervention and its results to be reliably
replicated in uncontrolled settings over the long
term.
This paper reports on the development phase of a
web-based program for personalized physical
exercise for community dwelling older adults.
According to the MRC framework, the development
phase was decomposed into three steps:
Identifying the existing evidence – a literature
review was performed, which included existing
guidelines of recommended physical activity
(e.g., (Ferguson, 2014; Committee PAGA,
2018; US Department of Health and Human
Services, 2018; World Health Organization,
2020; Izquierdo et al., 2021)) and systematic
reviews related to the implementation of
physical activity and physical exercise
programs (e.g., (Sherrington et al., 2020; Di
Lorito et al., 2021; Rodrigues, Domingos,
Monteiro & Morouço, 2022)).
Identifying the developing theory –
considering the results of the literature review,
a schematic model of the intervention was
prepared to systematize target behaviour,
intervention components, and long-term
outcomes.
Modelling the intervention – the
responsibilities of the practitioner and the
actions of the participant were identified, as
well as the nature of the exercises and the
methods of organizing and delivering these
exercises. Moreover, practicalities and the
concrete structure of the intervention were
developed and refined, including the
information models of the physical exercise
program and exercises, interfaces of the
proposed web-based application, and a
preliminary exercise set.
Modelling the intervention might include studies
to progressively refine the design before embarking
on a full-scale evaluation (Craig et al., 2008).
Therefore, in the near future, practitioners and
potential participants will be involved in a focus
group and a usability study to assess respectively the
practitioner and participant instructions and the
adequacy of the proposed practitioner and participant
user interfaces to identify and surpass potential
drawbacks.
3 RESULTS
This section reports the results of the three steps of
the MRC development phase, as stated in the
Methods section.
3.1 Identifying the Existing Evidence
Although physical activity has been identified as a
protective factor against physical and cognitive
decline, cardiorespiratory, metabolic and immune
systems’ dysregulation, mental illness and falls
(Committee PAGA, 2018), a large percentage of
older adults have a sedentary behaviour defined as
spending more than 5.5h per day sitting at work or
driving, sitting at home while watching TV, reading,
eating, or sitting at a desk (Remón, Díaz-Benito,
Beatty & Lozano, 2020).
Physical activity is defined as any activity that
incorporates bodily movement produced by muscle
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
222

contraction and that requires an increase in energy
expenditure relative to the resting condition
(Caspersen, Powell & Christenson, 1985; Ferguson,
2014). In turn, physical exercise is defined as a
subtype of physical activity, which is planned,
structured, repetitive, and purposeful to preserve or
improve skill-related components of physical fitness
(Caspersen et al., 1985; Ferguson, 2014).
Physical exercise can be performed in several
settings, from clinical to home settings, supervised or
not, in an individual or group format (US Department
of Health and Human Services, 2018), being the most
important aspect, the motivation of the participant. In
this sense, physical exercise performed by a group has
been recommended as a facilitator of adherence by
older adults when compared to exercise performed
alone at home (Di Lorito et al., 2021).
To guarantee the various aspects to consider when
prescribing an exercise program, the American
College of Sports Medicine (ACSM) proposed the
Frequency, Intensity, Time, Type, Volume, and
Progression (FITT-VP) principles (Ferguson, 2014;
Bushman, 2018). Specifically, (i) frequency defines
how often are the physical exercises done each week
(Bushman, 2018), (ii) intensity defines how hard is
the physical exercise (e.g., very light, light, moderate
or vigorous) (Bushman, 2018), (iii) time represents
the duration of an exercise modality within a session,
as well as, the total duration of an physical exercise
program, (iv) type defines the modality of a physical
exercise, being an exercise modality a category that
encompasses exercises with a common primary goal
related to a specific health or skill component of
physical fitness (Caspersen et al., 1985), (v) volume
represents the total amount of physical exercise
(Bushman, 2018), and (vi) progression characterizes
how the physical exercise program is advanced
(Bushman, 2018).
Considering the type of exercise or modalities,
mobility exercises refer to an exercise set that
explores the maximum range of motion available in a
joint (Kisner & Colby, 2009). They aim to preserve
or improve the range of motion to allow a body
segment to have more freedom of movement to
perform functional tasks (Kisner & Colby, 2009).
These exercises may include movements to improve
the range of motion in a specific joint, as well as to
promote the participant’s ability to transfer from one
body position to another (e.g., lying to sitting or
sitting to standing).
In turn, resistance exercises require muscle
contraction against an external resistance or weight,
which can be the body itself (or just part of it) to
increase muscle mass and strength (American
College of Sports Medicine, 2009; Rodrigues et al.,
2022). There are different types of resistance
exercises including muscle strength (i.e., to improve
the muscle´s ability to exert force), endurance (i.e., to
improve the ability of muscles to exert external force
for many repetitions), and power (i.e., the ability to
exert muscle force at high speed) (Caspersen et al.,
1985; Ferguson, 2014; Rodrigues et al., 2022).
Moreover, balance exercises aim to assure the
ability to maintain the equilibrium, while stationary
(i.e., static balance) or moving (i.e., dynamic
balance), while flexibility exercises play an important
role in functional mobility, as they encompass
movements/postures to improve or maintain the
extensibility of soft tissues that cross or surround the
joints.
Finally, aerobic exercises (American College of
Sports Medicine, 2009; Ferguson, 2014) aim to
improve cardiovascular endurance, and should
incorporate exercises such as walking, running,
cycling, and dancing (Ferguson, 2014; US
Department of Health and Human Services, 2018) to
increase heart rate and optimize the venous return.
A recent systematic review comprising more than
one hundred studies and twenty-five thousand
participants showed that general physical activity
reduces the rate of falls by 23% when compared with
control and that this ratio increases up to 28% when
multiple modalities of exercise are included
(Sherrington et al., 2020).
Independently of the exercise modalities, warm-
up and cool-down exercises should be performed
before and after the conditioning phase, respectively,
allowing a gradual increase in heart and respiratory
rate and facilitating the return of the participant to
baseline activity, respectively (US Department of
Health and Human Services, 2018).
3.2 Identifying the Developing Theory
Figure 1 presents a schematic model of the
intervention supported by the web-based program for
personalized physical exercise for older adults. This
model highlights target behaviour, intervention
components, and long-term outcomes.
The intervention aims to promote the practice of
physical exercise and has four main components:
Initial functional assessment – the intervention
begins with the initial functional assessment of
the participant performed by the practitioner,
which is essential to define a personalized
exercise program.
Prescription – the exercise program is
materialized in a variable number of exercises
Development of a Web-based Program for Personalized Physical Exercise for Older Adults
223
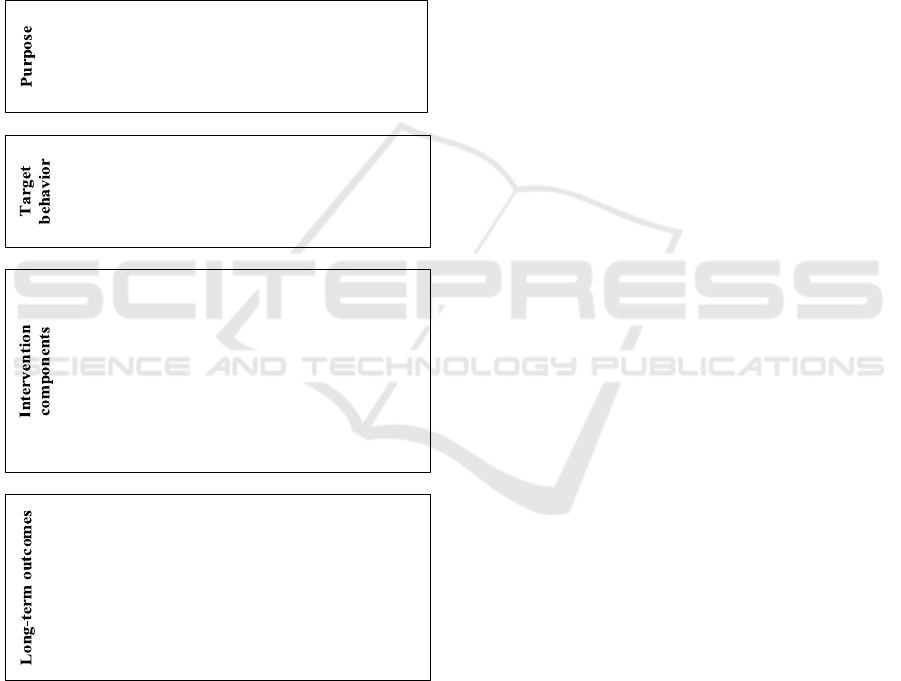
that must be structured according to a specific
prescription protocol. This prescription is
supported by the practitioner interface of the
web-based application. In addition to the type
and number of exercises, the prescription also
comprises additional parameters related to
frequency, intensity, time or duration, volume,
and progression of the exercises.
Implementation – the exercise program is
performed remotely by the participant with the
support of the web-based application. This
presents the exercises and respective
instructions and gathers the participant
feedback.
Figure 1: Schematic model of the physical exercise
intervention.
Supervision – periodically, the practitioner
performs an assessment of the participant and
an analysis of the respective progression to
determine if it is necessary to adjust the initial
prescription.
Considering the long-term outcomes, the web-
based physical exercise program aims to promote
adherence to the practice of physical exercise by older
adults. This adherence not only promotes functional,
cognitive, musculoskeletal, and cardiovascular
benefits but also helps to prevent falls and fall-related
injuries (Fragala et al., 2019). This means that long-
term outcomes include functional, cognitive,
musculoskeletal, and cardiovascular benefits, as well
as falls and fall-related injuries prevention, which,
consequently, might reduce the use of healthcare
resources.
3.3 Modelling the Intervention
Based on the existing evidence and the identified
developing theory, information models for both the
physical exercise program and the individual
exercises that constitute it were defined. These
supported the development of the web-based
application, both in terms of the practitioner and the
participant interaction. Moreover, a preliminary
exercise set was created.
3.3.1 Modelling the Exercise Program
A physical exercise program is composed by a
variable number of exercises that must be structured
according to a specific prescription protocol, which,
as already mentioned, defines the frequency,
intensity, time, type, volume, and progression of the
exercises.
The program duration together with frequency
(i.e., the number of sessions per week) determines the
total number of sessions. In turn, the sessions are
composed of sets of exercises, although a period of
rest is recommended between two consecutive sets of
exercises.
Moreover, there are different types of exercises
(i.e., modalities). Independently of the respective
modality, each exercise might be repeated and
progressed as appropriate to each participant.
The progression of exercise might be
operationalized by manipulating diverse parameters,
such as speed, load, type of contraction (e.g., isotonic,
or isometric), type of resistance (e.g., body weight or
external resistance), base of support (e.g., feet
position) or a combination of these, considering the
specificities of the different exercise modalities and
the characteristics of the individuals. However,
having too many parameters to characterize each
physical exercise makes the prescribing process
difficult, time-consuming, and error prone. To
overcome this drawback, the proposed information
• To develop a web-based program for
personalized physical exercise.
• Practice of physical exercise.
• Initial functional assessment.
• Prescription of the physical exercise
program.
• Implementation of the physical exercise
program.
• Supervision of the implementation of the
physical exercise program.
• Adherence to the practice of physical
exercise.
• Functional, cognitive, musculoskeletal, and
cardiovascular benefits.
• Prevention of falls and fall-related injuries.
• Reduction in health care resources use.
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
224
exercise model defines that each exercise has
different difficulty levels, which abstracts the
configuration parameters. For instance, Table 1
illustrates the use of speed, surface incline, body
weight, additional weight, coordination element, and
feet position to distinguish difficulty levels of an
aerobic exercise (i.e., walking), a resistance exercise
(i.e., hip abductors strengthening), and a balance
exercise (i.e., calf raises).
Finally, each exercise difficulty level must have
instructions (i.e., both instructions to the practitioner
and participant).
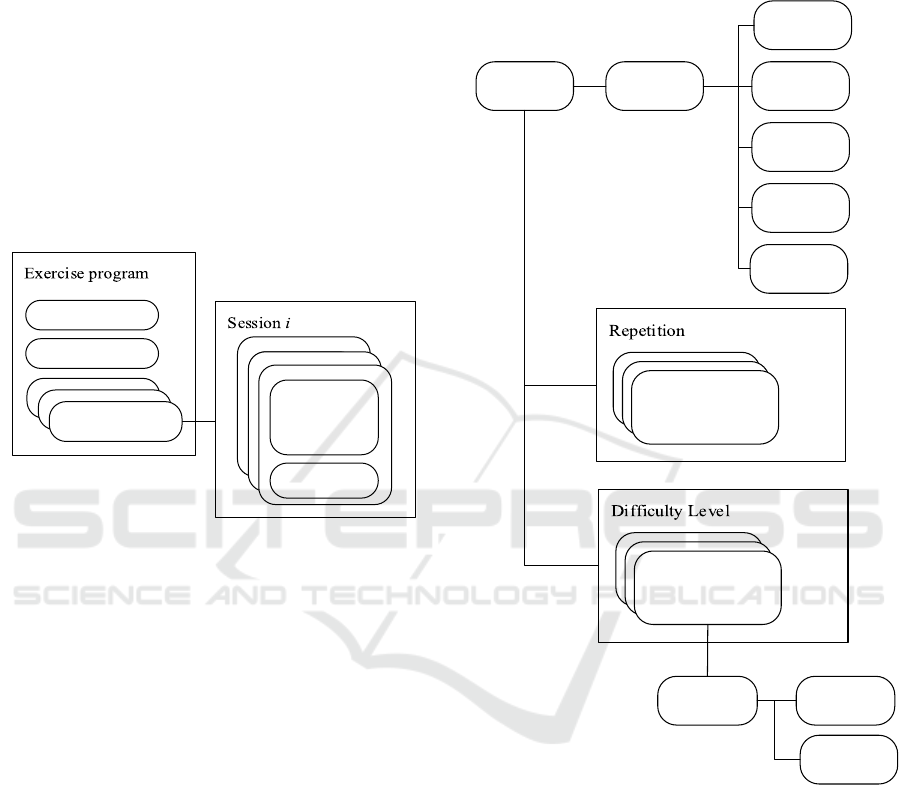
Figures 2 and 3 formalize the information models
of both the program (Figure 2) and the physical
exercise (Figure 3).
Figure 2: Information model of the physical exercise
program.
The physical exercise program (Figure 2) has a
duration and a frequency, which are translated into
sessions 1 to i. Each session has 1 to j exercise sets,
and after each exercise set, there might be a rest
period.
In turn, each exercise (Figure 3) is associated with
one of the following modalities, according to its
characteristics: (i) mobility training; (ii) resistance
training; (iii) balance training; (iv) flexibility training;
and (v) aerobic training. Moreover, a particular
exercise might be repeated (i.e., 1 to k repetitions) and
has 1 to l difficulty levels.
Finally, for each difficulty level of each exercise,
instructions need to be prepared for both the
practitioner and participant, which contain textual,
graphical, and video information.
The practitioner’s instructions include:
Joint name (only for exercises involving more
than one joint).
Starting position (in the case of exercises
performed in a standing position, it should be
specified whether the exercise should be done
with or without hand support).
Inclusion of progression parameters as
mentioned before, when applicable.
Description of the movements with reference to
the joints involved (if necessary).
Figure 3: Information model of the physical exercise.
Table 2 presents an example of the instructions for
the practitioner of a mobility exercise (i.e., ankle
mobility) with four difficulty levels.
On the other hand, the instructions for the
participant must include the material that is required
to carry out the exercise (e.g., additional weight), a set
of safety instructions (e.g., 'place the chair against a
wall so that it doesn't move' or 'support both feet on
the floor shoulder-width apart, torso straight and look
straight ahead') and specific instructions for carrying
out the exercise.
Set of
Exercices k
Rest in
between
Set of
Exercices k
Rest in
between
Exercise set j
Rest between
exercise sets
Duration
Frequency
Session i
Exercise Modality
Mobility
Resistance
Balance
Level l
Repetition k
Instructions Practitioner
Participant
Flexibility
Aerobic
Development of a Web-based Program for Personalized Physical Exercise for Older Adults
225

Table 1: Examples of parameters that might be used to
distinguish the difficulty levels of walking, hip abductors
strengthening, and calf raises exercises.
Difficult
y
Level Parameters
Walkin
g
Walkin
g
slowl
y
(
flat surface
)
Speed.
Walking at a speed of 5km/h (flat
surface
)
Walking at a moderate pace
carrying a light weight of no more
than 4.5 k
g
(
flat surface
)
.
Surface
inclination and
additional weight.
Walking at a moderate pace
carrying a light weight between
4.5 and 19 kg (inclined surface).
Hip abductors strengthening
Isotonic contraction, body weight,
with support and without
coordination element.
Resistance (body
weight)
Isotonic contraction, external
resistance, with support and
without coordination element.
Isotonic contraction, external
resistance, without support and
without coordination element.
Coordination
element.
Isotonic contraction, external
resistance, without support and
without coordination element.
Calf
r
aises
Feet hip-width apart, hands
support and without coordination
element.
Feet position.
Feet together, hands support and
without coordination element.
Table 2: Instructions for the practitioner of the ankle
mobility exercise.
Difficulty
Level
Instruction
1 Ankle plantar /dorsal flexion: sitting
p
osition.
2 Ankle circumduction: sitting position.
3 Ankle circumduction: standing position.
Supported hands. hip and knee flexion
from 45° to 90°.
4 Simultaneous hip, knee and ankle flexion:
standing position. Supported hands.
Simultaneous hip, knee, and ankle flexion,
followed by maximum extension of the
knee and tibiotarsal to the
g
round.
Concerning the specific instructions, these
include guidance regarding:
Information about the initial position, namely
the alignment of the upper or lower limbs. In
the case of exercises performed in a standing
position with single leg support, specify
whether it should be done with or without hand
support.
Movement guidelines (e.g., breath control to
facilitate the performance of certain exercises).
In situations where the participant must always
return to the initial position before performing
the next repetition, this information must come
before the information about the number of
repetitions to be performed.
Table 3 presents the specific instructions for the
participant of the aforementioned ankle mobility
exercise.
Finally, it should be noted that the textual
instructions of Tables 2 and 3 are complemented with
figures and videos. The videos will be presented and
repeated while the participant is performing the
exercises.
3.3.2 Practitioner Console
The practitioner console allows the definition of
personalised prescriptions including the choice of the
intended modality, the exercises within each
modality, the level of difficulty of each one of them,
the number of repetitions to be performed for each
exercise, as well as the respective duration. This
structure provides the module responsible for the
participant interaction all the information that is
required to present the sequence of exercises and
respective repetitions according to the prescription
characteristics (i.e., frequency, intensity, time, type,
volume, and progression).
3.3.3 Participant Interaction
The participant interaction is divided into three main
components:
Session preparation – the application
determines if there is a prescription containing
at least one open session. If this is not the case,
the participant is informed that there are no
exercises available. Otherwise, the application
displays an introductory screen with
information about the next exercise to be
performed.
Session realization – the web-based application
supports the participant during the realization
of the physical exercise. While there is a
session with exercises to be performed and the
participant wishes to continue, the application
will repeat the following actions: (i) determines
the next exercise and presents the respective
instruction; (ii) after the indication that the
participant wants to start, repeats the video with
the exercise instructions the prespecified
number of repetitions; (iii) waits for the
indication that the participant has finished the
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
226

exercise; and (iv) if there is an indication for a
period of rest after the completion of the
exercise, transmits this indication to the
participant.
Session closure – the session ends when there
are no more exercises to be performed or the
participant does not wish to continue. When
this happens, the application gathers the
participant feedback (e.g., the Borg Rating of
Perceived Exertion Scale).
Table 3: Specific instructions for the participant to carry out
the ankle mobility exercise.
Difficulty
Level
Instruction
1 Sitting: straighten your right knee. In this
position, move your toes up and down as
far as you can. After completing the set
number of repetitions, return to the
starting position and repeat the movement
to the left side.
2 Sitting: straighten your right knee. In this
position, make circles with the tip of your
foot (as big as you can). After completing
the set number of repetitions, return to the
starting position and repeat the movement
to the left side.
3 Standing: support yourself on a stable
surface (e.g., a wall). Raise the leg with the
knee straight to about 45 degrees. In this
position, make circles with the tip of your
foot (as big as you can). After completing
the set number of repetitions, return to the
starting position and repeat the movement
to the left side.
4 Standing: support yourself on a stable
surface (e.g., a wall). Raise the leg with the
knee straight to about 45 degrees. In this
position, make circles with the tip of your
foot (as big as you can). After completing
the set number of repetitions, return to the
starting position and repeat the movement
to the left side. Standing: Support yourself
on a stable surface (e.g., a wall). Raise
your right knee. In this position, pull the
ball of the foot up as far as you can. Then
lower the leg by straightening the knee and
bringing the toe down as far as you can.
After completing the set number of
repetitions, return to the starting position
and repeat the movement to the left side.
3.3.4 Preliminary Exercise Program
To assess the feasibility of the web-based program for
personalized physical exercise for community
dwelling older adults a set of 35 exercises was
prepared, each one with six difficulty levels. This set
includes mobility, resistance, balance, flexibility, and
aerobic exercises:
Mobility exercises – head and neck mobility
(sitting and standing), shoulder and arm
mobility (sitting and standing), trunk and spine
mobility, hip and knee mobility, or ankle
mobility.
Resistance exercises – hip abduction, hip
extension, sit-to-stand, squat, hip flexion, knee
extension, knee flexion, elbow flexion, lifting a
weight (sitting and standing), arm spread
(sitting and standing), squeezing a ball (sitting
and standing), pulling towel (sitting and
standing).
Balance exercises – Straight-line walking, heel
raises, or heel-walking are examples of static
balance exercises, while maintaining balance in
single-leg or two-leg positions are examples of
dynamic exercises.
Flexibility exercises – trunk and arm stretch,
pectoral stretch, quad stretch, hamstring
stretch, calf stretch, or wrist stretch.
Aerobic exercises – dance and aerobic step.
All the exercises considered have been applied in
different exercise programs for older adults, namely
face-to-face exercise programs performed in clinical
settings. However, since these exercises are intended
to be carried out remotely, a critical aspect to consider
is the suitability of the instructions provided.
Therefore, to assess the adequacy of the instructions
prepared for the different exercises of a preliminary
exercise program, a focus group was recently
approved by an ethics committee, involving potential
practitioners and participants to consolidate the
instructions provided by the web-based application.
4 DISCUSSION AND
CONCLUSION
There are many international guidelines on exercise
prescription for older adults (American College of
Sports Medicine, 2009; Ferguson, 2014; US
Department of Health and Human Services, 2018;
World Health Organization, 2020), which agree on
several recommendations, including the delivery
modes and the need to include different exercise
modalities and to establish a rate of progression.
However, they differ in terms of frequency, duration,
intensity, and the parameters to configure the
progression rates. This means that the prescription of
a physical exercise program must be flexible.
Development of a Web-based Program for Personalized Physical Exercise for Older Adults
227

The information models for both the program
(Figure 2) and the physical exercise (Figure 3) were
defined to integrate the inherent complexity of a
physical exercise program and to guarantee the
flexibility of the prescriptions by allowing their
personalization.
An aspect that deserved special attention was the
progression of the exercise program. The rate of
progression might be established by manipulating
diverse factors such as exercise duration, frequency,
and intensity, and by adding different elements
related to motor and cognitive function or integrating
multiple health- and skill-related components of
physical fitness simultaneously in the same exercise.
The literature is not clear about which progression
parameters should be used for each exercise modality,
but some parameters might be considered to assist the
prescription according to the plausibility of each
modality. For general mobility exercises, an example
of how the progression factors can be used is
performing the exercises in single or multiple
anatomical planes of movement, as well as choosing
to perform exercises involving one or more joints
(single-joint versus poly-joint movement) (Kisner &
Colby, 2009). Regarding resistance training, some
progression factors that can be explored are different
types of muscle contraction within the same exercise
(isotonic versus isometric versus isotonic/isometric
combination), using body weight or an external
resistance as a load, unstable surfaces, and the
velocity at which the movement is performed, and the
inclusion of a coordination element (Fragala et al.,
2019). Progression factors can also be included in
balance exercises, integrating the different systems
involved in the control of body balance, namely the
width of the base of support, external support, support
surface stability, sensory input, dynamic movements
that perturb the centre of gravity, coordinating
element, among others (Akerman, Gonçalves &
Perracini, 2011). In terms of flexibility exercises,
different body positions to stretch the same muscle
group can be used. When it comes to aerobic training,
there are a wide variety of progression factors that can
be used, depending on the type of cardiovascular
training chosen (Ferguson, 2014).
In the present study, the diversity of progression
factors was abstracted by difficulty levels, which
resulted from the instantiation of diverse parameters
such as speed, load, type of contraction, type of
resistance, type of support or coordination.
In terms of the instructions for a specific exercise,
each difficulty level must present instructions for the
practitioner and participant. The practitioner
instructions include, for instance, information related
to joint name, the starting position, the inclusion of
progression parameters and a description of the
movements with reference to the joints involved. In
turn, the instructions for the participant include the
identification of the material necessary to carry out
the exercise, safety instructions and specific
instructions related to the initial position, movement
guidelines, suggestion of specific positions or
alternative movements.
Finally, concerning the practitioner and
participant interaction, two different user interfaces
were defined (i.e., the prescription console for the
practitioner, and the participant interface).
From the implementation standpoint, the
proposed models (i.e., physical exercise program and
physical exercise information models, difficulty
levels, instructions, and practitioner and participant
interactions) were adequate and led to a coherent
development of the web-based application with a
preliminary set of 30 different exercises. These
exercises can be aggregated to constitute coherent
individual sessions, which in turn form a physical
exercise program adaptable to individual needs and
characteristics.
In what concerns the experience of the application
of the MCR framework to develop the web-based
physical exercise program and respective
components and models, it is possible to conclude
that the first phase of this framework (i.e., the
development phase) provided efficient guidance on
the methodological and practical decision-making.
To complete the development phase of the MCR
framework, two additional studies are underway: (i)
content validation of the practitioner and participant
instructions, by conducting a focus group; and (ii) a
usability study to assess the practitioner and
participant user interaction, by conducting a heuristic
evaluation involving experts, and a user-centred
evaluation involving practitioners and potential
participants.
Future work also includes the remaining three
phases of the MCR framework, that is, feasibility and
piloting (i.e., assessment of acceptability,
compliance, and retention), evaluation (i.e.,
assessment of the effectiveness and cost-
effectiveness, and understanding the changes
introduced by the new processes), and
implementation (i.e., dissemination, surveillance and
long-term follow up).
ICT4AWE 2023 - 9th International Conference on Information and Communication Technologies for Ageing Well and e-Health
228

AKNOWLEDGEMENTS
This work was supported by Programa Operacional
Competitividade e Internacionalização (COMPETE
2020), Portugal 2020 and Lisboa 2020 of the Fundo
Europeu de Desenvolvimento Regional (FEDER) /
European Regional Development Fund (ERDF),
under project ACTIVAS - Ambientes Construídos
para uma Vida Ativa, Segura e Saudável, POCI-01-
0247-FEDER-046101.
REFERENCES
Akerman A., Gonçalves D.J., & Perracini M.R. (2011)
Tratamento das Disfunções do Balance em Idosos. In
Funcionalidade e Envelhecimento. Guanabara Koogan,
Rio de Janeiro.
American College of Sports Medicine. (2009). American
College of Sports Medicine position stand. Exercise
and physical activity for older adults. Med Sci Sport
Exerc., 41(7),1510–30.
Bushman, B.A. (2018). Developing the P (for Progression)
in a FITT-VP Exercise Prescription. ACSM's Health &
Fitness Journal, 22(3), 6-9.
Caspersen, C.J., Powell, K.E., & Christenson, G.M. (1985).
Physical activity, exercise, and physical fitness:
definitions and distinctions for health-related research.
Public health reports, 100(2), 126.
Committee PAGA. (2018). 2018 Physical activity
guidelines advisory Committee scientific report. US
Department of Health and Human Services,
Washington, DC.
Craig, P., Dieppe, P., Macintyre, S., Michie, S., Nazareth,
I., & Petticrew, M. (2008). Developing and evaluating
complex interventions: the new Medical Research
Council guidance. Bmj, 337.
Di Lorito, C., Long, A., Byrne, A., Harwood, R.H.,
Gladman, J.R., Schneider, S., & van der Wardt, V.
(2021). Exercise interventions for older adults: A
systematic review of meta-analyses. Journal of Sport
and Health Science, 10(1), 29-47.
Ferguson, B. (2014). ACSM’s guidelines for exercise
testing and prescription 9th Ed. 2014. The Journal of
the Canadian Chiropractic Association, 58(3), 328.
Fragala, M.S., Cadore, E.L., Dorgo, S., Izquierdo, M.,
Kraemer, W.J., Peterson, M.D., & Ryan, E.D. (2019).
Resistance training for older adults: position statement
from the national strength and conditioning association.
The Journal of Strength & Conditioning Research,
33(8).
Izquierdo, M., Merchant, R.A., Morley, J.E., Anker, S.D.,
Aprahamian, I., Arai, H., & Singh, M.F. (2021).
International exercise recommendations in older adults
(ICFSR): expert consensus guidelines. The journal of
nutrition, health & aging, 25(7), 824-853.
Kannus, P., Sievänen, H., Palvanen, M., Järvinen, T., &
Parkkari, J. (2005). Prevention of falls and consequent
injuries in elderly people. The Lancet, 366(9500), 1885-
1893.
Kisner C., Colby L.A. (2009) Amplitude de Movimento. In
Exercícios terapêuticos: fundamentos e técnicas.
Barueri, São Paulo, Brazil.
Medical Research Council (2000). A framework for
development and evaluation of RCTs for complex
interventions to improve health. Medical Research
Council, London.
Queirós, A., Silva, A., Alvarelhão, J., Rocha, N. P., &
Teixeira, A. (2015). Usability, accessibility and
ambient-assisted living: a systematic literature review.
Universal Access in the Information Society, 14, 57-66.
Remón, Á.L.C., Díaz-Benito, V.J., Beatty, J.E.J., &
Lozano, J.A.S. (2020). Levels of physical activity
among older adults in the European Union. Journal of
aging and physical activity, 29(2), 242-249.
Rodrigues, F., Domingos, C., Monteiro, D., & Morouço, P.
(2022). A review on aging, sarcopenia, falls, and
resistance training in community-dwelling older adults.
International journal of environmental research and
public health, 19(2), 874.
Sherrington, C., Fairhall, N., Kwok, W., Wallbank, G.,
Tiedemann, A., & Bauman, A. (2020). Evidence on
physical activity and falls prevention for people aged
65+ years: systematic review to inform the WHO
guidelines on physical activity and sedentary
behaviour. International journal of behavioral nutrition
and physical activity, 17(1), 1-9.
Turner, S., Kisser, R., & Rogmans, W. (2015). Falls among
older adults in the EU-28: Key facts from the available
statistics. EuroSafe, Amsterdam.
US Department of Health and Human Services (2018).
Physical Activity Guidelines for Americans. US
Department of Health and Human Services
Washington, DC.
Vozzi, F., Palumbo, F., Ferro, E., Kreiner, K., Giugni, F.,
Dutton, R., & Parodi, O. (2022). Nutritional and
physical improvements in older adults through the
doremi remote coaching approach: a real-world study.
Intelligent Medicine, 2(4), 181-192.
World Health Organization (2020). WHO guidelines on
physical activity and sedentary behaviour. World
Health Organization, Geneva.
Development of a Web-based Program for Personalized Physical Exercise for Older Adults
229
