
Application of Blood Flow Velocity Study based on Electromagnetic
Flowmeter in the Treatment of Cerebral Infarction
Xuejing Li
1,2
, Jinchuan Wu
1,2
, Huichen Zhu
1,2
, Zhenghao Lin
1,2
, Zhongli Zhang
1,2*
and Lujia Tang
3,*
1
Shanghai Institute of Measurement and Testing Technology, Shanghai, China
2
Shanghai Key Laboratory of On-line Testing and Control Technology, Shanghai, China
3
Emergency Department, Xin Hua Hospital affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China
Keywords: Blood Flow Rate, Cardiovascular Disease, Electromagnetic Folwmeter.
Abstract: Epidemiological studies on people infected with novel coronavirus have found that patients with underlying
diseases, especially cardiovascular diseases, account for the first place in mortality. The treatment effect of
cardiovascular diseases is proportional to time, and the more timely the discovery and treatment, the higher
the success rate of cure. Because of the special requirements for medical procedures during the COVID-19,
the monitoring before the onset of the disease is particularly important. This study aims to conduct long-
term monitoring of blood flow velocity and predict the condition of cardiovascular disease based on the
monitoring results, which is of great significance for effective treatment time and provides strong reference
for improving the medical level of cardiovascular disease in the future.
1
INTRODUCTION
Cardiovascular disease is one of the leading causes
of death in China. According to statistics, there are
290 million people affected by cardiovascular
disease in China (Stevens, 2016), more than cancer.
According to statistical analysis, the highest
mortality rate of cardiovascular disease in more than
200 diseases in nearly 200 countries around the
world is myocardial infarction (Eisen A- Le May
MR). Acute myocardial infarction (AMI) is
myocardial necrosis caused by acute and persistent
ischemia and hypoxia of coronary artery, which is an
important manifestation of coronary heart disease.
Chest pain is the most common symptom of
cardiovascular disease (CVD). Consultations for
myocardial infarction in the emergency department
account for 10 % of the emergency department
(Berger PB - Mc Namara RL), and acute ST-
segment elevation myocardial infarction (STEMI)
patients are more significant in myocardial
infarction. Long term monitoring of blood flow
velocity and analysis of monitoring results can
provide useful references for the prevention and
control of ischemic stroke. The model studied in this
article is not only simple, but also has strong
operability characteristics, and has the value of
promoting to society.
The chest pain center was first established in the
United States, founded by the St. ANGLE Hospital
in Baltimore, and then appeared in France, Britain,
Canada, Germany and other developed countries. It
was not until 2011 that China established the first
batch of chest pain centers recognized by the SCPC.
The purpose of establishing a chest pain center is to '
send patients with acute chest pain to hospitals with
treatment capacity and receive the best treatment in
the shortest possible time '. The outbreak of
coronavirus disease 2019 (COVID-19) has brought
severe challenges to the diagnosis and treatment of
STEMI patients undergoing emergency PCI in chest
pain center. On the one hand, COVID-19 poses a
great threat to medical staff. On the other hand, the
screening and infection control procedures required
to reduce the nosocomial transmission of COVID-19
may seriously delay the PCI time and have a
negative impact on the prognosis of patients.
2
DATA AND OBJECTS OF
PAPER
2.1 Research Object
The data of Shanghai Chest Pain Center from 2019
to 2021 were collected. In order to more clearly
Li, X., Wu, J., Zhu, H., Lin, Z., Zhang, Z. and Tang, L.
Application of Blood Flow Velocity Study Based on Electromagnetic Flowmeter in the Treatment of Cerebral Infarction.
DOI: 10.5220/0012278800003807
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 2nd International Seminar on Artificial Intelligence, Networking and Information Technology (ANIT 2023), pages 233-236
ISBN: 978-989-758-677-4
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
233
analyze the results according to the outbreak of the
epidemic, grouped by time. Patients from January
2019 to December 2019 were divided into pre-
epidemic group A (n = 222), and patients from
January 2020 to December 2021 were divided into
epidemic group B (n = 190). The pre-epidemic
group was again divided into group A1 (self-
admission group, n = 131) and group A2 (120
admission, n = 91). The epidemic group was divided
into group B1 (self-admission group, n = 112) and
group B2 (120 admission, n = 78).
Compared with before the epidemic, patients
need to complete the examination of the new
coronavirus before treatment and carry out shunt
treatment according to the examination results, as
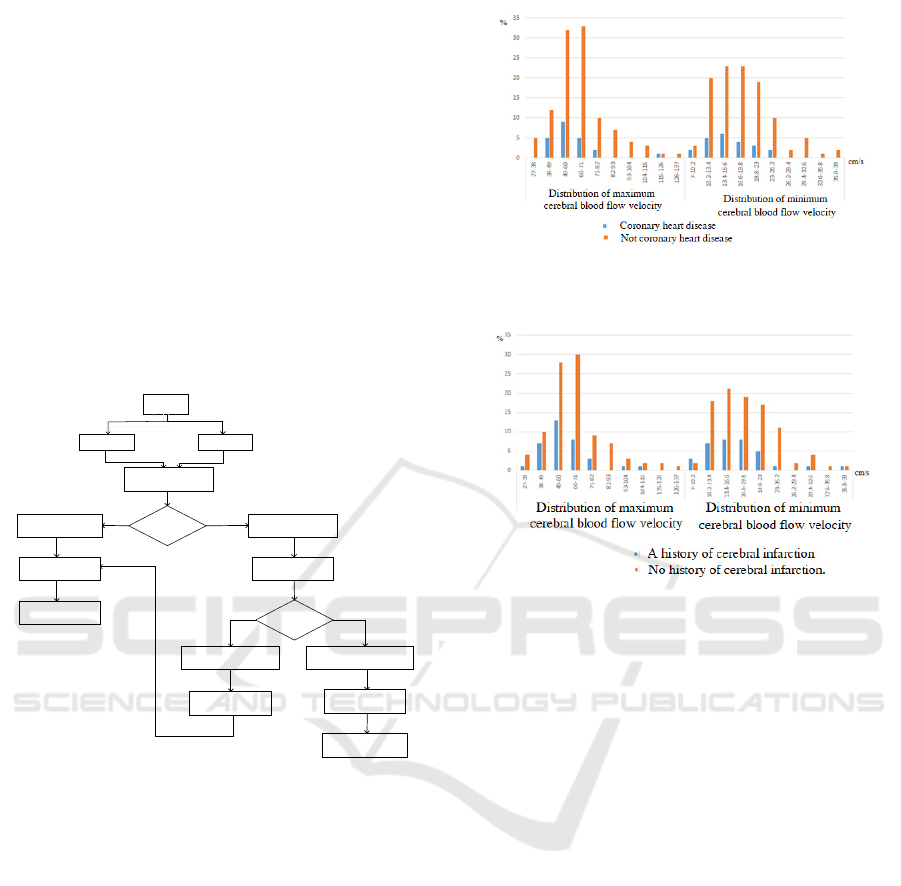
shown in Fig.1.
Chest pain
patients
Self-treatment
120 sent for
treatment
Whether there are fever
symptoms
Screening for COVID-19
infections
No fever and respiratory
symptoms
Have fever symptoms and
respiratory symptoms
Chest pain emergency
Co nven tional th erap y
Special fever clinic
COVID-19 disease
Fever patients with definite
etiology or low possibility of
COVID-19 infection
To investig ate suspected patients with
COVID-19 based on the sym ptoms and
epidemiological history.
Lsolation and further
examination
Transferred to epidemic
designated hospital for
treatment
Exclusion of COVID-19
patients
No
Yes
No
Yes
Figure 1: Flow chart of triage treatment.
2.2 Analysis of the Influence of Blood
Flow Velocity
Because the data sources are extensive and diverse,
two variables related to coronary heart disease,
cerebral infarction and cerebral blood flow velocity
are extracted from the preprocessed database. The
multivariate features were extracted and represented
as binary vectors to compare the effects of novel
coronavirus infection on blood flow velocity in
patients with coronary heart disease and cerebral
infarction.
Figure 2: Characteristics of cerebral blood flow velocity in
patients with coronary heart disease.
Figure 3: Effect of coronary heart disease on cerebral
blood flow velocity.
According to Figures 2 and 3, A history of
coronary heart disease and cerebral infarction has a
more significant impact on minimum blood flow
velocity.
The minimum blood flow velocity of patients
with a history of coronary heart disease and cerebral
infarction is higher than that of normal individuals.
3 COMPARISON OF
TREATMENT-RELATED TIME
NODES
3.1 Research Method
The measurement data of normal distribution were
expressed as (x ± s), and the comparison between
groups was performed by independent sample t test.
The measurement data is expressed as [M (Q1-Q3)]
and is a non normal distribution. The study used
Mann Whitney rank sum test for inter group
comparison. Where [n (%)] represents counting data.
Comparison between groups using χ 2 Inspection.
ANIT 2023 - The International Seminar on Artificial Intelligence, Networking and Information Technology
234

3.2 Data Statistics
Table 1: Hospitalization days and cost table before and
after the epidemic.
item Before the
e
p
idemic
After the
e
p
idemic
hospital days(d)
7.96±2.12 8.57±2.58 Self-
treatment
Hospitalization expenses
(
ten thousand
y
uan
)
5.96±0.57 6.37±1.27
Dru
g
p
ro
p
ortion
(
%
)
4.88 7.53
hospital days(d)
8.34±2.46 8.76±1.98 120 sent for
treatment
Hospitalization expenses
(
ten thousand
y
uan
)
6.07±0.34 6.77±1.08
Drug proportion ( % ) 5.88 6.93
The treatment time is very valuable for patients with
chest pain. Here, the time required for medical
contact to complete the first electrocardiogram,
detection of troponin, entry of a guide wire, catheter
room activation test ( x ± s, min ) after self-service
and 120 admissions were compared and analyzed.
Table 2: Time node analysis.
item Before the
e
p
idemic
After the
e
p
idemic
p
Medical contact to
complete the first
electrocardio
g
ra
m
5.8±0. 43 9.6±0.63 0.009 Self-
treatment
Detection of troponin 8.6±0.41 20±0.54 0. 016
Introduction A guide
wire
82.5±12.8
4
85.7±14.34 0.023
cardiac catheterization
laborator
y
activations
21.2±8.52 26.3±9.75 0.043
Medical contact to
complete the first
electrocardio
g
ra
m
5.2±2.59 8.7±4.06 0.020
120 sent
for
treatment
Detection of tro
p
onin 7.9±0.89 21±19.64 0.045
Introduction A guide
wire
89.2±12.3
9
105.2±30.0
4
0.039
cardiac catheterization
laborator
y
activations
26.8±11.2
9
27.5±13.65 0.047
By comparing the test time shown in Table1 and 2, it
can be seen that the novel coronavirus epidemic has
indeed prolonged the time of diagnosis and
treatment. The reasons for the analysis are as follows:
(1) In order to avoid nosocomial infection, the
time of shunt treatment increased, as shown in Fig.4.
(2) Some patients, usually do not pay attention to
their chronic underlying diseases, until the symptoms
of life crisis to the hospital, resulting in increased
hospital staff.
(3) Some doctors can 't work because of the
epidemic.
4 CONCLUSION
In this paper, during the COVID-19 pandemic, the
number of severe cases of chest pain has been on the
rise, and the number of deaths has gradually
increased. The main reason is that severe cases of
COVID-19 have severe respiratory distress
syndrome, or even respiratory failure. According to
research data, it can be inferred that
(1) Patients with a history of coronary heart
disease and cerebral infarction have significantly
different blood flow velocities compared to healthy
individuals. The development of stroke can be
indirectly obtained based on changes in blood flow
velocity;
(2) The minimum blood flow velocity of patients
with coronary heart disease and cerebral infarction is
usually lower than that of non diseased patients, so
special attention should be paid to changes in the
minimum blood flow velocity during monitoring. It
is worth noting that if the patient takes anticoagulant
drugs, the monitoring results may be affected.
On the basis of analyzing the blood flow rate,
the patient 's medical time before and after the
epidemic was analyzed. The hospitalization time,
cost and time node were compared. The results
showed that the chest pain examination time during
the epidemic was longer than that before the
epidemic. Effective monitoring of blood flow
velocity in patients with chronic underlying diseases
is of great significance to avoid severe chest pain
and even death.
ACKNOWLEDGMENTS
This work was supported by the Science and
technology project of Shanghai market supervision
and Administration Bureau (Development of a
dynamic calibration device for the BP measurement
devices using the oscillometric method) No.2022-
03and (Research on online multi-parameter
measurement method and device of gas-water two-
phase flow based on IFT) No. 2022-06. This work
was also supported by the Shanghai Institute of
Measurement and Testing Technology Research
Project:E00RY2303 and E00RY2304).
REFERENCES
Stevens W, Peneva D, Li JZ, et al. Estimating the future
burden of cardiovascular disease and the value of
lipid and blood pressure control therapies in
China[J]. BMC Health Serv Res,2016,16:175.
Eisen A,Giugliano R P,Braunwald E.Updates on acute
coronary syndrome: a review[J].JAMAcardiol, 2016,
1(6):718-730.
Application of Blood Flow Velocity Study Based on Electromagnetic Flowmeter in the Treatment of Cerebral Infarction
235

Keeley EC, Boura JA, Grines CL. Primary
angioplasty versus intravenous thrombolytic therapy
for acute myocardial infarction: a quantitative
review of 23 randomised trials[J].
Lancet,2003,361(9351):13–20.
Le May MR, Davies RF, Labinaz M, et al. Hospitalization
costs of primary stenting versus thrombolysis in acute
myocardial infarction: cost analysis of the Canadian
STAT Study[J]. Circulation,2003,108(21): 2624–2630.
Berger PB, Ellis SG, Holmes DR Jr, et al. Relationship
between delay in performing direct coronary
angioplasty and early clinical outcome in patients with
acute myocardial infarction: results from the global
use of strategies to open occluded arteries in
Acute Coronary Syndromes (GUSTO-IIb) trial[J].
Circulation,1999,100(1):14–20.
Mc Namara RL,Wang Y,Herrin J,etal. Effect of door-to-
balloon time on mortality inpatients with ST-
segment elevation myocardial infarction[J].Coll
Cardiol,2006,47(11):2180–2186.
Xu Wei, Wang Kai, Wang Gang, etc. Multidisciplinary
Collaborative Management and Evaluation of Chest
Pain Center [J]. China Health Economy, 2018, 37 (11)
: 71-72 ;
Liu Peng, Lin Fan, Zhang Jinxia, etc. Effect of target value
management of quality control indicators in chest pain
center on in-hospital treatment efficiency and effect of
STEMI patients [J]. Chinese Journal of Emergency
Medicine, 2019,28 ( 4): 498-503
ANIT 2023 - The International Seminar on Artificial Intelligence, Networking and Information Technology
236
