
A WIRELESS APPLICATION THAT MONITORS ECG SIGNALS
ON-LINE: ARCHITECTURE AND PERFORMANCE
1
Jimena Rodríguez, Lacramioara Dranca, Alfredo Goñi and Arantza Illarramendi
University of the Basque Country (UPV/EHU).LSI Department. Donostia-San Sebastián. Spain
Keywords: Wireless Application, Mobile Co
mputing, Wireless Network, ECG Monitoring System
Abstract: In this paper, we present an innovating on-line monitoring system that has been developed by applying new
advances in biosensors, mobile devices and wireless technologies. The aim of the system is to monitor
people that suffer from heart arrhythmias without having to be hospitalized; and therefore, living a normal
life while feeling safe at the same time. On the one hand, the architecture of the system is presented; and, on
the other hand, some performance results and implementation details are explained showing how the
previous solution can be effectively implemented and deployed into a system that makes use of PDAs, and
wireless communications: Bluetooth and GPRS. Moreover, special attention is paid to two aspects: cost of
the wireless communications and notification latency for the detected serious heart anomalies.
1
This work was mainly supported by the University of the Basque Country and the Diputación Foral de Gipuzkoa (co-
supported by the European Social Fund)
1 INTRODUCTION
Innovations in the fields of PDAs, wireless
communications and vital parameter sensors enable
the development of revolutionary medical
monitoring systems, which strikingly improve the
lifestyle of patients, offering them security even
outside the hospital.
In this context we are developing a system that
t
akes advantage of the latest advances in the
technology in order to monitor on-line, people that
suffer from heart arrhythmias. The system allows an
anywhere and at any time monitoring and provides
to its users the adequate medical assistance. So, the
patient could have a normal life in his/her habitual
environment without being constrained to a hospital
room. The patient's tool, which replaces the
traditional monitor (Holter) and supports Bluetooth
technology, is reflected in a standard PDA that is a
small, handheld computer that captures, processes,
detects, analyzes and notifies possible abnormalities
to a medical unit through the wireless network
(GPRS) from anywhere and at any time. Moreover,
the Bluetooth communication makes this tool even
more comfortable for the user, replacing the cables
of the sensors that pick up the cardiological signals.
Concerning related works, on the one hand, there
are se
veral commercial tools designed to monitor
heart patients outside the hospital; from the
traditional Holter (Despopoulos, 1994) that simply
records heart signals named ECG
(electrocardiogram), for 24 or 48 hours, which are
later analyzed in the hospital, until the modern
cellular phones e.g Vitaphone (Daja, 2001) that, in
case of an emergency, can record the signals through
the metal electrodes situated on its back and transmit
them to the cardiac monitor center situated in the
hospital. There are other commercial monitoring
systems that use PDAs to store the ECG signals, e.g.
Ventracor (Ventracor, 2003), Cardio Control (Cardio
Control, 2003). For these systems additional features
like GSM/GPRS transmission to an analyzing unit
are also being developed.
On the other hand, in the research m
onitoring
area, stand out several research projects like:
@Home (Sachpazidis, 2002), TeleMediCare
(Dimitri, 2003), or PhMon (Kunze, 2002), whose
aims are to build platforms for real time remote
monitoring.
All these systems are continuously sending
ECGs to a
medical center through a wireless
communication network, where the signals are
138
Rodríguez J., Dranca L., Goñi A. and Illarramendi A. (2004).
A WIRELESS APPLICATION THAT MONITORS ECG SIGNALS ON-LINE: ARCHITECTURE AND PERFORMANCE.
In Proceedings of the Sixth International Conference on Enterprise Information Systems, pages 138-145
DOI: 10.5220/0002640101380145
Copyright
c
SciTePress

analyzed. In spite of the advantages these kinds of
systems provide in relation to holters, they still
present main problems related to the fact that the
analysis is not performed in the place where the
signal is acquired. Therefore, there is a loss of
efficiency in the use of the wireless network because
normal ECGs are also sent (and wireless
communications imply a high cost); and, if the
wireless network is not available at some moment
(e.g. in a tunnel, in an elevator, etc.), there might be
a loss of ECG signal with the corresponding risk of
not detecting some anomalies.
Our proposal, the MOLEC system, is a PDA-
based monitoring system that records user ECG
signals and locally analyzes them in order to find
arrhythmias. In case of detecting a high risk situation
for the user, it sends an alarm with the
corresponding ECG signal through the wireless
network (GPRS) to a health center for further
analysis and medical assistance.
The advantages of this approach are that
provides 1) local analysis: even if wireless
communication with the health center were
unavailable, the signal could be analyzed locally at
the PDA; 2) low cost communication since not the
entire signal is sent; 3) fast medical response in risk
situations for the user; 4) accessibility: data recorded
in the system can always be queried whether locally
or remotely; 5) distributed computation: the local
analysis in each PDA implies a serious decrease of
computational costs in the health center; 6)
openness: it can be easy integrated in hospitals that
manage clinical data through the XML and HL7
standard (HL7, 2003), a representation of clinical
documents; 7) adaptability: possibility of working
with different kinds of ECG sensors; 8) simplicity:
making technical issues transparent to the users from
the point of view of software and hardware
components.
The goals of this paper are to present the global
architecture of MOLEC, and more specifically the
software modules needed in the PDA (in section 2);
and to introduce some implementation details (in
section 3) and performance results (in section 4),
focusing on two important aspects: minimizing the
cost of the wireless communications and obtaining a
reasonable notification latency for the detection and
notification of serious heart anomalies. Finally, in
section 5, we present the conclusions.
2 GLOBAL ARCHITECTURE
Three main components form the global architecture
of MOLEC (see figure 1, from left to right): 1) The
ECG Sensors that pick up the electric impulses of
the heart. These sensors are the “intelligent” chips
that communicate with the PDA through the
bluetooth protocol. 2) The PDA-Holter that acquires
the data signal in a PDA, records them, detects
abnormalities and notifies them immediately in case
they are considered serious. 3) The Molec Hospital
receives the user alarm signals that are shown to the
medical personal so that they can react promptly.
Figure 1: Architecture
2.1 ECG Sensors
The ECG sensors are carried by the user in order to
register heart signals and send them to the PDA
through the bluetooth protocol (Bluetooth, 2003).
Bluetooth is a new standard for very low cost, short-
range wireless communication. It enables different
types of equipment to communicate wireless with
each other and has been thought of as a cable
replacement becoming the fastest growing
communication standard ever.
Hence we consider that this technology has a
promising future for the area of the ECG sensors and
we developed the MOLEC project for the integration
with bluetooth ECG sensors.
ECG Sensor emulating module
Emulate Sensor
MIT-BIH
Sequence of 16 bit
0 1 0 1 0 1 1 1 0 1 0 1 1 0 1 1
Figure 2: ECG sensor emulating module
Unfortunately, nowadays ECG sensor providers
only sell their products with proprietary
electrocardio analyzer software. That is why, in our
case, the PDA communicates through bluetooth with
an ECG sensor emulator placed in a computer
device. The ECG signals are taken from a
recognized freely distributed database, namely MIT-
BIH Arrhythmia database (MIT-BIH, 2003), and
sent in real-time as bit sequences to the PDA
through the wireless network (see figure 2).
On the other hand, in the PDA-Holter, the
Acquisition module receives the bit chains and
translates them into a standard format that the whole
system understands.
A WIRELESS APPLICATION THAT MONITORS ECG SIGNALS ON-LINE: ARCHITECTURE AND
PERFORMANCE
139
2.2 Molec Hospital
The other system that interacts with the PDA-Holter
is the MOLEC Hospital whose main function is to
customize the PDA-Holter for each user and to
receive users' possible abnormalities. It maintains a
large database with all the users registered, their
historical and their progress. This could be very
useful for the specialists when diagnosing or taking
fast decisions in alarm cases.
Furthermore, MOLEC Hospital provides web
services that allow querying user data stored in the
PDA.
Those web services provide the same
functionality that holters have associated in the
specialized literature (Farreras, 2001) by a set of
reports, which enables physicians to analyze the data
easily and quickly and shows information about: 1)
automatic arrhythmia detection and identification; 2)
analysis of ST segments evolution; 3) ECG
parameters. Therefore the data in the database can be
queried, locally or remotely, to know different
aspects that can be related to the anomalous
situations.
In addition, the hospitals can easily incorporate
the MOLEC Hospital system into their
administration system since it does not interfere with
existing applications.
2.3 PDA-Holter
The PDA-Holter is the user tool of MOLEC. It is
responsible for acquiring the ECG data signal,
recording it, detecting abnormalities and notifying
them immediately in case they are considered
serious. The PDA-Holter is formed by several
modules that are explained in the next subsections.
ECG Signal Acquisition
The ECG signal acquisition module receives the
digital signal and converts it into a format
understandable by the whole system. It manages the
Bluetooth communication among the ECG sensors
and the PDA. Moreover it has to build signal
packages (the “source packages”) with a defined size
from the bit chains received from the ECG sensors.
In section 4, we present the experimental results that
have leaded us to define the correct size of these
packages.
Data Preprocessing Module
This module obtains the ECG signal in form of
source packages and detects the typical part of the
beat. An ECG signal consists of several beats that
succeeds with a frequency between 60 and 100 per
minute. A normal beat contains a P wave, a QRS
complex and one or two T waves. For the
arrhythmia detection it is significant the
identification of the presence or absence of these
waves, the points where start, end and the peaks of
them. We call these points ‘wave events’.
ECG Signal
Sequence of peaks and limits of
P,QRS,T waves (wave events)
Sequence of N wave events
Sequence of <beat, frequency, intervals>
ECG Signal Processing
Beat Detector
Data Preprocessing Module
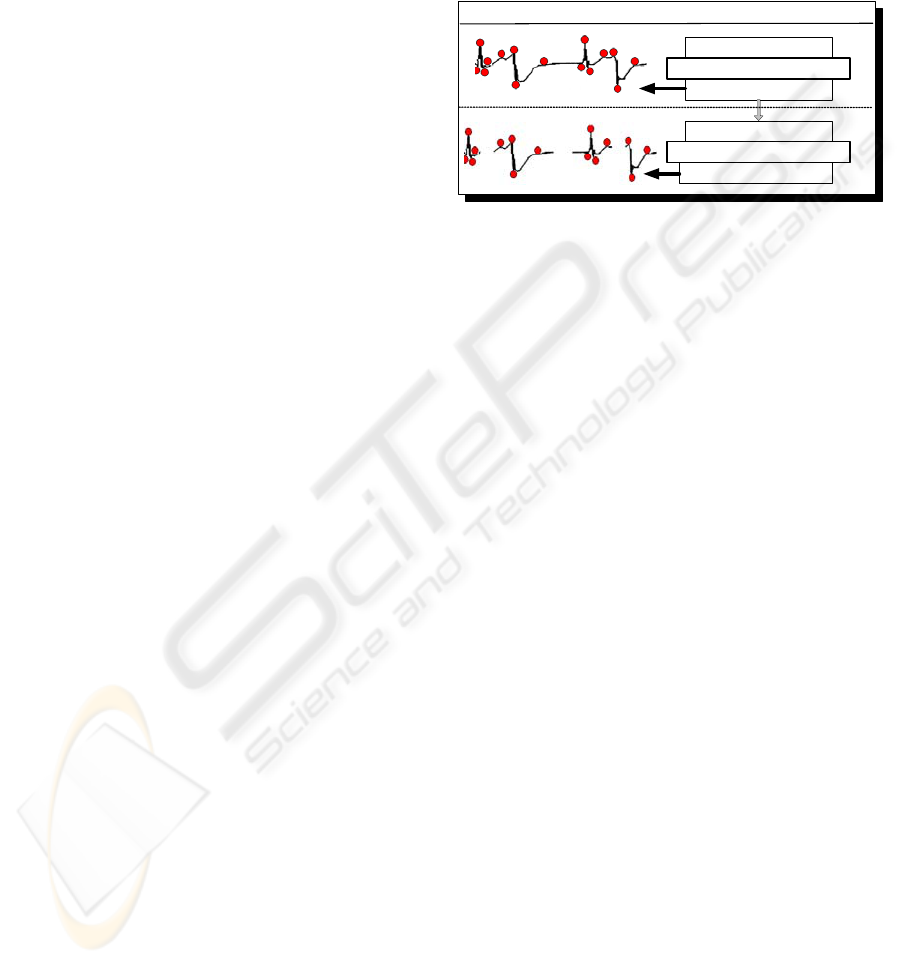
Figure 3: Data preprocessing module
The goal of the data processing module is to
detect each beat from the original signal and the
points that characterize it. This work is even more
difficult if the signal has a high level of noise.
The task is realized in two steps (see Figure 3):
Firstly, the ECG signal is processed in order to
detect wave events (ECG Signal Processing). For the
implementation of the ECG Signal Processing we
have used, although slightly changed, a Fortran
implementation (Jané, 1997) of an on-line detection
algorithm developed by Pan & Tompkins (Pan,
1985) and provided by the recognized PhysioNet
(PhysioNet, 1997). This tool was not specifically
designed to be run in small computers like PDAs
and usually has been used to process long ECG
signals. However, we have been able to run it
successfully in the PDA using as input small ECG
signals (those corresponding to the “source
packages” previously mentioned). Only minor
changes related to memory management have been
made in the “open source” of Ecgpuwave with the
goal of increasing the processing speed.
Secondly, the sequence of wave events is
transformed into a sequence of beats, it is computed
the length of the relevant intervals and segments
determined by two wave events (Beat Detector).
Decision Support Module
Once the beats with the corresponding wave
events have been detected, the system can start the
arrhythmia detection, task which is realized by the
Decision Support Module (see Figure 4). Two main
steps take place during this analysis: identification of
the beat types and classification of the arrhythmias.
ICEIS 2004 - SOFTWARE AGENTS AND INTERNET COMPUTING
140
beat
Beat + beat type
Sequence of four beats
Rhythm
4. Beat Classifier
5. Rhythm Classifier
Decision Support Module
Figure 4: Decision Support Module
In order to classify the beat we have tested
seventeen methods (Rodriguez, 2003) from the
machine learning area and we have chosen the most
appropriate one for this kind of data: the decision
tree methods (Le Blanc, 1986) that approach
discrete-valued target functions. The learned
functions are represented by decision trees, but they
can also be re-represented as a set of if-then rules to
improve human readability. Those rules have been
extracted, codified in a programming language and
tested. The validation of the rules previously
generated took place using the hold-out validation.
In order to classify the rhythms, we used a
combination of rules: Cardiologic and Inferring
rules. The Cardiologic rules were obtained through
the translation of the arrhythmia descriptions found
in the specialized cardiologic literature (Farreras,
2001) and in parallel, we obtained the Inferring rules
by using techniques based on decision trees. Finally
we combined them and chose the best rules to detect
each rhythm. More details about the decision
support module can be found in (Rodriguez, 2003).
Data Manager Module
The main goal of this module is to efficiently
manage the restricted memory resources available in
the PDA, at least when compared to the great
capacity of ECG sensors to generate data.
It has knowledge about all the signals that are
being acquired and the stage of its processing. For
each packet, once the classification of the beats and
rhythm is done, the Data Manager decides how to
store each beat: in a regular file or in a database.
Normal ECGs are stored in compress files and the
anomalous ones are stored at the PDA database.
More details about the data manager module can be
found in (Rodriguez DOA, 2003).
Alarm Manager Module
This module receives the current heart rhythm
and associated parameters and decides whether to
generate an alarm. Not all the arrhythmias should be
sent in real time to cardiologists so that they can
confirm them and/or make their decisions: only
those considered very dangerous by them.
With the help of some cardiologists, we have
considered two groups, one for high-risk
arrhythmias, that is, arrhythmias that should be
notified to the hospital when they were detected by
the system and the other one for the moderate-risk
arrhythmias and normal rhythms that are stored but
not immediately notified.
Moreover, we have defined a personalized alarm
notification policy that allows deciding if an alarm is
sent or not depending on the user parameters. For
example: if the patient X presents a short ventricular
tachycardia (a high-risk arrhythmia), that alarm
would not be notified if the physician had previously
defined that, for patient X, only tachycardias longer
that thirty seconds should be notified. It has to be
noticed that an on-line monitoring system like this
would be useless if the cardiologists were bothered
with not really relevant arrhythmias very often.
Sender Module
This module is in charge of the communication
control between the PDA and the hospital. Hence, it
establish and maintain the connection in order to
send the alarm messages with the corresponding
ECG signal fragments and to answer to the report or
query solicitations that the hospital could make. A
standard is used to transmit medical data: HL7
(HL7, 2003) that is contained into the XML
message. An HL7 representation of clinical
documents is called Clinical Document Architecture
(CDA). The CDA is a document that specifies the
structure and semantics of a clinical document. It
can include text, image, sounds and other
multimedia content. When the message is received
by the hospital, the physician reads the report and
confirms the result obtained by MOLEC. Notice that
there are tools that can show the data represented in
HL7 messages to physicians.
Interface Module
The interface module is responsible for data
visualization and measurements display. The figure
5 shows a picture of the PDA-Holter. It provides a
friendly interface that draws the ECG signal as soon
as the current beat and rhythm types are obtained on-
line by the Decision Support Module.
3 IMPLEMENTATION DETAILS
The platform used for the implementation of the
PDA-Holter part of MOLEC has been the next PDA:
A WIRELESS APPLICATION THAT MONITORS ECG SIGNALS ON-LINE: ARCHITECTURE AND
PERFORMANCE
141

an iPaq 3970 which is a powerful device with a
400Mhz XScale processor, 64MB SDRAM and 48
MB Flash memory. Besides, it has a Linux support,
the Familiar Linux distribution (Handhelds 2003),
converting it in a complete embedded Linux system.
In figure 6, it can be observed that Linux has
been the chosen operating system. The external layer
of the figure shows the MOLEC modules that have
been explained in the previous section and in the
middle layer they can be seen the programming
languages used for the implementation of them.
We chiefly have used Java because it is: 1) an
object oriented language, 2) platform independent,
3) type safe; it provides 4) automatic memory
management, 5) built in threads, 6) synchronized
primitives and 7) exception handling, which makes
it proper for the development of a critical time
system like MOLEC is. Although many people
agree that the Java performance is not as good as the
one offered by other programming languages, this
happens only with interpreted Java. In our prototype,
we have compiled the Java source code with the
GNU compiler for Java (GNU, 2003), what
increased dramatically the processing performance.
For the signal preprocessing part, as this task
supposes several mathematical calculus, we chose
the Fortran and C languages.
For the implementation of the interface module,
we have used the SWT libraries (Eclipse, 2003)
because it has been possible to integrate them into
our PDA platform (Xscale processor and Linux
operating system), and to compile them with the
GNU compiler. Moreover, they have provided a
very acceptable processing performance (faster than
graphical libraries that usually come with Java
distributions like AWT and Swing).
For the wireless communications, two
technologies have been used: the Bluetooth
technology and the General Packet Radio Server
(GPRS). Bluetooth is a digital connection wireless
standard that can transmit data up to a rate of 1
Mbps; and GPRS is a wireless network that allows
sending and receiving data packages and its
bandwidth is up to 56 Kbps. In section 2.1, we
explain the difficulty to obtain the ECG sensors, so
for the tests we have performed, the PDA
communicates through Bluetooth with an ECG
sensor emulator placed in a computer device. The
ECG signals are taken from a recognized freely
distributed database, namely MIT-BIH Arrhythmia
database (MIT-BIH, 2003).
Data Manager
Alarm
Mana
g
e
r
Decison
support
Java
Sender
Linux
4 PERFORMANCE RESULTS
The main goal of our system is to monitor on-line
the ECG signal from people suffering from heart
arrhythmias. The technology proposed for the
system, PDAs and wireless communications,
imposes some restrictions that affect the design of
MOLEC.
On the one hand, working with wireless
communication technology is more expensive than
using wired communication technology. Therefore,
it is interesting to pay special attention to try to
minimize the cost of the wireless communications
and, at the same time, not to delay the notification of
serious heart anomalies to the hospital.
On the other hand, it is known that the most
powerful current PDAs, even with the latest
technological advances, are environments with
limited computing resources if compared to PCs.
Moreover, the processing tasks that a monitoring
system implies require a high computation cost: the
signal processing that obtains the sequence of beats,
the classification process of those beats and the
corresponding rhythms, and the visualization of the
ECG signal. Note that the ECG sensors generate
data very quickly. In our case, the data stored
correspond to a signal with a frequency of 360
samples per second what is equivalent to 21,600
samples/minute.
Hence, we focus on efficiency in order to prove
that a local processing of the ECG signal in a PDA
would not introduce too much latency in detection of
Figure 5: ECG visualization in MOLEC
Data Preprocessing
Fortran
C
Interface
Acquisition
Figure 6: PDA platform
ICEIS 2004 - SOFTWARE AGENTS AND INTERNET COMPUTING
142
eventual alarms, compared with a system where the
processing is made remotely.
The proposed architecture in section 3 is a
functional solution for an ECG monitoring.
However, it is also necessary a proper configuration
of the processing threads of the system in order to
obtain a system stable in time.
Therefore, it is essential to answer to the next
question: how often does the analysis process have
to be executed?, or, in other words, which is the
proper size of the “source package” provided by the
“ECG Signal Acquisition Module” that starts the
processing in the PDA?
In this section, we are going to present the
experiments that we have made with the goals of:
calculating the rate of the processing cycle that the
system can tolerate in order to not get overloaded,
thus the smallest rhythm detection delay (finding the
optimal processing rate); and of estimating the
latency of the alarm notification and the
communication costs with a medical monitoring
center.
The test results are compared with the results
obtained for the same parameters in a PC.
4.1 The optimal processing rate
Each time the ECG Signal Acquisition receives ECG
samples, the system must analyze them in order to
find arrhythmias, performing in this way an entire
processing cycle. The question we try to answer here
is how frequently we should perform this
processing, in other words, which is the processing
rate for the system.
On the one hand, as we have mentioned in
section 3, in order to identify arrhythmias, first we
have to detect the beats from the ECG signal. The
typical occurrence of the beats, in one minute, is
between 60 and 100, therefore, the entire processing
cycle (that means also the size of the ECG signal
package analyzed) should not be less than one
second since the probability to find a beat in such a
short time interval is really tiny and besides, the
algorithm of detecting the wave events is more
accurate with longer signals.
On the other hand, the smaller the cycle duration
is the faster the alarm detection could be.
Unfortunately the computation cost for each cycle
does not decrease proportionally to the cycle size
and the system can get overloaded. Moreover, this
cost differs from PDA to a normal PC since they
have different computation power.
Hence, in order to establish the optimal
processing rate we have tested the system
performance for processing cycles of one and two
seconds respectively. Both types of test have been
performed in the PDA and in the PC.
0
10 0
200
300
400
500
600
700
800
61 129 199 281 368 454 542 634
ECG adquisition time
ECG procesing time
PDA_1 PC_1
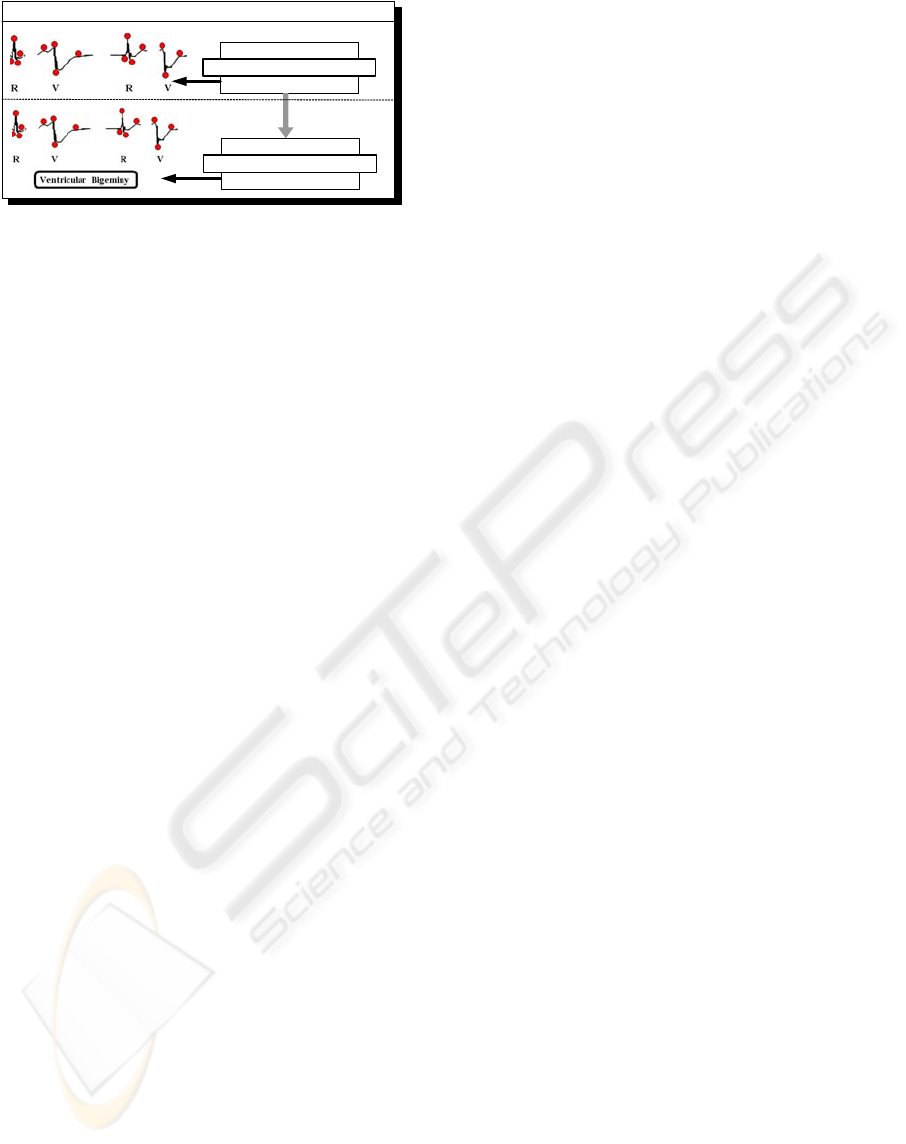
Figure 7: Processing rate of one
second
0
10 0
200
300
400
500
600
700
66 132 196 260 324 388 452 518 582 646
ECG adquision time
ECG procesing time
PDA-2 PC-2
Figure 8: Processing rate of two seconds
The figures 7 and 8 show four functions: PC-1,
PDA-1, PC-2 and PDA-2. Every point (x,y) of all
those functions indicates that the signal package
provided by the ECG Signal Acquisition at the
second x is processed by the system at the second y.
For PC-1 and PDA-1 functions, the entire processing
cycle is of 1 second, and for PC-2 and PDA-2
functions it is of 2 seconds. In PC-1 and PC-2, the
entire processing cycle is performed in the PC, and,
obviously PDA-1 and PDA-2 in the PDA.
As it can be observed in the figures, in both
cases the system running in the PC achieves a stable
state since the corresponding functions are very
close to the diagonal function (that would mean that
the signal packet received at second x is processed
by the system at second x). The stability comes from
the fact that the difference between the diagonal and
the PC-x functions does not grow along the time. In
other words, the system performs all the tasks before
A WIRELESS APPLICATION THAT MONITORS ECG SIGNALS ON-LINE: ARCHITECTURE AND
PERFORMANCE
143
the next signal package has been arrived. In the PDA
case, for processing cycles of one second, this
property is not achieved. Nevertheless, good results
are obtained for processing cycles of two seconds.
As we have explained before, the package size
has a direct influence on the rhythm delay detection,
and therefore, in the alarm detection. The average of
the time necessary to detect the rhythm for this type
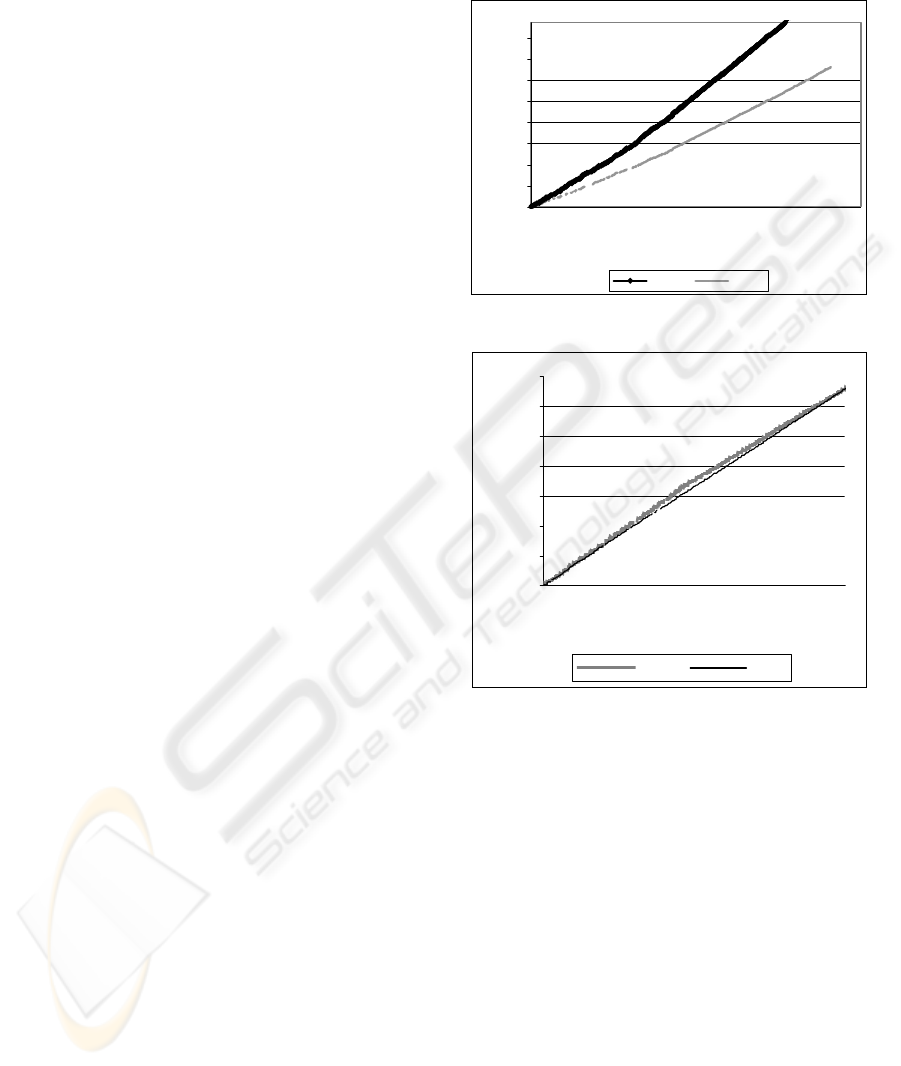
of packages appears in figure 9.
Figure 9: Rhythm detection delay
For packages of one second the PC achieves an
average of 4.43 seconds in obtaining the rhythm,
meanwhile the PDA needs 10.3 seconds, but, as the
processing cannot be performed in real time, the
rhythm detection delay would grow if the
experiment duration were longer.
For packages of two seconds the PC obtains an
average of 5.2s to detect the rhythm meanwhile the
PDA needs approximate 6.66s to detect it.
Notice that we have also experimented with
signal packages of 3 seconds and seen that real-time
processing is also possible. But, as the rhythm delay
time is greater than with signal packages of 2
seconds, so we conclude that the entire ECG
analysis process should be performed in the PDA
every 2 seconds.
Finally, an explanation of the rhythm detection
delays obtained is because the detection algorithm
used needs the previous beat types and the next three
ones, in order to detect the rhythm for the current
beat.
4.2 Alarm notification: cost and
latency
The aim of this subsection is to compare the
MOLEC system, which only sends alarm signals to
the medical center (according to the Alarm Manager
Module policy described in section 3), with a system
that continuously sends the ECG signals picked up
from the sensors and detects the alarm in the medical
center. Supposing that a GPRS network is used for
communication, we present further the
communication costs for the alarm notification
during 30 minutes of monitoring.
For this test we used three ECG records: the 100
record that does not contain any alarm, so there is no
communication with the medical center; the 207
record that is from a patient with serious health
problems and contains five minutes of alarms; and
124 record that is from a typical user, so it contains
an average notifications amount. All the ECG
signals used have the same sampling frequency (360
samples/second). For the system that sends all the
signals we supposed that each sample has 2 bytes.
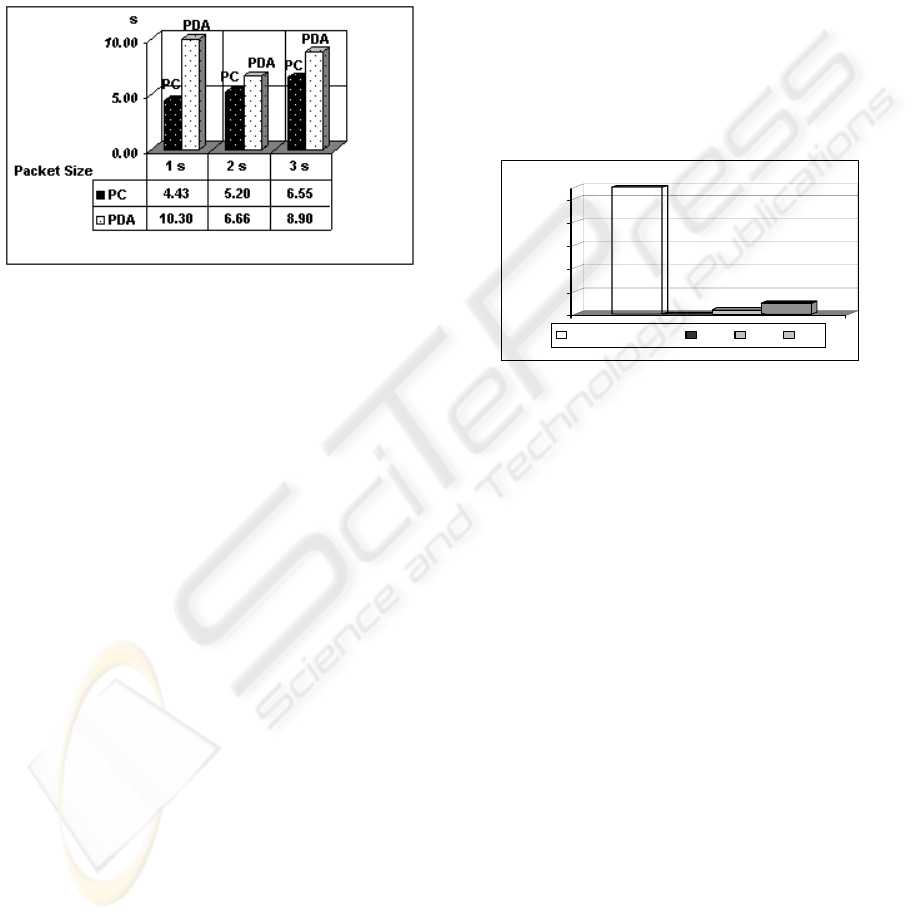
In the next figure it can be observed the amount
of data that the system would send in each case.
1296
0
40.3
96.1
0
200
400
600
800
1000
Kb
Monitor Center
100
124
207
Figure 10: Communication costs
A system, that does not make any processing and
compressing of the signal, would send
approximately 1296Kb for each 30 minutes which
means more than 2Mb/hour, meanwhile the
MOLEC-PDA-Holter, in the worst case would send
more than 100 times less. If no abnormalities are
detected then there is no communication with the
health center, as in the case of the record 100.
Therefore the amount of communication with the
health center is drastically reduced, and so the
communication costs.
Another variable that should be taken into
account is the delay between the time when the risk
episode starts and the moment when the health
center notices it.
The time needed for the MOLEC system to
notify an alarm is
t
notify
= t
rhythm detection
+t
alarm compression
+ t
communication latency
In other words the notification delay depends on
the time needed to detect the rhythm in the PDA, the
time needed to compress the alarm message and the
latency that the GPRS network involves in order to
send it to the monitor center.
On the other hand, in the case of the systems that
continuously send ECG signals to the medical center
the notification delay would depend only on the
ICEIS 2004 - SOFTWARE AGENTS AND INTERNET COMPUTING
144

communication delay over the GPRS network and
the rhythm detection time in the medical center.
As it could be observed in the figure 9, the delay
of the rhythm detection, with our algorithm, is
greater in the PDA (around seven seconds) than in a
normal PC with only one user (around four seconds).
In a system with more users that continuously send
ECG signals the costs to obtain the same results
would be greater.
Moreover, a system that continuously sends
ECG signals to a monitor center would send many,
but small signal packages through the network, what
means, if the connection is stable, a constant latency
in the communication; meanwhile the MOLEC
system sends compressed alarm messages from time
to time but with a bigger amount which suppose a
bigger latency to send it.
Therefore, the notification latency is a few
seconds bigger in the MOLEC system but still
remains in a reasonable threshold giving the
possibility to the user to obtain medical assistance in
time.
5 CONCLUSIONS
In this paper we have presented the global
architecture of an innovative system called MOLEC
that allows an on-line monitoring of people suffering
from heart arrhythmias. Among the advantages of
that system are the following ones: 1) Promptness:
MOLEC detects anomalous rhythms, anywhere and
anytime, as soon as they are produced, and sends the
corresponding alarm to the hospital; and 2)
Efficiency: MOLEC optimizes the use of wireless
communications and PDA resources.
In order to achieve those advantages, we have
designed and performed some experiments that
consisted in calculating the rate of the processing
cycle that the system can tolerate in order to be
efficient, stable and the rhythm detection delay
minimal. That time has been 2 seconds in the case of
the PDAs. Special attention has also been paid in
minimizing the cost of the wireless communications
without increasing the delay time for the detected
serious heart anomalies. That can be achieved by
performing the ECG signal processing and rhythm
classification locally in the PDA and by sending
only alarms to the hospital.
REFERENCES
Bluetooth. 2003. www.bluetooth.com
Cardio Control.2003.
www.cardiocontrol.com/cardio.htm
Daja, N., Relgin, I., Reljin B., 2001. Telemonitoring in
Cardiology –ECG transmission by Mobile Phone.
Annals of the Academy of Studenica 4, 2001.
Despopoulos, A.., Silbernagl, S. 1994, Texto y Atlas de
fisiología. ISBN: 84-8174-040-3.
Dimitri Konstansas Val Jones, Rainer Hersog. 2003.
MobiHealth- innovative 2.5/3G mobile services and
applications for healthcare. Workshop on
Standardization in E-Health. Geneva, Italy.
Eclipse 2003.
http://www.eclipse.org/.
Farreras and Rozman, “Medicina interna”. Decimatercera
edición. Edición en CD-ROM. Sección 3. Cardiologia
pag 395 – 523. October, 2001.
GNU 2003.
http://gcc.gnu.org/java/
Handhelds 2003.
http://www.handhelds.org/.
Health Level 7 (HL7). 2003.
http://www.hl7.org/.
Jané, P., Blasi, A., García, J., Laguna, P. 1997. Evaluation
of an Automatic Threshold Based Detector of
Waveform Limits in Holter ECG with the QT
database”. Computers in Cardiology, vol. 24, pp. 295-
298.
Kunze, C., Gromann, U., Stork, W., Müller-Glaser,
K.D.,2002. Application of Ubiquitous Computing in
Personal Health Monitoring Systems. 36. annual
meeting of the German Society for Biomedical
Engineering.
Le Blanc, R., “Quantitative analysis of cardiac
arrhythmias.” CRC: Critical Review in Biomedical
engineeering, 14(1):1-43, 1986
MIT-BIH Database Distribution. 2003.
http://ecg.mit.edu/
Mitchell, T.M., “Machine Learning.” ISBN 0-07-042807-
7. Section 3: Decision tree learning. Pages 52-75.
Pan, J., Tompkin, W. J. 1985. A real-time QRS detection
algorithm". IEEE Trans. Biom. Eng. BME-32: 230-
236.
Rodríguez, J., Goñi A., Illarramendi, A. 2003. Classifying
ECG in an On-Line Monitoring System. Submitted for
Publication.
Rodríguez, J., Goñi A., Illarramendi, A. Capturing,
Analyzing and Managing ECG Sensors Data in
Handheld Devices. DOA 2003.
Sachpazidis 2002. @Home: A modular telemedicine
system. Mobile Computing in Medicine, Proceedings
of the 2. Workshop on mobile computing. Heidelberg,
Germany, 2002.
Ventracor Limited. 2003 http://www.ventracor.com
A WIRELESS APPLICATION THAT MONITORS ECG SIGNALS ON-LINE: ARCHITECTURE AND
PERFORMANCE
145
