
Telesurveillance of the Dependent Seniors Using Passive
Infra-red Sensors in a Geriatric Hospital
François Steenkeste
1
, Soutrik Banerjee
1-2
, P. Couturier
3
1
Institut National de la Santé et de la Recherche Médicale Unité 558, 37 Allées Jules Guesde,
31073 Toulouse, France
2
Laboratoire Interuniversitaire de Gérontologie et de Gériatrie, CHU, 38043 Grenoble Cedex09
Abstract: To study the validity of a 'smart' system of telesurveillance in elderly
patients, GARDIEN
©
, a passive infra-red sensor network, was connected to a
computer placed at a remote site from the patient. It switched on automatically
every day and remained active throughout the night. Data corresponding to
movements within the room were collected twice per second. During the
experimental period, the data file were analyzed manually and automatically;
the results of the automatic processing were displayed in the form of a list with
all movements noted together with the time and each movement’s duration was
stored in a patient file. GARDIEN showed the patient data either in the form of
curves or as three-dimensional histograms. We studied the nocturnal activity of
23 Alzheimer patients, with or without cognitive impairment. Their activity
profiles were different. Moreover, the nocturnal motor activity patterns
permitted to identify pathological states.
1 Introduction
At present, elderly people consume a high proportion of health-care services and in
future this proportion is likely to rise considerably. It is therefore evident that high-
quality health care may in future be available universally if substantial savings can be
made through the greater use of modern technology.[1] A major concern in
supporting the sick, disabled and frail elderly people at home is the potential risks
involved, such as falling on the ground and illness. An increasing effort has been
made to develop systems to monitor people in their homes by the use of intelligent
systems, for instance with the help of 'smart' sensors.
Most of the telemedicine technologies are concerned with the care of the elderly
people living in the community, but there is also a distinct necessity of having a
system of passive telealarm for the care of the elderly patients admitted in a geriatric
hospital.[2, 3] Patients who are at-risk of suffering a fall, wandering out of their
bedrooms, or have poor safety awareness like the demented, need a system of passive
teleassistance in addition to the conventional system of summoning help through the
use of bed-side or pendant alarms.
Steenkeste F., Banerjee- S. and Couturier P. (2004).
Telesurveillance of the Dependent Seniors Using Passive Infra-red Sensors in a Geriatric Hospital.
In Proceedings of the 1st International Workshop on Tele-Care and Collaborative Virtual Communities in Elderly Care, pages 86-96
DOI: 10.5220/0002679800860096
Copyright
c
SciTePress

With a view to improve the care of the elderly patients admitted in the hospital,
we installed a system of telesurveillance consisting of a passive infra-red sensor
network in a patient’s bedroom of a geriatric hospital in Grenoble, France. The main
purpose of our research was to study the validity of a ‘smart’ system of continuous
telesurveillance of the elderly patients consisting of a passive infra-red sensor network
in a hospital bedroom.[4] We also intended to monitor the nocturnal activities that
took place inside a patient’s room and eventually to find out any ‘deviation’ from the
‘normal’ pattern in case of a particular patient who happens to stay for a substantial
period in the hospital. It was developed with the aim of remote monitoring and
follow-up of chronic patients or elderly (or handicapped) people in order to prevent
accidents and aggravation of the disease.
2 Method
2.1 Consent
We had obtained a written consent from each patient (or his or her relatives in cases
where the patient was unable to provide a written consent) before he or she could
participate in the research.
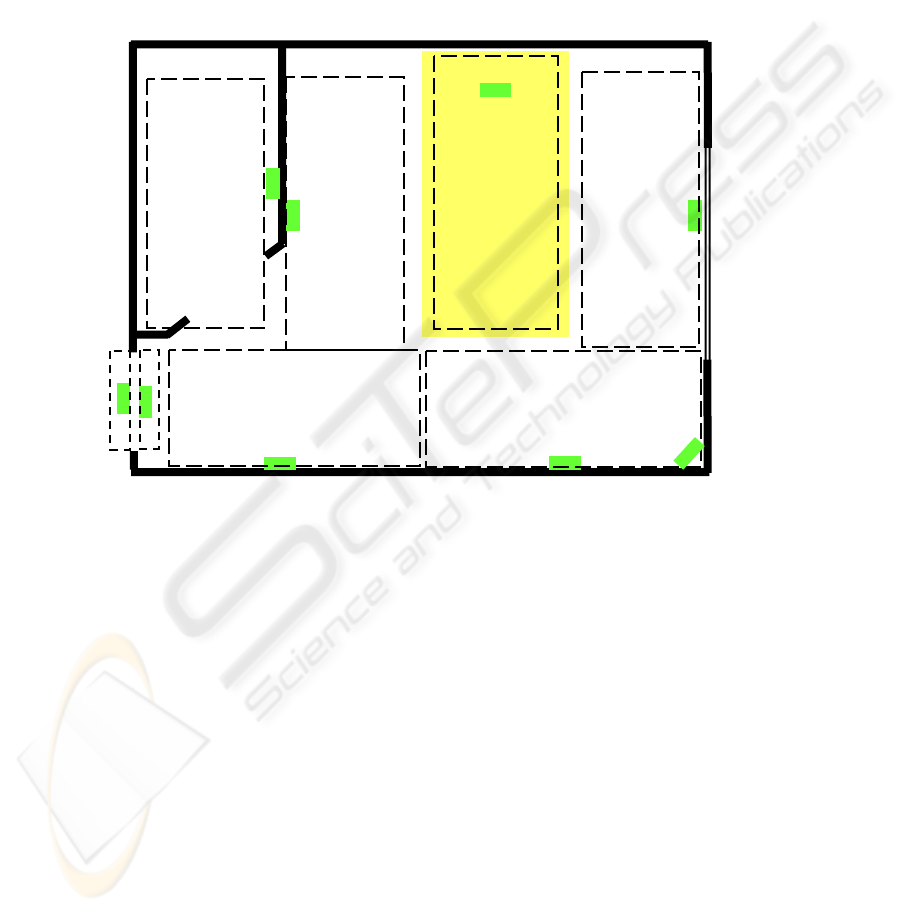
2.2 Sensors and Network
A hospital bedroom (3m by 3m) for a single patient was selected for the purpose of
study in Grenoble. Nine passive infra-red sensors were installed in the patient’s
bedroom; 8 of them were fixed vertically, at the ceiling level, in the different walls
and inside the toilet, the ninth (number 5) was screwed horizontally into the wall, at
1.2 meter above the ground. The plan of the room with the position of the sensors is
depicted in Fig. 1. These sensors are activated by human movements taking place in
the field of capture of the sensors, which is in the shape of a rectangular pyramid
covering approximately 1m by 2m area on the floor. The field of capture of the ninth
sensor covers horizontally entire room; its aim is to improve fall’s detection. The field
of capture or range of the other sensors can be narrowed down with the use of masks
if required in certain cases, so that they can only detect the passage of human beings
while passing just below a sensor. We used masks to reduce the field of detection in
cases of the door (both inside and outside) and the toilet sensors. These sensors were
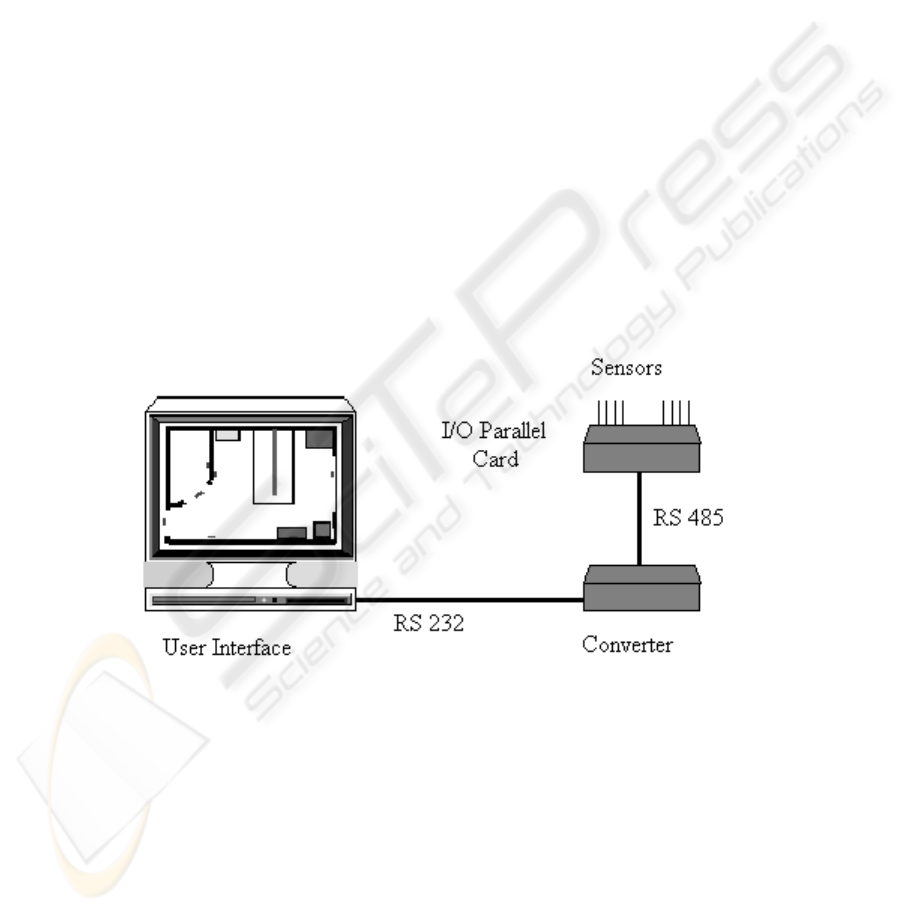
connected through cables to an I/O parallel card, which in turn was connected to a
Pentium III, 64 MB RAM computer kept in another observation room (Fig. 2).
2.3 Registration of movements during the night
The computer automatically captured and registered data obtained from the different
sensors every day from 10 a.m. till 8 a.m. in the next morning with the help of a
program known as GARDIEN
©
. Data corresponding to movements were collected
twice per second, and stored with indication of time when they differed. That is when
a different sensor or a different combination of sensors was activated due to the
movements of the patient, it was registered sequentially in that order, until the
sensor(s) came back to the original inactivated state, which was again registered
87
indicating the time in every instance. GARDIEN
©
registered movements made by the
single patient (along with occasional visits by the personnel or relatives) in the
bedroom during this span of 22 hours and saved them in a file with an extension name
‘.dat’. The artificial intelligence program analysed the data at the end of the
surveillance period and then generated a report showing a list of the activities[5]
taking place in the room with indication of the time of start and end of each
movement as well as the type of movement, like ‘Getting up and movement in room’,
‘Agitation in the bed’ and so on.
Fig. 1. Figure showing the different locations of the sensors inside the room. The dashed lines
represent the field of capture of the vertically set sensors
2.4 Document sheet maintained by the night personnel
In addition, the patient’s room was always visited by the personnel during the night.
This resulted in more than one person being present in the room during the period of
visit by the personnel. GARDIEN
©
was programmed in such a way that it could
differentiate the entry and exit of a personnel from that made by the patient. The night
personnel were given a document sheet to note their time of entry into the room,
number of persons entering the room, duration of stay and special remarks.
2.5 Analysis of the file and its comparison with the report generated by
GARDIEN
©
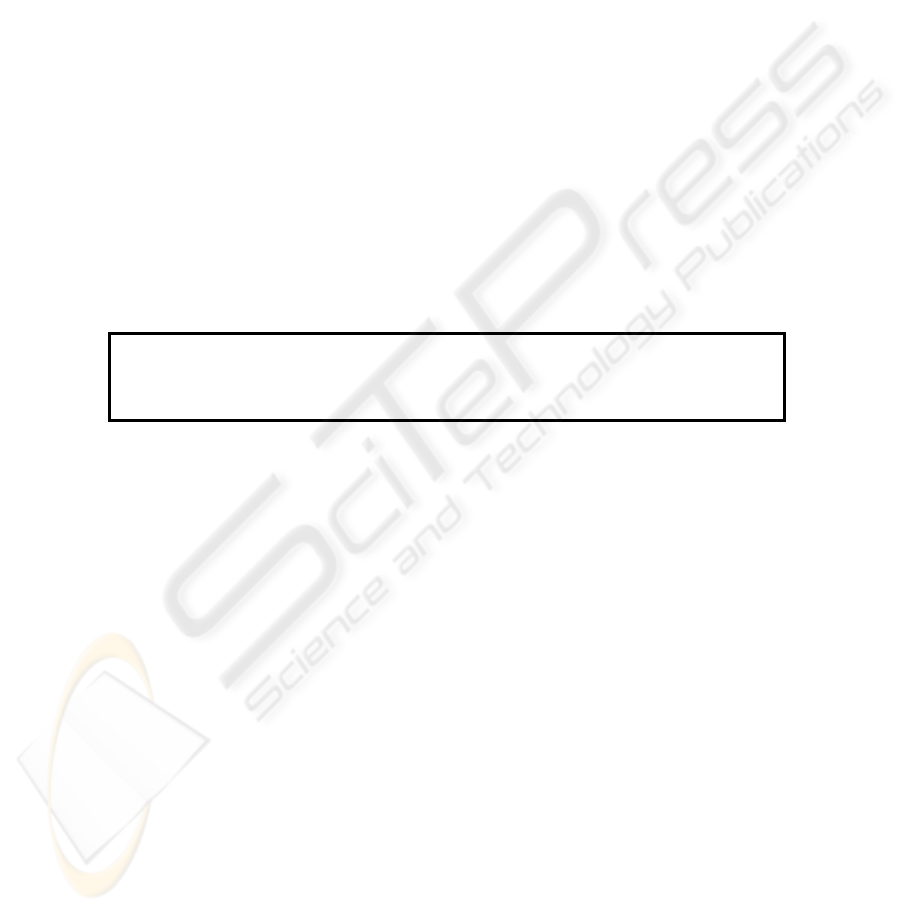
Every file that was created during the day was opened with a word processor the
following day and printed. A portion of a file is shown in Fig. 3. This print-out was
Bed
Toilet
1
3
2
4
6 A
C
8
5
88
analysed manually and thoroughly by an expert to find out all the activities that took
place in the bedroom during the night taking into account the document sheet filled by
the night personnel. The method of analysis is described as follows: at first, the file to
be analysed was divided into successive different sequences of valid movements (or
displacements) according to the rules described in the latter part of this section. Next,
within each sequence, each sensor denoted by a number, was noted with respect to the
previous sensor(s) registered in the file. In this manner, the ‘pattern’ of sensors
appearing in a sequence was noted one after another just as analysing a raw data
obtained from a discrete signal. The resulting analysed sequence was then compared
with the entry of the night personnel if noted in the document sheet and then a proper
movement name, like “Visit by the personnel, or Movement in the bathroom, etc.”,
was assigned to that particular analysed sequence, taken from a list of 24 movements.
Other sequences were also analysed in the same manner. The utility of the document
sheet by the night personnel was to confirm the presence of a visitor (more than one
person) in the room or the patient leaving the room, etc. when the same was found on
manual analysis. Following this, it was compared with the report generated by
GARDIEN
©
, which was programmed to analyse the sequences automatically and
independently by an intelligent algorithm and then put it in the form of a report (Fig
4) containing a series of activities (with reference to time) taking place during the
night, i.e., each movement analysed manually was compared with each movement
reported by GARDIEN
©
to find out if they matched with one another.
Fig. 2. The GARDIEN
©
system
Certain conditions were applied while analysing the print-outs manually and
comparing them with the reports produced by GARDIEN
©
. The determination of a
displacement, whether by manual analysis or automatic treatment by GARDIEN
©
, is
based on two criteria: Interval I (in seconds) separating two consecutive data (lines)
and D number of data (minimum number) lines of activation of sensors in a sequence)
89
was corresponding to a state of activation of the sensor network. When a sensor is
activated by the passage of a person underneath, it remains activated as long
Fig 3 This sequence was analyzed as “Movement in the room and in the toilet”
ACTIMETRIE DEAMBULATOIRE
Nuit du : 15 Mar 2003 au : 16 Mar 2003
Copyright 1999 © INSERM U518
Nota : Les agitations au lit, de moins de 3 mouvements, ne sont pas notées.
Les déplacements sont séparés par des temps de repos d’au moins 30 secondes.
Déplacement
Début Fin Commentaires
21 :00 :59 21 :03 :10 Plusieurs personnes dans la chambre
21 :03 :35 21 :04 :20 Recoucher du patient accompagné par le personnel
21 :07 :30 21 :09 :53 Lever, Déplacements dans la chambre et recoucher
21 :19 :31 21 :23 :05 Lever, Déplacements dans la chambre et recoucher
22 :58 :01 23 :00 :46 Lever, Déplacements dans la chambre et recoucher
23 :44 :08 23 :44 :33 Lever et Déplacements dans la chambre
23 :57 :44 23 :58 :51 Lever du patient et sortie de la chambre
00 :01 :27 00 :03 :31 Recoucher du patient accompagné par le personnel
00 :04 :06 00 :04 :42 Agitation au lit
01 :03 :21 01 :03 :22 Ronde du personnel
01 :13 :00 01 :14 :08 Lever du patient et sortie de la chambre
01 :15 :54 01 :16 :36 Retour et sortie du patient
01 :17 :27 01 :19 :37 Retour du patient et recoucher
05 :20 :49 05 :22 :25 Lever du patient et sortie de la chambre
05 :22 :56 05 :24 :29 Retour du patient et recoucher
Fig 4 A report of nocturnal activities
4 6 Fri Mar 07 10:49:14 2003
4 Fri Mar 07 10:49:14 2003
34 Fri Mar 07 10:49:17 2003
3 Fri Mar 07 10:49:17 2003
23 Fri Mar 07 10:49:19 2003
2 Fri Mar 07 10:49:20 2003
Fri Mar 07 10:49:22 2003
2 Fri Mar 07 10:49:23 2003
Fri Mar 07 10:49:23 2003
2 Fri Mar 07 10:49:24 2003
Fri Mar 07 10:49:26 2003
C Fri Mar 07 10:49:28 2003
Fri Mar 07 10:49:29 2003
C Fri Mar 07 10:49:34 2003
90

as there is movement under that particular sensor and for an additional duration of 0.5
second after the cessation of the movement. At that instance, the state of the sensor
network is modified (inactive state), which is registered with indication of time. If a
new change of state appears during the interval I following it, the movement which
provoked this change of state is considered to belong to the same displacement.
Whereas, if there is movement producing a change of state after the interval I, it is
considered to be a new set of data for the next displacement. In order to be considered
a significant movement, a displacement must consist of D data (lines) in accordance
with the above criterion. In our experiment, we had fixed I = 30 seconds and D = 5.
This means that if there is a movement causing activation of the sensor after 30
seconds of inactivity, it will be considered to be a part of the following displacement.
In addition, there has to be at least five data (lines) in a displacement in order to
consider significant. GARDIEN
©
is provided with a facility to alter these thresholds,
with I being 60 seconds and D as 20 maximum.
In the same time, a counter was increased by the duration of the movement; there
was a counter for each kind of movement (bed activity, room activity, …). Each
quarter of an hour, the activation’s duration of each sensor was calculated too. When
GARDIEN
©
finished analyzing the data file, patient’s references ( name, address .)
were asked to the medical user and then the report was printed, the movement’s
counters and the sensors counters were stored in a patient file with an extension name
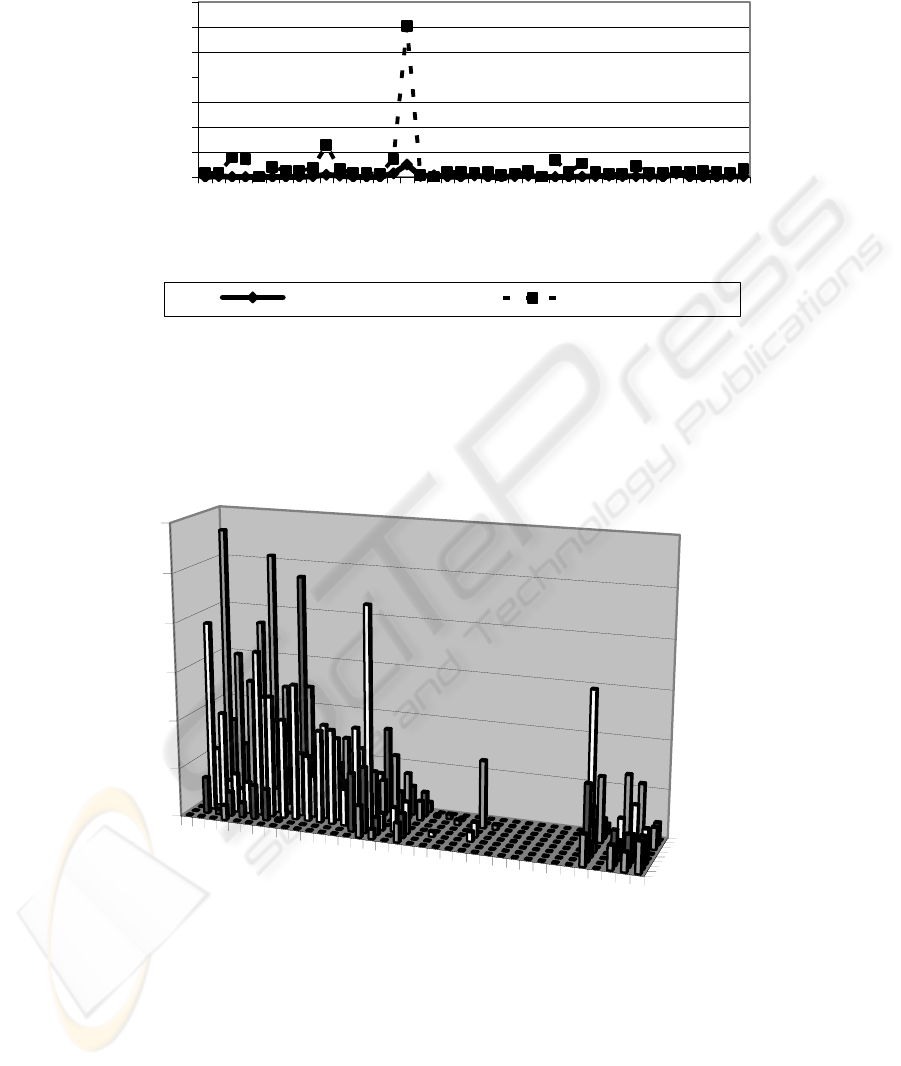
‘.reu’, together with the date. This file was used by the Graphical User Interface to
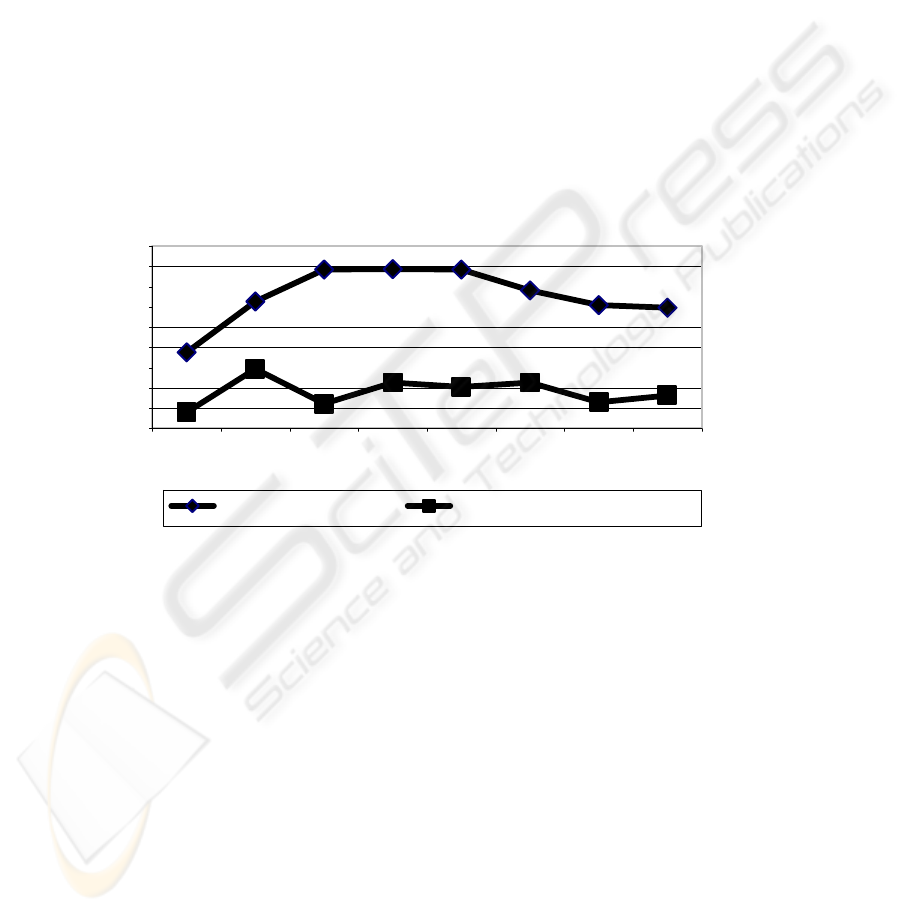
display in the form of curves, the duration of each kind of movement per night (Fig 5)
and in the form of three-dimensional histograms the duration‘s activation of sensors
in each part of the room per quarter of an hour (Fig 6).
3 Results
During the technical evaluation period, we detected 1637 valid sequences [6] of
movements taking place in the room by analysing manually. Of these, 10 movements
were not detected by GARDIEN
©
(i.e., 1627 movements were detected). In addition,
1450 movements, i.e., 88.6% of the movements, analysed manually by the expert
were interpreted in the same manner by GARDIEN
©
.
The total number of entries made by the night personnel entering the room was
found to be 341, of which GARDIEN
©
was able to pick-up 332 times (97.4%) that
there was an external person visiting the room, which indicates the ‘sensitivity’ of the
system to detect any reported event. The nine instances when these events remained
undetected could be either due to the passage of the night personnel in the corridor
passing ‘near’ the patient’s room without actually entering ‘inside’ or due to the faulty
noting of the ‘time of entry’ by the night personnel.
The clinical evaluation period of GARDIEN
©
continued during 486 days. 23
Alzheimer patients occupied the room during this time; 16 of them had cognitive
impairment and a MMS (Mini Mental State) score lower than 25, the others had a
MMS score higher than 25 but no cognitive problems. The median motor activity was
stable during the without cognitive impairment patient’s stay. On the other hand, this
activity was more important at the beginning of the stay and decreased during the
observation period of the patients with cognitive disease (Fig 7).
91
0
20
40
60
80
100
120
140
1 4 7 1013161922252831343740
N° of Continuous nights
Duration (min.)
Bed activity Room activity
Fig 5 Nocturnal activity in an 77-year-old patient with hyperactivity in room on the 16
th
night
21 H 15
21 H 45
22 H 15
22 H 45
23 H 15
23 H45
0 H 15
0 H 45
1 H 15
1 H 45
2 H 15
2 H 45
3 H 15
3 H 45
4 H 15
4 H 45
5 H 15
5 H 45
Entree
Salle de bains
0
20
40
60
80
100
120
No.
of
activation of sensors
Time
W
Fig. 6 Activity in the room during one particular night when the patient was excessively
agitated initially followed by a period of sleep and finally waking up at five o’clock in the next
morning
92
Although, all the patients were Alzheimer patients, their nocturnal motor activity
patterns were different and we found three kind of pattern:
- acute nocturnal agitation,
- chronic nocturnal hyperactivity
- mental confusion.
These features are illustrated by three patients. In the first case, the patient
was 77 year-old male patient. His was admitted in the geriatric department for
agitation, aggressiveness and violence against his wife at home. He was observed for
41 nights. On the 12
th
day, he complained of shortness of breath and abdominal pain.
On the 16
th
night (Fig 5), he moved excessively in the room as well as in the corridor
(this fact was noted by the night personnel). On the basis of previous complaints and
excessive activity, a pulmonary Scintigraphy and Echo-Doppler study were
performed. The scintigraphy showed a strong possibility of Pulmonary Embolism. An
anticoagulant therapy was started, the nocturnal motor activity became less important
and the patient recovered fully after treatment.
0
100
200
300
400
500
600
700
800
900
12345678
N° Of Continuous Nights
Duration (s )
Cognitive impairment Without cognitive impairment
Fig 7 Influence of cognitive problems on nocturnal motor activity
The second case was an 87 year-old female patient. She was admitted in the
geriatric unit for rehabilitation after a rib fracture. During her entire stay, she never
presented with agitation or an episode of fugue. She frequently suffered from spatio-
temporal disorientation. Her room activity chart (Fig 8) showed irregular fluctuations
but we did not know precise cause. We found only that she slept several times during
small intervals interrupted by motor activity sequences. She stayed for 63 days in the
geriatric department.
The third patient was a 93 year-old man. He was admitted for agitation,
aggressiveness and violence against his wife. He stayed 38 days in the department.
This patient was very calm during the day but his nocturnal motor activity was
important. On the 14
th
day, the treating physician changed therapy in order to reduce
the patient’s daytime somnolence and restore sleep during the night. The therapeutic
93
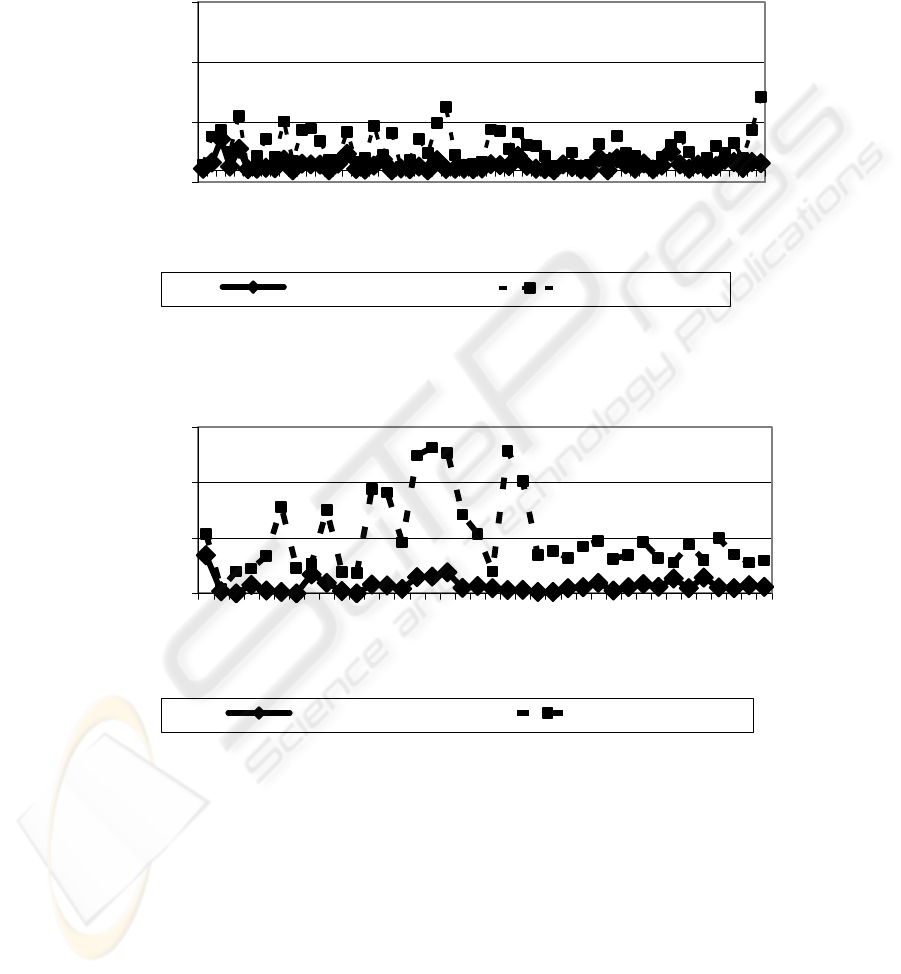
change had effect about one week later and the nocturnal motor activity of this patient
decreased progressively (Fig 9).
-10
40
90
140
1 5 9 13172125293337414549535761
N° of Continuous nights
Duration (min.)
Bed activity Room activity
Fig 8 Example of chronic nocturnal hyperactivity
0
50
100
150
1 3 5 7 9 1113151719212325272931333537
N° of Continuous nights
Duration (min.)
Bed activity Room activity
Fig 9 Example of mental confusion superimposed on chronic hyperactivity
4 Discussion
We found that the most important step in determining the accuracy or reliability of the
system was to find out how the program (algorithm) treated or analysed the data thus
obtained. That is whether GARDIEN
©
was able to interpret the data in the same
manner as it would have appeared to the expert analysing the data manually. This
accuracy (88.6%) was consistent throughout the period of observation that is there
94

was not significant fluctuation in the day to day results obtained. However, 10
movements (out of a total of 1637 movements) were undetected by the system. We
found that all the movements that were not detected were actually of very short
sequence (5 or 6 sensors). The reason was due to failure of the treatment of data
stored in the .dat file by the program.
The system is generally capable of detecting all major movements in the room.
But in the event, when the patient happens to stand near the door, but not causing
movement for a long period without actually leaving the room, will be detected as
‘patient leaving the room’, since the last sensor to be activated will be the outside
door sensor. Similarly, the system couldn’t tell where the patient is lying in the room
if he or she is stationary for a long period, either on the bed or on the floor, since the
infra-red sensors will become inactive due to the absence of movement. But if the
patient falls and stirs on the floor, his movement is detected by the vertical sensors but
it is not detected by the ninth sensor (horizontal). In this case, GARDIEN
©
can sound
an alarm. Since the ninth sensor is working, GARDIEN
©
and the caregivers did not
note a patient fall; consequently, we can’t conclude yet about the efficiency of this
sensor.
Most of the telesurveillance systems that have been developed or tested until now,
used a system of multisensors in which infra-red sensors were used along with other
types of environmental sensors or wearable sensors (fall sensor for example). [7-10]
In all these cases, the data obtained from different sources were combined by ‘fusion
of data’ regarding activity of a person within an intelligent habitat. The installation of
a multisensor system increases the complexity of the habitat in addition to increasing
the expenditure. Moreover, the infra-red sensors that were used in all these cases, only
detected the presence or absence of a person by noting the movements within the
room.
GARDIEN
©
, on the other hand, was developed only with passive infra-red
sensors, which due to its intelligent algorithm could not only detect the presence or
absence of a person, but also detected the type of activities done by the person within
the room including his or her exit from the room. This is an important aspect of the
system since it permits distinction between the entry and exit of night personnel with
that of the patient. This feature could well, in future, be combined with a system of
passive telealarm that can alert the caregivers in real-time whenever the patient tries
to leave the room, which are many times associated with falls or getting injured in the
corridor. The simplicity of installation of infra-red sensors within a room is a plus
point, since no other type of sensor is required.
Another important feature of the system is that nocturnal actimetry of the persons
living in the room is possible. The activity inside the room during one night is shown
in Fig. 6. In this figure, one can note that the patient was extremely agitated from
21.15 till 01.30 hours in the next morning. Following which, there was a period of
sleep lasting till 05.00 hours, when activity due to waking up was noted. For patients
staying for a longer period, it may serve as a means of identifying motor activity
trends that can provide data to the physicians to monitor the patient and attribute
deviations in the activity trend to various therapeutic interventions.
Studying behaviour trends in relation to treatment may help planning therapy and
follow-up of the patients. In addition, sleep patterns may be discovered in patients
suffering from insomnia. A patient with a known seizure disorder showing excessive
agitation in the bed on a particular night could signal a convulsion and in turn may be
95

programmed to activate the alarm, although further studies are necessary to accept the
reliability of the system in alerting the health personnel in such emergency conditions.
On the other hand, diminished motor activity in the bed in a bed-ridden patient could
forewarn the onset of bed-sores.
As GARDIEN
©
is an environmental sensor, it is compatible to be used
simultaneously with any other medical or body-attached sensors providing
complementary data on the patient, like devices measuring heart rate, ECG, blood
pressure, or fall detectors (accelerometers).
At last, the patients who stayed in the room during the period of observation did
not feel any discomfort with the system, but further study is necessary to establish its
acceptability in the community.
References :
1 Doughty K, Cameron K, Garner P. Three generations of the telecare of the elderly. J
Telemed Telecare 1996; 2(2): 71-80
2 Tyrrell J. Evaluation of Telemedicine: Patient needs and perceived benefits of an innovative
communication system in a geriatric rehabilitation unit. European Commission : Training
and Mobility of Researchers Programme 1998
3 Couturier P, Tyrrell J, Banerjee S, Debray M, Moulin P, Franco A. Téléassistance en milieu
gériatrique : besoin du patient et réponses technologiques. Aides techniques et matériel
d’assistance en gériatrie (édition: Masson), 2002: 63-73
4 Steenkeste F, Bocquet H, Chan M, Campo E. La mise en place d'une technologie pour
observer le comportement nocturne des personnes âgées en institution. ITBM-RBM 2001;
22: 25-30
5 Steenkeste F., Banerjee S., Couturier P., Franco A. GARDIEN: un système de
telesurveillance pour personnes âgées dépendantes. Proc. of Les Nouvelles Technologies
dans la Cité Rennes 11 décembre 2003
6 Banerjee S., Steenkeste F., Couturier P., Debray M., Franco A. Telesurveillance of elderly
patients by use of passive infra-red sensors in a ‘smart room’. J Telemed Telecare 2003; 9;
23-29
7 Coyle G, Boydell L, Brown L. Home telecare for the elderly. J Telemed Telecare 1995; 1:
183-184
8 Ogawa M, Togawa T. Monitoring daily Activities and behaviors at home by using brief
sensors. Proc. of the 1
st
Annual International IEEE-EMBS Special Topic Conference on
Microtechnologies in Medicine and Biology 2000
9 Chan M, Bocquet H, Campo E, Val T, Estève D, Pous J. . Multisensor system and artificial
intelligence in housing for the elderly. Gerontechnology, IOS Press, 1998: 145-149
10 Rialle V, Lauvernay N, Franco A, Piquard JF, Couturier P. A smart room for hospitalised
elderly people: essay of modelling and first steps of an experiment. Technol and Health
Care 1999; 7(5): 343-357
Acknowledgement
The authors would like to thank the patients who participated in the research and the hospital
staff of Elisée Chatin, Grenoble, France who filled the document sheet every night.
This work was supported by the French Ministry of National Education, Research and
Technology, The France Alzheimer Association, and the Agrica Fondation.
96
