
A CASE-BASED DIALOGUE SYSTEM FOR INVESTIGATING
THERAPY INEFFICACY
Rainer Schmidt and Olga Vorobieva
Institute for Medical Informatics and Biometry, University of Rostock, Rembrandtstr. 16/17, Rostock, Germany
Keywords: Case-Based Reasoning, Therapy Support, Medicine, Endocrine, Psychiatry.
Abstract: ISOR is a Case-Based Reasoning system for long-term therapy support in the endocrine domain and in
ps
ychiatry. ISOR performs typical therapeutic tasks, such as computing initial therapies, initial dose
recommendations, and dose updates. ISOR deals especially with situations where therapies become
ineffective. Causes for inefficacy have to be found and better therapy recommendations should be
computed. In addition to former already solved cases, ISOR uses further knowledge forms, especially
medical histories of query patients themselves and prototypes. Furthermore, the knowledge base consists of
therapies, conflicts, instructions etc. So, different forms and steps of retrieval are performed, while
adaptation occurs as an interactive dialog with the user.
1 INTRODUCTION
In medical practice, therapies prescribed according
to a certain diagnosis sometimes do not give desired
results. Sometimes therapies are effective for some
time but suddenly stop helping any more. There are
many different reasons. A diagnosis might be
erroneous, the state of a patient might have changed
completely or the state might have changed just
slightly but with important implications for an
existing therapy. Furthermore, a patient might have
caught an additional disease, some other
complication might have occurred, or a patient
might have changed his/her lifestyle (e.g. started a
diet) etc.
For long-term therapy support in the endocrine
dom
ain and in psychiatry, we have developed a
Case-Based Reasoning system, named ISOR, that
not only performs typical therapeutic tasks but also
especially deals with situations where therapies
become ineffective. Therefore, it first attempts to
find causes for inefficacy and subsequently
computes new therapy recommendations that
should perform better than those administered
before.
ISOR is a medical Case-Based Reasoning system
th
at deals with the following tasks:
- choose appropriate (initial) therapies,
- compute doses for chosen therapies,
- update dose recommendations according to
lab
oratory test results,
- establish new doses of prescribed medicine
according to changes in a pat
ient’s medical status
or lifestyle,
- find out probable reasons why administered
th
erapies are not as efficient as they should,
- test obtained reasons for inefficacy and
make
sure that they are the real cause, and
- suggest recommendations to avoid inefficacy of
presc
ribed therapies.
ISOR deals with long-term diseases, e.g.
psychiatric
diseases, and with diseases even lasting for a
lifetime, e.g. endocrine malfunctions.
For psychiatric diseases some Case-Based
R
easoning systems have been developed, which deal
with specific diseases or problems, e.g. with
Alzheimer’s disease (Marling and Whitehouse,
2001) or with eating disorders (Bichindaritz, 1994).
Since we do not want to discuss various psychiatric
problems but intend to illustrate ISOR by
understandable examples, in this paper we focus
mainly on some endocrine and psychiatric disorders,
namely on hypothyroidism and depressive
symptoms. Inefficacy of pharmacological therapy
for depression is a widely known problem (e.g.
(Barbee and Jamhour, 2002), (Cuffel et al, 2003),
(Hirschfeld, Montgomery et al, 2002), (Keitner,
Posternak, and Ryan, 2003), (Lam, Wan, Cohen, and
Kennedy, 2002)). There are many approaches to
171
Schmidt R. and Vorobieva O. (2007).
A CASE-BASED DIALOGUE SYSTEM FOR INVESTIGATING THERAPY INEFFICACY.
In Proceedings of the Second International Conference on Software and Data Technologies - PL/DPS/KE/WsMUSE, pages 171-178
Copyright
c
SciTePress
solve this problem. Guidelines and algorithms have
been created (e.g. (Alacorn, Glover, Boyer, and
Balon, 2000), (Expert Consensus Guideline Series,
2000) (Osser and Patterson, 1998)). ISOR gives
reference to a psychopharmacology algorithm (Osser
and Patterson, 1998) that is available on the website
htp://mhc.com/Algorithms/Depression.
The paper is organized as follows. Firstly, we
introduce typical therapeutic tasks, subsequently
we present the architecture of ISOR and finally we
illustrate how it works by examples.
2 TYPICAL THERAPEUTIC
TASKS
As a consequence of our experiences with ICONS
(Schmidt and Gierl, 2001) a system for antibiotic
therapy advice, and with therapy support programs
for hypothyroidism (Vorobieva, Gierl, and
Schmidt, 2002), we believe that four tasks exist for
medicinal therapies. The first one means
computing an initial therapy, secondly an initial
dose has to be determined, later on dose updates
may be necessary, and finally interactions with
further diseases, complications, and especially with
already administered therapies have to be
considered.
In the following we illustrate the four tasks by
our programs that deal with therapy support for
hypothyroid patients. The antibiotics therapy
adviser ICONS deals only with two of these tasks:
computing initial therapies and initial doses.
2.1 Computing an Initial Therapy
Probably, the most important task for therapies is
the computation of initial therapies. The main task
of ICONS is to compute promising antibiotic
therapies even before the pathogen that caused the
infection is determined in the laboratory. However,
for hypothyroidism ISOR does not compute initial
therapies but only initial doses, because for
hypothyroidism only one therapy is available: it is
thyroid hormone, usually in form of levothyroxine.
2.2 Computing an Initial Dose
In ICONS the determination of initial doses is a
rather simple task. For every antibiotic a specific
calculation function is available and has to be
applied.
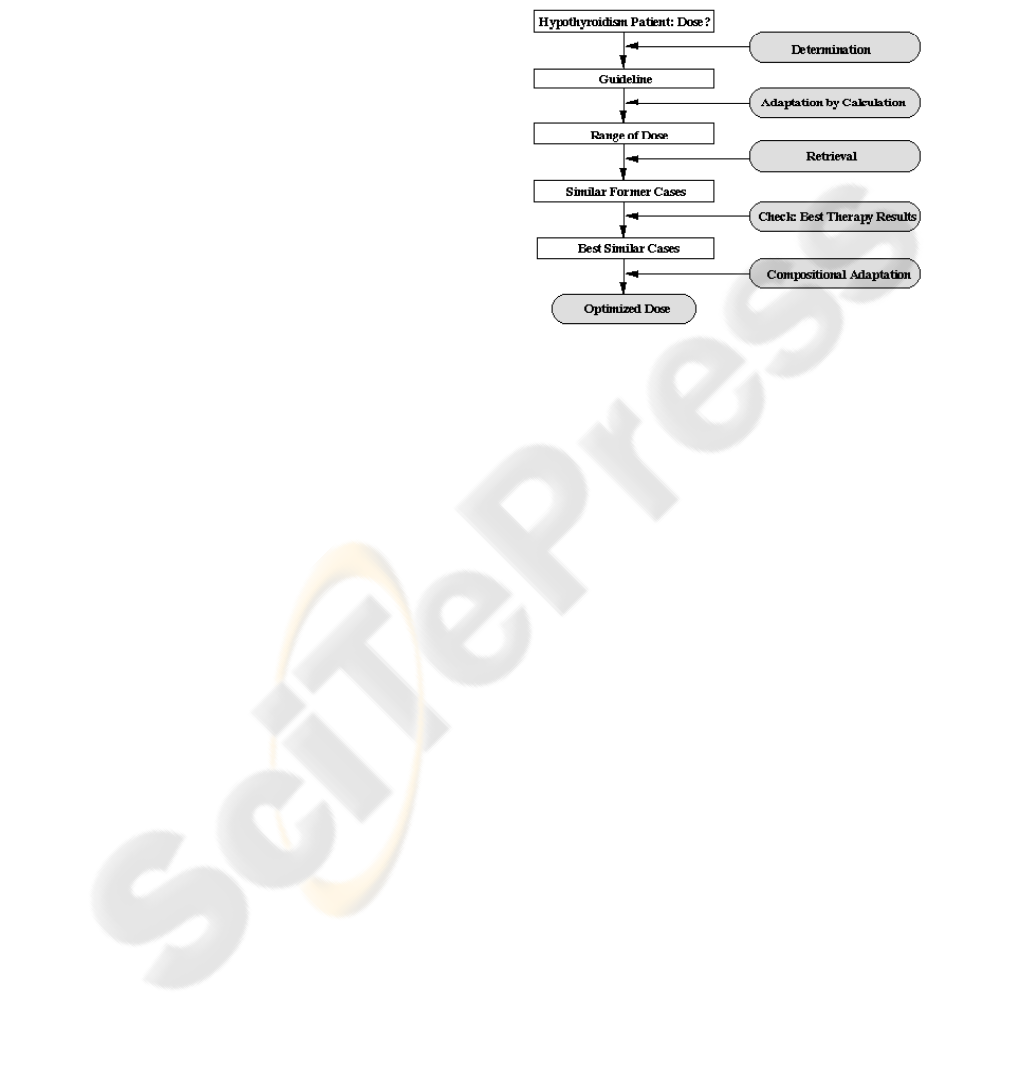
For hypothyroidism the determination of initial
doses (figure 1) is more complicated. Firstly, a
couple of prototypes exist. These are
recommendations that have been defined by expert
commissions. Though we are not sure whether they
are officially accepted, we call them guidelines. The
assignment of a patient to a fitting guideline is
obvious because of the way the guidelines have been
defined. With the help of these guidelines a range
for good doses can be calculated.
Figure 1: Determination of an initial levothyroxine dose.
To compute a dose with best expected impact, we
retrieve similar cases whose initial doses are within
the calculated ranges. Since cases are described by
few attributes and since our case base is rather
small, we use Tversky's sequential measure of
dissimilarity (Tversky, 1977). On the basis of those
retrieved cases that had best therapy results an
average initial therapy is calculated. Best therapy
results can be determined by values of a blood test
after two weeks of treatment with the initial dose.
The opposite idea to consider cases with bad
therapy results does not work here, because bad
results can also be caused by various other reasons.
To compute optimal dose recommendations, we
apply two forms of adaptation. First, a calculation of
ranges according to guidelines and patients attribute
values. Secondly, we use compositional adaptation.
That means, we take only similar cases with best
therapy results into account and calculate the
average dose for these cases, which has to be
adapted to the query patient by another calculation.
2.3 Updating the Dose in a Patient's
Lifetime
For monitoring a hypothyroidism patient, three basic
laboratory blood tests (TSH, FT3, FT4) have to be
undertaken. Usually the results of these tests
correspond to each other. Otherwise, it indicates a
more complicated thyroid condition and additional
tests are necessary. If the results of the basic tests
ICSOFT 2007 - International Conference on Software and Data Technologies
172

show that the patients thyroid hormone level is
normal, it means that the current levothyroxine dose
is OK. If the tests indicate that the thyroid hormone
level is too low, the current dose has to be increased
by 25 or 50 μg, if it is high, the dose has to be
decreased by 25 or 50 μg ((DeGroot, 1994),
(Hampel, 2000)). So, for monitoring, adaptation
means calculating according to some rules, which
are based on guidelines. Since an overdose of
levothyroxine may cause serious complications for a
patient, a doctor cannot simply consider test results
and symptoms that indicate a dose increase but
additionally he/she has to investigate reasons why
the current dose is not appropriate any more. In
ISOR this situation is described as a problem of
therapy inefficiency. In most cases the solution is
obvious, e.g. puberty, pregnancy etc. These
situations are covered by adaptation rules.
Sometimes cases are observed in which the
hypothyroidism syndromes are unexplained. For
these cases ISOR uses the problem solving program.
2.4 Additional Diseases or
Complications
It often occurs that patients do not only have
hypothyroidism, but they suffer from further chronic
diseases or complications. Thus, a levothyroxine
therapy has to be checked for contraindications,
adverse effects and interactions with additionally
existing therapies. Since no alternative is available
to replace levothyroxine, if necessary additionally
existing therapies have to be modified, substituted,
or compensated ((DeGroot, 1994), Hampel, 2000)).
ISOR performs three tests. The first one checks
if another existing therapy is contraindicated to
hypothyroidism. This holds only for very few
therapies, namely for specific diets like soybean
infant formula, which is the most popular food for
babies who do not get enough mother’s milk but it
prevents the effect of levothyroxine. Such diets have
to be modified. Since no exact knowledge is
available to explain how to accomplish this, our
program just issues a warning saying that a
modification is necessary.
The second test considers adverse effects. There
are two ways to deal with them. A further existing
therapy has either to be substituted or it has to be
compensated by another drug. Such knowledge is
available, and we have implemented corresponding
rules for substitutional and compensational
adaptation.
The third test checks for interactions between
both therapies. We have implemented some
adaptation rules, which mainly attempt to avoid the
interactions. For example, if a patient has heartburn
problems that are treated with an antacid, a rule for
this situation states that levothyroxine should be
administered at least four hours after or before an
antacid. However, if no adaptation rule can solve
such an interaction problem, the same substitution
rules as for adverse effects are applied.
3 SYSTEM ARCHITECTURE
ISOR is designed to solve typical problems,
especially inefficacy of prescribed therapies that
can arise in different medical domains. Therefore
most algorithms and functions are domain
independent. Another goal is to cope with
situations where important patient data is missing
and/or where theoretical domain knowledge is
controversial.
ISOR does not generate solutions itself. Its task
is to help users by providing all available
information and to support them to find optimal
solutions. Users shall be doctors, maybe together
with a patient.
Technically, ISOR is implemented in Delphi 7,
the format for the case and knowledge bases is
Paradox 7, and retrieval is performed by SQL.
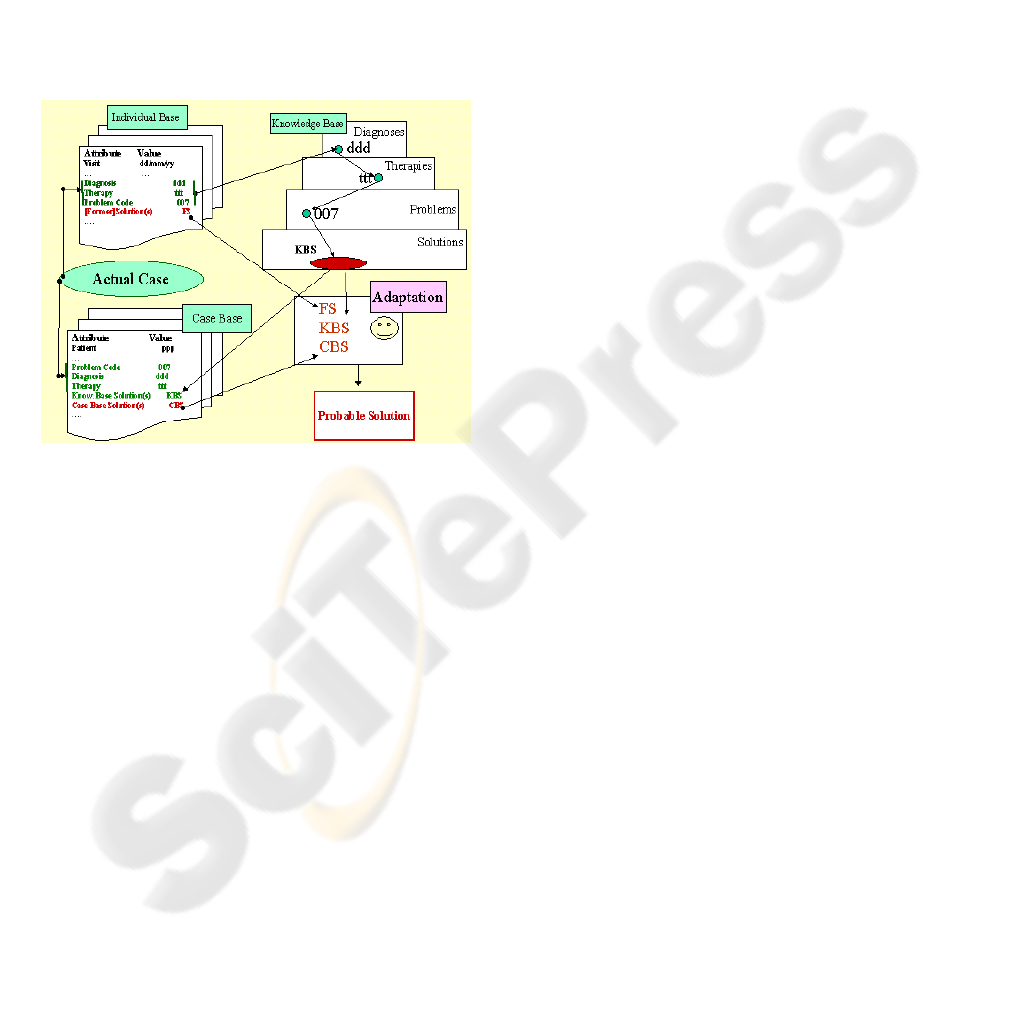
In addition to the typical Case-Based Reasoning
knowledge, namely former already solved cases,
ISOR uses further knowledge components, namely
medical histories of query patients themselves and
prototypical cases (prototypes). Furthermore,
ISOR’s knowledge base consists of therapies,
conflicts, instructions etc. The architecture is
shown in figure 2.
In this section we explain the components and
in the next chapter we present examples to show
how the main knowledge components work
together.
3.1 Medical Case Histories
Ma and Knight (Ma and Knight, 2003) have
introduced a concept of case history in Case-Based
Reasoning. Such an approach is very useful when
we deal with chronic patients, because often the
same complications occur again, former successful
solutions can be helpful again, while former
unsuccessful solutions should be avoided.
The case history is written in the patient’s
individual base as a sequence of records. A
patient’s base contains his/her whole medical
history, all medical information that is available:
diseases, complications, therapies, circumstances
of his/her life etc. Each record describes an episode
in a patient’s medical history. Episodes often
characterise a specific problem. Since the case base
A CASE-BASED DIALOGUE SYSTEM FOR INVESTIGATING THERAPY INEFFICACY
173
is problem oriented, it contains just episodes and
the same patient can be mentioned in the case base
a few times, even concerning different problems.
Information from the patient’s individual base
can be useful for a current situation, because for
patients with chronic diseases very similar problems
often occur again. If a similar situation is found in
the patient’s history, it is up to the user to decide
whether to start retrieval in the general case base or
not.
In endocrinology, case histories are designed
according to a standard scheme, one record per visit.
Every record contains the results of laboratory tests
and of an interrogatory about symptoms, complaints
and physiological conditions of a patient.
Figure 2: ISOR’s architecture.
Therefore the retrieval of former similar situations
from the individual base of an endocrine patient is
easy to organise.
For psychiatric patients, case histories are often
unsystematic and they can be structured in various
forms. A general formalisation of psychiatric cases
and their histories is not achieved yet. The design of
case histories is problem dependent.
In both domains, we first search in the query
patient’s history for similar problems and for similar
diagnoses.
3.2 Knowledge Base, Case Base, and
Prototypes
The knowledge base contains information about
problems and their solutions that are possible
according to the domain theory. It has a tree
structure and it consists of lists of diagnoses,
corresponding therapies, conflicts, instructions, and
medical problems (including solutions) that can arise
from specific therapies. The knowledge base also
contains links to guidelines, algorithms and
references to correspondent publications ((Alacorn,
Glover, Boyer, and Balon, 2000), (Expert Consensus
Guideline Series, 2000), (Osser, and Patterson,
1998)).
The case base is problem oriented. Thus a case in
the case base is just a part of a patient’s history,
namely an episode that describes a specific problem
that usually has a solution too. So, the case base
represents decisions of doctors (diagnosis, therapies)
for specific problems, and their generalisations and
their theoretical foundations (see the examples). A
solution is called “case solution”, abbreviated “CS”.
Every case solution has (usually two)
generalisations, which are formulated by doctors.
The first one is expressed in terms of the knowledge
base and it is used as a keyword for searching in the
knowledge base. Such a generalisation is called
“knowledge base solution”, abbreviated “KBS”. The
second generalisation of a solution is expressed in
common words and it is mainly used for dialogues.
It is called “prompt solution”, abbreviated “PS”.
Former cases (attribute value pairs) in the case
base are indexed by keywords. Each case contains
keywords that have been explicitly placed by an
expert. For retrieval three main keys are used: a code
of the problem, a diagnosis, and a therapy. Further
keys such as age, sex etc. can be used optionally.
Prototypes (generalized cases) play a particular
role. Prototypes help to select a proper solution from
the list of probable or available solutions. A
prototype may help to point out a reason of
inefficacy of a therapy or it may support the doctor’s
choice of a drug.
3.3 Retrieval, Adaptation, and
Dialogue
For retrieval keywords are used. Since our system
is problem oriented, the first one is a code that
implies a specific problem. The second keyword is
the diagnosis and the other ones are retrieved from
the knowledge base.
Adaptation takes place as a dialogue between
the doctor, the patient, and the system. The system
presents different solutions, versions of them, and
asks questions to manifest them. The doctor
answers and selects suggestions, while the patient
himself or herself suggests possible solutions that
can be considered by the doctor and by the system.
We differentiate between two steps of
adaptation. The first one occurs as a dialogue
between ISOR and a user. Usually, doctors are the
users. However, sometimes even a patient may take
part in this dialogue. The goal of these dialogues is
to select probable solutions from all information
sources mentioned in sections 3.1 and 3.2. Pieces
ICSOFT 2007 - International Conference on Software and Data Technologies
174

of information are retrieved by the use of
keywords. Specific menus support the retrieval
process. The first step of adaptation can be
regarded as partly user based: ISOR presents lists
of probable solutions and menus of keywords, the
user selects the most adequate ones. The second
adaptation means proving obtained solutions. This
proving is rule based and it includes further
dialogues, laboratory test results, and consultations
with medical experts. While the procedures
supporting the first adaptation step are domain
independent, the adaptation rules of the second step
are mainly domain dependent.
4 EXAMPLES
By three examples we illustrate how ISOR works.
The first and the second one are from the endocrine
domain, the third one deals with a psychiatric
problem.
4.1 Hypothyroidism
4.1.1 Inefficacy of Levothyroxine Therapy
Every morning a mother gives her 10 year-old boy
not only the prescribed Levothyroxine dose but
also vitamin pills. These pills have not been
prescribed but they are healthy and have lately
been advertised on TV. Part of this medication is
Sodium Hydrocarbonate (cooking soda) that causes
problems with Levothyroxine.
Individual base. The same problem, inefficacy
of Levothyroxine therapy, is retrieved from the
patient’s history. The solution of the former
problem was that the boy did not take the drug
regularly. This time it must be a different cause,
because the mother controls the intake.
Knowledge base. It has a tree structure that is
organised according to keys. One main key is
therapy and the keyword is Levothyroxine. Another
keyword is instructions. These instructions are
represented in form of rules that concern the intake
of Levothyroxine. For Levothyroxine a rather long
list of instructions exists. Since the idea is that the
boy may break an instruction, this list is sorted
according to the observed frequency of offences
against them in the case base.
Concerning these instructions a couple of
questions are asked, e.g. whether the boy takes
Sodium Hydrocarbonate together with
Levothyroxine. Since the mother is not aware of
the fact that Sodium Hydrocarbonate is contained
in the vitamin pills, she gives a negative answer
and no possible solution can be established by the
knowledge base. However, soda is generated as
one keyword for retrieval in the case base.
So, the following solutions are retrieved from
the knowledge base, the third one does not fit for
the boy.
Knowledge base solution 1: Sodium Hydrocarbon
Knowledge base solution 2: Soy
Knowledge base solution 3: Estrogene
Case base. Using the keyword soda eight cases
with the following seven solutions are retrieved
(case solution 4 occurs twice).
Case solution 1: Aspirin Upsa
Case solution 2: Cooking Soda
Case solution 3: Soluble juice
Case solution 4: Alka Seltzer
Case solution 5: “Invite”
Case solution 6: Vitamin “Teddy”
Case solution 7: Lime Pills”
Thus we get a list of drugs and beverages that
contain sodium Hydrocarbonate, all of them belong
to the generalised solution “soluble”.
Solution. The boy admits to take Levothyroxine
together with an instantiation of the generalised
solution “soluble”, namely soluble vitamin.
Recommendation. The boy is told to take
vitamin four hours later than Levothyroxine.
Additionally, further interactions between vitamin
and Levothyroxine must be checked, because it
might be necessary to adjust the Levothyroxine
dose.
4.1.2 Improving the Efficacy by Dose
Updates
Figure 3 shows an example of a case study. We
compared the decisions of an experienced doctor
with the recommendations of ISOR. The decisions
are based on basic laboratory tests and on lists of
observed symptoms. Intervals between two visits
are approximately six months. In this example
there are three deviations between the doctor’s and
ISOR’s decisions, usually there are less. At the
second visit (v2), according to laboratory results
the Levothyroxine should be increased. ISOR
recommended a too high increase. The applied
adaptation rule was not precise enough. So, we
modified it. At visit 10 (v10) the doctor decided to
try to decrease the dose. The doctor’s reasons were
not included in our knowledge base and since his
attempt was not successful, we did not alter any
adaptation rule. At visit 21 (v21) the doctor
increased the dose because of some minor
symptoms of hypothyroidism, which were not
A CASE-BASED DIALOGUE SYSTEM FOR INVESTIGATING THERAPY INEFFICACY
175

included in ISOR’s list of hypothyroidism
symptoms. Since the doctor’s decision was
probably right (visit 22), we added these symptoms
to the list of hypothyroidism symptoms of ISOR.
0
20
40
60
80
100
120
V1 V2 V3 V4 V5 V6 V7 V8 V9 V10 V11 V12 V13 V14 V15 V17 V18 V19 V20 V21 V22
Levothyroxine µg/day
Doctor
Program
Figure 3: Dose updates recommended by our program
compared with doctor’s decision. V1 means the first visit,
V2 the second visit and so on.
4.2 Inefficacy of Psychiatric Drugs
Originally, ISOR was developed for the endocrine
domain, especially for hypothyroidism, but later on
it has been generalised. Now it can solve the same
types of problems in different medical domains.
Now we present an example from psychiatry.
A man, 55 years of age, has been treated for
depression for 15 years. Symptoms of depression
appeared after he was cruelly beaten near his house.
Since he did not see any connection between his
depression and the violence, he did not tell it to his
doctor. At first, the antidepressant Tofranil for
intake in the morning and the sedative Tisercin for
better sleep at bedtime were prescribed. Later on,
during another depression stage the antidepressant
Fluoxetine helped. Now, his problem is that neither
Fluoxetine, nor any other proposed antidepressant
helps any more.
Retrieval. Keywords are used to retrieve
information from all data sources. Since optional
keywords about a patient’s feeling (e.g. feeling
worse) are used for retrieval of the patient’s medical
history, even biographical events of a patient can be
retrieved.
Individual base. Since the problem of inefficacy
of an antidepressant never arose in the patient’s past,
no solution can be found. However, indirect
information was retrieved. The keyword feeling
better provided a trip to Switzerland, while the result
of the keyword feeling worse provided a trip to
Israel, where the latest very severe depression
began.
Feeling better: A trip to Switzerland
Feeling worse: A trip to Israel
The knowledge base contains information about
depression, anxiety and other psychiatric diseases,
possible complications and references to their
theoretical grounds ((Davidson, 1991), (Flor-Henry,
P., 1983), (Gelder, Lopez-Ibor, and Andeasen,
2000), (Leonhard, 1979), (Tucker and Liotti,
1989)). References to similar problems are retrieved,
the most remarkable one is a link to the algorithm
for psychopharmacology of depression
(htp://mhc.com/Algorithms/Depression, (Osser and
Patterson, 1998). Though the idea of the algorithm is
to solve the problem of non-response to an
antidepressant, it does not really fit here, because it
does not cover the situation that a therapy helped for
some time and then stopped having an effect.
Case base. Eleven cases with similar depression
problems are retrieved. Three of them are
characterised by the general idea depression is
secondary to anxiety resulting from a psychical
trauma.
Case solution 1: Severe stress during the World War 2
Case solution 2: Bad experience in a Jail
Case solution 3: Sexual assault in childhood
The other cases have solutions that are
generalised to changes in therapy.
Adaptation. ISOR displays retrieved
information pieces. In this case, two strategies are
offered. The first one suggests trying some other
therapy. This strategy is supported by the majority
of the retrieved cases and partly by theoretical
recommendations. The second strategy means to
check the diagnosis. This strategy is supported by
three retrieved cases and by the patient’s medical
history. The choice between both strategies is up to
the user. In this example the doctor chooses to
attempt the second strategy at first. The doctor is
especially led by the patient’s medical history,
because Switzerland is usually associated with a safe
life (especially in comparison to life in Russia),
while living in Israel is considered as unsafe.
Furthermore, this strategy is supported by the
general situation that some sedative drugs (e.g.
Tisercin at the beginning) had helped for some time.
ISOR offers a list of questions for the favoured
strategy and as a result the doctor concludes that in
this case depression is in fact only second to anxiety.
The man is permanently afraid of possible violence
and anxiety is based on strong fear that occurred
long ago.
Explaining remarks. Diagnosing anxiety needs
good medical skills, because patients try to suppress
traumatic events from their memory (Stein, 2003).
In this example depression even served as a
mechanism of suppression. The accepted case-based
ICSOFT 2007 - International Conference on Software and Data Technologies
176

solution spared the patient unnecessary experiments
with other psychopharmacological drugs.
So, the first problem is solved, a new diagnosis
is ascertained.
The next problem is prescription of a therapy.
According to the domain theory and to our
knowledge base anxiety implies Neuroleptics
(Gelder, Lopez-Ibor, and Andeasen, 2000.),
(Kalinowsky, and Hippius, 1969). Many of them are
available but a good choice is not trivial.
Individual base. From the patient’s history
those sedatives (Neuroleptics) are retrieved that he
took in his lifetime and that had positive effects on
his psychical condition: Tisercin and Paxil, which is
a drug that has both sedative and antidepressive
effects.
Prototype. Among those prototypes that have
been defined by doctors (based on their long
experience with cases) the prototypical solution
Paxil is retrieved.
Adaptation. Before described, every drug must
be checked for conflicts with the patient’s additional
diseases and already existing therapy. Though the
query patient has already taken Paxil in the past, our
system checks all possible conflicts. If necessary,
adaptation has to be performed. In this case no
conflicts are discovered and Paxil is prescribed.
5 CONCLUSION
We have presented a CBR system that helps doctors
to solve medical problems, particularly to
investigate causes of inefficacy of therapies. It
includes different knowledge containers, namely a
case base, a knowledge base, prototypes, and
individual bases of patients that reflect their medical
histories. Information retrieved from these
containers is arranged in form of dialogues.
The case base plays a central role in the dialogue
forming process. It serves as a kind of filter when
the knowledge base suggests too many possible
solutions for the problem (as in the first example). In
this situation the most typical cases are retrieved
from the case base. When a solution from the
knowledge base is not convincing or when it is
hardly adaptable, the case base may provide better
alternatives (as in the third example).
Generalisations, keywords and references to
other knowledge components belong to the case
base. The adaptation program uses them to create
dialogues. In the part that concerns the case base and
the dialogues ISOR can be considered as domain
independent.
The design of the case base and our
implementation allow solving problems from
different medical domains. Specific, domain
dependant features are attributed mostly to the
individual base, because every domain requires a
special design of case histories. The knowledge base
in ISOR is domain-oriented, but all algorithms and
functions are completely domain independent.
ACKNOWLEDGEMENTS
We thank Dr. Monika Mix, Children’s Hospital of
the University Clinic of Rostock, and Prof. Nikolai
Nikolaenko, Sechenov Institute of Evolutionary
Physiology and Biochemistry in St.Petersburg, for
their data and for their help and time during our
consultations.
REFERENCES
Alacorn, R.D., Glover, S., Boyer, W., Balon, R., 2000.
Proposing an algorithm for the pharmacological
treatment of posttraumatic stress disorder. Ann Clin
Psychiatry 12 (4) 239-246
Barbee, J.G., Jamhour, N.J., 2002. Lamotrigine as an
augmentation agent in treatment-resistant depression.
J Clin Psychiatry 63 (8) 737-41
Bichindaritz,I., 1994. A case-based assistant for clinical
psychiatry expertise, Journal of the American Medical
Informatics Association, Symposium Supplement 673-
677
Cuffel, B.J., Azocar, F., Tomlin, M., Greenfield, S.F.,
Busch, A.B., Croghan, T.W., 2003. Remission,
residual symptoms, and nonresponse in the usual
treatment of major depression in managed clinical
practice. J Clin Psychiatry 64 (4) 397-402
Davidson, R.J., 1991. Cerebral asymmetry and affective
disorders: A developmental perspective. In: Cicchetti,
D., Toth, S.L. (eds.): Internalizing and externalizing
expressions of dysfunction. Rochester Symp. on
Developmental Psychopathology 2, Erlbaum,
Hillsdale, 123-133
DeGroot, L.J., 1994. Thyroid Physiology and
Hypothyroidsm. In: Besser, G.M., Turner, M. (eds.):
Clinical endocrinilogy, Wolfe, London, Chapter 15
Expert Consensus Guideline Series Treatment of
Posttraumatic Stress Dosorder, 2000. J Clin
Psychiatry 60 (suppl 16) 1-76
Flor-Henry, P., 1983. Cerebral Basis of Psychopathology.
John Wright, Boston
Gelder, M.G., Lopez-Ibor, U., Andeasen, N.C. (eds.),
2000. New Oxford Textbook of Psychiatry. Oxford
University Press, Oxford
Hampel, R., 2000. Diagnostik und Therapie von
Schilddrüsenfunktionsstörungen. UNI-MED,
Bremen
A CASE-BASED DIALOGUE SYSTEM FOR INVESTIGATING THERAPY INEFFICACY
177

Hirschfeld, R.M., Montgomery, S.A., et al, 2002. Partial
response and nonresponse to antidepressant therapy:
current approaches and treatment options. J Clin
Psychiatry 63 (9) 826-37
Kalinowsky, L., Hippius, H., 1969. Pharmacolological,
convulsive and other somatic treatments in psychiatry.
Grunee&Stratton, New York London
Keitner, G.I, Posternak, M.A., Ryan, C.E., 2003. How
many subjects with major depressive disorder meet
eligibility requirements of an antidepressant efficacy
trial? J Clin Psychiatry 64 (9) 1091-3
Lam, R.W., Wan, D.D., Cohen, N.L., Kennedy, S.H.,
2002. Combining antidepressants for treatment-
resistant depression: a review, J Clin Psychiatry 63 (8)
685-93
Leonhard, K., 1979. The Classification of the Endogenous
Psychoses. John Wiley, New York
Ma, J., Knight, B.A., 2003. Framework for Historical
Case-Based Reasoning. In: Proc ICCBR-2003,
Springer, Berlin, 246-260
Marling, C., Whitehouse, P., 2001. Case-Based Reasoning
in the care of Alzheimer’s disease patients. In: Proc
ICCBR-2001, Springer, Berlin, 702-715
Osser, D.N., Patterson, R.D., 1998. Algorithms for the
pharmacotherapy of depression, parts one and two.
Directions in Psychiatry 18, 303-334
Schmidt, R., Gierl, L., 2001. Case-based Reasoning for
Antibiotics Therapy Advice: An Investigation of
Retrieval Algorithms and Prototypes. Artificial
Intelligence in Medicine 23 (2) 171-186
Stein, M.B., 2003. Attending to anxiety disorders in
primary care. J Clin Psychiatry 64 (suppl 15) 35-39
Tucker, D.M., Liotti, M., 1989. Neuropsychological
mechanisms of anxiety and depression. In: Boller, F.,
Grafman, J. (eds.): Handbook of Neuropsychology,
vol. 3. Elsevier, Amsterdam, 443-456
Tversky, A., 1977. Features of similarity. Psychological
review 84, 327-352
Vorobieva, O., Gierl, L., Schmidt, R., 2002. Case-based
Adaptation in Medicine - Focusing on
Hypothyroidism. In: Proc UK-Workshop on CBR,
University of Paisley Press, Paisley, 61-68
ICSOFT 2007 - International Conference on Software and Data Technologies
178
