
A COMMUNITY-CENTERED ARCHITECTURE FOR THE
DEPLOYMENT OF UBIQUITOUS TELEMEDICINE SYSTEMS
Federico Cabitza, Marco P. Locatelli and Carla Simone
Universit`a degli studi di Milano-Bicocca, Via Bicocca degli Arcimboldi 8, 20126 Milano, Italy
Keywords:
Ubiquitous Computing, Home Care, Telemedicine, Hypertension, Awareness.
Abstract:
In this paper, we present an ubiquitous and pervasive computing architecture, CASMAS, aimed at supporting
cooperation among the members of a community and their devices. We also show how CASMAS can be
augmented by the WOAD framework, which was developed independently to model and express coordination
mechanisms in document-mediated communities. We take the distributed hypertension monitoring case as
an exemplifying and sufficiently complex scenario to show the feasibility and advantages of the our seman-
tically informed modular approach. The scenario is then declined in terms of architectural components and
cooperation-oriented mechanisms that are shared between the devices and entities of the designed community
of care.
1 INTRODUCTION
The technological trend toward Ubiquitous/Pervasive
Computing allows for an easy and cheap connectiv-
ity among the various actors involved in the care of
patients with chronic diseases: the patient, her family
doctor and relatives, the caring facilities of the city
where they live, and so on. Being connected however
is not enough. What it is needed is to make those con-
nected people a social network that could provide the
patient with a communication environment where she
can feel safe. This is obviously true for elder people
who can otherwise experience loneliness and fragility
with respect to their disease but it also holds true for
people who are engaged in full time activities involv-
ing work, family care, leisure and so on. What is dif-
ferent is the kind of social network that is needed in
the various situations to deal with the normal moni-
toring of the disease development and to face unex-
pected conditions when ad hoc treatments which can
involve several actors at the same time are needed.
On the other hand, even if the physical conditions
are the same, patients and their relatives are not alike
when confronting those events: individual and fam-
ily history can generate different psychological states
that require a strongly personalized communication to
avoid that these factors have a negative impact on the
caring process. The communication dimension is a
necessary factor for this to happen but it is not suffi-
cient: for a patient to feel safe, for a family to feel con-
fident and for a doctor to feel able to achieve the best
possible results, they all need to be part of a caring
process where they cooperate to achieve a common
goal. The technology has to be challenged against this
richer view, in that technological solutions should not
only be conceived from an engineering point of view
to make connectivity robust, fast, protected since it
involves sensible data, and so on, but equally from
the point of view of the disciplines that take coop-
eration through and in interaction with the technol-
ogy as their main concerns. In this respect, Com-
puter Supported Cooperative Work (CSCW), Com-
puter Human Interaction (CHI) and what has been re-
cently called Computer Supported Cooperative Care
(CSCC) (Consolvo et al., ) offer a rich set of indica-
tions that are mostly derived from observations and
studies in the field and from experimental practices
oriented to the evaluation of the impacts of technol-
ogy introduction both in work and every day life situ-
ations. Too often indeed technology adoption is con-
sidered a “secondary” problem to be considered “af-
ter” that the technology has been already put there.
We like to take the opposite attitude: since technol-
ogy can be “easily” put there, we have to anticipate
its impacts on the basis of a stratification of expe-
riences (sometimes of failures) that the above men-
tioned studies offer to the research and development
of new solutions. This paper is a step in this direction.
9
Cabitza F., P. Locatelli M. and Simone C. (2008).
A COMMUNITY-CENTERED ARCHITECTURE FOR THE DEPLOYMENT OF UBIQUITOUS TELEMEDICINE SYSTEMS.
In Proceedings of the First International Conference on Health Informatics, pages 9-16
Copyright
c
SciTePress

1.1 Our Main Contribution
Telemedicine (as any other tele-something involving
cooperation) is not a technological field that aims to
reproduce the current social relations among the in-
volved actors nor to change them in a predefined way
by “optimizing” communication patterns. Both goals
have been proved impossible: technology becomes an
effective support if its developers and users under-
stand that technology is unable, on the one hand, to
reproduce the reality without losing some of its pe-
culiar and tacit aspects; and, on the other hand, to
constrain human behavior to prescriptive rules that
can hold just in a virtual world. In telemedicine (as
in any other application domain), technology has to
harmonize with real life in both directions: i.e., to-
ward both the offering of new possibilities and ca-
pabilities, and the modification of the current ones
without disrupting or disregarding existing individ-
ual and social behaviors. For these reasons, we like
to speak of communities of care, which are consti-
tuted by the patient, close relatives, selected health
assistants and nurses, the family doctor and possi-
bly involved specialists: practitioners are members of
a number of communities, one for each of their pa-
tients. Accordingly, in order to conceive of a support-
ive technology, we claim that design has to be based
on an application layer (i.e., a layer on top of the un-
avoidable one that guarantees physical connectivity)
that reflects the nature and needs of those communi-
ties. To this aim, we propose a framework that in-
corporates the notion of community as a first class
object and it allows to express the community’s co-
operation mechanisms abstractly, i.e., at the seman-
tic level of articulation work. From the technological
point of view, the framework recognizes the need of
allowing for a high degree of flexibility and adaptabil-
ity to the actual domain and current situation since it
separates the cooperation and communications con-
cerns of all the entities involved in a telemedicine
systems by taking a semantically informed modular
approach. These characteristics make our approach
quite different from that recently adopted to make
computation “ambient aware” (Baker et al., 2007).
Indeed, our proposal is not only aimed at making
the members of a community of care aware of what
happens in the enlarged environment. Rather, it is
aimed at making these distributed and heterogeneous
actors aware of the local conventions by which they
can make sense of environmental conditions, consider
them as meaningful parts of a patient-centered logic
environment of care and trust, and correlate those
conditions with timely and effective behaviors when-
ever they occur. Consequently, for our implementa-
tion, we do not adopt third-party middlewares that
are mainly devoted to context awareness, such as the
Context Toolkit (Salber et al., 1999) or the Java Con-
text Awareness Framework (JCAF) (Bardram, 2005);
these can provide “only” the context abstraction and
reasoning part of our model. Conversely, we need,
and achieve, support for both coordination and prop-
agation of awareness information, in addition to the
ability to enhance the behavior of any application
by providing it with a larger access to its context of
use (Dey et al., 2001).
Our approach will be illustrated by means of a
reference scenario that is described in the next sec-
tion. The following sections present the approach
and illustrate it through a subset of functionalities
we focus on for the sake of simplicity. We chose
the domain of hypertension monitoring as the refer-
ence domain where to place our technological pro-
posal since high blood pressure is recognized as one
of the most dangerous silent killer (Hoel and Howard,
1997) and the main concern of physicians involved
in its treatment is that many hypertensive persons are
unaware of the importance of following monitoring
and treatment with commitment in a lifelong perspec-
tive (WHO/ISH, 1999).
2 AN INTEGRATED CARE
SCENARIO
Let us imagine that a patient, Ms Dorothy, has been
inserted in the Hypertension Monitoring Programme
(HMP) by her family doctor, Dr. Robert. HMP pa-
tients suffer for a kind of hypertension that requires
both lifestyle change and medication. For this rea-
son, Ms Dorothy is provided with a series of devices
aimed at making continuous monitoring easier and
seamless with respect to her daily life at home: these
devices are, namely, (1) an electronic agenda; (2) an
automatic drug dispensing machine; (3) an automatic
blood pressure machine; (4) an electronic paper form;
and (5) a simple mobile phone (her own was fine).
All these devices are able to transmit and receive in-
formation from the communicationnetwork, although
in different ways (e.g., via GPRS, cabled ADSL, wi-
fi and GSM) and have been selected to require an as
much as natural interaction with the patient, which
in many cases can lack the necessary skills and prac-
tice to use personal computers, palmtops and complex
smart-phones.
In order to take her blood pressure, Ms Dorothy
uses the Automatic Blood Pressure Machine (ABP).
She can use it on her own since the process is com-
pletely automatic and does not require a specific tech-
nological skill. Today, Ms Dorothy has just taken

her blood pressure and her values are 140/90 mmHg.
Then, she switches on the electronic paper form (EPF)
to send those values to her family doctor, Dr Robert.
The EPF is an A5-sized touch screen using E Ink’s
technology
1
that is thinner than a postcard, has the
clarity of a traditional paper sheet, can be bent with no
distortion and can be inscribed with a regular stylus.
Once switched on, the EPF presents Dorothy with a
regular form, where her latest pressure values, the cur-
rent date and her identity data (e.g., name, social se-
curity number) are copied in the corresponding fields
of the form automatically. As any other HMP patient,
also Ms Dorothy is supposed to fill in additional fields
by hand. The most important is the ‘further remarks’
field: this is where she is asked to annotate the pres-
sure data with some notable past event or condition
that could help the doctor make sense of the pressure
measurement (e.g., “I had a discussion with a neigh-
bor the morning before I took the pressure”). While
the patient is left free to either jot down her remarks
or not when all is well, the system invites her to add a
further justification to collected data whenever it has
detected unexpected pressure values, with respect to
either previous data, current trends or medication reg-
imens.
Since today Ms Dorothy exhibits a blood pressure
that is fairly high for a person under pharmacological
treatment and with her risk factors (i.e., overweight,
smoker), the system also automatically imports from
Dorothy’s personal agenda those items that she had
labeled as ‘work overload’ (i.e., a series of meetings
in the previous two weeks), according to some con-
ventions agreed upon with Dr Robert: specifically,
they agreed upon the need to note into an electronic
agenda Ms Dorothy’s daily engagements and, when-
ever reasonable, to characterize her schedules in terms
of simple categories of events, like ‘passive sport’
(e.g., watching a football match on tv), ‘active sport’
(e.g., working out at the gym), but also ‘business
meeting’, ‘office assignment delivery’ and any event
that could be associated with stressful states, discom-
fort and anxiety. These conventional data allow the
doctor to find specific correlations between high pres-
sure peaks and risky behaviors and to isolate the ac-
tual risk factors of a specific person in order to iden-
tify more discriminating dietary and less generic prac-
tice restrictions and hence a better and patient-focused
treatment. Obviously, these schedule data are strictly
confidential and Ms Dorothy can remove the entries
reported in the EPF. If she leaves them, Dr Robert can
read them only after that Ms Dorothy also gives ex-
plicit consent by signing the form. Since the pressure
values are high and Dorothy was used to be an inten-
1
http://www.eink.com/products/index.html
sive smoker, the system also asks Ms Dorothy to fill
in the form and to report how many cigarettes she has
smoked in the last week (if any), as well as any event
that could justify these values. Also this rule has been
agreed upon by Dr Robert and Ms Dorothy. She re-
ports she did not take any cigarette in that time lapse
and jots down in the remark field that she has often
had evening headaches, fatigue and anxiety. More-
over, since Dr Robert has prescribed her a low-calory
diet, the form displays a field where to fill in the cur-
rent weight also. Indeed, the EPF form can change its
structure according to the doctor’s requests and addi-
tional fields can be presented to patients to be filled
in; in this case, after that Ms Dorothy has annotated
her weight on the EPF, Dr. Robert can also assess
if the dietary regimen is yielding its fruits and give
her some feedback on that. To put it briefly, the EPF
form is a regular document that can hold extra-data
beyond what regularly fed in by digital devices. It is
used to consolidate those health data, in that to sign
it implies giving an explicit consent for their manage-
ment. Besides the reasons of legal accountability, the
form is also used to have patients get an active ap-
proach in monitoring their own blood pressure, since
trend awareness and active inclusion in the monitor-
ing process can give patients the necessary motiva-
tion to change her lifestyle if this is the case. The
EPF form is also used to enable asynchronous com-
munication between patients and their doctor via ei-
ther typed or handwritten messages. Asynchronous
messaging is used in order to reduce the number of
phone calls that could interrupt doctors during their
work. This kind of messaging is particularly appreci-
ated by Ms Dorothy since the EPF represents a writ-
ten source of information to rely on for those doubts
that do not require vis-a-vis or phone talks. Handwrit-
ing with a regular stylus is allowed to enable patients
that do not have - or are not confident with - personal
computers and keyboards to write messages and send
them online. As last thing before signing the form,
Ms Dorothy writes down in the question field whether
she can have some herb tea before going to bed. Then
she puts her signature at the bottom of the form and,
in doing so, the form content is sent to the Dr Robert
officially. Besides being an input device, the EPF is
also a flexible output device. The form can also serve
to reproduce the official headed notepaper where the
doctors jots down drug prescriptions and puts her sig-
nature. In this way, the form can be used to buy drugs
at the pharmacist. Likewise, prescriptions can be up-
dated by the doctor even remotely without any effort
by the patient. The mobile phone is the other main
output device at patients’ home. The mobile phone
is used to convey small messages to remind the pa-

tient, for instance, that she has to take the pills, that
the family doctor has changed the therapy remotely
(and it is available at the EPF) or that he has just sent
her a message.
The doctor, Dr Robert, is informed of the incom-
ing message from her patient while he is going up-
stairs, headed to his office. Indeed, also family doc-
tors are endowed by a couple of smart devices that
are supplied for the HMP to convey alerts when they
are not at their desktop or are engaged in some im-
portant administrative task. These alerts regard the
occurrence of extremely high pressure values of a pa-
tient or, less critically, the notification that a patient
has sent a message via the electronic form. Then Dr
Robert’s mobile phone vibrates and a short message
tells him that Ms Dorothy has written him. He can-
not recall exactly who she is and puts away the mo-
bile as he opens the door of his office. When he sits
at his desk, he switches on a small, flat monitor and
sees a couple of pulsating circles on it. This monitor
is much alike a digital picture frame like the Widget-
Station
2
. This smart frame (SF) runs various “wid-
gets”, i.e., small, user-tuned applications that perform
a variety of tasks, like displaying current agenda, cal-
endar, website and news feeding. One of these wid-
gets is devoted to represent the patients involved in
the HMP programme. Each patient is a small dot
and the color indicates whether she is under drug
therapy or not and whether her last pressure values
are on average or not. If the dot’s border winks,
the corresponding patient has sent the doctor a mes-
sage that has been also forwarded to his email client
and to his mobile if he is out of office. If pressure
values of a patient become critical, the correspond-
ing dot enlarges to become a small quivering cir-
cle whose color indicates the seriousness of the case
(e.g., red, orange, yellow). By touching the circle,
the doctor can have the electronic patient record of
the related patient displayed, as well as a timeline
overview of the pressure data collected so far and
the related medications (in a manner quite similarly
to that used in the Danish TMBP project (Bardram
et al., 2005)). Once seated, Dr Robert touches the
only circle whose border is also winking and the sta-
tion displays the name ‘Ms Dorothy’. He then tips
again on the circle and maximizes in a two-side view
both the last page of Dorothy’s personal record and
her current pressure trend. Since the trend over a two
month period does not show any significant pressure
reduction, Dr Robert decides that the previous ther-
apy is not enough and an additional drug is neces-
sary. He then changes the current drug regimen in the
Ms Dorothy’s file within his electronic patient record.
2
http://www.emtrace.com/widgetstation/
Finally, he opens his mail client and finds the mes-
sage from Ms Dorothy quite immediately amidst the
daily spam since the system has assigned the message
a high priority as it comes from a patient of the HM
programme. Dr Robert answers Ms Dorothy that herb
teas are fine as long as they do not contain theine.
This message will be displayed on the EFP of Ms
Dorothy in a thread-like fashion inside the question
field the next time that she will switch the form on.
In a while, a number of devices at Ms Dorothy’s side
react to the new drug prescription. Ms Dorothy’s mo-
bile rings once and a short message notifies her that a
message and a new prescription have been dispatched
from Dr Robert. The prescription can be displayed at
full screen on the EPF form so that it can be presented
to the pharmacist at due time.
Also the Automatic Drug Dispensing Machine
(ADD) receives the prescription data. According to
these data, the ADD provides the patient with the
right drugs by dispensing just the right dosage and by
allowing the patient to open the drug-till only at the
right interval of time. When the patient withdraws the
drug pill, the ADD records the drug administration as
accomplished. In our vignette, the ADD detects that
the new drug is not loaded in its tills. Consequently,
both Ms Dorothy and her closest relatives are notified
of it by mobile phone. Specific relatives or friends
that were pointed out as the patient’s closest helpers
are also notified whenever the patient has skipped two
drug administrations in a row or if she presents very
high values of hypertension. This is done to commit
the relatives in paying attention to their dears and in
reminding them due commissions at due time.
3 THE CASMAS
ARCHITECTURE
In the architecture that we defined in (Cabitza et al.,
2006), ubiquitous-computing systems are viewed as
constellations of dynamically defined communities of
human and technological entities that interact through
cooperation mechanisms and coordinate themselves
on the basis of awareness information related to the
community context. Communities are identified by
points of aggregation, called community fulcra: en-
tities gather around them to access the information
that characterizes the community and contributes to
its definition. The structure of an entity and how it
relates to the other elements of the model is described
in Figure 1. Each entity — composed of inner ele-
ments as depicted in Figure 1.a — is depicted as a
rounded rectangle, and can be linked to multiple ful-
cra to enable intra- and inter-community coordination

(see Figure 1.b) and to awareness topological spaces
(represented as graphs, space site in Figure 1.a) to
promote awareness information sharing. More specif-
ically, a Coordination agent (C-agent, C in Figure 1.a)
is instantiated for each connection to a fulcrum, i.e.,
for each of the communities in which the entity partic-
ipates; an Awareness agent (A-agent, A in Figure 1.a)
is instantiated for each connection to an awareness
space.
An example of technological entity is the ABP de-
vice; this is typically connected to a fulcrum of an en-
tity that represents a person, Ms Dorothy in this case,
so as to be part of the community of devices that are
associated to that person. The notation used to depict
this situation is showed in Figure 1.c; in this case,
a C-agent is created when an entity connects to an-
other one and it docks to its own entity fulcrum. Fig-
ure 2 represents the set of entities corresponding to
the patient community of care described in Section 2:
in this case the community encompasses both human
and technological entities.
Once created, all C-agents are provided with
generic inference capabilities and with a set of entity-
specific facts (i.e., declarative data structures) and
mechanisms (i.e., rules). By being connected to a
community fulcrum (Figure 1.b), C-agents associated
to entities can share information (facts) and acquire
community-specific behaviors (mechanisms) that are
either defined at design-time or injected into the ful-
crum by other entities at run-time. To this aim, the
model provides mechanisms, for instance to either
insert facts into fulcra (i.e.,
assertion
) or to move
facts from a source’s to a destination’s fulcrum (i.e.,
translation
), by which to define the behavior of C-
agents (Cabitza et al., 2006).
The behaviors of C-agents might be influenced
by the degree of participation of entities in com-
munities, according to additional context information
that is supplied by the part of the model that man-
ages awareness promotion (on the basis of the above
mentioned awareness spaces and A-agents populating
them). This part of the model has been illustrated and
used in a previous work (Locatelli and Simone, 2006)
and will not be further described since the degree of
participation is not used in the considered scenario.
Instead, we give more details on the part of the ar-
chitecture that computes the awareness information
to be promoted, in a simplified way, to entities that
occupy isolated nodes of the awareness spaces (i.e.,
without using the space topology). From now on, we
will use entities without any further reference to their
internal structure since they support the semantically
based modular approach mentioned in the introduc-
tion.
Figure 1: Notation used to represent the entities.
Figure 2: The involved entities in the scenario.
3.1 The Woad Framework
Within the CASMAS architecture, the WOAD frame-
work is what we used to model community con-
ventions and mechanisms of awareness provision.
WOAD is a conceptual and design-oriented frame-
work that we proposed (Cabitza and Simone, 2007b;
Cabitza and Simone, 2007a) to provide a set of high-
level concepts – like those of documental artifact,
fact, fact space, and fact interpreter – that guide
the design of a rule-based reference architecture for
context-aware and coordination-oriented electronic
document systems. In the CASMAS architecture, the
community fulcrum can be seen as a fact space and
one of the agents can plays the role of fact interpreter.
This agent would be supposed to import into its pri-
vate fulcrum (i.e., its working memory) the WOAD
mechanisms of the related community of care and
then apply them to the content of the community ful-
crum so as to produce consistent awareness informa-
tion. In WOAD, two main abstract kinds of compo-
nents are distinguishable: a fact space, i.e., a com-
mon and shared repository where contextual informa-
tion – i.e., what we call facts – is stored; and a fact-
interpreter, i.e., an inference agent that is able to re-
act to the content of the fact space and produce new
contextual information, usually meta-data by which
situational awareness (Endsley, 1995) information is
associated to data. Situational awareness is any infor-
mation about either an event or new contextual condi-
tion which the system can conveyin any way (e.g., vi-
sual, aural, textual) to support the user become aware
of it, know what is going on and figure out what to do
consequently. The WOAD language is a high-level
programming interface by which to express mecha-
nisms of awareness provision and conventional pat-
terns of data production and routing. These mech-
anisms are intended to reflect the local conventions
that practitioners and patients can agree upon about

how to manage data and interventions within a given
community. WOAD mechanisms can be shared into
a fact space and be used by any fact-interpreter shar-
ing this space to (a) provide suitable awareness infor-
mation to support human actors in articulating their
activities of integrated care; and (b) to process the
content of a document according to locally defined
and agreed patterns of coordination. WOAD encom-
passes a set of both static and dynamic constructs by
which the designer can express either contextual, or-
ganizational or procedural knowledge about a work
arrangement in a declarative manner, that is by fo-
cussing on the expression of what a system should do,
rather than worrying about how it really accomplishes
it. These static data structures and dynamic behaviors
are expressed by two specific constructs: facts and
mechanisms, respectively. In the WOAD language,
whatever is given the suffix -fact (e.g., activity-fact,
relation-fact and awareness-fact) is a key-value data
structures, by which the programmer can character-
ize the relevant entities of a documental domain by
simply assigning a value to specific attributes. The
WOAD language provides designers with templates
(i.e., entity-facts) for the most generic categories of
articulation work (cf. (Simone and Divitini, 1997)),
like those of actor, activity and artifact; yet, by means
of its extends primitive, it also allows for the defini-
tion of domain-specific entities (such as patient, doc-
tor and care activity) that inherit from and specialize
those general categories. Mechanisms can be seen
as simple conditional statements, like if-then rules:
they produce some output according to the actions ex-
pressed in their consequent (the then part) whenever
specific contextual conditions, which are expressed in
their antecedent (the if part), are evaluated true by
matching their patterns with the internal state of a fact
interpreter (i.e., usually but not necessarily, the work-
ing memory of the rule-based system). Mechanisms
are hence intended to make explicit the relationship
between some contextual conditions regarding either
the existence or the content of some facts within the
fact space and some behavior (i.e., functionality) that
the system should exhibit in that particular situation,
whenever it occurs. In our application domain, the
production of suitable awareness information is con-
veyed as attached to some contextual or documental
data. In the next section we will see two examples of
information flows derived from the scenario depicted
in Section 2.
4 APPLICATION TO THE HM
SCENARIO
The scenario described in Section 2, identifies
a community, called Patient Care Community
(PCC), that contains the following logical en-
tities interacting through the PCC fulcrum (see
Figure 2): Patient (we denote entities with
this typographical notation), Doctor, and
Relative i.e., entities managing the information
pertaining to each person involved; ADD, Agenda,
ABP, E-paper Form, and Mobile phone are
linked to Patient; Smart Frame, Mobile
phone, EPR, and Email gateway are linked
to Doctor; finally, Mobile phone is linked to
Relative. Moreover, there is a framework-specific
entity, FI-WOAD, that is the WOAD Fact Interpreter;
this entity perceives the facts published by the enti-
ties that take part to the patient care community and
infers on them. The patient care community provides
the involved entities with proper mechanisms to co-
ordinate and exchange information as illustrated in
the scenario. In the following, we give some exam-
ples of mechanisms involving Patient, FI-WOAD,
Doctor and Relative. Patient is in charge of
making available in the PCC’s fulcrum the fact rep-
resenting that the form has been signed (generated by
E-paper form), and the fact that a specific drug
is unavailable (generated by ADD): this transfer of in-
formation is realized by means of the
translation
mechanism, which accomplishes a mere copy of in-
formation from the source’s to the destination’s ful-
crum.
By using the same mechanism, Doctor (asso-
ciated to Dr Robert) can put into the PCC fulcrum
mechanisms expressing criteria to evaluate pressure
values for the patient at hand and identify “critical
values” accordingly. In this way, FI-WOAD can ac-
quire them to assess when pressure values are critical
for the patient at hand and publish both alerting and
reminding facts, in particular those on critical blood-
pressure valuesand, in a similar way, on newprescrip-
tions.
Let us now consider a more articulated situa-
tion. According to the conventions established be-
tween Dr Robert and Ms Dorothy, her Agenda pub-
lishes in the Patient’s fulcrum the events labeled
as “work overload” (see Figure 3.a, step 1a). When
Ms Dorothy takes her blood pressure using the ABP,
ABP publishes this information into the Patient’s
fulcrum (step 1b); E-paper form reacts to this in-
formation (step 2) and shows the form to Ms Dorothy
so that she can fill in the pieces of information re-
quired by the EPF’s structure that is dynamically set
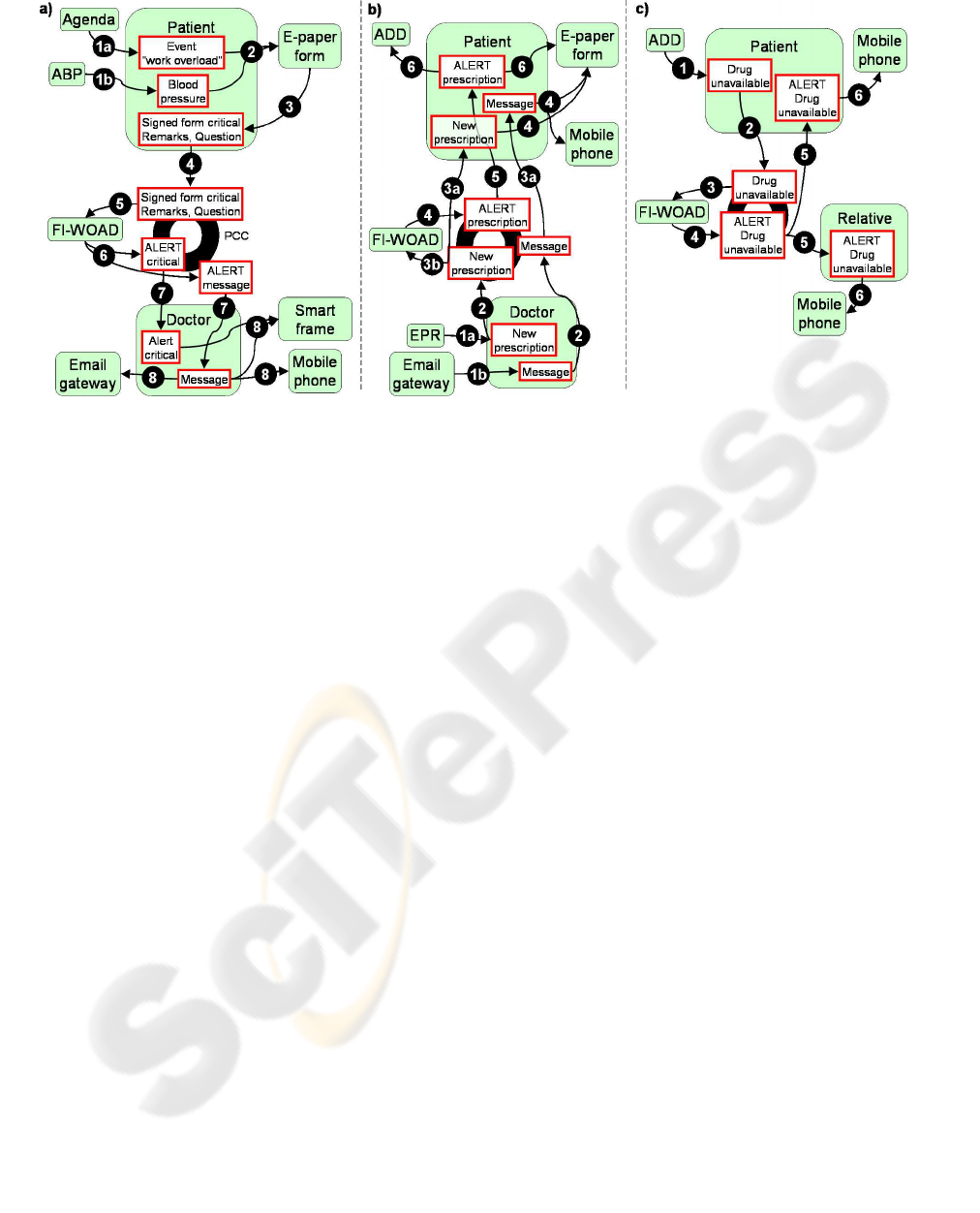
Figure 3: The step sequences for the three main cases depicted in the scenario.
by Dr Robert for her, such as her weight, and write
her remarks and questions. Ms Dorothy signs the
form to submit the information and E-paper form
publishes the form to the Patient’s fulcrum (step
3); then Patient publishes the signed form into
the PCC fulcrum (step 4). Once the signed form is
published into the community fulcrum, all the enti-
ties in charge of managing the form’s content can per-
ceive it; in our case, FI-WOAD perceives the form
(step 5) and, due to its mechanisms, it asserts an alert-
ing fact both for the critical pressure values and for
the message that contains the Ms Dorothy’s question
(step 6). Since Dr Robert must be warned of alerts,
Doctor reacts on these facts and
translates
the
information into its fulcrum (step 7) to make it avail-
able to the entities of its private community. The
alert about critical values is rendered only by the SF
that executes the HM awareness widget; the mes-
sage activates other three entities (step 8): Email
gateway
translates
the message into an email for
Dr Robert, Smart Frame providesawareness about
the received message, and Mobile phone notifies
Dr Robert of the incoming message since he is not in
his office.
Dr Robert evaluates the received information and
writes the new prescription in the EPR; once Dr
Robert is done, EPR asserts the new prescription
into the Doctor’s fulcrum (see Figure 3.b, step
1a); moreover, Dr Robert replies the question of Ms
Dorothy using his email client. This event is caught
by Email gateway that extracts the information
and asserts the corresponding message in Doctor’s
fulcrum (step 1b). Doctor
translates
both the
message and the new prescription into the PCC ful-
crum (step 2) to make them available to the com-
munity. Then Patient
translates
this infor-
mation into its fulcrum (step 3a) and, concurrently,
FI-WOAD reacts on the new prescription (step 3b)
and asserts an alert to the community (step 4). Now
Patient
translates
also the alert into its fulcrum
(step 5). E-paper form reacts to all this informa-
tion because it has to (a) convey Dr Robert’s reply,
(b) show Ms Dorothy the new prescription, and ob-
viously (c) alert her by providing awareness of the
changes occurred (step 4 and 6). Due to the impor-
tance of these changes, Ms Dorothy is also notified
by her mobile phone that a new prescription has been
made available. Also the ADD is programmed to re-
act on changes of prescription (step 6): it checks then
whether the drug is available in its tills or not. Conse-
quently, ADD detects that the new drug is not available
and asserts this information into the Patient’s ful-
crum (see Figure 3.c, step 1). Patient
translates
this information in the community fulcrum (step 2),
FI-WOAD perceives it (step 3) and asserts an alert
(step 4). In this situation, the relative selected by Ms
Dorothy is involved too: Relative perceives the
alert fact (step 5) and
translates
the corresponding
information into its fulcrum so that the relative’s de-
vices (such as her mobile phone) can warn her. The
same happens for Ms Dorothy when she is informed
by her mobile phone (step 5 and 6).
5 CONCLUSIONS
The paper presented the CASMAS architecture. This
architecture is aimed at the development of applica-

tions that take advantage from ubiquitous/pervasive
computing to support cooperation among the mem-
bers of a community. The paper also showed how
CASMAS could be used in the construction of mech-
anisms that are useful to enhance cooperationin a spe-
cific domain, namely within communities of care that
take patients as their “fulcrum”. Two are the main
features of the proposed approach. On the one hand,
the identification of the components is guided by the
idea that they all have access to information (i.e., local
conventions and mutual awareness) that constitutes
the glue of the community but they are also left free
of using the shared information autonomously in or-
der to contribute to the community’s good functioning
and behavior. On the other hand, the mechanisms sup-
porting cooperation are defined in terms of a modular
and declarative approach that defines them in an ab-
stract manner as reactive behaviors with respect to the
changes of the shared information mentioned above.
These two features implement the semantically in-
formed modular approach and support the application
flexibility and adaptability to the context that we men-
tioned in Section 1: indeed, each behavior (from a
whole component up to the atomic constituents of a
single mechanism) is aimed at the goal of support-
ing cooperation and awareness provision between the
members of the community (of care). Hence, these
community-specific behaviors can be naturally exter-
nalized and appropriated by the members, also while
they are interacting with the community designers,
in order to adapt the application to the single con-
text of usage. This context is always locally char-
acterized by the kinds of patients and their diseases,
their family relationships, the local caring structure
and conventional practices and so on. In addition,
the abovementioned separation of concerns applies to
the devices too (seen as a special kind of community
“members”) so as to define a clear interface toward
any underlying layer that guarantees the general pur-
poses of the communicationinfrastructure. The future
work is aimed at making the integration between the
CASMAS architecture and WOAD framework more
transparent and at improving its usability from the de-
signer’s point of view. In doing so, we would provide
an integrated framework that responds to the basic
requirements of cooperation within communities (of
care) and that can be fully validated in the field.
REFERENCES
Baker, C. R. et al. (2007). Wireless sensor networks for
home health care. In AINAW’07 proceedings, pages
832–837, Washington, DC, USA. IEEE Computer So-
ciety.
Bardram, J. E. (2005). The java context awareness frame-
work (jcaf) - a service infrastructure and programming
framework for context-aware applications. In Lecture
Notes in Computer Science, volume 3468, pages 98–
115. Springer.
Bardram, J. E. et al. (2005). Designing for transformations
in collaboration: a study of the deployment of home-
care technology. In GROUP ’05 proceedings, pages
294–303, New York, NY, USA. ACM Press.
Cabitza, F., Locatelli, M. P., and Simone, C. (2006). De-
signing computational places for communities within
organizations. In CollaborateCom’06 proceedings,
Atlanta, Georgia, USA, pages 1–10.
Cabitza, F. and Simone, C. (2007a). A language for the ex-
ecutable specification of coordinative functionalities
for electronic document systems. In CHItaly’07 pro-
ceedings, Padova, Italy, June, 28–30.
Cabitza, F. and Simone, C. (2007b). “. ..and do it the
usual way”: fostering awareness of work conventions
in document-mediated collaboration. In ECSCW’07
proceedings, Limerick, Ireland, 24–28 September.
Consolvo, S. et al. (2004). Technology for care networks of
elders.
Dey, A. K. et al. (2001). A conceptual framework and a
toolkit for supporting the rapid prototyping of context-
aware applications. Human-Computer Interaction,
16(2–4):97–166.
Endsley, M. (1995). Toward a theory of situation awareness
in dynamic systems. Human Factors, 37(1):32–64.
Hoel, D. and Howard, R. (1997). Hypertension—stalking
the silent killer. Postgrad Med Journal, 101(116–121).
Locatelli, M. P. and Simone, C. (2006). Supporting care
networks through an ubiquitous collaborative environ-
ment. In Nugent, C. and Augusto, J., editors, Smart
Homes and Beyond, volume 19, pages 204–211. As-
sistive Technology Research, IOS Press.
Salber, D., et al. (1999). The context toolkit: Aiding the de-
velopment of context-enabled applications. In CHI’99
proceedings, pages 434–441.
Simone, C. and Divitini, M. (1997). Ariadne: Supporting
coordination through a flexible use of the knowledge
on work processes. Journal of Universal Computer
Science, 3(8):865–898.
WHO/ISH (1999). Guidelines for the management of
hyper-tension, volume 1. Blood Press.
