
GESTURE THERAPY
A Low-Cost Vision-Based System for Rehabilitation after Stroke
L. Enrique Sucar
1
, Ron S. Leder
2
, David Reinkensmeyer
3
, Jorge Hernández
4
, Gidardo Azcárate
5
Nallely Casteñeda
6
and Pedro Saucedo
7
1
Departamento de Computación, INAOE, Tonantzintla, Puebla, México
2
División de Ingeniería Eléctrica, UNAM, México D.F., México
3
Department of Mechanical and Aerospace Engineering, UC Irvine, USA
4
Unidad de Rehabilitación, INNN, Mexico D.F., Mexico
5
ITESM Campus Cuernavaca, Morelos, México
6
Unidad de Rehabilitación, INNN, Mexico D. F., Mexico
7
Universidad Anáhuac del Sur, Mexico D.F., Mexico
Keywords: Rehabilitation, stroke, therapeutic technology.
Abstract: An important goal for rehabilitation engineering is to develop technology that allows individuals with stroke
to practice intensive movement training without the expense of an always-present therapist. We have
developed a low-cost, computer vision system that allows individuals with stroke to practice arm movement
exercises at home or at the clinic, with periodic interactions with a therapist. The system intgrates a web-
based system for facilitating repetitive movement training, with state-of-the art computer vision algorithms
that track the hand of a patient and obtain its 3-D coordinates, using two inexpensive cameras and a
conventional personal computer. An initial prototype of the system has been evaluated in a pilot clinical
study with positive results.
1 INTRODUCTION
Each year in the U.S. alone over 600,000 people
survive a stroke (ASA 2004), and similar figures
exist in other countries. Approximately 80% of
acute stroke survivors lose arm and hand movement
skills. Movement impairments after stroke are
typically treated with intensive, hands-on physical
and occupational therapy for several weeks after the
initial injury. Unfortunately, due to economic
pressures on health care providers, stroke patients
are receiving less therapy and going home sooner.
The ensuing home rehabilitation is often self-
directed with little professional or quantitative
feedback. Even as formal therapy declines, a
growing body of evidence suggests that both acute
and chronic stroke survivors can improve movement
ability with intensive, supervised training. Thus, an
important goal for rehabilitation engineering is to
develop technology that allows individuals with
stroke to practice intensive movement training
without the expense of an always-present therapist.
We have developed a prototype of a low-cost,
computer vision system that allows individuals with
stroke to practice arm movement exercises at home
or at the clinic, with periodic interactions with a
therapist. The system makes use of our previous
work on a low-cost, highly accessible, web-based
system for facilitating repetitive movement training,
called “Java Therapy”, which has evolved into T-
WREX (Fig. 1) (Reinkensmeyer 2002 and Sanchez
2006). T-WREX provides simulation activities
relevant to daily life. The initial version of Java
Therapy allowed users to log into a Web site,
perform a customized program of therapeutic
activities using a mouse or a joystick, and receive
107
Enrique Sucar L., S. Leder R., Reinkensmeyer D., Hern
´
andez J., Azc
´
arate G., Caste
˜
neda N. and Saucedo P. (2008).
GESTURE THERAPY - A Low-Cost Vision-Based System for Rehabilitation after Stroke.
In Proceedings of the First International Conference on Health Informatics, pages 107-111
Copyright
c
SciTePress

quantitative feedback of their progress. In
preliminary studies of the system, we found that
stroke subjects responded enthusiastically to the
quantitative feedback provided by the system. The
use of a standard mouse or joystick as the input
device also limited the functional relevance of the
system. We have developed an improved input
device that consists of an instrumented, anti-gravity
orthosis that allows assisted arm movement across a
large workspace. However, this orthosis costs about
$4000 to manufacture, limiting its accessibility.
Using computer vision this system becomes
extremely attractive because it can be implemented
with low cost (i.e. using an inexpensive camera and
conventional computer).
For “Gesture Therapy” we combine T-WREX
with state-of-the art computer vision algorithms that
track the hand of a patient and obtain its 3-D
coordinates, using two inexpensive cameras (web
cams) and a conventional personal computer (Fig.
2). The vision algorithms locate and track the hand
of the patient using color and motion information,
and the views obtained from the two cameras are
combined to estimate the position of the hand in 3-D
space. The coordinates of the hand (X, Y, Z) are sent
to T-WREX so that the patient interacts with a
virtual environment by moving his/her impaired
arm, performing different tasks designed to mimic
real life situations and thus oriented for
rehabilitation. In this way we have a low-cost system
which increases the motivation of stroke subjects to
follow their rehabilitation program, and with which
they can continue their arm exercises at home.
Figure 1: Screen shot of T-WREX. Arm and hand
movements are focused as a mouse pointer to activate an
object in the simulation. In this case a hand interacts with
a basketball. The upper left insert shows the camera views,
frontal and side, of the patient’s hand tracked by the
system.
Figure 2: Set up for the Gesture Therapy system. The
patient is seated in front of a table that serves as a support
for the impaired arm, and its movements are followed by
two cameras. The patient watches in a monitor the
simulated environment and his/her control of the
simulated actuator.
A prototype of this system has been installed at
the rehabilitation unit at the National Institute of
Neurology and Neurosurgery (INNN) in Mexico
City, and a pilot study was conducted with a patient
diagnosed with ischemic stroke, left hemi paresis,
with a time of evolution of 4 years. After 6 sessions
with Gesture Therapy, the results based on the
therapist and patient opinions are positive, although
a more extensive controlled clinical trial is required
to evaluate the impact of the system in stroke
rehabilitation. In this paper we describe the Gesture
Therapy system and present the results of the pilot
clinical study.
2 METHODOLOGY
Gesture Therapy integrates a simulated environment
for rehabilitation (Java Therapy) with a gesture
tracking software in a low-cost system for
rehabilitation after stroke. Next we describe each of
these components.
Figure 3: Reference pattern used for obtaining the intrinsic
parameters of each camera (camera 1 and 2).
HEALTHINF 2008 - International Conference on Health Informatics
108

2.1 Java Therapy/T-WREX
The Java Therapy/T-WREX web-based user
interface has three key elements: therapy activities
that guide movement exercise and measure
movement recovery, progress charts that inform
users of their rehabilitation progress, and a therapist
page that allows rehabilitation programs to be
prescribed and monitored
The therapy activities are presented in the
software simulation like games and the system
configuration allows therapists to customize the
software to enhance the therapeutic benefits for each
patient, by selecting a specific therapy activity
among others in the system
The therapy activities were designed to be
intuitive even for patients with minimal cognitive or
perceptual problems to understand. These activities
are for repetitive daily task-specific practice and
were selected by its functional relevance and
inherent motivation like grocery shopping, car
driving, playing basketball, self feeding, etc.
Additionally, the system gives objective visual
feedback of patient task performance, and patient
progress can be illustrated easily by the therapist by
a simple statistical chart. The visual feedback has the
effect of enhancing motivation and endurance along
the rehabilitation process by patients awareness of
his/her progress.
2.2 Gesture Tracking
Using two cameras (stereo system) and a computer,
the hand of the user is detected and tracked in a
sequence of images to obtain its 3-D coordinates in
each frame, which are sent to the T-WREX
environment. This process involves several stages:
Calibration,
Segmentation,
Tracking,
3-D reconstruction.
Next we describe each stage.
2.2.1 Calibration
To have a precise estimation of the 3-D position in
space of the hand, the camera system has to be
calibrated. The calibration consists in obtaining the
intrinsic (focal length, pixel size) and extrinsic
(position and orientation) parameters of the cameras.
The intrinsic parameters are obtained via a reference
pattern (checker board) that is put in front of each
camera, as shown in figure 3.
The extrinsic parameters are obtained by giving
the system the position and orientation of each
camera in space with respect to a reference point,
see figure 2. The reference point could be the lens of
one of the cameras, or an external point such as a
corner of the table. The colors on the checker board
pattern and the status bar shown in figure 3 above
indicate the progress of the calibration process.
Note that the calibration procedure is done only
once and stored in the system, so in subsequent
sessions this procedure does not need to be repeated,
unless the cameras are moved or changed for other
models.
2.2.2 Segmentation
The hand of the patient is localized and segmented
in the initial image combining color and motion
information. Skin color is a good clue to point
potential regions where there is a hand/face of a
person. We trained a Bayesian classifier with many
(thousand) samples of skin pixels in HSV (hue,
saturation, value), which is used to detect skin pixels
in the image. Additionally, we use motion
information based on image subtraction to detect
moving objects in the images, assuming that the
patient will be moving his impaired arm. Regions
that satisfy both criteria, skin color and motion, are
extracted by an intersection operation, and this
region corresponds to the hand of the person. This
segment is used as the initial position of the hand
for tracking it in the image sequence, as described in
the next section. This procedure is applied to both
images, as illustrated in figure 4.
Figure 4: Hand detection and segmentation in both
images. The approx. hand region is shown as a rectangle,
in which the center point is highlighted, used later for
finding the 3-D coordinates.
The system can be confused with objects that
have a similar color as human skin (i.e wood), so we
assume that this does not occur. For this it is
recommended that the patient uses long sleeves, and
to cover the table and back wall with a uniform cloth
GESTURE THERAPY - A Low-Cost Vision-Based System for Rehabilitation after Stroke
109
in a distinctive color (like black or blue). It is also
recommended that the system is used indoors with
artificial lighting (white). Under these conditions
that system can localize and track the hand quite
robustly in real time.
2.2.3 Tracking
Hand tracking is based on the Camshift algorithm
(Bradski, 1998). This algorithm uses only color
information to track an object in an image sequence.
Based on an initial object window, obtained in the
previous stage, Camshift builds a color histogram of
the object of interest, in this case the hand. Using a
search window (define heuristically according to the
size of the initial hand region) and the histogram,
Camshift obtains a probability of each pixel in the
search region to be part of the object, and the center
of the region is the “mean” of this distribution. The
distribution is updated in each image, so the
algorithm can tolerate small variation in illumination
conditions.
In this way, the 2-D position of the hand in
each image in the video sequence is obtained, which
corresponds to the center point of the color
distribution obtained with Camshift. The 3-D
coordinates are obtained by combining both views,
as described in the next section.
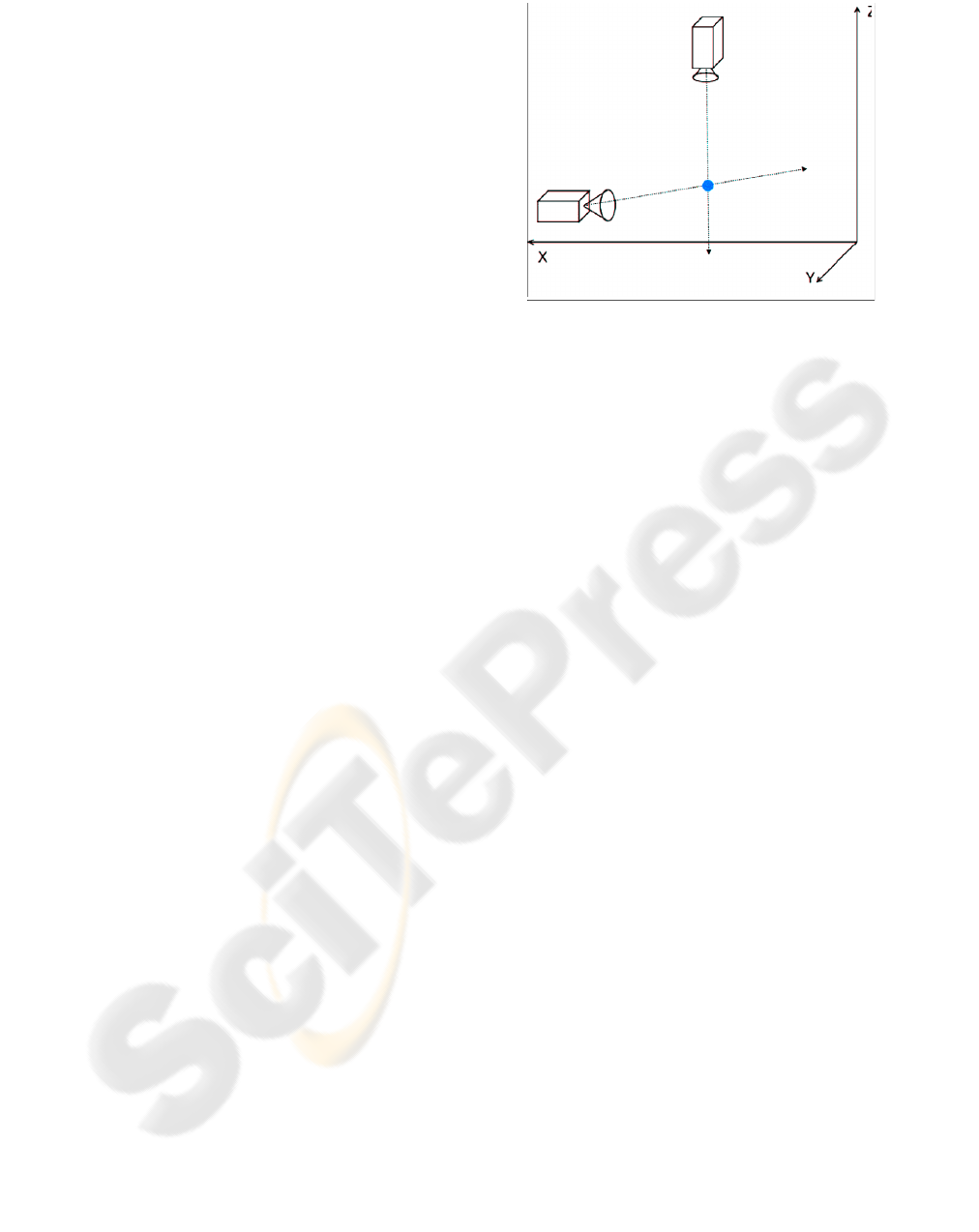
2.2.4 3-D Reconstruction
Based on the 2-D coordinates of the center point of
the image region in each image, the 3-D coordinates
are obtained in the following way. For each image, a
line in 3-D space is constructed by connecting the
center of the hand region and the center of the
camera lens, based on the camera parameters. This is
depicted in figure 5. Once the two projection lines
are obtained, their intersection provides the
coordinates in 3-D (X, Y, Z).
Thus, we have the 3-D position of the hand for
each processed image pair (about 15 frames per
second in a standard PC), which are sent to T-
WREX so that the patient can interact with the
virtual environments.
3 PILOT STUDY
We performed a pilot study with one patient using
"Gesture Therapy" at the National Institute for
Neurology and Neurosurgery (INNN) in Mexico
City. The purpose of this pilot study was to improve
the protocol for a larger clinical trail with Gesture
Therapy, anticipating potential problems and gaining
experience using the technology in the hospital
Figure 5: Estimation of the 3-D position of the hand by
intersecting the projection lines obtained from the images.
setting.
The patient was diagnosed with ischemic stroke,
left hemi paresis, with a time of evolution of 4 years.
An evaluation with the Fugl-Meyer (Fugl-Meyer,
1975) scale was performed at the start and end of the
study.
The patient used Gesture Therapy for 6 sessions,
between 20 and 45 minutes each session. The main
objective of the exercises was the control of the
distal portion of the upper extremity and hand. The
patient performed pre exercises for stretching,
relaxation, and contraction of the fingers and wrist
flexors and extensors. The patient performed several
of the simulated exercises in the virtual
environment, increasing in difficulty as the sessions
progressed (clean stove, clean windows, basketball,
paint room, car race).
After the 6 sessions the patient increased his
capacity to voluntarily extend and flex the wrist
through relaxation of the extensor muscles. He also
tried to do bimanual activities (such as take and
throw a basket ball) even if he maintained the
affected left hand closed; he increased use of the
affected extremity to close doors.
In the therapist’s opinion: "The GT system
favours the movement of the upper extremity by the
patient. It makes the patient maintain the control of
his extremity even if he does not perceive it. GT
maintains the motivation of the patient as he tries to
perform the activity better each time (more control
in positioning the extremity, more speed to do the
task, more precision). This particular patient gained
some degree of range of movement of his wrist.
There are still many problems with the fingers flexor
synergy, but he feels well and motivated with his
achievements. It is also important to note the
motivation effect the system has on patient
endurance to complete the treatment until the last
HEALTHINF 2008 - International Conference on Health Informatics
110

day by increasing the enthusiasm of the patient in
executing the variety of rehabilitation exercises.”
In the patient's opinion: “At the beginning I felt
that my arm was too "heavy", and at the shoulder I
felt as if there was something cutting me, now I feel
it less heavy and the cutting sensation has also been
reduced.”
An “analogical visual scale” in the range 1-10
(very bad, ..., excellent) was applied, asking the
patient about the treatment based on GT, he gave it a
10. Asked about if he will like to continue using GT,
his answer was “YES”.
The Fugl-Meyer scale (3 points increase) was not
sufficiently sensitive to detect the clear clinical and
subjective improvement in the patient.
4 CONCLUSIONS AND FUTURE
WORK
This single case shows the importance of motivation
in rehabilitation. Involving the patient in simulated
daily activities helps the psychological rehabilitation
component as well. The potential ease of use,
motivation promoting characteristics, and objective
quantitative potential are obvious advantages to this
system. The patient can work independently with
reduced therapist interaction. With current
technology the system can be adapted to a portable
low-cost device for the home including
communications for remote interaction with a
therapist and medical team.
It is possible to extend the system to a full arm
tracking, including wrist, hand and fingers for more
accurate movements. Movement trajectories can be
compared and used to add a new metric of patient
progress. To make the system easier to use a GUI
tool is planned for system parameters configuration,
including the camera. Future work includes more
games to increase the variety of therapy solutions
and adaptability to patient abilities, so that a
therapist or patient can match the amount of
challenge necessary to keep the rehabilitation
advancing.
In the current low-cost, vision-based system the
table top serves as an arm support for 2D movement
until the patients are strong enough to lift their arms
into 3D. Extending the system to wrist, hand, and
finger movement is planned to make a full superior
extremity rehabilitation system.
Wrist accelerometers can be used to increase the
objectivity of clinical studies in addition to
subjective reports of patients and caregivers;
especially when the patient spends less time in the
clinic. (Uswatte 2006). fMRI of patients’ brains, pre
and post training, are planned for increasing our
understanding of the biological basis for
rehabilitation (Johansen-Berg 2002).
ACKNOWLEDGEMENTS
This work was supported in part by a grant from
UC-MEXUS/CONACYT.
REFERENCES
American Stroke Association, 2004. Retrieved July 10,
2007 from http://www.strokeassociation.org.
G.R. Bradski, 1998. Computer vision face tracking as a
component of a perceptual user interface. In Workshop
on Applications of Computer Vision, pp. 214-219.
A. R. Fugl-Meyer, L. Jaasko, I. Leyman, S. Olsson, and S.
Steglind, 1975. The post-stroke hemiplegic patient: a
method for evaluation of physical performance. In
Scand J Rehabil Med, vol. 7, pp. 13-31.
D. Reinkensmeyer, C. Pang, J. Nessler, and C. Painter,
2002. Web-based telerehabilitation for the upper-
extremity after stroke. In IEEE Transactions on
Neural Science and Rehabilitation Engineering, vol.
10, pp. 1-7.
R. J. Sanchez, J. Liu, S. Rao, P. Shah, R. Smith, T.
Rahman, S. C. Cramer, J. E. Bobrow, and D.
Reinkensmeyer, 2006. Automating arm movement
training following severe stroke: Functional exercise
with quantitative feedback in a gravity-reduced
environment. In IEEE Trans. Neural. Sci. Rehabil.
Eng., vol. 14(3), pp. 378-389.D. Reinkensmeyer, S.
Housman, Vu Le, T. Rahman and R. Sanchez, 2007.
Arm-Training with T-WREX After Chronic Stroke:
Preliminary Results of a Randomized Controlled Trial.
In ICORR 2007, 10
th
International Conference on
Rehabilitation Robotics, Noordwijk.
D. Reinkensmeyer and S. Housman, 2007. If I can’t do it
once, why do it a hundred times?: Connecting volition
to movement success in a virtual environment
motivates people to exercise the arm after stroke. In
IWVR 2007
G, Uswatte, C. Giuliani, C. Winstein, A. Zeringue, L.
Hobbs, SL Wolf, 2006. Validity of accelerometry for
monitoring real-world arm activity in patients with
subacute stroke: evidence from the extremity
constraint-induced therapy evaluation trial. Arch Med
Rehabil: 86:1340-1345.
H. Johansen-Berg, H. Dawes, C. Guy, S.M. Smith, D.T.
Wade and P.M. Matthews, 2002 Correlation between
motor improvements and altered fMRI activity after
rehabilitative therapy. Brain Journal: 125, 2731-2742
GESTURE THERAPY - A Low-Cost Vision-Based System for Rehabilitation after Stroke
111
