
DO MOBILE PHONES AFFECT SLEEP?
Investigating Effects of Mobile Phone Exposure on Human Sleep EEG
Andrew Wood, Sarah Loughran, Rodney Croft, Con Stough
Australian Centre for Radiofrequency Bioeffects Research, Brain Sciences Institute
Swinburne University of Technology, Melbourne, Australia
Bruce Thompson
Allergy, Immunology and Respiratory Medicine, The Alfred Hospital, Melbourne, Australia
Keywords: Mobile phone radiation, sleep, EEG analysis.
Abstract: This paper will summarize the results of a human volunteer study on the effects on sleep parameters of
exposure to RF emissions from a mobile phone handset for 30min prior to going to sleep. A cohort of 55
volunteers were tested over 4 nights in a double-blind design. The significant outcomes were: Rapid Eye
Movement (REM) sleep latency reduced by 16%; EEG alpha power enhanced by 8% during 1
st
non-REM
period. These results are compared for overall internal consistency and with studies from other laboratories.
Part of the program of the Australian Centre for Radiofrequency Bioeffects Research extending these
studies is described.
1 INTRODUCTION
The issue of whether or not mobile phone handset
radiofrequency (RF) and other emissions are able to
alter sleep patterns is controversial. The World
Health Organisation has a RF research agenda which
highlighted the need to extend and replicate earlier
studies which demonstrated effects on sleep [WHO
http://www.who.int/peh-emf/research/rf03/en/
index2.html]. A series of experiments have been
carried out at Swinburne University in the period
1999 – 2007 involving human volunteers on a range
of immediate psychological and physiological
consequences of use of mobile phone handsets,
including sleep. In terms of health risk assessment,
alterations of sleep quality may not appear to be as
severe as possible links with cancer, but in terms of
society’s expectations, if phone emissions are linked
to any biological changes, these need to be
thoroughly understood. Although the basic research
question we have asked is ‘do the emissions from
mobile phone handsets lead to an immediate change
in ability to get a good night’s sleep?’, we have
specific hypotheses formulated on the basis of
previous research. A review of literature conducted
at the start of the period (Hamblin and Wood, 2002)
identified EEG alpha band power increase (both in
awake and sleep experiments) as being the most
consistent observation. The present experiment was
designed to specifically examine the ‘increased
alpha power’ hypothesis.
2 MATERIALS AND METHODS
2.1 Exposure
A popular handset (Nokia 6110) has been used
throughout the series of experiments. The
manufacturer’s software is used to set into GSM
pulsed ‘test’ mode (0.25 W average) via a serial
cable which is then disconnected once the setting is
complete. Since the current drawn from the battery
follows the GSM pulsing scheme (217 Hz, 1/8 duty
cycle), there is a strong extremely low-frequency
magnetic field associated with this, in addition to the
RF at 914 MHz. The other house-keeping pulses
(including the blank 26
th
frame) were absent. Since
all exposures were carried out with neither the
participants nor those involved in administering
cognitive tests aware or the exposure status, it is
necessary to have independent verification that the
phone was in the correct mode at each testing
session. The RF output was checked i) by holding
565
Wood A., Loughran S., Croft R., Stough C. and Thompson B. (2008).
DO MOBILE PHONES AFFECT SLEEP? - Investigating Effects of Mobile Phone Exposure on Human Sleep EEG.
In Proceedings of the First International Conference on Bio-inspired Systems and Signal Processing, pages 565-569
DOI: 10.5220/0001061505650569
Copyright
c
SciTePress

the handset near to a landline phone and checking
for a ‘buzz’ ii) direct connection of the antenna
feedpoint to a RF power meter iii) by measurements
in SAR phantom. The first of these was performed
on each occasion, the second at six-monthly
intervals to check the constancy of RF output over a
3-hour period and the third was performed once to
determine the appropriate Specific Absorption Rate
(SAR) in the users’ heads.
The peak SAR was 0.19 ± 0.03 W/kg (based on 1g
average). At the relevant moment during the testing
the phone was attached to a cradle in a normal
position next to cheek, with the antenna
approximately 2 cm from the skin. The phone was
set in one of two modes: i) turned on and
transmitting (active); ii) turned off (sham). In other
experiments in our series we also used handsets in
‘standby’ mode (turned on, but not emitting RF,
except in intermittent bursts every few minutes or
so). In order to ensure blinding, the phone was
checked for audible cues from the phone circuitry,
an important requirement in a quiet sleep laboratory.
This was done by asking participants to indicate
whether or not they thought the phone was
transmitting. In order to fully prevent participants
picking up the faint ‘buzz’ even with the
loudspeaker disabled, a plastic foam pad was placed
around the phone in a pouch. This also minimised
the sensation of warmth when the phone was in
active mode.
The phone exposure consisted of the handset
being placed next to the participants’ cheek for 30
min just prior to having monitoring electrodes
attached and getting into bed.
2.2 Subjects
60 subjects were recruited to the study, but five of
these withdrew after provision for their participation
had been made. Five more were excluded because of
confirmed apnoeic event during at least one of their
nights in the study. The final study sample thus
comprised 50 healthy volunteers aged from 18 to 60
years (Mean =27.9 SD = 10.9 years). Subjects were
recruited from advertisements in local and state
newspapers, and posters located at several
universities and organizations in Melbourne. In the
final sample there were 27 males and 23 females, 45
of whom were right handed. No participant reported
any psychological or neurological condition, serious
head injury or extended periods of unconsciousness.
The study took place at a purpose-made sleep
laboratory (Eastern Sleep Disorders Service,
Mitcham Private Hospital, Vic), which consisted of
three individual bedrooms, a central monitoring
room, together with a kitchen and a bathroom..
2.3 Design
A double blind crossover design was used to collect
the data i.e. both the subject and the tester were
blind to the exposure condition. Participants
attended the sleep laboratory on Saturday and
Sunday nights on two consecutive weekends. The
Saturday nights were adaptation nights, to enable
participants to become accustomed to sleeping in a
strange environment and with monitoring sensors
attached. Full sleep monitoring data were obtained
and stored for these nights. On Sunday nights
participants were required to sit for 30 min prior to
getting into bed with the phone in either the
transmitting condition or switched off, with the
opposite condition the following Sunday. During
this time the participants were instructed to look at a
blank wall. At the cessation of real/sham exposure
electrodes and sensors were attached, a task which
normally occupied 15 – 20 min.
2.4 Measures
Sleep was recorded and stages were visually scored
for 30 s epochs according to standard criteria
(Rechtschaffen and Kales, 1968) by an experienced
independent sleep technician who was blind to the
experimental conditions. During sleep, EEG (C3
and C4), ECG, EOG, EMG, SaO2 and nasal airflow
were monitored along with thoracic, abdominal, and
leg movements, using the Compumedics™ E-series
polysomnography system. All EEG electrode
impedances were below 5 kΩ initially. Data were
sampled as shown in Table 1. Data was stored in
records of 1 second in duration in European Data
Format (EDF). This format stores data points as 2
byte binary representation and as such can be
converted into continuous data records for each
channel. This was then exported to Matlab™ in
order to resample the data for subsequent analysis
using Neuroscan data processing software.
BIOSIGNALS 2008 - International Conference on Bio-inspired Systems and Signal Processing
566

Table 1: Sample rates for all recorded channels.
Channel
Number of
samples in each
data record
EEG 250*
EEG(second) 250*
EOG(L) 50
EOG(R) 50
EMG 250
ECG 50
Leg(L) 50
Leg(R) 50
SaO2 5
Airflow 25
Thoracic Respiration 25
Abdominal Respiration 25
Sound 25
CPAP 25
Oxygen 1
Total 1131
*In some records the EEG was sampled at 125 Hz because of
monitoring constraints: the EDF header provided the recording-
specific information.
2.5 Analysis
The sleep staging was carried out in accordance with
routine procedures followed by the Eastern Sleep
Disorders Service. Each 30 s epoch of sleep was
assigned to a stage using the standard R & K
(Rechtschaffen and Kales, 1968) classification. This
analysis also provided timing markers for
subsequent analysis of EEG records. Matlab was
used to extract the first 6 channels of each
participant’s EDF file (EEG1, EEG2, EOGleft,
EOGright, EMG, and ECG). The individual channel
files were then converted to continuous files and
opened using Matlab, where they were re-sampled
(due to the original acquisition rates being different)
so that all channels had the same number of points.
The individual files were then recombined in Matlab
as an EDF file for subsequent spectral analysis using
Neuroscan software. Using the staging data, the first
NREM period (the time from sleep onset, defined as
the first occurrence of stage 2, until the onset of the
first REM sleep period) was extracted and artefact
removal was performed by visual inspection (with
the experimenter blind to the exposure condition).
Only artefact free epochs were used for further
analysis. The first 30 minutes of each file was taken
and the two EEG channels (C3, C4, referenced to
linked mastoids) were extracted and spectral
analysis was performed on the average of the two
channels for each 20 second epoch (FFT routine,
Hanning window, averages of five 4-second
epochs). Data was then exported to SPSS statistical
package Version 11.5 for further statistical analysis.
Spectral data, with a resolution of 0.25 Hz, was thus
obtained for each 20 second epoch for the first 30
minutes from first stage 2 occurrence. The spectrum
for each participant (and for each night) was an
average of the spectra for 3 x 30 = 90 epochs. For
each individual, the averaged spectrum on the active
exposure night is then divided by the spectrum for
the sham night an the ratio converted to a
percentage. These intra-subject ratios are then
averaged over the number of subjects (n = 50) and
the overall percentage (± SEM) calculated. This is
shown in Fig. 1 below, along with the overall
averaged spectra for active and sham exposure
nights.
3 RESULTS
3.1 Sleep Parameters
Of the 10 sleep parameters measured all were non-
significant, except for REM latency, which was
reduced 16% by exposure (p = 0.02) (Loughran et
al., 2005). This was contrary to previous work which
found a suppression of REM sleep (Mann and
Röschke, 1996) and when corrected for multiple
comparisons, the level of significance is marginal.
3.2 Spectral Analysis of EEG
As outlined above, the prior hypothesis was that
EEG alpha power would be increased. Spectral
analysis of the sleep EEG in the first 30 minutes of
the first NREM period revealed no significant
effects of EMF exposure on EEG power density in
the alpha frequency range (8-13Hz) as a whole.
Two alpha sub-bands (11.5-12.25Hz, 13.5-14Hz)
that have previously shown effects in the first
NREM period of an overnight polysomnography
following EMF exposure (Huber et al., 2003) were
also analysed. EEG power density was found to be
significantly enhanced by around 8% in the 11.5 –
12.25 Hz frequency range following EMF exposure,
F(1,48) = 5.56, p = 0.022 (Figure 1). No significant
enhancement was found to be present in the 13.5 –
14 Hz frequency range. Effect sizes (partial eta
squared) were also calculated for the 0-25 Hz region
and are shown in Figure 2. This shows a raised
effect size for the 13.5 – 14 Hz sub-band which
failed to reach significance.
DO MOBILE PHONES AFFECT SLEEP? - Investigating Effects of Mobile Phone Exposure on Human Sleep EEG
567
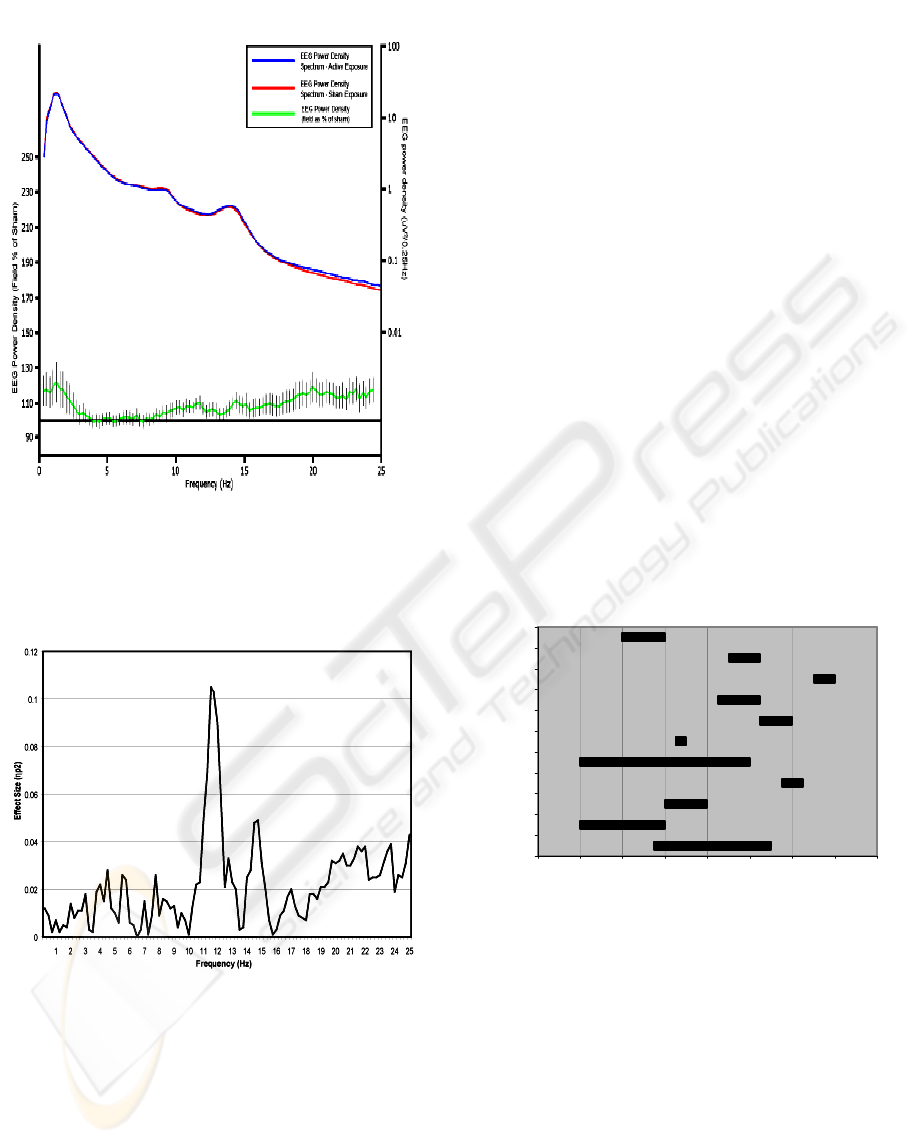
Figure 1: Upper: Averaged EEG spectra for active and
sham exposure nights respectively (for 50 paricipants);
Lower: Mean EEG Power Density Spectrum for real
exposure as a % of sham. Bars represent Standard Error of
Mean.
Figure 2: Effect sizes of EMF exposure on First 30
minutes of the first NREM period. Effect sizes for each
0.25 Hz bin (0 – 25 Hz) are illustrated and were calculated
using the formula
η
p
2
= SS
effect
/(SS
effect
+ SS
error
). (See
Loughran et al. 2005).
It should be noted that in the region 0 – 3 Hz and 17
– 25 Hz there are enhancements of up to 20%, but as
Figure 2 reveals, these are not statistically
significant. Some of these data have previously been
reported (Loughran et al., 2005). The averaged
cross-participant spectra have a 1/f character (note
log scale) with characteristic alpha and theta peaks
shown. The differences in the spectra are only just
distinguishable when plotted conventionally. Note
that below 2 Hz the spectral estimates become
unreliable.
4 DISCUSSION
Since our review paper which discusses papers
published up to 2001 (Hamblin and Wood, 2002),
we have continued to track the literature relating to
reported EEG alpha band enhancements. Up to the
end of 2006, we had noted that of the 18 papers
reviewed, 9 showed data supporting alpha
enhancement, 8 showed no effects, or a reduction
and 1 showed both an enhancement and a reduction,
based on gender. Although all reporting
enhancement refer to the EEG band to be in the
alpha region, further analysis shows that there is
very little overlap between the actual sub-bands over
which the significant changes were reported. In
Figure 3 these bands are illustrated, in reverse
chronological order of publication. Where multiple
bands were shown to be significant in a single study
these are shown as separate rows.
7 8 9 101112131415
[Reiser]
Krause
Borbely
Huber
[Croft]
Huber 02.1
Huber 02.2
Huber 03.1
Huber 03.2
Loughran
Curcio
Hz
Figure 3: Frequency ranges over which increases in EEG
p
ower elicited by mobile phone radiation have bee
n
reported. In some cases, more than one sub-
b
and was
significantly enhanced. The studies are as follows: (Curcio
et al., 2005, Huber et al., 2003*, Huber et al., 2002*, Croft
et al., 2002, Huber et al., 2000*, Borbely et al., 1999*,
Krause et al., 2000, Reiser et al., 1995. Those indicate
d
thus (*) are during a non-REM period of sleep, the others
were with awake subjects (Huber et al. 2002 showed
increases with participants both awake and asleep.
BIOSIGNALS 2008 - International Conference on Bio-inspired Systems and Signal Processing
568

5 FURTHER WORK
A repeat study is now underway in which 20 of the
original cohort of 50 have repeated their
participation. The aim is to discover if those who
showed strong Alpha power changes in the first
study show similar changes in the second. There has
been some speculation that sensitivity to EMF may
vary with the individual.
6 CONCLUSIONS
Alpha power findings are inconsistent across studies,
but sleep studies may show slightly more
consistency. The actual frequency range for
significant increases varies between studies and even
between studies from the same laboratory.
Nevertheless, the preponderance is of reported
increases in alpha power: this may relate to
increased blood flow in superficial regions of the
face or ear or increased tympanic membrane
temperature. It is difficult however to envisage how
these effects could persist several hours after
exposure. Overall, the evidence is insufficiently
strong to conclude that mobile phone emissions
affect sleep.
ACKNOWLEDGEMENTS
Supported by the National Health and Medical
Research Council of Australia, Grant No. 154905.
REFERENCES
Borbely, A. A., Huber, R., Graf, T., Fuchs, B., Gallmann,
E. & Achermann, P. (1999) Pulsed high-frequency
electromagnetic field affects human sleep and sleep
electroencephalogram. Neurosci Lett, 275, 207-10.
Croft, R. J., Chandler, J. S., Burgess, A. P., Barry, R. J.,
Williams, J. D. & Clarke, A. R. (2002) Acute mobile
phone operation affects neural function in humans.
Clin Neurophysiol, 113, 1623-32.
Curcio, G., Ferrara, M., Moroni, F., D'inzeo, G., Bertini,
M. & De Gennaro, L. (2005) Is the brain influenced by
a phone call? An EEG study of resting wakefulness.
Neurosci Res, 53, 265-70.
Hamblin, D. L., Anderson, V., Mcintosh, R. L., Mckenzie,
R. J., Wood, A. W., Iskra, S. & Croft, R. J. (2007)
EEG electrode caps can reduce SAR induced in the
head by GSM900 mobile phones. IEEE Trans Biomed
Eng, 54, 914-20.
Hamblin, D. L. & Wood, A. W. (2002) Effects of mobile
phone emissions on human brain activity and sleep
variables. Int J Radiat Biol, 78, 659-69.
Huber, R., Graf, T., Cote, K. A., Wittmann, L., Gallmann,
E., Matter, D., Schuderer, J., Kuster, N., Borbely, A.
A. & Achermann, P. (2000) Exposure to pulsed high-
frequency electromagnetic field during waking affects
human sleep EEG. Neuroreport, 11, 3321-5.
Huber, R., Schuderer, J., Graf, T., Jutz, K., Borbely, A. A.,
Kuster, N. & Achermann, P. (2003) Radio frequency
electromagnetic field exposure in humans: Estimation
of SAR distribution in the brain, effects on sleep and
heart rate. Bioelectromagnetics, 24, 262-76.
Huber, R., Treyer, V., Borbely, A. A., Schuderer, J.,
Gottselig, J. M., Landolt, H. P., Werth, E., Berthold,
T., Kuster, N., Buck, A. & Achermann, P. (2002)
Electromagnetic fields, such as those from mobile
phones, alter regional cerebral blood flow and sleep
and waking EEG. J Sleep Res, 11, 289-95.
Krause, C. M., Sillanmaki, L., Koivisto, M., Haggqvist,
A., Saarela, C., Revonsuo, A., Laine, M. &
Hamalainen, H. (2000) Effects of electromagnetic
field emitted by cellular phones on the EEG during a
memory task. Neuroreport, 11, 761-4.
Loughran, S. P., Wood, A. W., Barton, J. M., Croft, R. J.,
Thompson, B. & Stough, C. (2005) The effect of
electromagnetic fields emitted by mobile phones on
human sleep. Neuroreport, 16, 1973-6.
Mann, K., Roschke, J. (1996) Effects of pulsed high-
frequency electromagnetic fields on human sleep.
Neuropsychobiology, 33, 41-47
Rechtschaffen, A. & Kales, A. (1968) A manual of
standardised terminology techniques and scoring
system for sleep stages in human subjects,
Washington, DC, US Public Health Service.
Reiser, H., Dimpfel, W. & Schober, F. (1995) The
influence of electromagnetic fields on human brain
activity. Eur J Med Res, 1, 27-32.
DO MOBILE PHONES AFFECT SLEEP? - Investigating Effects of Mobile Phone Exposure on Human Sleep EEG
569
