
USING CASE-BASED REASONING TO EXPLAIN
EXCEPTIONAL CASES
Rainer Schmidt
1
and Olga Vorobieva
1,2
1
Institute for Medical Informatics and Biometry, University of Rostock, Rostock, Germany
2
Sechenov Institute of Evolutionary Physiology and Biochemistry, St.Petersburg, Russia
Keywords: Case-Based Reasoning, Medicine, Exceptional Cases.
Abstract: In medicine many exceptions occur. In medical practice and in knowledge-based systems too, it is necessary
to consider them and to deal with them appropriately. In medical studies and in research, exceptions shall be
explained. We present a system that helps to explain cases that do not fit into a theoretical hypothesis. Our
starting points are situations where neither a well-developed theory nor reliable knowledge nor a case base
is available at the beginning. So, instead of reliable theoretical knowledge and intelligent experience, we
have just some theoretical hypothesis and a set of measurements. In this paper, we propose to combine
Case-Based Reasoning with a statistical model. We use Case-Based Reasoning to explain those cases that
do not fit the model. The case base has to be set up incrementally, it contains the exceptional cases, and their
explanations are the solutions, which can be used to help to explain further exceptional cases.
1 INTRODUCTION
In medical studies and in research, exceptions shall
be explained. We have developed ISOR, a case-
based dialogue system that helps doctors to explain
exceptional cases. ISOR deals with situations where
neither a well-developed theory nor reliable
knowledge nor a proper case base is available. So,
instead of reliable theoretical knowledge and
intelligent experience, we now have just some
theoretical hypothesis and a set of measurements. In
such situations the usual question is, how do
measured data fit to theoretical hypotheses. To
statistically confirm a hypothesis it is necessary that
the majority of cases fit the hypothesis.
Mathematical statistics determines the exact quantity
of necessary confirmation (Kendall and Stuart,
1979). However, usually a few cases do not satisfy
the hypothesis. We examine these cases to find out
why they do not satisfy the hypothesis. ISOR offers
a dialogue to guide the search for possible reasons in
all components of the data system. The exceptional
cases belong to the case base. This approach is
justified by a certain mistrust of statistical models by
doctors, because modelling results are usually
unspecific and “average oriented” (Hai, 2002),
which means a lack of attention to individual
"imperceptible" features of concrete patients.
The usual case-based reasoning (CBR)
assumption is that a case base with complete
solutions is available. Our approach starts in a
situation where such a case base is not available but
has to be set up incrementally. So, we must
1. Construct a model,
2. Point out the exceptions,
3. Find causes why the exceptional cases do not
fit the model, and
4. Develop a case base.
So, we combine case-based reasoning with a model,
in this specific situation with a statistical one. The
idea to combine CBR with other methods is not new.
For example Care-Partner resorts to a multi-modal
reasoning framework for the co-operation of CBR
and rule-based reasoning (RBR) (Bichindaritz et al,
1998). Another way of combining hybrid rule bases
with CBR is discussed by Prentzas and
Hatzilgeroudis (Prentzas and Hatzilgeroudis, 2002).
The combination of CBR and model-based
reasoning is discussed in (Shuguang et al, 2000).
Statistical methods are used within CBR mainly for
retrieval and retention (e.g. Corchado et al, 2003;
Rezvani and Prasad, 2003). Arshadi proposes a
method that combines CBR with statistical methods
like clustering and logistic regression (Arshadi and
Jurisica, 2005).
119
Schmidt R. and Vorobieva O. (2008).
USING CASE-BASED REASONING TO EXPLAIN EXCEPTIONAL CASES.
In Proceedings of the Tenth International Conference on Enterprise Information Systems - AIDSS, pages 119-124
DOI: 10.5220/0001669501190124
Copyright
c
SciTePress

1.1 Dialyse and Fitness
Hemodialysis means stress for a patient’s organism
and has significant adverse effects. Fitness is the
most available and a relative cheap way of support.
It is meant to improve a physiological condition of a
patient and to compensate negative dialysis effects.
One of the intended goals of this research is to
convince the patients of the positive effects of
fitness and to encourage them to make efforts and to
go in for sports actively. This is important because
dialysis patients usually feel sick, they are physically
weak, and they do not want any additional physical
load (Davidson et al, 2005).
At our University clinic in St. Petersburg, a specially
developed complex of physiotherapy exercises
including simulators, walking, swimming etc. was
offered to all dialysis patients but only some of them
actively participated, whereas some others
participated but were not really active. The purpose
of this fitness offer was to improve the physical
conditions of the patients and to increase the quality
of their lives.
2 EXPLANATION MODEL
For each patient a set of physiological parameters is
measured. These parameters contain information
about burned calories, maximal power achieved by
the patient, his oxygen uptake, his oxygen pulse
(volume of oxygen consumption per heart beat),
lung ventilation and others. There are also
biochemical parameters like haemoglobin and other
laboratory measurements. More than 100 parameters
were planned for every patient. But not all of them
were really measured.
Parameters are supposed to be measured four times
during the first year of participating in the fitness
program. There is an initial measurement followed
by a next one after three months, then after six
months and finally after a year. Unfortunately, since
some measurements did not happen, many data are
missing. Therefore the records of the patients often
contain different sets of measured parameters.
It is necessary to note that parameter values of
dialysis patients essentially differ from those of non-
dialysis patients, especially of healthy people,
because dialysis interferes with the natural,
physiological processes in an organism. In fact, for
dialysis patients all physiological processes behave
abnormally. Therefore, the correlation between
parameters differs too.
For statistics, this means difficulties in applying
statistical methods based on correlation and it limits
the usage of a knowledge base developed for normal
people. Non-homogeneity of observed data, many
missing values, many parameters for a relatively
small sample size, all this makes our data set
practically impossible for usual statistical analysis.
Our data set is incomplete therefore we must find
additional or substitutional information in other
available data sources. They are databases – the
already existent Individual Base and the sequentially
created Case Base and the medical expert as a
special source of information.
2.1 Setting up a Model
We start with a medical problem that has to be
solved based on given data. In our example it is:
"Does special fitness improve the physiological
condition of dialysis patients?" More formally, we
have to compare physical conditions of active and
non-active patients. Patients are divided into two
groups, depending on their activity, active patients
and non-active ones.
According to our assumption, active patients should
feel better after some months of fitness, whereas
non-active ones should feel rather worse. We have to
define the meaning of “feeling better” and “feeling
worse” in our context. A medical expert selects
appropriate factors from ISOR’s menu. It contains
the list of field names from the observed database.
The expert selects the following main factors
- F1: O2PT - Oxygen pulse by training
- F2: MUO2T - Maximal Uptake of Oxygen by
training
- F3: WorkJ – performed Work (Joules) during
control training
Subsequently the “research time period” has to be
determined. Initially, this period was planned to be
twelve months, but after a while the patients tend to
give up the fitness program. This means, the longer
the time period, the more data are missing.
Therefore, we had to make a compromise between
time period and sample size. A period of six months
was chosen.
The next question is whether the model shall be
quantitative or qualitative? The observed data are
mostly quantitative measurements. The selected
factors are of quantitative nature too. On the other
side, the goal of our research is to find out whether
physical training improves or worsens the physical
condition of the dialysis patients.
We do not have to compare one patient with another
patient. Instead, we compare every patient with his
own situation some months ago, namely just before
the start of the fitness program. The success shall not
be measured in absolute values, because the health
statuses of patients are very different. Thus, even a
ICEIS 2008 - International Conference on Enterprise Information Systems
120
modest improvement for one patient may be as
important as a great improvement of another.
Therefore, we simply classify the development in
two categories: “better” and “worse”. Since the
usual tendency for dialysis patients is to worsen in
time, we added those few patients where no changes
could be observed to the category” better”.
The three main factors are supposed to describe the
changes of the physical conditions of the patients.
The changes are assessed depending on the number
of improved factors:
- Weak version of the model: at least one factor
has improved
- Medium version of the model: at least two
factors have improved
- Strong version of the model: all three factors
have improved
The final step means to define the type of model.
Popular statistical programs offer a large variety of
statistical models. Some of them deal with
categorical data. The easiest model is a 2x2
frequency table. Our “Better/ Worse” concept fits
this simple model very well. So the 2x2 frequency
table is accepted. The results are presented in Table
1.
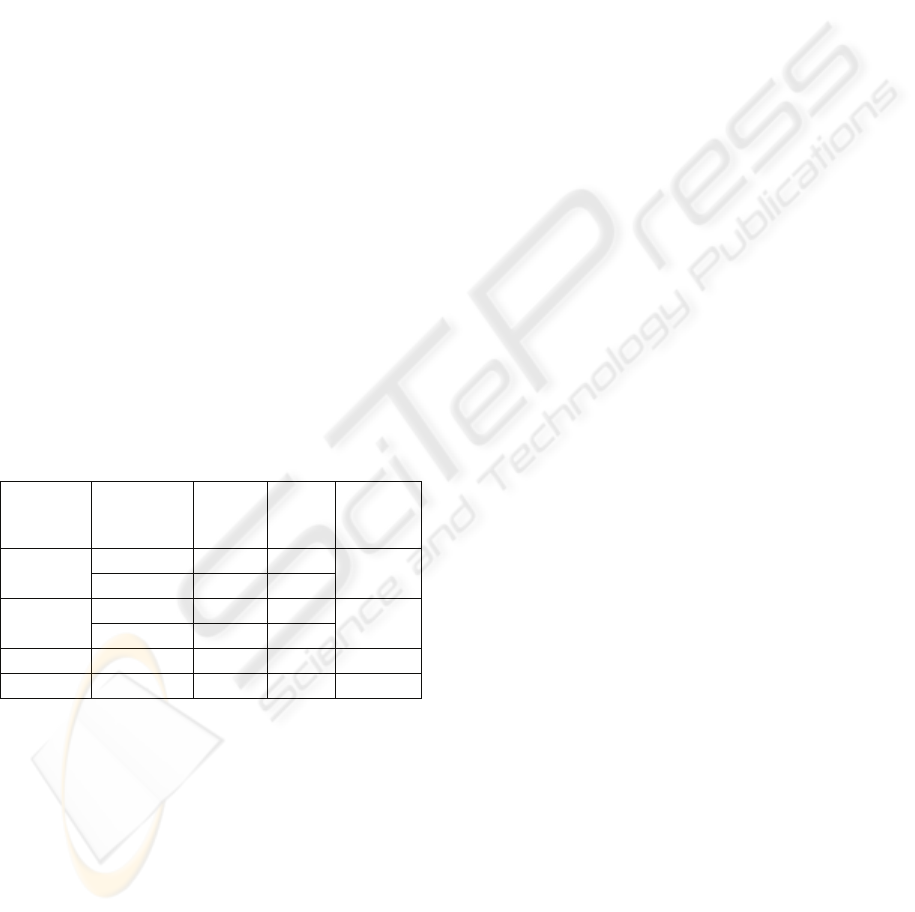
Table 1. Results of Fisher’s Exact Test, performed with an
interactive Web-program:
http://www.matforsk.noIola/fisher.htm. The cases printed
in bold have to be explained.
Improve-
ment
mode
Patient’s
physical
condition
Active
Non-
active
Fisher
Exact p
Better 28 2
Strong
Worse 22 21
< 0.0001
Better 40 10
Medium
Worse
10 12
< 0.005
Weak Better 47 16 < 0.02
Worse
3 6
According to our assumption after six months of
active fitness the conditions of the patients should be
better.
Statistical analysis shows a significant dependence
between the patient’s activity and improvement of
their physical condition. Unfortunately, the most
popular Pearson Chi-square test is not applicable
here because of the small values “2” and “3” in
Table 1. But Fisher’s exact test (Kendall and Stuart,
1979) can be used. In the three versions shown in
Table 1 a very strong significance can be observed.
The smaller the value of p is, the more significant
the dependency.
Exceptions. So, the performed Fisher test confirms
the hypothesis that patients doing active fitness
achieve better physical conditions than non-active
ones. However, there are exceptions, namely active
patients whose health conditions did not improve.
Exceptions should be explained. Explained
exceptions build the case base. According to Table
1, the stronger the model, the more exceptions can
be observed and have to be explained. Every
exception is associated with at least two problems.
The first one is “Why did the patient’s condition get
worse?” Of course, “worse” is meant in terms of the
chosen model. Since there may be some factors that
are not included in the model but have changed
positively, the second problem is “What has
improved in the patient’s condition?” To solve this
problem we look for significant factors where the
values improved.
In the following section we explain the set-up of a
case base on the strongest model version.
2.2 Setting up a Case Base
We intend to solve both problems (mentioned
above) by means of CBR. So we begin to set up the
case base up sequentially. That means, as soon as an
exception is explained, it is incorporated into the
case base and can be used to help explaining further
exceptional cases. We chose a random order for the
exceptional cases. In fact, we took them in
alphabetical order.
The retrieval of already explained cases is performed
by keywords. The main keywords are “problem
code”, “diagnosis”, and “therapy”. In the situation
of explaining exceptions for dialysis patients the
instantiations of these keywords are “adverse effects
of dialysis” (diagnosis), “fitness” (therapy), and two
specific problem codes. Besides the main keywords
additional problem specific ones are used. Here the
additional key is the number of worsened factors.
Further keywords are optional. They are just used
when the case base becomes bigger and retrieval is
not simple any longer.
However, ISOR does not only use the case base as
knowledge source but further sources are involved,
namely the patient’s individual base (his medical
history) and observed data (partly gained by
dialogue with medical experts). Since in the domain
of kidney disease and dialysis the medical
knowledge is very detailed and much investigated
but still incomplete, it is unreasonable to attempt to
create an adequate knowledge base. Therefore, a
medical expert, observed data, and just a few rules
serve as medical knowledge sources.
USING CASE-BASED REASONING TO EXPLAIN EXCEPTIONAL CASES
121

2.2.1 Expert Knowledge and Artificial Cases
Expert’s knowledge can be used in many different
ways. Firstly, we use it to acquire rules, and
secondly, it can be used to select appropriate items
from the list of retrieved solutions, to propose new
solutions and last but not least – to create artificial
cases.
Initially, artificial cases are created by an expert,
afterwards they can be used in the same way as real
cases. They are created in the following situation.
An expert points out a factor F as a possible solution
for a query patient. Since many values are missing, it
can happen that just for the query patient values of
factor F are missing. The doctor’s knowledge in this
case can not be applied, but it is sensible to save it
anyway. Principally there are two different ways to
do this. The first one means to generate a
correspondent rule and to insert it into ISOR’s
algorithms. Unfortunately, this is very complicated,
especially to find an appropriate way for inserting
such a rule. The alternative is to create an artificial
case. Instead of a patient’s name an artificial case
number is generated. The other attributes are either
inherited from the query case or declared as missing.
The retrieval attributes are inherited. This can be
done by a short dialogue (Figure 1) and ISOR’s
algorithms remain intact. Artificial cases can be
treated in the same way as real cases, they can be
revised, deleted, generalised etc.
2.2.2 Solving the Problem “Why Did some
Patients Conditions Became Worse?”
As results we obtain a set of solutions of different
origin and different nature. There are three
categories of solution: additional factor, model
failure, and wrong data.
Additional Factor. The most important and most
frequent solution is the influence of an additional
factor. Only three main factors are obviously not
enough to describe all medical cases. Unfortunately,
for different patients different additional factors are
important. When ISOR has discovered an additional
factor as explanation for an exceptional case, the
factor has to be confirmed by a medical expert
before it can be accepted as a solution. One of these
factors is Parathyroid Hormone (PTH). An increased
PTH level sometimes can explain a worsened
condition of a patient (Davidson et al, 2005). PTH is
a significant factor, but unfortunately it was
measured only for some patients.
Some exceptions can be explained by indirect
indications. One of them is a very long time of
dialysis (more than 60 months) before a patient
began with the training program.
Another solution was a phosphorus blood level. We
used the principle of artificial cases to introduce the
factor phosphorus as a new solution. One patient’s
record contained many missing data. The retrieved
solution meant high PTH, but PTH data in the
current patient’s record was missing too. The expert
proposed an increased phosphorus level as a possible
solution. Since data about phosphorus data was
missing too, an artificial case was created, that
inherited all retrieval attributes of the query case
while the other attributes were recorded as missing.
According to the expert high phosphorus can explain
the solution. Therefore it is accepted as an artificial
solution or a solution of an artificial case.
Model Failure. We regard two types of model
failures. One of them is deliberately neglected data.
Some data had been neglected. As a compromise we
just considered data of six months and further data
of a patient might be important. In fact, three of the
patients did not show an improvement in the
considered six month but in the following six
months. So, they were wrongly classified and should
really belong to the “better” category. The second
type of model failure is based on the fact that the
two-category model was not precise enough. Some
exceptions could be explained by a tiny and not
really significant change in one of the main factors.
Wrong data are usually due to a technical mistake or
to not really proved data. For example, one patient
was reported as actively participating in the fitness
program but really was not.
2.3 Illustration of the Program Flow
Figure 1 shows the main dialogue of ISOR where
the user at first sets up a model (steps one to four),
subsequently gets the result and an analysis of the
model (steps five to eight), and then attempts to find
explanations for the exceptions (steps nine and ten).
Finally the case base is updated (steps eleven and
twelve). On the menu (Figure 1) we have numbered
the steps and explain them in detail.
At first the user has to set up a model. To do this he
has to select a grouping variable. In this example
CODACT was chosen. It stands for “activity code”
and means that active and none active patients are to
be compared. Provided alternatives are the sex and
the beginning of the fitness program (within the first
year of dialysis or later). In another menu the user
can define further alternatives. Furthermore, the user
has to select a model type (alternatives are “strong”,
“medium”, and “weak”), the length of time that
should be considered (3, 6 or 12 months), and main
factors have to be selected. The list contains the
factors from the observed database. In the example
ICEIS 2008 - International Conference on Enterprise Information Systems
122

three factors are chosen: O2PT (oxygen pulse by
training), MUO2T (maximal oxygen uptake by
training), and WorkJ (work in joules during the test
training). In the menu list, the first two factors have
alternatives: “R” instead of “T”, where “R” stands
for state of rest.
When the user has selected these items, the program
calculated the table. “Better” and “worse” are meant
in the sense of the chosen model, in the example of
the strong model. ISOR does not only calculate the
table but additionally extracts the exceptional
patients from the observed database. In the menu,
the list of exceptions shows the code names of the
patients. In the example patient “D5” is selected”
and all further data belong to this patient.
Figure 1: ISOR’s program flow.
The goal is to find an explanation for the exceptional
case “D5”. In point seven of the menu it is shown
that all selected factors worsened (-1), and in point
eight the factor values according to different time
intervals are depicted. All data for twelve months are
missing (-9999).
The next step means creating an explanation for the
selected patient “D5”. From the case base ISOR
retrieves general solutions. The first retrieved one in
this example, the PTH factor, denotes that the
increased Parathyroid hormone blood level may
explain the failure. Further theoretical information
(e.g. normal values) about a selected item can be
received by pressing the button “show comments”.
The PTH value of patient “D5” is missing (-9999).
From menu point ten the expert user can select
further probable solutions. In the example an
increased phosphorus level (P) is suggested.
Unfortunately, phosphorus data are missing too.
However, the idea of an increased phosphorus level
as a possible solution shall not be lost. So, an
artificial case has to be generated.
The final step means inserting new cases into the
case base. There are two sorts of cases, query cases
and artificial cases. Query cases are stored records of
real patients from the observed database. These
records contain a lot of data but they are not
structured. The problem and its solution transform
them into cases and they get a place in the case base.
Artificial cases inherit the key attributes from the
query cases (point seven in the menu). Other data
may be declared as missing. By the update function
the missing data can be inserted later on. In the
example of the menu, the generalised solution “High
P” is inherited, it may be retrieved as a possible
solution (point 9 of the menu) for future cases.
3 EXAMPLE
By an example we demonstrate how ISOR attempts
to find explanations for exceptional cases. Because
of data protection we cannot use a real patient. It is
an artificial case but it is a typical situation.
Query Patient. a 34-year old woman started with
fitness after five months of dialyse. Two factors
worsened Oxygen pulse and Oxygen uptake, and
consequently the condition of the patient was
assessed as worsened too.
Problem. Why the patient’s condition deteriorated
after six months of physical training.
Retrieval. The number of worsened factors is used
as an additional keyword in order to retrieve all
cases with at least two worsened factors.
Case Base. It does not only contain cases but more
importantly a list of general solutions. For each of
the general solutions there exists a list that contains
the concrete solutions based on the cases in the case
base.
The list of general solutions contains five items:
1.) Concentration of Parathyroid Hormone
2.) Period of dialyse is too long.
3.) An additional disease
4.) A patient was not very active during the
fitness program.
5.) A patient is very old.
Individual Base. The patient suffers from a chronic
disease, namely from asthma.
USING CASE-BASED REASONING TO EXPLAIN EXCEPTIONAL CASES
123

Adaptation. Since the patient started with fitness
already after five months of dialyse, the second
general solution can be excluded. The first general
solution might be possible, though the individual
base does not contain any information about PTH.
Further lab tests showed PTH = 870. So, PTH is a
solution.
Since an additional disease, bronchial asthma, is
found in the individual base, this solution is
checked. Asthma is not contained as solution in the
case base, but the expert concludes that asthma can
be considered as a solution. Concerning the
remaining general solutions, the patient is not too
old and she proclaims that she was active at fitness.
Adapted Case. The solution consists of a
combination of two factors, namely a high PTH
concentration and an additional disease, asthma.
4 CONCLUSIONS
In this paper, we have proposed to use CBR in ISOR
to explain cases that do not fit a statistical model.
Here we presented one of the simplest statistical
models. However, it is relatively effective, because
it demonstrates statistically significant dependencies,
in our example between fitness activity and health
improvement of dialysis patients, where the model
covers about two thirds of the patients, whereas the
other third can be explained by applying CBR. Since
we have chosen qualitative assessments (better or
worse), very small changes appear to be the same as
very large ones. We intend to define these concepts
more precisely, especially to introduce more
assessments. The presented method makes use of
different sources of knowledge and information,
including medical experts. It seems to be a very
promising method to deal with a poorly structured
database, with many missing data, and with
situations where cases contain different sets of
attributes.
ACKNOWLEDGEMENTS
We thank Professor Alexander Rumyantsev from the
Pavlov State Medical University for his close co-
operation. Furthermore we thank Professor Aleksey
Smirnov, director of the Institute for Nephrology of
St-Petersburg Medical University and Natalia
Korosteleva, researcher at the same Institute for
collecting and managing the data.
REFERENCES
Arshadi, N., Jurisica, I., 2005. Data Mining for Case-based
Reasoning in high-dimensional biological domains.
IEEE Transactions on Knowledge and Data
Engineering 17 (8). 1127-1137
Bichindaritz, I., Kansu, E., Sullivan, K.M., 1998. Case-
based Reasoning in Care-Partner. In: EWCBR-98,
European Workshop on Case-Based Reasoning.
Springer, Berlin, 334-345
Corchado, J.M., Corchado, E.S., Aiken, J., Fife, C.,
Fernandez, F., Gonzalez, M., 2003. Maximum
likelihood Hebbian learning based retrieval method
for CBR systems. In: ICCBR-2003, International
Conference on Case-Based Reasoning. Springer,
Berlin, 107-121
Davidson, A.M., Cameron, J.S., Grünfeld, J.-P. (eds.),
2005. Oxford Textbook of Nephrology, Volume 3.
Oxford University Press
Hai, G.A., 2002. Logic of diagnostic and decision making
in clinical medicine. Politheknica publishing, St.
Petersburg
Kendall, M.G., Stuart, A., 1979. The advanced theory of
statistics. Macmillan publishing, New York
Prentzas, J., Hatzilgeroudis, I., 2002. Integrating Hybrid
Rule-Based with Case-Based Reasoning. In ECCBR-
2002, European Conference on Case-Based
Reasoning. Springer, Berlin 336-349
Rezvani, S., Prasad, G., 2003. A hybrid system with
multivariate data validation and Case-based
Reasoning for an efficient and realistic product
formulation. In ICCBR-2003, International
Conference on Case-Based Reasoning. Springer,
Berlin (2003) 465-478
Shuguang, L., Qing, J., George, C., 2000: Combining
case-based and model-based reasoning: a formal
specification. In APSEC'00, Asia Pacific Software
Engineering Conference, 416
ICEIS 2008 - International Conference on Enterprise Information Systems
124
