
AN MRP-BASED ARCHITECTURE TO PLAN RESOURCES
AND TO MANAGE WAITING QUEUE IN HOSPITAL SYSTEMS
Raffaele Iannone, Claudia Pepe and Stefano Riemma
Department of Mechanical Engineering, University of Salerno, via Ponte don Melillo 1, 84084, Fisicano (SA), Italy
Keywords: Healthcare System Management, MRP logic, resources planning systems.
Abstract: In the last decades, the interest in the development of healthcare planning and control systems is quickly
spreading. Hospitals quality improvement, in fact, is actually a continuous process mainly aiming at
improving the professional services rendered to patients, not only in terms of effectiveness of cures but also
in terms of efficiency of supplying services system. For a long time, researchers have discussed about how
the benefits in terms of reduction of waiting times and waiting queue, obtained by the IT application in
manufacturing, can be achieved also in hospital systems without forgetting that healthcare supplies the basic
good: health. Resources coordination according to patients who are in hospital, allows the reduction of
“slacks” at resources due to discharge delays, late-start surgeries and slow laboratories turnaround.
Therefore a resources planning system has been implemented in order to reduce the high waiting times and
increase resources utilization in hospitals. The paper describes the methodology to create a dependent
demand starting from patients needs and proposes the implementation of an MRP (Material Requirements
Planning) procedure for hospitals. The PDTs (Diagnostic Terapeutic Path) for each patient in hospital are
generated. All the PDTs are used to calculate resources, materials and facilities requirement in short-mid
term, after having linked resources to the services that hospitals are equipped to provide (BORM – Bill of
Resources and Materials). In this way the MRP procedure is able to plan resources, facilities, materials and
HR in accordance with the real “demand of patients” and highlight potential overloads and problems.
1 INTRODUCTION
The dynamism of hospital systems represents a
penalty for healthcare organization and
management. More and more, in last decades, these
structures have been considered like enterprises and
the complexity of their problems has increased the
necessity to provide hospitals with information
technologies in order to make easier to collect,
archive and manage data. A relevant example is the
introduction of electronic patient case sheet whose
aim is to collect and store clinic data about patients
and their case history (Grimson J., Grimson W.,
Hasselbring, 2000).
Besides data recording and management, one of
the biggest problem hospitals have to face with is the
wide waiting time, due to the increasing of demand,
as well as poor coordination of available resources.
At the moment, for example, in healthcare
organizations it is not possible to know, in advance,
the utilization of resources and their availability.
Often, the time necessary to provide services to
patients is estimated by doctors and physicians only
according to their experience. Moreover, like any
manufacturing firm, hospitals are organized in
departments and wards which are specialized in
supplying particular services. Most of these work
units are formally independent, have their own
resources and work with autonomy. Nevertheless,
some departments and wards are transversal towards
other departments. That means they need to face
with departments to whose they supply services. The
resources of transversal departments are critical so
their management and coordination by monitoring
their utilization can bring benefits in terms of time
and costs.
For this reason, hospitals need a planning and
control system to plan patient admissions and
required capacity in order to optimize services
supplying times and the utilization of resources. This
matter has always been object of scientific
researches directed to hospitals performances
improving. In the past, researchers considered the
possibility to use an MRP system, based on
dependent demand, to solve planning problems in
478
Iannone R., Pepe C. and Riemma S. (2009).
AN MRP-BASED ARCHITECTURE TO PLAN RESOURCES AND TO MANAGE WAITING QUEUE IN HOSPITAL SYSTEMS.
In Proceedings of the International Conference on Health Informatics, pages 478-483
DOI: 10.5220/0001551104780483
Copyright
c
SciTePress
healthcare systems by developing a new system,
named HRP - Hospital Resources Planning - (Roth
and Van Dierdonck, 1995). After them, other
authors presented a hierarchical planning framework
for production planning and control in healthcare
organizations (Vissers, Bertrand, and de Vries,
2001). Their research confirmed that MRP logics
can be applied to services environments besides
industries differently from Shahani who said that
hospitals correspond to complex stochastic systems
so the common deterministic approach for planning
and managing is inadequate (Shahani, 1991).
MRP has been used almost universally in
manufacturing firms and has proven to be a valuable
technique for reducing inventory investment and
improving production planning, getting “the right
materials to the right place at the right time” (Chase,
Aquilano Jacobs, 1998). Then, ERP and MRPII
systems allow production activities planning and
material needs definition by considering resources
availability in order to satisfy the production plan
based on forecasting and orders. It means that
systems, knowing orders and forecasting elaborate
data about stock inventories, lead-times, BOMs of
products, production cycles, resources capacity and
managerial strategies to define the working plan and
the allocation of resources to the jobs, optimizing
times and reducing costs (Chase, Aquilano Jacobs,
1998).
This paper deals with the development of a
prototype for managing and planning hospital
resources. The idea is to implement an ad hoc
system for healthcare organizations based on
ERP/MRPII functionality, born and developed in
manufacturing environments. The system is able to
plan activities, in mid-short time, according to needs
of patients who are in hospitals and those who are
waiting for their entry.
2 THE MODEL
Hospitals are service companies whose aim is to
supply an important good, health, by coordinating
and managing a large quantity of resources. They,
often, are characterized by high waiting times and
costs which can be due to a bad management of
resources. In order to apply to hospitals the logics
used in manufacturing, and try to obtain the same
advantages, it has been necessary to analyze and
schematize the dynamics of services supplying in
healthcare structure.
The design of a planning process for healthcare
organizations firstly requires knowledge about
processes.
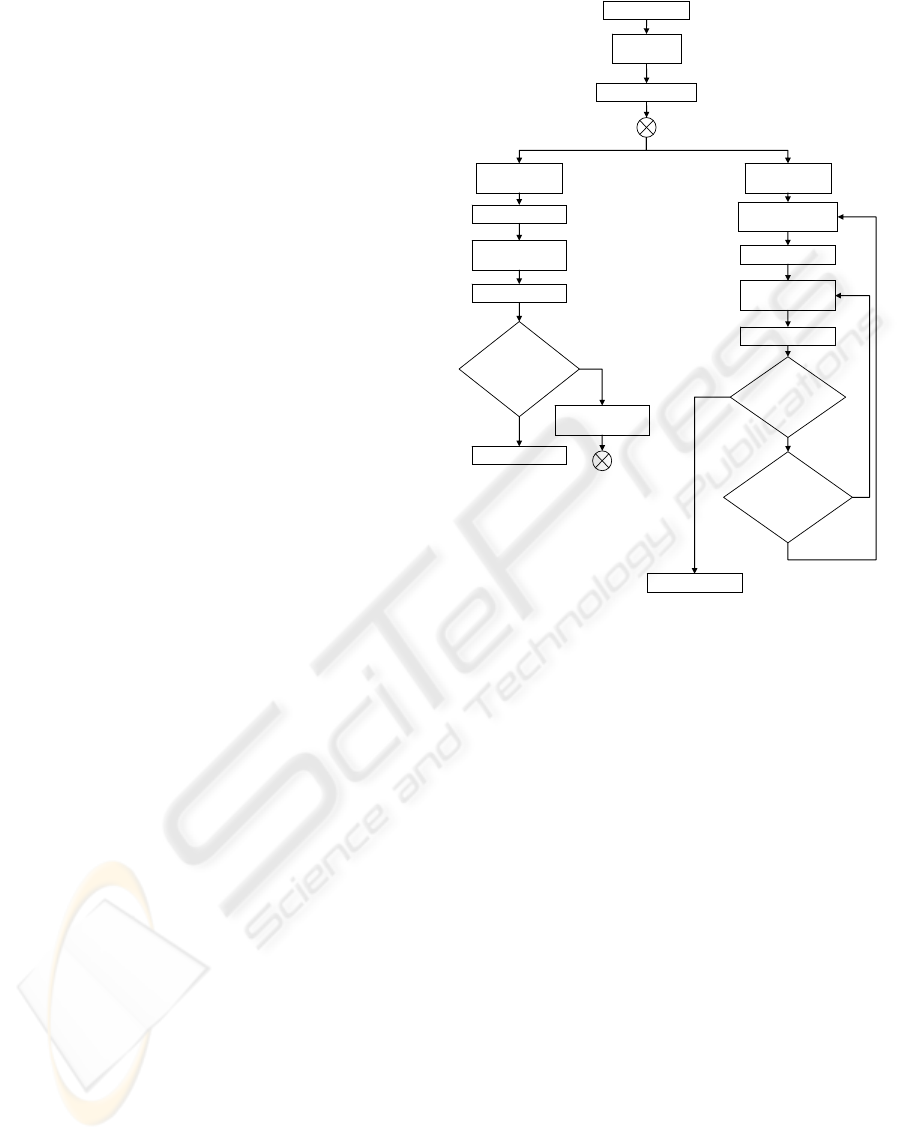
NO
YES
Patient’s arrival
Medical
examination
Diagnosis/Treatment
Planning of new
admission
Medical check
YES
NO
Is it necessary
to modify
diagnosis/
t
reatment?
Discharge of Patient
It is possible
to discharge
the patient?
YES
NO
Does the
patient need
more
assistance?
Planning activities
Patient’s
admission
Patient’s
admission
IP Access
DH/DS Access
A
Execution of
activities
A
Diagnosis/Treatment
Check
Planning activities
Execution of
activities
Medical check
YES
Discharge of Patient
Figure 1: Flowchart of hospital processes.
Figure 1 shows the flowchart of an hospital
patient after being admitted. First of all the patient
receives a medical examination to evaluate his
health and define the treatment he needs. After that,
according to the state of his health, the typology of
access in hospital is defined. During their stay in
hospital patients are often examined by physicians
who decide whether patients have to be discharged,
or the treatment has to be changed or new diagnostic
examinations are required. The patients path ends
with their discharges from hospital. Figure 1 also
points out that patients are the most important actors
inside hospitals and all the decisions are taken
according to their diagnosis and their reactions to
treatments.
During his stay in hospital each patient needs
specific resources, materials and facilities that are
shared with all other admitted patients. Most of time
hospital administration is not able to check the real
availability of resources because the resources
utilization according to the admitted patients’ needs
can not be a priori known.
AN MRP-BASED ARCHITECTURE TO PLAN RESOURCES AND TO MANAGE WAITING QUEUE IN HOSPITAL
SYSTEMS
479
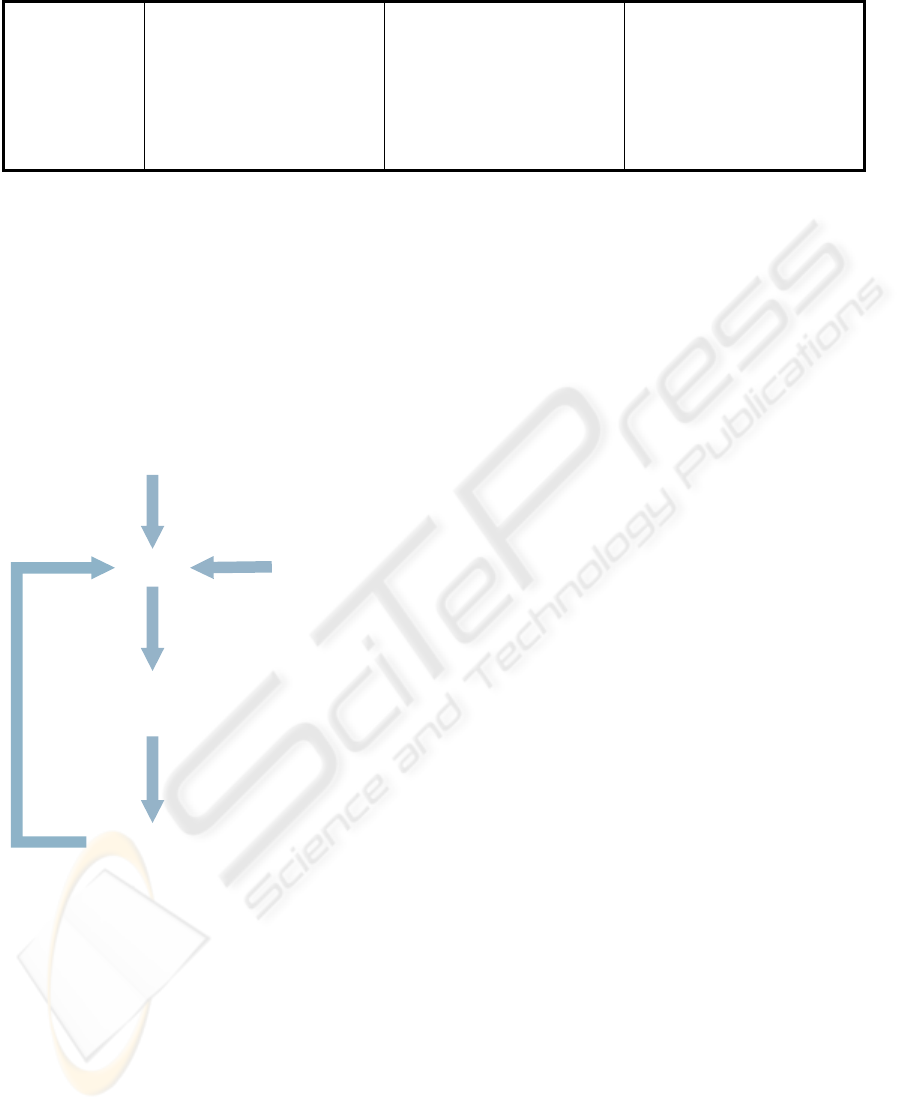
Table 1: General-Paths’ phases of PDT types.
To apply the MRP logic to hospitals we have to
look at the patient as the “customer” of the
healthcare structure and the required services
(diagnostic examination, treatment, specialist
consultation) as the “products” hospitals have to
realize (Iannone, Pepe, Riemma, 2007). In this way
patients can be linked to services and services to
resources.
Patients’ demand
PDT
Bill of
Resource
Planning
(acitivities/resources)
Check
Figure 2: Flowchart about logic of system
The totality of patients needs represents the demand
the hospital has to satisfy in a time as short as
possible, and according to whom it has to organize
available resources. After having defined the
demand and therefore the net requirement to supply,
a link between each patient requirement and the
related materials and resources has to be defined in
order to fulfil a suitable activities and resources
planning,. For this reason, a Diagnostic-Therapeutic
Path (PDT) has been associated to each patient. It
contains all the information about the patient and his
“medical” path inside the hospital where he is
requiring services. By PDT it is possible to know all
the activities that have to be realized in order to
guarantee the service supply. For each activity the
time, materials and resources necessary to complete
the service are specified through the “Bill of
Resources and Materials” (BORM). PDT is dynamic
because physicians can change the treatment process
and when a change occurs resources are re-planned
in real time according to the new necessities (Figure
2).
2.1 Patient’s access and PDTs
First of all, hospitals organize patients’ access:
the Emergency Department for emergencies case;
the Outpatient Department for patients who need
Day-Surgery; the diagnostic centres for diagnostic
Day-Hospital and Inpatient Wards for admitting
patients that require overnight treatments.
In this project two main group of patients’ access
typologies have been considered: OutPatient and
InPatient.
OutPatients are patients who do not need to
occupy bed-resources or who need them maximum
for one night/day. The choice of supplying services
in one day, when it is possible, is more widespread
and often physicians decide to operate on patients in
Day Surgery. Two access typologies are defined for
this type of patient:
• Day Hospital (DH): the patient stays in
hospital just for the time necessary to do
NOT INVASIVE medical examinations,
tests or treatments and then he is able to go
back to home without requiring any bed
(blood transfusion, chemotherapy,
moisturizing, etc.)
• Day Surgery (DS): the patient is admitted
in hospital and requires a bed just for one
day. It is possible to do surgical operation,
INVASIVE diagnostic or therapeutic
activities that need partial or total
anaesthesia (ophthalmological surgery,
gastroenterology, gynaecology, otolaryn-
gologist, orthopaedic, etc.).
IP PDT type DS PDT type DH PDT type
Phase 1
Outpatient Check Outpatient Check Outpatient Check
Phase 2
Diagnostic Tests Diagnostic Tests Diagnostic Tests
Phase 3
Pre-Surgery Evaluation Surgery Follow-up
Phase 4
Surgery Stay in Hospital Discharge
Phase 5
Stay in Hospital Follow-up
Phase 6
Follow-up Discharge
Phase 7
Discharge
HEALTHINF 2009 - International Conference on Health Informatics
480
InPatient, instead, is the typology of patient who
needs to stay in hospital more than one day and
night. In this case the access typology is just one:
• InPatient (IP)
The PDT (Diagnostic-Therapeutic Path) is defined
as “complete route patient follows inside healthcare
structure to solve patient’s health problem”
(Università L. Bocconi . CeRGAS, 2001). That
means it describes the sequence of activities
necessary to supply the suitable aid to the patient
when symptom and diagnosis are known.
PDT is characterized by a General Path that
highlights the main operational tasks linked to the
typology of patient’s access (Table 1) and a Specific
Path which represents all the activities that the
patient has to follow to obtain the service he asks
for.
The General Path of a PDT is associated to the
patient according to his access to the hospital. On
the contrary, the activities of the Specific Path are
defined, time to time, by physicians or qualified
persons.
The described schematization has been used to
facilitate the inserting of patients data on the
electronic planning system. When a patient goes to
hospital he is registered on the data system. In fact,
it is not possible to start the planning procedure if
patients data and requests are not inserted in the
planning software.
Patients data are put in a sheet, called PATIENT
SHEET, that allows the storage of all the necessary
patients data and the unequivocal identification of
the customer inside the system. Moreover, it records
all data about previous stays in hospital of all the
patients.
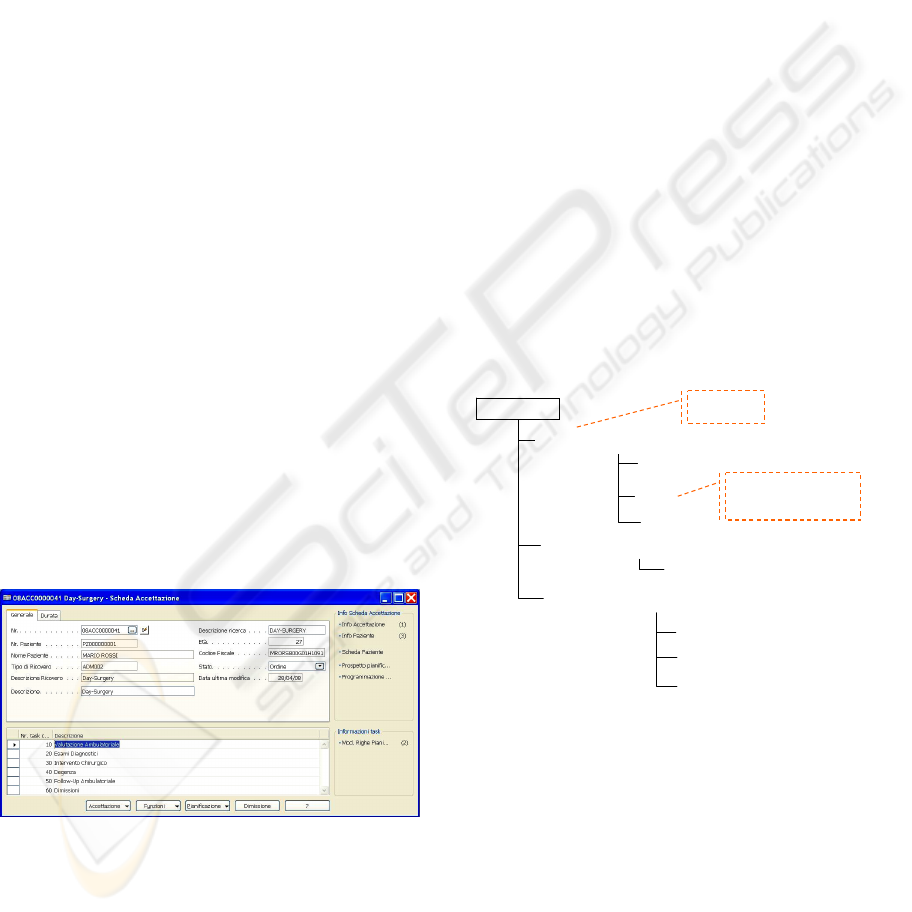
Figure 3: Admission Sheet
If a patient has already been in the healthcare
structure, the related Patient Sheet is not recreated
but it represents the first step for the planning
process: starting from it, in fact, the ADMISSION
SHEET (it is linked to the particular typology of
patient access), which contains all the information
about admission and stay in hospital, is opened.
In the lower part of the sheet, the General Path
phases can be imported according to the specific
patients access typology. Afterwards they can be
modified by specifying the Specific Path activities.
The Admission Sheet is active and can be modified
during the whole period the patient is in hospital;
that means it allows the registration of the whole
path the patient follows from his access to his
discharge..
2.2 PDTs and Resources
PDTs are characterized, as we already said, by two
parts, General Path and Specific Path, that differ
from one another in their levels of detail. The
Specific Path contains the list of the elementary
activities and services (RX to leg, blood test,
electrocardiogram) that the patient needs according
to physicians or qualified persons.
Therefore, these elementary activities are linked
to the “Bill of Resources and Materials” that
specifies the resources, time and materials necessary
to realize a specific activity or service provided by
the hospital.
Blood Test
No. Phase 10 – Blood Sample
No. Phase 20 – Test Tube Transfer
Syringe
Nurse
Assistant
No. Phase 30 – Blood Sample Processing
Phases
Materials and Resources
necessary to realize the service
Test Tube
Machine for Blood Sample Processing
Technician
Biologist
Figure 4: Example of BOR for Blood Test activity.
The explosion of BORM for each activity/service of
a specific path of the phases of a general path of all
patients PDTs allows the availability of necessary
human resources, facilities and materials to be
known.
The physician or the qualified person, through
the ADMISSION SHEET, is able to specify the
required service or the suitable drug-treatment for
each phase of the General Path (the lower part of
window).
AN MRP-BASED ARCHITECTURE TO PLAN RESOURCES AND TO MANAGE WAITING QUEUE IN HOSPITAL
SYSTEMS
481
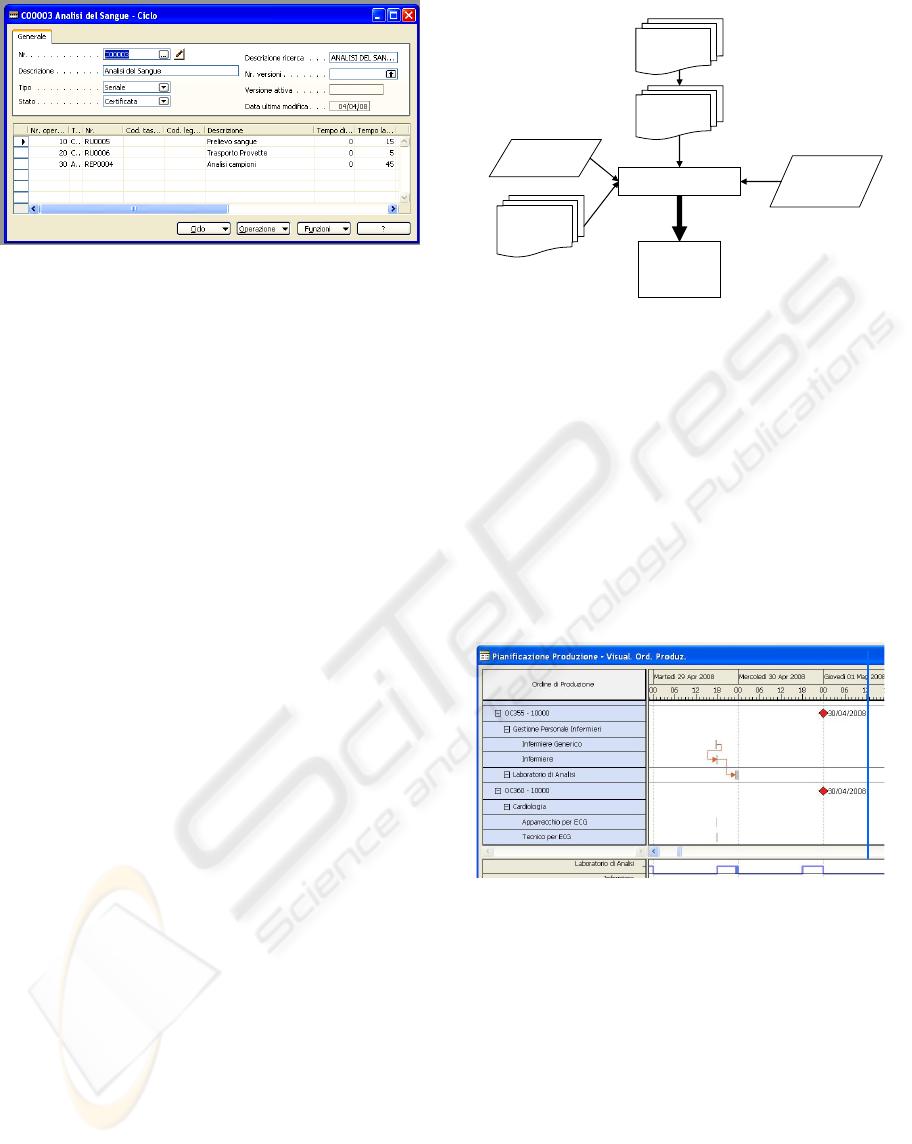
Figure 5: Example of BOR on software system.
Each service, material or drug is registered and
archived on the electronic system using a form,
called “Item Sheet. In detail, when the form is
related to services, it contains information about
BOMs (necessary material for supplying services)
and cycles (necessary time and resources to do
activities); if the form is related to support materials
or drugs the Item Sheet contains information about
stocks of support material and drug. In this way, it is
possible to obtain information about inventory and
generate purchasing orders when it is necessary.
2.3 The Planning Process
Services supplied by healthcare organizations
(surgeries, diagnostic tests, etc.) represent
“products” to realize that, as showed, can be linked
to their relative necessary time, materials and
resources. They are defined in the electronic system
through the ITEM SHEET which contains all the
information necessary for their realization.
Resources, grouped in Human Resources,
Facilities and Materials (Iannone, Pepe, Riemma,
2007), are defined in the electronic system as work
stations that are allocated to departments and
influence their total capacity and availability.
The activities linked to the new PDTs, the
unpdated PDTs, the capacity and availability of
resources are input data for the system. These
collected data are suitably elaborated by the system
that plans activities and resources according to
patients needs.
After having collected information about the
required activities, the system is able to produce a
list of the planned activities through the calculation
of the date at which each activity could be realized
based on the resources availability evaluation
(Figure 6).
The generated list is confirmed by the planner
together with the physician in charge or the depart-
ment chief who has to realize the activities. When
Patient
Sheet
New
Resources
Planning
Eletronic Planner
Admission
Sheet
Old
Resources
Planning
Resources
Capacity
Item Sheet
Figure 6: Information flowchart.
the activity starts, the person who realizes the
activity or supplies service changes its state from
“confirmed” to “released”. An activity is “released”
when the required resources are really occupied.
After having completed an activity, its state is
declared “closed” and the occupied resources are
released becoming “available”.
When the patient is discharged from hospital all
the activities linked to his Admission Sheet become
closed and resources are available again, even if they
(activities) are not completed.
Figure 7: Gantt of resources and activities.
Beside the list of planned resources, another
output created by the system is the Gantt chart of the
planned activities and resources utilization (Figure
7). The physician or the person who should confirm
the planning plan, can change it directly on the chart,
by shifting activities that he thinks are bad planned.
Once a change on the chart occurs, the system is
automatically able to replan all the activities which
can be shifted. Moreover, through the reading of the
Gantt diagram, it is possible to know the workload
of the single resource as well as the specific patient
who uses each resource.
HEALTHINF 2009 - International Conference on Health Informatics
482

3 CONCLUSIONS
The output of the described system is the activities
Gantt chart which represents a calendar of the
activities that have to be realized inside hospitals
according to patients demand.
The proposed logic allows a more suitable
management of the resources capacity and
availability and, consequently, the improvement of
waiting queues management by basing the activities
planning and the resources scheduling on
requirements. In fact, after building a Gantt’s chart
of the monitored resources, their availability
(facilities, personnel, laboratories, etc.) can be
known in real time or even in advance,. When
resources are overloaded and it is not possible to
realize one or more of the planned activities, patients
can be rescheduled in order to meet the available
capacity. At the same way, when an emergency
occurs it is possible to reschedule not-emergency
patients exactly when the resources they need are
available. In this manner, the eventuality that a
patient is admitted in advance and uselessly occupies
resources (beds or food service) in waiting for
services that cannot be supplied in that moment is
avoided. The update of the system, moreover, allows
the real time check of resources overloads or delays
in supplying services for patient who are already in
the hospital.
The described system can be seen as the first
step toward the development of a network able to
manage more hospitals and able to sort out patients
in healthcare structures according to the required
services and the real availability of resources.
REFERENCES
Chase, R. C., Aquilano, N. J., Jacobs, R.F. 1998.
Production and Operation Management.
Manufacturing and Service, Irwin McGraw-Hill
de Vries, G., Vissers, J., de Vries, G., 2000. The use of
patient classification system for production control of
hospitals CASEMIX, Vol. 2, No 2.
Grimson, J., Grimson, W., Hasselbring, W., 2000. The SI
Challenge in Healthcare, Comunication of the ACM,
Vol.43, No.6.
Iannone, R., Pepe, C., RiemmaS., 2007. A proposal of a
management framework to optimize waiting queue in
healthcare organizations, 6
th
Annual HTCM
Conference
Roth, A. V. Van Dierdock, R. 1995. ‘Hospital resource
Planning: Concepts, Feasibility and Framework,
Production and Operation Management, Vol. 4, No. 1,
pp.1-29
Shahani, A.K. 1991 ‘Reasonable Averages that give
Wrong Answers’, Teaching Statistics, Vol. 13, No. 2,
pp.50-54.
Università L. Bocconi. CeRGAS, 2001. La Gestione dei
Procesi Produttivi Sanitari attraverso lo strumento dei
Percorsi-Diagnostici terapeutici, Azienda Ospadaliera
Luigi Sacco.
Vissers, J.M.H. Bertrand, J.W.M. de Vries, G. (2001) ‘A
framework for Production Control in Healthcare
Organization’, Production Planning and Control, Vol.
12, No. 6, pp.591-604
AN MRP-BASED ARCHITECTURE TO PLAN RESOURCES AND TO MANAGE WAITING QUEUE IN HOSPITAL
SYSTEMS
483
