
THE POWER SPECTRA RESPONSE OF STROKE VOLUME AND
ARTERIAL BLOOD PRESSURE VARIABILITY SIGNALS TO
AUTONOMIC NERVOUS SYSTEM MODULATION OF THE HEART
Abdul-Hakeem H. AlOmari
1,3
, Andis Graudins
2,3,4
1
School of Electrical Engineering and Telecommunications;
2
Prince of Wales Clinical School, Faculty of Medicine
3
The University of New South Wales;
4
Clinical and Experimental Toxicology Unit and Department of Emergency Medicine
Prince of Wales Hospital , Sydney, Australia
Andrey V. Savkin
School of Electrical Engineering and Telecommunications, The University of New South Wales, Sydney, Australia
Keywords:
Stroke volume variability (SVV), Systolic blood pressure variability (SBPV), Power spectral analysis, Sym-
pathovagal balance, Levosimendan, Verapamil, Calcium channel sensitizers, Calcium channel blockers.
Abstract:
This study presents results that describe the short term oscillations in SBPV and SVV signals due to calcium
channel blockers poisoning with verapamil treated with continuous infusion of levosimendan. In addition, we
used average spectra of these oscillations to observe the activity and sympathovagal balance of the autonomic
nervous system. Then, we compared the average spectra obtained from both signals. The frequency contents
of the average spectra of SVV and SBPV signals to levosimendan treatment of verapamil-poisoned rats were
analyzed and related to the activity of sympathetic and parasympathetic tones. In control group, average
spectra of SVV and SBPV exhibited a low-frequency band (LF: 0.03− 0.8 Hz) peaked at ∼ 0.4 Hz and a high-
frequency (HF: 0.8 − 3.0 Hz) peaked at ∼ 1 Hz. LF peak was abolished after verapamil infusion. The LF
component of both spectra was observed to recover after continuous infusion of levosimendan. Additionally,
a new frequency component was observed at 1.5 Hz in the spectrum of SBPV. Significant correlations were
found between bands of the average spectra in both signals in all groups of treatment studied in this paper. Our
results revealed that, like SBPV, SVV can herald useful information regarding the sympathovagal balance and
cardiac output improvements.
1 INTRODUCTION
Power spectra analyses of blood pressure and heart
rate variability (HRV) signals have previously been
used as a window to monitor the autonomic ner-
vous activity in the cardiovascular system (see e.g.
(Julien et al., 2003; Cerutti et al., 1994) and the ref-
erences therein). Using power spectral techniques,
systolic blood pressure variability (SBPV) can be de-
constructed into variabilities at different frequencies.
These variabilities can be divided into respiratory and
vasomotor components in a similar way to that seen
with HRV signals. Previously, it has been shown that
vasomotor-related SBPV correlates well with vascu-
lar sympathetic function of α-adrenoceptors (Brown
et al., 1994).
In rats, SBPV exhibits low-frequency(LF), known
as Mayer waves (Julien et al., 2003; Brown et al.,
1994), and high-frequency (HF) oscillations. The LF
oscillations are related to the activity of sympathetic
nervous system and the HF one is related to respira-
tory activity to be mediated by parasympathetic ac-
tivity (Cerutti et al., 1994; Japundzic et al., 1990).
Recently, seeking new methods to provide a clini-
cally useful information about the autonomic nervous
system, power spectrum of stroke volume variability
(SVV) signal has been employed. Previous studies
(Liu et al., 2004; Siebert et al., 2004) have compared
the spectra responses of SVV and HRV in healthy
subjects.
In the present study, we analyzed the spectral
properties of the systolic blood pressure variability
411
H. AlOmari A., Graudins A. and V. Savkin A. (2009).
THE POWER SPECTRA RESPONSE OF STROKE VOLUME AND ARTERIAL BLOOD PRESSURE VARIABILITY SIGNALS TO AUTONOMIC
NERVOUS SYSTEM MODULATION OF THE HEART.
In Proceedings of the International Conference on Bio-inspired Systems and Signal Processing, pages 411-415
DOI: 10.5220/0001775804110415
Copyright
c
SciTePress

(SBPV) signal to assess the effects of levosimendan
on the autonomic nervous activity in verapamil poi-
soning in a rodent model and then compare it with the
results obtained from applying the same procedure to
the estimated stroke volume variability signal. To our
knowledge, there are no studies that have compared
the spectra of SBPV and SVV estimated from contin-
uous blood pressure recordings.
2 Materials and Methods
The methods used in surgery, instrumentation, treat-
ment and data collection for this research has been
described in detail elsewhere (Graudins et al., 2008).
To summarize, experiments were conducted on
healthy, anaesthetized, intubated, and ventilated male
Wistar rats weighing between 300 and 500 grams.
Jugular, femoral venous and carotid catheters were in-
serted. Continuous recordings of ECG, arterial blood
pressure was performedusing a PowerLab data acqui-
sition system and Chart Version 5.0 software (ADIn-
struments, Castle Hill, Australia). After an equilibra-
tion period, all rats were then administered verapamil
hydrochloride(AbbottAustralasia, Botany, Australia)
6µg/kg/h (IsoptinInjection)until systolic blood pres-
sure (SBP) fell to 50% of baseline values. Then, an-
imals were randomized to one of the following treat-
ment groups:
Group 1. Control: rats received a loading dose of
normal saline (1 mL) followed by a continuous infu-
sion (1 mL/h). n = 7 rats.
Group 3. Levosimendan: levosimendan (donated by
Abbott Australasia, Sydney, Australia) was adminis-
trated to rats by loading dose of 6µg/kg, then levosi-
mendan infusion at 0.4µg/kg/min. n = 6 rats.
3 SIGNAL PROCESSING AND
SPECTRUM ANALYSIS
The blood pressure signal was processed by an al-
gorithm that extracts the cyclical features of the sig-
nal such as SBP (P
s
), diastolic pressure (P
d
), pulse
pressure (P
p
), integrated mean blood pressure (MAP),
stroke volume (SV), cardiac output (CO), heart rate
(HR), systolic time (T
s
), and diastolic time (T
d
). To
summarize, ABP signal, sampled at 400 Hz, has to
pass through four stages of processing which are: 1)
low-pass filtering to remove the high frequency noise,
2) a windowed and weighted slope sum function to
support and enhance the up slope of the arterial blood
pressure signal and remove the remainder of the sig-
nal, 3) a logic circuit that detects the edges of the pro-
cessed slope sum function, and 4) threshold and deci-
sion rule that is used to suppress the edges resulting
from the dicrotic notch and noise. To obtain SBPV
signal, SBP was detected from the continuous record-
ing of ABP signal as follows: after low-pass filtering
of ABP signal, the signal is processed using the slope
sum function (Moody et al., 2003) defined as follows:
s
k
=
k
∑
j= k−w
∆y
j
, (1)
where
∆y
j
=
(
∆x
j
if ∆x
j
> 0,
0 if ∆x
j
≤ 0.
(2)
Here w is the number of samples representing the
analyzing window of the first derivative of the BP sig-
nal ∆x
j
= x
j
−x
j− 1
, and x
j
is the ABP signal. w is cho-
sen to be 32 samples which is equal to the upslope of
the ABP peaks. Pulse contour method (Kouchoukos
et al., 1970) was used to estimate beat-by-beat values
of SV.
The time series of SBPV and SVV signals were
extracted from the raw beat-by-beat ABP and divided
into epochs after down and equidistant sampling were
applied to the signals. For each block of discrete data,
power spectral density was calculated directly from
the signal itself using the FFT algorithm. Average
spectral densities of SBPV and SVV obtained from
all rats within each group was then calculated and
compared. For each data block, the spectral density
estimates were smoothed. In this study, the spectral
estimate was performed on 312 data blocks of 512
samples overlapping by a half to reduce the loss of
stability.For each data set, the linear trends were re-
moved to reduce their contributions to the LF compo-
nent. Average spectra were evaluated approximately
every 5 minutes for each block of data. Spectral esti-
mates were found in each groupbeforeand after drugs
infusion has started.
4 Results
The extracted physiological parameters observed
from control group (baseline), after verapamil poi-
soning, and after continuous infusion of levosimen-
dan are summarized in Table 1.
Figure 1 shows the average spectra of SBPV and
SVV signals obtained from control group before ad-
ministration of any of the study drugs. Spectra of
SBPV and SVV exhibited LF band (0.03 − 0.8 Hz),
which corresponds to the activity of the sympathetic
BIOSIGNALS 2009 - International Conference on Bio-inspired Systems and Signal Processing
412
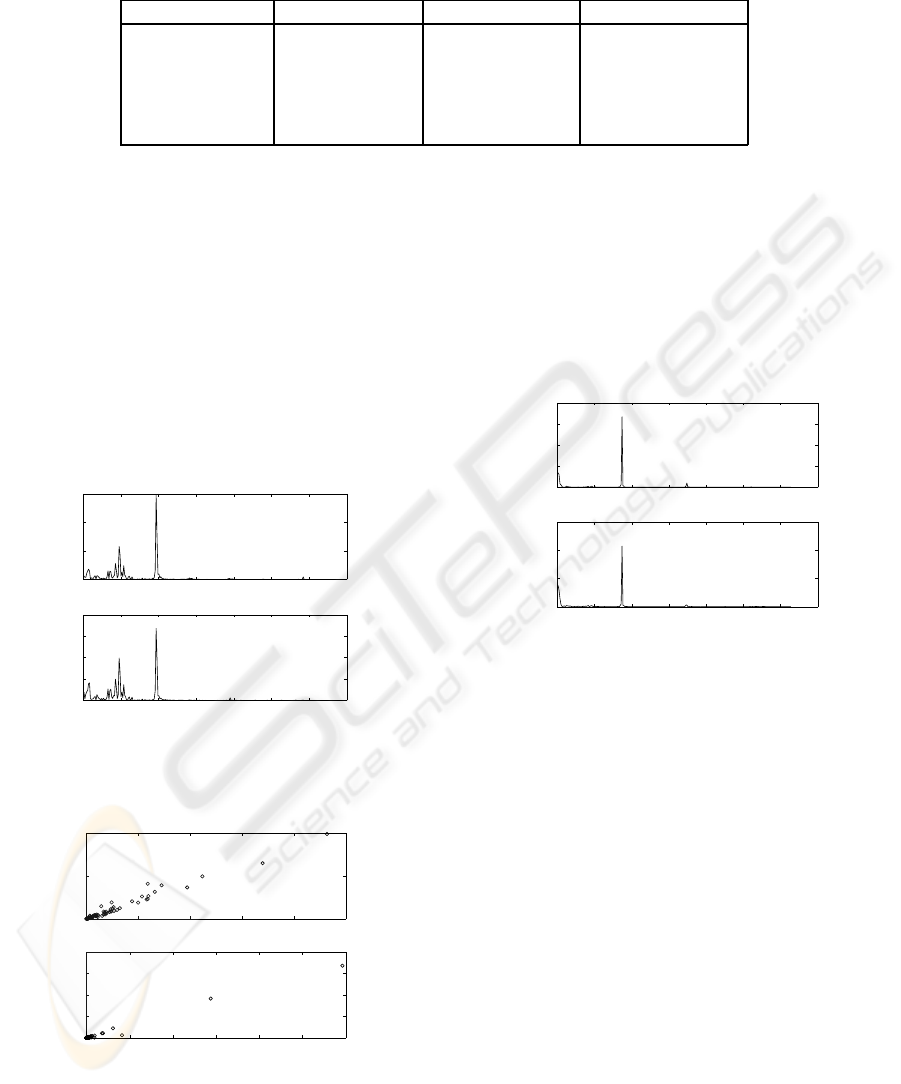
Table 1: Cardiovascular parameters extracted form continuous recording of ABP signals. Values included are the average
values obtained within each group. ABP: arterial blood pressure.
Variable Control Verapamil Levosimendan
P
s
(mmHg) 124.138±8.218 56.149±4.086
∗
57.108±5.087
†
MAP (mmHg) 92.731±7.258 63.709±12.537
§
66.643±2.953†
SV (µL/beat) 271.178±5.43 141.773±2.583
§
182.178±0.827
§
CO (mL/min) 76.089±1.89 24.278±1.670
§
56.598±6.975
§
HR (beats/min) 328.393±6.12 262.503±4.366
∗
301.737±10.293
∗
Values shown as Mean±SD. Paired t-test
§
p < 0.05,
∗
p < 0.01, and
†
: not significant.
part of the autonomic nervous system, and a HF one
(0.8 − 3) Hz. Two clear peaks were detected in each
frequency band; the HF peak at ∼ 1 Hz which syn-
chronized by respiration and related to the parasym-
pathetic tone, and the LF peak at ∼ 0.4 Hz which
is related to sympathetic nervous activity. Note the
dominance of the vagal tone in the non-stressed state
prior to the induction of verapamil toxicity. This is
evidenced by the HF component being larger than
the LF one. Significant positive correlation between
spectra of SBPV and SVV are seen in both LF and
HF bands (figure 2).
0 0.5 1 1.5 2 2.5 3 3.5
0
200
400
600
mmHg
2
/Hz
0 0.5 1 1.5 2 2.5 3 3.5
0
5
10
15
20
Frequency (Hz)
ml
2
/Hz
Figure 1: Average spectra for both signals SBPV (top
panel), and SVV (bottom panel) estimated from control
group prior administration of any drugs.
0 50 100 150 200 250
0
5
10
SBPV (LF)
SVV (LF)
0 100 200 300 400 500 600
0
5
10
15
20
SBPV (HF)
SVV (HF)
r = 0.967, p < 0.05
r = 0.988, p < 0.05
Figure 2: Correlation analysis between LF bands in SBPV
and SVV (top panel), and between HF band (bottom panel)
in control group.
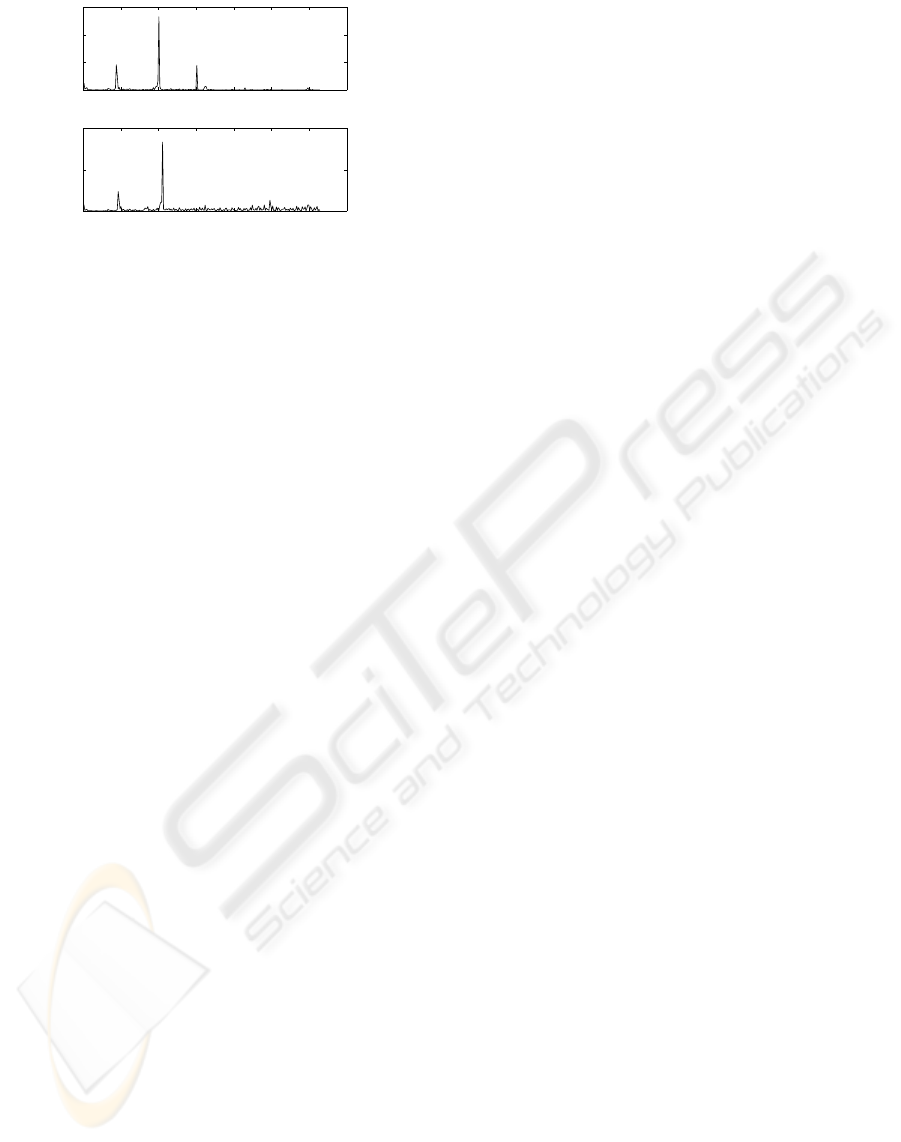
Shock state was introduced by an overdose infu-
sion of verapamil. As shown in figure 3, this com-
pletely abolished the LF component and shift the HF
component to ∼ 0.9 Hz of both SBPV and SVV spec-
tral traces. The HF peaks in both spectra were en-
hanced suggesting that sympathovagal balance was
shifted to the parasympathetic predominance. A
highly significant correlation (R
2
= 0.977, p < 0.05)
between the two frequency bands LF and HF in both
spectra was obtained.
0 0.5 1 1.5 2 2.5 3 3.5
0
500
1000
1500
2000
mmHg
2
/Hz
0 0.5 1 1.5 2 2.5 3 3.5
0
20
40
60
Frequency (Hz)
ml
2
/Hz
Figure 3: Average spectra for both signals SBPV (top
panel), and SVV (lower panel) estimated after verapamil
infusion.
The shape of power spectra of SBPV and SVV
observed after the continuous infusion of levosimen-
dan were markedly altered (figure4). Clearly, com-
pared with spectra obtained immediately after the in-
duction of verapamil, the LF component of both spec-
tra was observed to recover with concomitant reduc-
tion in the HF band peak. These results suggest that
there is a recovery of sympathetic tone after the con-
tinuous infusion of levosimendan. This may be due
to the improvements of the contractility profile of the
heart. Additionally, a new frequency component was
observed at ∼ 1.5 Hz in the spectrum of the SBPV
which does not appear in SVV spectrum. Signifi-
cant correlation were noted between LF (R
2
= 0.943,
p < 0.05) and MF (R
2
= 0.978, p < 0.05) bands from
both spectra, while a poor correlation was noticed be-
tween HF (R
2
= 0.295, p = 0281) bands.
THE POWER SPECTRA RESPONSE OF STROKE VOLUME AND ARTERIAL BLOOD PRESSURE VARIABILITY
SIGNALS TO AUTONOMIC NERVOUS SYSTEM MODULATION OF THE HEART
413
0 0.5 1 1.5 2 2.5 3 3.5
0
100
200
300
mmHg
2
/Hz
0 0.5 1 1.5 2 2.5 3 3.5
0
5
10
Frequency (Hz)
ml
2
/Hz
Figure 4: Average spectra for both signals SBPV (top
panel), and SVV (lower panel) estimated after a continuous
infusion of levosimendan.
5 DISCUSSION
Spectral analysis of HRV has been used to study the
sympathovagalbalance of the autonomic nervous sys-
tem due to therapeutic verapamil infusion in humans
after acute myocardial infarction (Pinar et al., 1998),
in hypertensive patients (Sahin et al., 2004), and nor-
mal humans (Fauchier et al., 1997).
In the present study, verapamil overdose resulted
in a sharp drop in systolic, diastolic, mean blood pres-
sure, SV, HR, and CO. Additionally, it completely
abolished the LF component and enhanced the HF
one in both spectra suggesting that verapamil has
an anti sympatholytic properties contributing to its
negative inotropic effects and its vasodilatory proper-
ties. Hemodynamically, compared with period maxi-
mal verapamil toxicity seen prior to the administra-
tion of levosimendan, it significantly improved CO
with no improvements in blood pressure while sig-
nificant improvements were noticed in SV and HR. In
this study, levosimendan produced improvements in
cardiac function in heart failure induced by verapamil
poisoning. The results of ourstudy correlate well with
the hemodynamicparameters reported by Graudins et
al. (2008) in verapamil poisoned rats. Levosimendan
helped restore the LF component and reduced the HF
component suggesting that both drugs restored sym-
pathovagal balance seen prior to the administration of
verapamil. This dominance of sympathetic tone may
be the reason for the improvements of the myocardial
muscle contractility which cause the improvementsin
cardiac output heralded by a new frequency compo-
nent at ∼ 1.5 Hz in both spectra of SBPV and in SVV.
6 CONCLUSIONS
Spectral analysis of SVV signal may provide, along
with SBPV, useful information to clinicians regarding
the activity of the autonomic nervous system, cardiac
output, and responses to therapies aimed at improving
hemodynamic stability in hypotension patients.
ACKNOWLEDGEMENTS
This work was supported in part by The Australian
Research Council. It is also supported by an Amer-
ican College of Medical Toxicology Antidotal Re-
search Grant. Levosimendan was kindly donated by
Abbott Australasia.
REFERENCES
Brown, D., Brown, L., Patwardham, A., and Randall, D.
(1994). Sympathetic activity and blood pressure are
tightly coupled at 0.4 hz in conscious rats. Am J Phys-
iol, 267(5 pt 2):R1378–84.
Cerutti, C., Berr´es, C., and Paultre, C. (1994). Baroreflex
modulation of blood pressure and heart rate variabil-
ities in rats: assessment by spectral analysis. Am J
Physiol, 266(35):H1993–H2000.
Fauchier, L., Babuty, D., Autret, M., Cosnay, P., and
Fauchier, J. (1997). Effects of verapamil on heart rate
variability in subjects with normal hearts. Am J Car-
diol, 80(9):1234–5.
Graudins, A., Najafi, J., and Perry, M. (2008). Treatment of
experimental verapamil poisoning with levosimendan
utilizing a rodent model of drug toxicity. Clin Toxicol,
46(1):50–6.
Japundzic, N., Grichois, M., Zitoun, P., Laude, D., and El-
ghozi, J. (1990). Spectral analysis of blood pressure
and heart rate in concious rats:effects of autonomic
blockers. J Auton Nerv Syst, 30(2):91–100.
Julien, C., Chapuis, B., Cheng, Y., and Barr´es, C. (2003).
Dynamic interactions between arterial pressure and
sympathetic nerve activity: role of arterial barore-
ceptors. Am J Physiol Regul Integr Comp Physiol,
285(4):R834–41.
Kouchoukos, N., Sheppard, L., and McDonald, D. (1970).
Estimation of stroke volume in the dog by a pulse con-
tour method. Circulation Research, 26(5):611–23.
Liu, H., Yambe, T., Sasada, H., Nanka, S., Tanaka, A., Na-
gatomi, R., and Nitta, S. (2004). Comparison of heart
rate variability and stroke volume variability. Auton
Neuro: Basic and Clinical, 116(1-2):69–75.
Moody, G., Mark, R., Zong, W., and Heldt, T. (2003). An
open-source algorithm to detect onset of blood pres-
sure pulses. IEEE Computers in Cardiology, 30:259–
262.
BIOSIGNALS 2009 - International Conference on Bio-inspired Systems and Signal Processing
414

Pinar, E., Garc´ıa-Alberola, E., LIamas, C., Vicente, T.,
L´opez-Candel, J., Rojo, J., Fern´andez, R., and Vald´es,
M. (1998). Effects of verapamil on indexes of heart
rate variability after acute myocardial infarction. Am
J Card, 81(9):1085–9.
Sahin, I., Kosar, F., Altunkan, S., and G¨unaydin, M. (2004).
Comparison of the effects of amlodipine and vera-
pamil on autonomic activity in hypertensive patients.
Eur J Intern, 15(4):225–230.
Siebert, J., Drabik, P., Lango, R., and Szyndler, K. (2004).
Stroke volume variability and heart rate power spec-
trum in relation to posture changes in healthy subjects.
Med Sci Monit, 10(2):MT31–7.
THE POWER SPECTRA RESPONSE OF STROKE VOLUME AND ARTERIAL BLOOD PRESSURE VARIABILITY
SIGNALS TO AUTONOMIC NERVOUS SYSTEM MODULATION OF THE HEART
415
