
Supporting Registration and Treatment of Clubfoot using
Mobile Devices
Weiqin Chen and Dag Skjelvik
Department of Information Science and Media Studies, University of Bergen
POB 7802, N-5020 Bergen, Norway
Abstract. In current congenital clubfoot treatment, clinicians use paper forms
to register and monitor the treatment process. Routines for registration and arc-
hiving are scarce, and the guideline for treating clubfoot is not always followed
strictly. This paper presents a PDA-based system (GenSupport) that can support
the registration of patient information, supervise the treatment process, as well
as provide advice during treatment. GenSupport has been evaluated in order to
investigate the perceived usefulness of such a system. The evaluation results
indicate that GenSupport has the possibility of improving the routines for regis-
tration and archiving of patient information as well as supporting the treatment
of clubfoot. The advice provided by GenSupport was perceived particularly
useful for inexperienced clinicians.
1 Introduction
Clinicians suffer almost universally from the problem of poor data quality, difficulty
of access and bad communication. In addition, some individuals need support in deci-
sion-making. Therefore well-designed patient oriented information systems which
improve the routines of registration and archiving of patient data and decision support
systems which monitor and support treatments are desperately needed throughout the
Health Service. In recent years, with the development of Internet and mobile technol-
ogies, research in healthcare has been shifted towards mobile Electronic health record
and clinical decision support systems.
Clubfoot (Talipes equinovarus) is a congenital condition where the foot is de-
formed and turns inward and downward. It is the most common birth defect, and in
most cases it is treated using mainly non-surgically methods. The Ponseti-Pirani me-
thod is now considered to be the worldwide standard of treating clubfoot [1]. In this
method the Pirani score is for classifying the severity of the clubfoot and the Ponseti
method for correction.
Pirani scoring is a standardized way of classifying a clubfoot. The score is built up
of six clinical signs, where each sign is assigned a value as following: 0 - normal, 0.5
- moderately abnormal, 1 - severely abnormal. The final score is the sum of these
values, ranging from 0 for a normal foot to 6 for a severe clubfoot.
With the use of regular cast, the Ponseti method corrects the clubfoot by weekly
corrections supported by the cast. This treatment is guided by the results of Pirani-
scoring of the clubfoot. After 5-8 weeks the foot is manipulated into the correct posi-
Chen W. and Skjelvik D. (2009).
Supporting Registration and Treatment of Clubfoot using Mobile Devices.
In Proceedings of the 1st International Workshop on Mobilizing Health Information to Support Healthcare-related Knowledge Work, pages 32-41
DOI: 10.5220/0001813700320041
Copyright
c
SciTePress

tion. In most cases the achilles tendon has to be cut in order to prolong it, this process
is called tenotomy and is usually done before the last application of cast. The final
part of the treatment is to use an orthosis (brace) at night until the foot stabilizes and
is fully corrected. If the child is older than two years and surgery can be performed at
the treating hospital, a small procedure called anterior tibialis transfer (ATT) is per-
formed. After this procedure is performed, the child should not start using the brace.
The treatment of clubfoot using the Ponseti method is as of today not computer
supported. The clinicians use paper forms to monitor the treatment. After the foot is
scored, the results are plotted with a pen into a graph on paper. Classification results
vary depending on the clinician performing it. Information registered about the pa-
tient is usually unstructured and archived in an ad-hoc manner and sometimes not
archived at all. Thus, there are few possibilities to perform statistical analysis. The
treatment process is in some cases ineffective because the Ponseti guideline is not
followed strictly. Mistakes made by clinicians during treatment are often discovered
too late and this can either corrupt or prolong the treatment process.
According to Osheroff et al.[2], the best opportunity for a computer-based system
to deliver interventions is usually when the pertinent persons can be reached with the
intervention and are prepared to act upon the information immediately. Handheld
computers are the most versatile in stressful clinical environments, especially in those
that are lack of infrastructure. Therefore we believe that a PDA-based system could
improve the treatment by controlling registration of patient information, supervising
the treatment process as well as providing advice during treatment. In this paper we
present the design and evaluation of such a system (GenSupport).
2 Methodology and Related Research
The project described in this paper follows a design research methodology. Design
research involves the analysis of the use and performance of designed artefacts to
understand, to explain and frequently to improve upon the behaviour of aspects of
information systems [3]. Design science research seeks to create innovations “through
which the analysis, design, implementation, management and use of information
systems can be effectively and efficiently accomplished” [3]. A general design
science methodology includes cycles of identification of need, development and eval-
uation. In addition, a final conclusion phase can be added [4]. In this project, itera-
tions of requirement analysis, development and evaluations have been conducted.
2.1 Clinical Decision Support Systems
Clinical decision support systems (CDSS) are computer systems designed to impact
clinician decision making about individual patients at the point in time that these
decisions are made [5]. The intention of a CDSS is to provide information to the
clinicians in the decision making process rather than to provide correct “answers” and
diagnoses to clinicians and consider the clinicians as passive users of the system.
Over the years research has been conducted in this area and many CDSS have been
developed and some have been integrated in clinical practice. For example, Dugas et
33

al. [6] constructed a CDSS for hepatic surgery. The system provides decision support
for the surgeon and the patient during risk assessment prior to critical surgery. Case-
based reasoning was adopted to provide guidance in the risk assessment process.
Dugas et al. also discussed success factors for a CDSS. The tool must be fast and easy
to use, and the system must provide a comprehensible benefit for the user. The clini-
cian’s work flow must be integrated in the system, and the knowledge base should
provide the clinician with the opportunity to view full patient data [6]. Similar to
GenSupport, the Standards-based Shareable Active Guideline Environment (SAGE)
computerizes clinical guidelines and providing decision support. A benefit of SAGE
is that clinical guidelines can be encoded using standard terminologies and standards-
based patient information models [7], amongst these HL7 and Snomed CT.
LogReg is a decision-support shell which runs on handheld computers [8]. This
system utilizes decision models encoded in XML to provide decision support. Avail-
ability on the location at which the decisions are made is considered as the reason for
choosing a mobile platform for the system. As in GenSupport, the system is entirely
configured with the XML file and the configuration process does not involve pro-
gramming or re-compilation of the system. Several XML files can be loaded in the
system at the same time, available to the user. LogReg is intended for single encoun-
ters only, and does not provide decision support for treatments with multiple encoun-
ters.
The GenSupport system can be considered as a CDSS for clubfoot treatment. In
addition, the system provides patient and treatment registration support in order to
improve the routines for registration and archiving of patient information.
2.2 Mobile Healthcare Systems
Mobile devices are increasingly popular in the medical domain [9]. By 2013, it is
expected that hospitals will use more mobile than stationary computers [10]. Mobile
technologies can improve responsiveness in healthcare and increase productivity [11].
Size and mobility are key benefits of mobile devices. The portability of the mobile
devices enables clinicians to access and register patient information wherever they
prefer [9].
However, there are a few challenges in designing mobile healthcare systems. A
small low-resolution screen and limited computational abilities makes it challenging
to implement user-friendly and complex applications [11]. Slow entry of data is
another problem with mobile devices [12]. Data entry is usually done with a pen
directly on the device’s screen by plotting letters on a keyboard displayed on the
screen. Most mobile devices do not support efficient and effective handwriting rec-
ognition. Patient information and medical knowledge must be available at the mobile
devices, thus data exchange is an important aspect of mobile healthcare. XML is a
format suitable for data exchange across devices, platforms and organizational units,
as long as they agree on the content of the data exchanged [11].
The PDA-based GenSupport system follows the principles of user-friendly mobile
interface design. XML is used for describing the knowledge and information needed
for clubfoot treatment.
34

3 The Design and Development of GenSupport
The design and development of GenSupport follows a user-centred approach [13].
The domain expert has been closely involved in the process. The project was carried
out in an iterative and incremental manner and emphasized the communication among
different stakeholders.
3.1 Requirements
The requirements were gathered through meetings and low-fidelity mock-ups. The
system should be able to:
− Allow clinicians to register core patient information,
− Allow clinicians to register attributes of the clubfoot,
− Provide treatment recommendations based on clubfoot treatment guideline and
information registered by the clinicians using it,
− Run on a handheld device (e.g. PDA with Windows mobile OS).
3.2 Patient Information
Core patient information is registered and stored in the system; this contains general
information about the patient and clubfoot treatment guideline specific information.
The clinician can register new patients and edit existing ones as well as search for
registered patients and encounters. The general patient information is standardized
information which is adapted from the data model of OpenMRS
(http://www.openmrs.org) and includes Name of the patient, Residence / Address,
Next of kin, Health center, and ID numbers. The clubfoot specific information in-
cludes history of encounters (dates, scores, actions).
3.3 Domain Knowledge (Clubfoot Treatment Guideline)
The domain knowledge acquisition process was carried out in several iterations. First,
the domain expert provided a diagram describing how clubfoot is treated. This dia-
gram described the entire process of clubfoot treatment, in addition to all the phases
of the treatment.
The diagram was later converted to a workflow of clubfoot treatment. This
workflow shows all steps possible for the clinician to go through at each encounter.
Preconditions determine when it is appropriate to include a step in the workflow. For
example, the step “Pirani score right foot” would not be included in the workflow for
a patient when only the left foot is affected.
The rules for providing treatment recommendations were extracted and represented
in a decision tree (Fig. 1). The decision tree is composed of two kinds of nodes; inter-
nal nodes and leaf nodes. Internal nodes have a list of child nodes, while the leaf
nodes have a list of statements. Each recommendation is a suggestion from GenSup-
port to the clinician to perform a certain action such as “Cast right foot for three
35
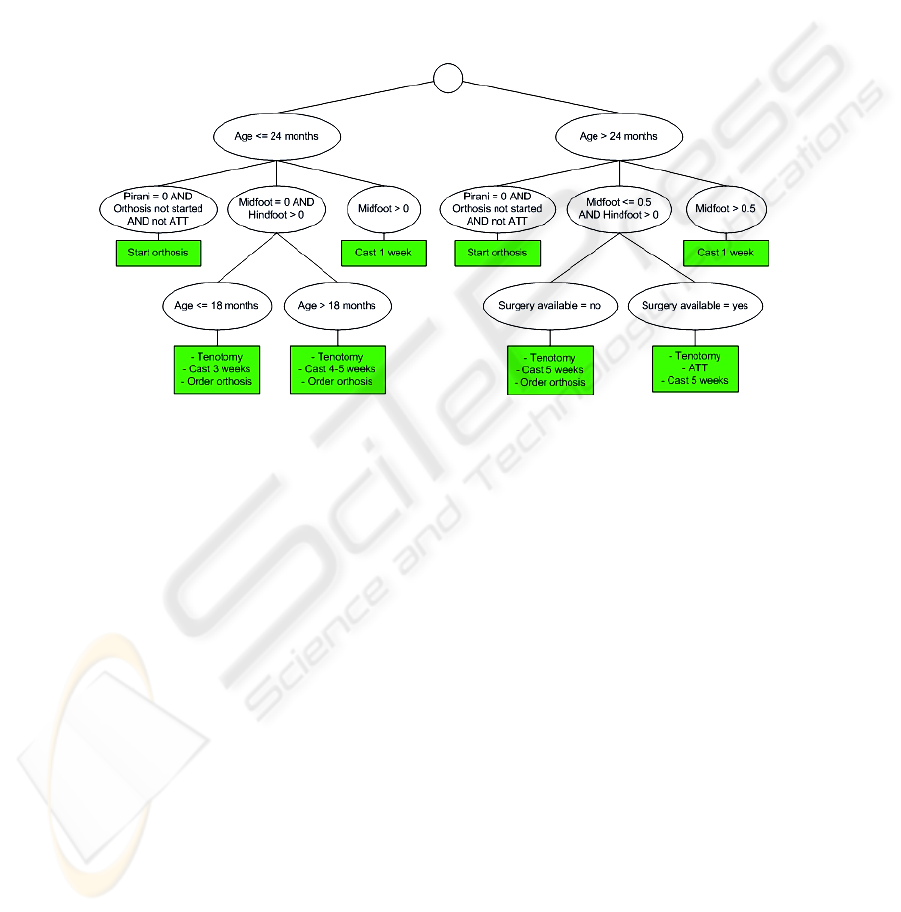
weeks” or “Perform tenotomy on left foot” In addition to suggesting which actions to
perform, GenSupport can also provide warning (e.g. “Warning! Check treatment of
right foot”) and error messages (e.g. “ERROR! Check treatment of left foot”). A
warning message is given when something could be wrong, i.e. when there are rea-
sons for suspecting that the treatment is not progressing as normal and special meas-
ures must be taken to prevent the treatment going wrong. When something indicates
that the treatment most likely has gone wrong, an error message is provided to the
user.
The workflow and decision tree were used further in the knowledge engineering
process as a communicating artefact to communicate with the domain expert.
Fig. 1. Decision tree for clubfoot treatment.
3.4 Rule Engine
A specific rule engine (Eval3RulesEngine) was implemented for PDAs. This rule
engine is based on an external library Eval3 which parses expressions represented by
strings, and returns the truth value of the expression. When the Eval3RulesEngine
runs, it parses the decision tree depth-first and evaluates the conditions of the rule at
each node. Internal nodes evaluated as true will be expanded, whilst the tree will be
cut at those internal nodes having a condition evaluated as false. When a leaf node is
evaluated as true, its statement will be placed on the agenda of the Eval3RulesEngine.
The agenda is a list of the statements contained in the leaf nodes evaluated as true.
This list is available after the execution is finished. The rules engine parses the full
decision tree, not stopping at the first leaf node evaluated as true.
3.5 Recommendations
When the clinician is provided with the recommendations for treatment, s/he can
choose to reject the recommendations, plan actions according to the recommendations
or add actions manually (Fig. 2).
36
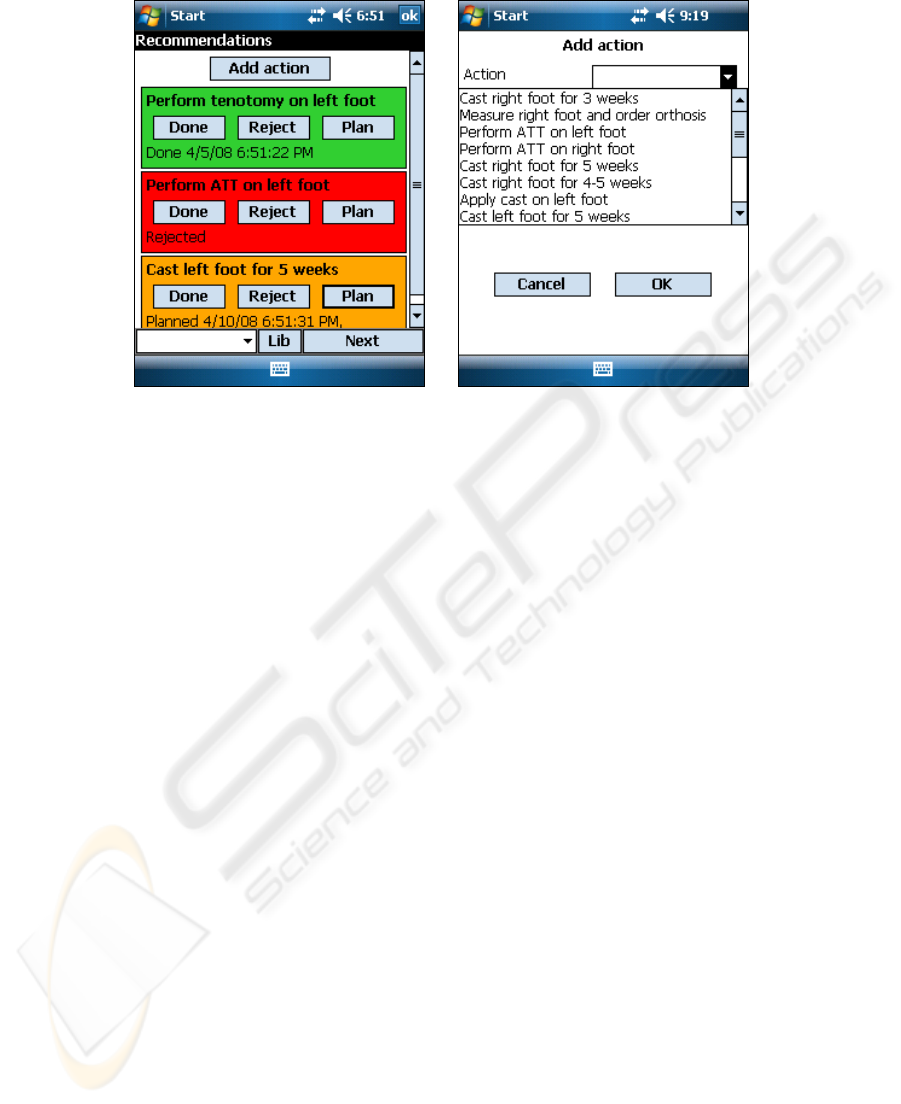
Fig. 2. Recommendations.
According to Osheroff et al. [2] there are standard reasons for rejecting treatment
recommendations: MD disagrees with recommendation, recommendation already
implemented, alert fired inappropriately, patient ineligible for recommended interven-
tion, patient refuses recommended intervention, and others. These standard reasons
are implemented in GenSupport. The clinician should also provide a comment ex-
plaining why the overriding was done.
It is not always possible or feasible to perform the recommended action instantly.
This calls for the need to be able to plan the actions. In GenSupport it is possible for
the clinician to postpone an action, and plan for when to perform it. A date must be
specified, and the clinician should state a comment about why the action is post-
poned.
The clinicians are able to manually invoke an action if they believe that a certain
action is correct to perform under the given conditions even though GenSupport has
not suggested it. They can choose amongst the actions which are specified in the
current guideline. When choosing an action manually, they should specify the reason
for the choice.
4 Evaluation
The evaluation of GenSupport focuses on whether it is able to support the clubfoot
treatment. First, a quantitative evaluation is conducted to test the quality of the rec-
ommendations given by the system. In this evaluation, we used the 17 patient data
from a different orthopaedian than our domain expert to test the quality of the rec-
ommendations provided by the system. A qualitative evaluation was also conducted
with three clinicians including our domain expert and two from another hospital,
where the goal is to evaluate the usability and usefulness of GenSupport, in addition
37
to identifying issues in need of improvement.
4.1 Quantitative Evaluation of Recommendations
Patient data were provided by another orthopaedian who works in a different hospital
from the domain expert. A data set containing full treatment history on 17 patients
having congenital clubfoot on right foot, left foot or both feet was used. These pa-
tients have been treated by this orthopaedian. The full treatment history is used to
compare with the recommendations by GenSupport.
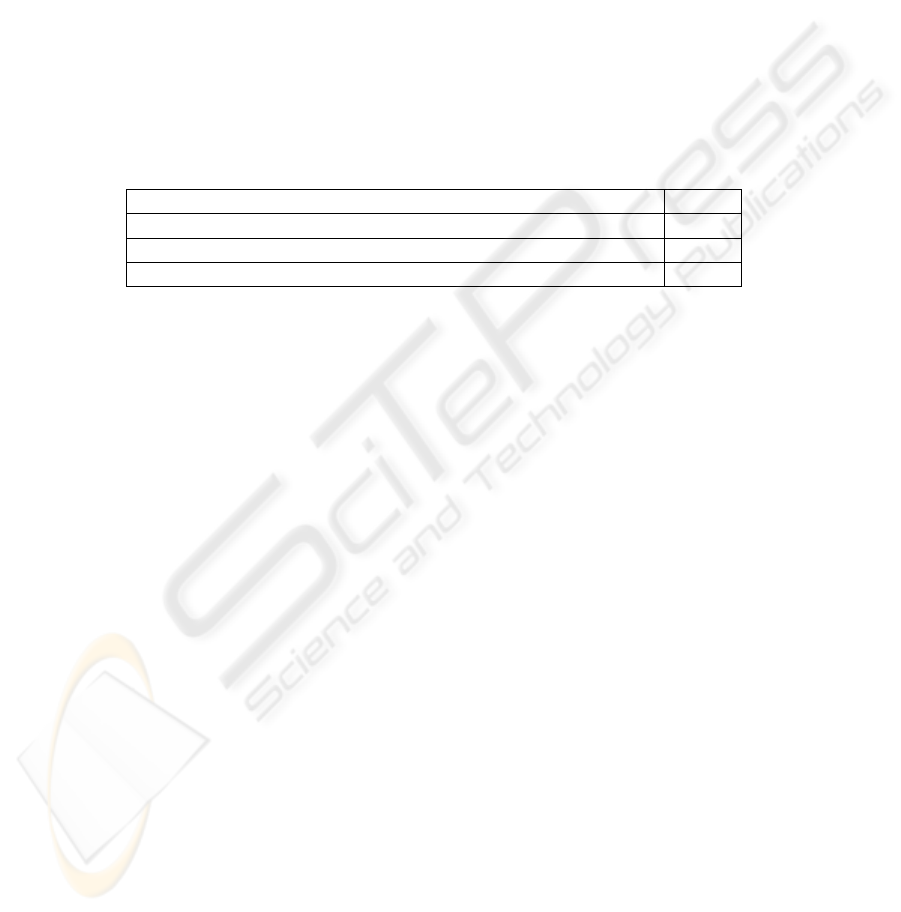
As shown in Table 1, GenSupport provided the same recommendations of the
treatment as performed by the clinician on 5 of the 17 patients. On the other patients,
the system advised to perform the tenotomy either before (7 of 17) or after (5 of 17) it
was actually performed by the orthopaedian.
Table 1. Evaluation of the recommendations by GenSupport.
Status Cases
Correct (identical with the treatment performed by the clinician) 5
Tenotomy advised before actually performed 7
Tenotomy advised later than actually performed 5
Since the data set used in this evaluation is from another orthopaedian than our do-
main expert, it is possible that there are small variances in how the different ortho-
paedians treat clubfoot. This can explain some of the incorrect cases in that evalua-
tion.
According to the domain expert, the Ponseti expert group specifically recommends
to perform tenotomy as soon as the midfoot score is 0. When the clinicians are in
doubt about whether the procedure should be performed, they should perform it [1].
In seven of the cases investigated in this test, tenotomy was not performed according
to the recommendations from the Ponseti expert group. In these cases, the recommen-
dations were correct and the clinicians provided a sub-optimal treatment.
In five of the cases, the clinicians performed tenotomy earlier than GenSupport
recommended. In these cases, there is no apparent pattern describing why the clini-
cians have acted as they have. The clinicians’ actions are most likely based on factors
not documented in the patient data available in this evaluation. It is reasonable to
believe that the clinicians provided what was considered to be the best care for their
patients in these cases.
4.2 Qualitative Evaluation of Functionality and Usefulness
Qualitative evaluation methods such as think aloud, observation and semi-structured
interviews were used in this part of the evaluation of GenSupport. All three clinicians
(one is our domain expert and the other two are from a different hospital. They are
referred as doctor 1, 2 and 3 respectively in the text) in the evaluation are experienced
orthopaedians in treating clubfoot.
38

First, clinicians were observed while carrying out some pre-defined tasks and us-
ing the system with patients who have finished the treatment to assess whether the
system gives the same advice as the clinician did when treating. After finishing this
phase, semi-structured interviews with the clinicians involved in the evaluation were
conducted to gather more information on the usability and usefulness of the system.
The interviews and the think-aloud sessions have been audio recorded. The inter-
views have been transcribed.
Functionality and Perceived Usefulness. All the clinicians were generally satisfied
with GenSupport. The clinicians had the same opinion about whether they believed
they could benefit from using the system. Due to their high level of expertise, they
did not believe they could benefit from getting treatment advice from this clinical
decision support system. Doctor 1 and 2 believed that GenSupport would be best
suited as a tool for training novice clinicians. They stated that “The registration would
be more efficient; (…) it would be a lot more reliable and efficient. When it comes to
the treatment, it depends on how experienced one is. Those who are experienced
know how to do the treatment. But it takes a long time to get experienced (…), for
those who have few patients, and who have just started learning this would be very
helpful. (...) Through a decision support system, an experienced person can convey
his/her knowledge to others.” “I believe that in an environment where there are inex-
perienced nurses, physiotherapist or physicians who are going to treat a lot of pa-
tients, [GenSupport] can be useful in the beginning (…).” Doctor 3 implied this by
saying that he felt the system was not necessary because of his level of competence:
“I would not use it to get recommendations in the treatment I provide, because I feel
that when you know how to do it, it is easy.” A decision support system is an impor-
tant tool to gather knowledge from experienced clinicians and use this knowledge to
train less experienced ones [14]. Clinicians are highly educated professionals, and
they have thorough training in the procedures they perform. A clinical decision sup-
port system might thus not be of much help to clinicians who have finished training,
especially when the treatment procedure is easy to understand. However, decision
making often becomes more complicated when the decision depends on many differ-
ent variables, and then skilled clinicians might also benefit from a tool like GenSup-
port when the condition is more complex than in this evaluation.
All the clinicians identified an area which GenSupport could help improving: the
current routines of registration and archiving data about the treatment. They stated
that these routines currently do not work as supposed to, and that they often expe-
rienced that treatment data are not registered as it should be. Treatment data are regis-
tered insufficiently, or not at all. This problem is most likely caused by the hectic
environment in which the clinicians work, since electronic medical records are used
as a standard at all hospitals. GenSupport can help to improve the registration by
“forcing” the clinicians to register proper treatment data while treating the patient.
Experience with PDA. One interesting findings from the evaluation is that none of
the clinicians in the evaluation had difficulties using the handheld computer although
none of them have any prior experience with PDAs. The soft keyboard which the
users of the handheld computers can utilize to input text can be difficult for regular
39

users to get used to, since using it requires a high level of precision. Observation
showed that the clinicians in the evaluation had no problems at all using the soft key-
board, even though they were not used to such a small user interface. This is most
likely because the clinicians in the evaluation are skilled and experienced surgeons,
who have extensive training in tasks requiring high precision.
When asked to compare mobile devices with desktop computers in the daily prac-
tice, doctor 2 emphasized that a handheld computer is easier to use and transport in a
hectic clinical environment. “(…) you can keep the handheld computer in your pocket
when working with the patient (…)”. He often works in several rooms, and appre-
ciates the mobility of the handheld computer. Also, he pointed out that the handheld
computers are more robust than a regular computer. They are resistant to dust and
shock. Another advantage which he emphasized is the quick start-up time of the
handheld computers, compared to a regular computer. While regular computers often
need several minutes before being ready to use, handheld computers are ready almost
instantaneously. The time saved can in some cases be both precious and valuable in a
hectic environment.
5 Conclusions and Future Work
This paper presents the development and evaluation of GenSupport—a mobile system
to support the registration and treatment of clubfoot. The system was found to be able
to improve and simplify the registration process and “force” the medical personnel to
follow routines more strictly. It is also considered to be an appropriate training tool.
The system has been designed as a generic framework for supporting clinical guide-
lines and clubfoot is used as the first instance. To support another guideline, one only
needs to replace the configuration XML file with a new one which contains the new
guideline.
The system will be further developed based on the feedback from the evaluation.
Some functions need to be revised and added. For example, adding functionality for
scheduling encounters so that the clinicians can plan and follow up the treatment. To
enhance the clinician’s confidence in the system, an explanation subsystem should be
added to GenSupport in order to provide evidence and rationales for the recommen-
dations”. In the near future, after we have made improvement on the system, we plan
to conduct a thorough evaluation focusing on the practitioner performance and patient
outcome [15].
Acknowledgements
The authors would like to thank Jørn Klungsøyr and Peter Klungsøyr (domain expert)
who initiated the project and other clinicians who participated in the evaluation.
40

References
1. Staheli, L.: Clubfoot: Ponseti Management (2nd Edition). Oxford Medical Publications
(2005)
2. Osheroff, J. A., Pifer, E. A., Teich, J. M., Sittig, D. F., Jenders, R. A.: Improving outcomes
with clinical decision support: an implementer’s guide. Healthcare Information and Man
agement Systems Society Press, Chicago (2005)
3. Hevner, A., March, S., Park, J., Ram, S.: Design Science in Information Systems Research.
MIS Quarterly 28 (2004) 75-105
4. Gregg, D., Kulkarni, U., Vinze, A.: Understanding the Philosophical Underpinnings of
Software Engineering Research in Information Systems. Information Systems Frontiers 3
(2001) 169-183
5. Berner, E.S.: Clinical decision support systems: Theory and practice. Springer, New York
(2007)
6. Dugas, M., Schauer, R., Volk, A., Rau, H.: Interactive decision support in hepatic surgery.
BMC Medical Informatics and Decision Making 2 (2002)
7. Tu, S. W., Campbell, J.R., Glasgow, J., Nyman, M.A., McClure, R., McClay, J.: The
SAGE guideline model: Achievements and overview. Journal of the American Medical In-
formatics Association 14 (2007) 589-598
8. Zupan, B., Porenta, A., Vidmar, G., Aoki, N., Bratko, I., Beck, J.R.: Decisions at hand: A
decision support system on handhelds. Studies in Health Technology and Informatics 84
(2001) 566-570
9. Lu, Y., Xiao, Y., Sears, A., Jacko, J.A.: A review and a framework of handheld computer
adoption in healthcare. International Journal of Medical Informatics 74 (2005) 409-422
10. Haux, R., Ammenwerth, E., Herzog, W., Knap, P.: Health care in the information society --
A prognosis for the year 2013. International Journal of Medical Informatics 66 (2002) 3-21
11. Siau, K., Shen, Z.: Mobile healthcare informatics. Informatics for Health and Social Care
31 (2006) 89-99
12. Embi, P. J.: Information at hand: Using handheld computers in medicine. Cleveland Clinic
Journal of Medicine 68 (2001) 840-853
13. Gulliksen, J., Göransson, B., Boivie, I., Blomkvist, S., Persson, J., Cajander, Å.: Key prin-
ciples for user-centred systems design. Behaviour & Information Technology 22 (2003)
397-409
14. Godin, P., Hubbs, R., Woods, B., Tsai, M., Nag, D., Rindfleisch, T., Dev, P., Melmon, K.
L.: A New Instrument for Medical Decision Support and Education: The Stanford Health
Information Network for Education. Proceedings of the 32nd Hawaii International Confe-
rence on System Sciences. IEEE Computer Society, Maui, Hawaii (1999)
15. Garg, A. X., Adhikari, N.K., McDonald, H., Rosas-Arellano, M.P., Devereaux, P.J.,
Beyene, J., Sam, J., Haynes, R.B.: Effects of computerized clinical decision support sys-
tems on practitioner performance and patient outcomes: a systematic review. Journal of the
American Medical Association 293 (2005) 1223-1238
41
