
COMPUTER-BASED SIMULATOR TRAINING IN THE
HOSPITAL
A Structured Program for Surgical Residents
Minna Silvennoinen
Department of Computer Science and Information Systems, University of Jyväskylä, Finland
Teuvo Antikainen, Jukka-Pekka Mecklin
Department of Surgery, Central Finland Central Hospital, Jyväskylä, Finland
Keywords: Computer-based simulator training, Surgical skills, Surgical resident education.
Abstract: Rapid developments in techniques and new skills requirements have increased the need for surgical training
outside the operating room (OR). Simulator training is often seen as a vital part of the surgical resident’s
education. This paper presents a simulator training program aimed at providing surgical skills training for
residents in a hospital. The theoretical background on the subject is considered and initial findings
discussed. The results highlight the need to organize the training systematically. Simulator training prior to
entering the OR should be mandatory for all residents, even though the study showed the motivation for
voluntary participation to be high. The role of the specialist surgeon emerged as an essential element in the
simulator training, both as an evaluator and as an instructor.
1 INTRODUCTION
During their university studies, physicians are
provided with the basic knowledge and skills of
medicine. After graduation, those aiming to become
surgical residents have to work in hospitals for
another period of 5-6 years to achieve the level of a
specialist. The basic university teaching is
thoroughly planned, but the six years of learning for
specialization may well include no detailed learning
or teaching program, and tends to be dependent on
local circumstances. In many medical specialities
self-study via books or the Internet can compensate
for possible defects caused by inadequate training
programs. However, surgical skills cannot be
achieved by reading. Learning comes from
experience in the operating room (OR) or from a
simulated learning environment. At least in Finland,
hospitals are mainly organized to take care of
patients; the training of personnel is a secondary
task.
Video-assisted surgery has changed traditional
surgery and new skills are needed in the OR.
Laparoscopy refers to a surgical technique
performed in the abdominal cavity in which the
operation is conducted through small incisions, with
the surgeon viewing the operating area from a video-
screen. Laparoscopic operations have proved to be
more difficult than traditional open surgery, for both
experienced and novice surgeons (Madan et al.,
2004; Soper et al., 1994). Rapid developments in
equipment have increased the time needed to learn
surgical procedures. There is thus a need to construct
teaching protocols (Reznick and McRae, 2006) that
are not only more effective in themselves, but also
capable of being embedded within fluent,
economical and routine organizational processes.
Simulator training has been introduced as one
solution that can help to solve the problem of
reducing the time needed to train residents in
acquiring the complex skills in question. Most
residents began their residency without any manual
skills in laparoscopy, hence one might expect this to
be the the best point at which to introduce simulator
training. However, there is, overall, a lack of
research on guided simulator training in hospitals.
This study discusses a pilot simulator training
program and presents initial results on the
participation of residents in the program, and on the
279
Silvennoinen M., Antikainen T. and Mecklin J. (2009).
COMPUTER-BASED SIMULATOR TRAINING IN THE HOSPITAL - A Structured Program for Surgical Residents.
In Proceedings of the First International Conference on Computer Supported Education, pages 278-283
DOI: 10.5220/0001979502780283
Copyright
c
SciTePress

motivation for training. The paper is organized as
follows: The theoretical grounds for the training are
introduced. A case study and training program in
progress is presented. The aim of the study is set out,
followed by analyses of the initial results. The
results are discussed, with mention of the challenges
that emerged in the study. We present brief
conclusions concerning the training program in its
present state, and make suggestions for the future.
2 THE THEORETICAL BASIS OF
SIMULATOR TRAINING
Here we present the main factors that have
contributed to the creation of simulators, and some
practical ideas for investigating the pedagogical
aspects of simulator training.
2.1 Challenges Regarding the Training
of Skills
It is important to train novices specifically in
laparoscopy, so that they can become automated in
instrument manipulation and in discerning the
transformation of spatial information (Gallagher and
Satava, 2002; Villegas et al., 2003) before entering
the OR. Surgical complications occur most
frequently during the first ten procedures (Jordan et
al., 2000). The technique has certain limitations,
including fixed instrument entry points and limited
degrees of freedom (Berguer et al., 2000). The risks
of the operation are particularly great when one is
working with instruments that are 30 cm in length,
inside the abdominal area, close to fragile organs,
without direct visual contact. The visual-motor tasks
of laparoscopy require excellent hand-eye
coordination. Problems of perceptual motor control
arise when one has to adjust to operating while
watching a two-dimensional monitor image, in a
situation where the camera is held by someone other
than the operating surgeon (Conrad et al., 2006).
One of the main difficulties in learning laparoscopic
skills lies in developing the ability to estimate the
surface roughness of tissues (Brydges et al., 2005).
Overall, it is clear that with this new technique the
challenges in acquiring surgical skills have
increased.
2.2 The Role of Simulators in Training
Simulator training has already given promising
results and has taken on a significant role in teaching
surgical skills, without putting patients at risk
(Cosman et al., 2002; Schjiven et al., 2005; Villegas
et al., 2003). In addition, research has confirmed a
transfer of skills between the simulator and the OR
(Ahlberg et al., 2005 & 2006). For trainees to
achieve the required level of skill, simulator training
should be integrated within the curriculum, and
should rely on the teaching skills of experts
(Ahlberg et al., 2005; Ström et al.,2002). Managing
simulator training has to be an active process, in
order to address the key issue of transferability from
the simulated to the real environment (Kneebone,
2003). The advantages of using simulation have
been listed by Kneebone (2003):
1. Training can be defined by needs of the learner,
not the patient or the teacher.
2. There is permission to fail, and to learn from
mistakes and failures, without risk.
3. The simulator provides objective proofs of
performance and feedback.
The expectations of simulator training have grown at
the same time as simulator technology has evolved.
It has been shown that simulator training improves
OR performance in laparoscopy. Simulators are
regarded as useful tools for introducing equipment
and training technical skills (Poulin et al., 2006).
Simulators could also be used to assess the readiness
of the resident surgeon to proceed to real patient
surgery (Feldman 2004).
3 CASE STUDY: A SIMULATOR
TRAINING PROGRAM FOR
SURGICAL RESIDENTS
The training program was organized in the Central
Hospital of Central Finland. This hospital caters for
a population of almost 280 000. The program forms
part of a multidisciplinary project bringing together
knowledge gained from education, cognitive science
and surgery. The study was performed in a medical
skills learning centre using the interactive Simbionix
Lap Mentor II virtual reality trainer. The training
program was designed to teach laparoscopic skills to
surgical residents, and to further develop existing
skills.
3.1 Study Design – Equipment and
Environment
The medical skills learning centre is an interactive
room containing simulators, cameras and other
CSEDU 2009 - International Conference on Computer Supported Education
280
equipment. The idea was to create a peaceful
learning environment where skills could be trained,
whenever actual patient care would allow this. The
Lap Mentor simulator enables the user to interact
with a three-dimensional database in real time, and it
offers games designed particularly for laparoscopic
skills training, plus a realistic image representation
of an organ system. The simulator has real
instrument handles attached to the machine through
robotic instrument ports; these give the sense of
realistic “touch” contact with tissues and organs.
Exercises vary from games and partial operation
exercises to advanced complete operations,
including laparoscopic suturing tasks performed in a
simulated abdomen.
3.2 The Training Program and Data
Collection
The training program for surgical resident education
was launched in March 2008. Prior to resident
instruction, the specialists were given time to
become familiar with the equipment and exercises.
Due to the complexity of the simulator as training
equipment, both the specialists and the resident
surgeons were offered additional help from the
facilitator of the training program. Working
independently or in pairs, the residents were
instructed by a specialist in using the simulator and
going through the exercises. The training program
exercises were selected by a specialist surgeon who
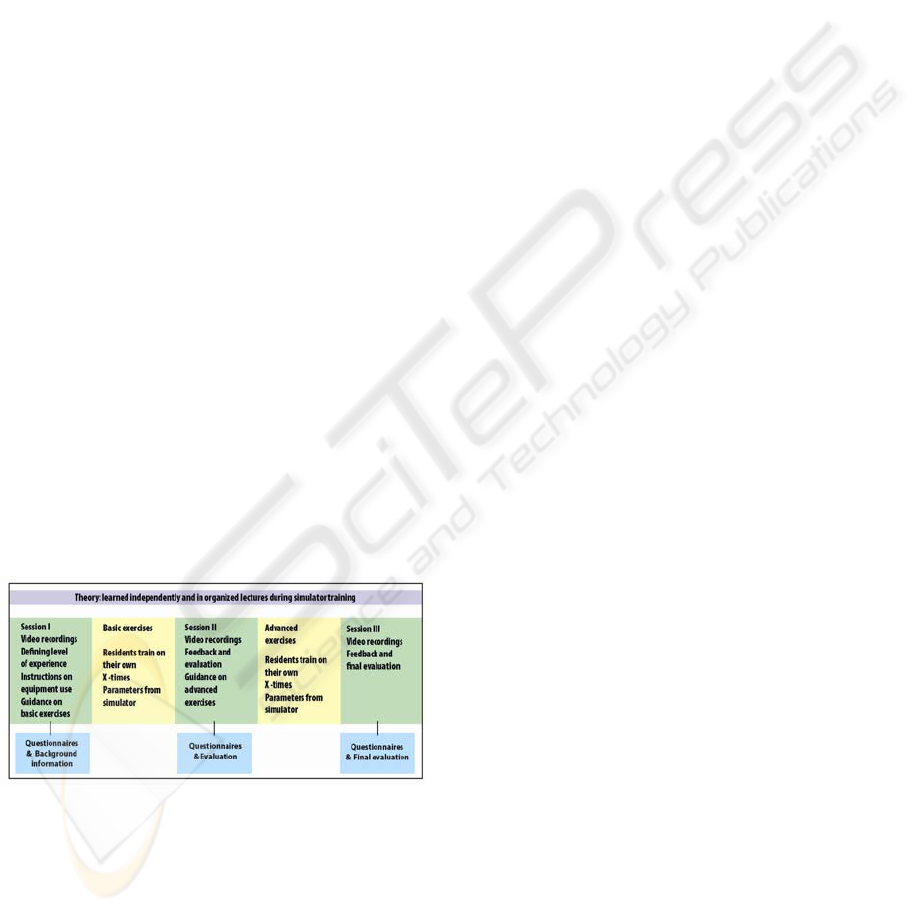
was experienced in simulator training. Figure 1
presents the structure of the simulator training,
including three videotaped training sessions and two
self-training periods.
Figure 1: The training program for surgical residents.
The training program has three instruction and
evaluation sessions in which both the specialist and
the resident surgeon are present. Simulator training
is seen as an element in surgical resident training,
where the overall aim is to integrate the learning of
theory and guided training within both authentic and
simulated environments. During independent
training, all the residents practise the same exercises
until they themselves are satisfied with their
performance.
Data was collected from the first part of the
training program (Session I), and also when the
participants made independent use of the basic skills
trainer (Basic Exercises). The research data consists
of background information on the surgical
specialists and residents, plus information
concerning skills training and exercises performed
with the simulator. This information was collected
via questionnaires. All the simulator exercise
parameters were measured automatically. The
parameters offer detailed information on the
surgeon’s performance, the amount of training, and
errors. The research subjects were all surgical
residents (N=19) who needed to practise their
laparoscopic skills. Three sessions (See Figure 1) in
which both specialist and resident surgeons
participated were videotaped. The video data was
collected with several cameras in order to get
detailed information on the events and actions
during the exercises.
4 THE AIM OF THE STUDY AND
THE RESEARCH QUESTIONS
The study focuses on the first part of the training
program, and the initial results of the residents’
training. We formulated the following research
questions:
1. What were the expectations of the residents at
the start of the training?
2. What is the relationship between motivation
and active participation in the training?
3. What is the relationship between one’s own
self-assessed skills and active participation in
the training?
4. What kind of constraints emerged regarding
participation?
5 RESULTS
The study investigated the main aspects of the
training in its early stage. These aspects include the
expectations and motivation of the participants, and
the resources they allocated to the training program.
An interesting aspect of the research was the self-
evaluated skills of the participants, and the amount
of practice that the participants put in.
COMPUTER-BASED SIMULATOR TRAINING IN THE HOSPITAL - A Structured Program for Surgical Residents
281
5.1 The Expectations and Motivation of
the Residents
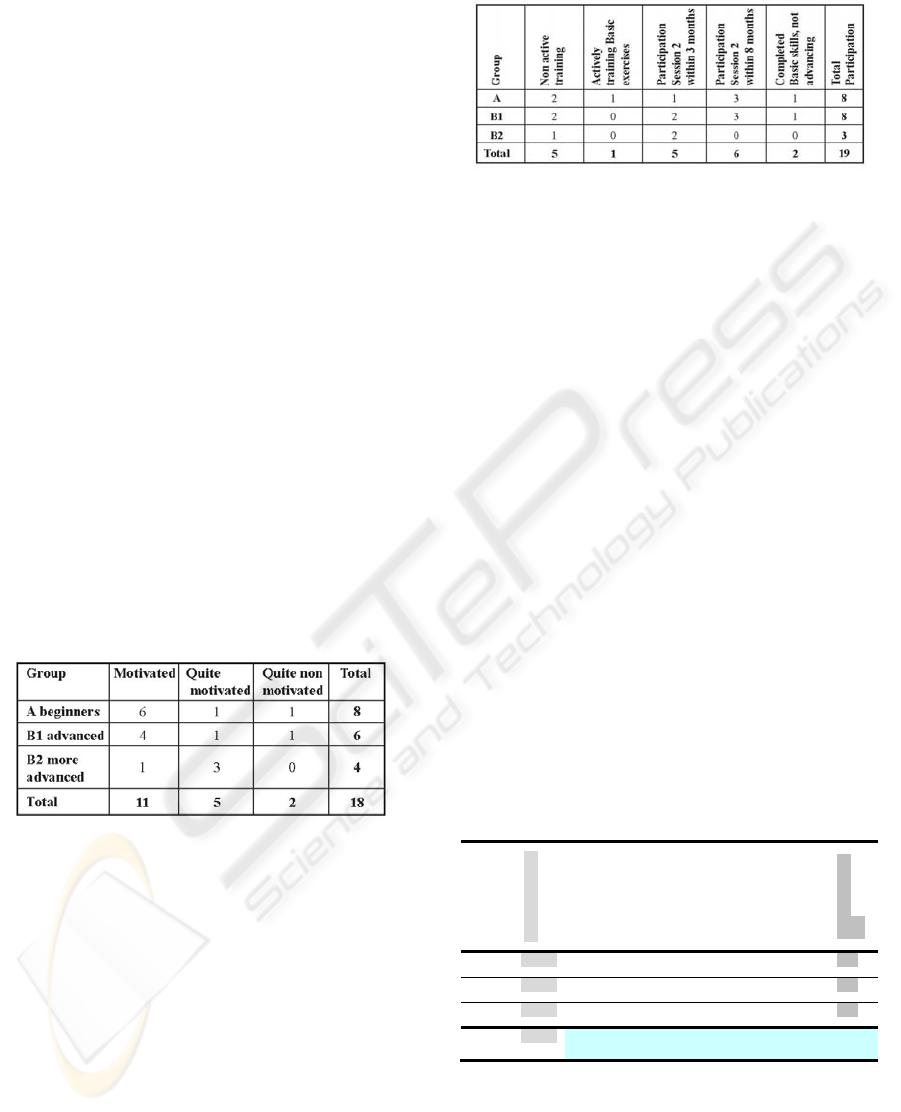
The trainees were divided into three groups
according to their level of experience. The beginners
(Group A) had just started their surgical resident
training in the hospital and were at an early stage in
their basic three-year training period. The advanced
trainees (Group B1) had done more than one year of
basic training. The more advanced trainees (Group
B2) had already completed three years basic of
training out of the total of six years resident training.
The expectations (N=17) of the residents
regarding the simulator training were obtained from
the questionnaire data. The less experienced
residents mostly expected to become better
acquainted with laparoscopic techniques and
instrument handling, and to adapt to the new surgical
technique. They also expected to be able to
comprehend a two-dimensional video picture while
they were operating. The more experienced trainees
mostly expected to achieve better dexterity and more
efficient hand-eye coordination. They further
expected to develop a routine in the procedure, and
to learn new procedures. Seventeen out of the total
of eighteen residents who answered agreed that
simulator training would be useful for them.
Table 1: Motivation to participate in training.
There were motivated trainees (see Table 1) in each
group. The majority (10/18) of the residents rated as
a demotivating factor future difficulty in finding the
time to practise with the simulator. However, there
was also a high rating (13/18) regarding the
possibility to practise with the simulator outside
normal working hours.
5.2 Levels of Participation and
Constraints
The findings regarding the training program were
based on the researcher’s experiences of the activity
of participants as well as on the questionnaires.
Table 2 summarizes the levels of active
participation.
Non-active training means that the resident
Table 2: Participation.
participated in Session 1, but thereafter did not
engage in independent practice with the simulator.
Participation problems were reported especially by
residents in Groups B1 and B2. The reasons for
cancellations and involvement problems were listed
by the researcher during the training, as follows: (1)
time problems; (2) problems (for both specialists and
residents) in sharing time for guidance sessions; (3)
a lack of motivation for participation among more
experienced residents. The reasons for cancelling
scheduled sessions were usually related to extra
workload situations in the clinic.
5.3 Skill Levels and Time Devoted to
the Training
Residents were given the freedom to train their skills
on the simulator without any upper or minimum
limit on their training times. They were only told to
practise until they felt confident and skilful in
performing the task. There were a total of five
different exercises within the Basic Exercises (see
Table 3). Table 3 shows the mean amount of time
(hours) spent by residents on each exercise. It also
shows the mean level of self-assessed laparoscopy
skill for each group, prior to starting the program.
Table 3: Residents skill level and practising times.
The most active trainees seemed to be the
experienced trainees from group B2. This group also
spent an almost equal amount of time on each
exercise. The residents from group A had less
participation in the more difficult exercises.
Groups
Skill level mean
Mean practice
time Exercise 1
Mean practice
time Exercise 1
Mean practice
time Exercise 1
Mean practice
time Exercise 1
Mean practice
time Exercise 1
Total practice
time
A 0.6 9.5 10.2 7.9 6.0 6.8 31.4
B1 1.6 9.4 6.8 8.0 6.8 7.4 38.4
B2 2.8 8.6 9.5 7.6 7.6 8.3 41.6
Total
mean
1.6 9.2 8.8 7.8 6.8 7.5 8.02
CSEDU 2009 - International Conference on Computer Supported Education
282

6 DISCUSSION
Simulator training is intended to aid surgical
residents in the efficient acquisition of good
operating skills. Since resident education tends not
to be very systematically organized in hospitals, new
training methods need to be adopted alongside
traditional ones. In this study simulator training had
a supplementary role within residents’ traditional
work-place learning; hence issues such as
participation and motivation were regarded as
crucial. Training with the simulator was a new and
for the most part unknown issue, for both the
specialist surgeons and the residents. The residents’
expectations were in line with studies mentioned
above, in which it was found that the simulator
seems to provide efficient training in aspects such as
depth perception and instrument control.
The motivation of the trainees was expected to
be lower when their experience level was higher.
Previous studies have recommended that simulator
training should be used at the novice stage of
training, due to anticipated higher motivation at this
stage, prior to the development of “negative
stereotypes” and incorrect practices (Ström et al.,
2002). The presumption was that groups B1 and B2
would be on the whole less motivated. One
unexpected finding in the present study was the
extent to which motivated trainees were present in
every group. There did seem to be more time
available for training at the early stage of residency.
Notwithstanding this, the motivation to train and
participate was not strictly dependent on the level of
the resident. Unmotivated residents did not take part
in the training at all, whereas those who participated
seemed to be committed to the training.
It had been anticipated that the residents would
actively participate in the guided training sessions,
and that they would also be willing to engage in
independent training within the times scheduled for
this. In fact, the levels of active participation of the
trainees emerged as roughly similar for each group,
with no decrease among residents with higher skill
levels. Almost all the participants seemed to be loyal
to the training program, and breaks in the training
were taken only for clearly valid reasons such as
maternity leave or transfer to another workplace.
The skills evaluations were consistent with the
level of experience of the trainees. The residents
evaluated their skills critically. Even if they had
performed operations independently on several
occasions, the skills were evaluated at no more than
4 in a scale of 1-10. The other hypothesis was that
self-assessment of the skill level would correspond
to the time spent on the simulator, and to the number
of training exercises carried out. In fact, what we
found was that the total hours of practice were
highest in group B2, i.e. among those residents who
already had the highest skill level; hence the causal
relationship between skills self-assessment and time
spent on the simulator could not be estimated
directly. One interesting observation concerned the
relationship between the times spent on training and
the difficulty level of the exercises (which increased
from Exercise 1 to Exercise 5). Group A (novices)
did less training on the more challenging tasks than
either group B1 or B2, who spent almost the same
time on all the exercises.
The differences between the times spent on the
tasks in each group could be explained according to
the likelihood that the more difficult tasks would
require more support and guidance in order to
succeed. Without such guidance, the less
experienced residents might well be deterred from
working through the more difficult exercises.
Whatever the reasons, the results do suggest that
self-training – without control of the amount of
training – may lead novice trainees to do merely the
same amount of practice, or even less, than more
experienced trainees. For this reason, the role of the
specialist surgeon (as both evaluator and instructor)
should be taken into account, as an essential element
in the training – even if residents can arrive at a
fairly objective evaluation of their own skills.
Previous studies, too (Kneebone, 2003), have
highlighted the importance of the teaching skills of
senior surgeons as part of simulator training. In our
study, no clear relationship was found between
motivation and active participation, however the
groups that trained most actively seemed to be
slightly more motivated, if we consider that in
Group B2 no participants fell into the “fairly non-
motivated” category.
Surgical training seems to be approaching its
outer limits, bearing in mind that no one knows what
the alternative to traditional education might be.
Over many decades, traditional training has become
incorporated within the everyday routines of
hospitals. Incorporating surgical simulator training
within normal hospital protocols is a demanding and
complex matter. It needs much more basic,
longitudinal research, since the innovations in
training methods that are clearly needed should be
based on real knowledge. There seems little doubt
that simulation has its place as a component in the
training of surgeons, provided that it supports and is
supported by research, technology, clinical practice,
professionalism and education.
COMPUTER-BASED SIMULATOR TRAINING IN THE HOSPITAL - A Structured Program for Surgical Residents
283

7 CONCLUSIONS
The study shows that it is possible to run a guided
and structured simulator training program in a
hospital where the primary task is patient care. The
surgical residents feel positive about simulator
training and wish to intensify and improve their
skills with it. Those who start the training program
seem to remain loyal to it. However, the study
suggests that simulator training needs to be fully
structured – and even mandatory – in order to get all
the residents involved in the training. An effective
and motivating training program necessitates intense
commitment from all the participants, including the
supervisors. Further study is required concerning
problematic features such as time allocation and the
commitment of residents, and the factors involved in
providing adequate supervision and support. The
next logical step would be the analysis of video-
recorded training sessions. The main challenges
seem to involve adapting new methods into hospital
routines, and creating a new learning/teaching
culture within the hospital setting.
REFERENCES
Ahlberg, G., Heikkinen, T., Iselius, L., 2006. Does
training in a virtual reality simulator improve surgical
performance? Surg. Endosc.16;126–129.
Ahlberg, G., Kruuna, O., Leijonmarck, C., Ovaska, J.,
Rosseland, A., Sandbu, R., Strömberg, C., Arvidsson,
D. 2005. Is the learning curve for laparoscopic
fundoplication determined by the teacher or the pupil?
The Am.J Surg. 189; 184-189.
Berguer, R., Forkey, D. L., Smith, W. D. 2000. The effect
of laparoscopic instrument working angle on surgeons'
upper extremity workload. Surg. Endosc. 15; 1027–
1029.
Brydges, R., Carnahan, H., Dubrowski, A. 2005. Surface
exploration using laparoscopic surgical instruments:
The perception of surface roughness. Ergonomics, 48;
874-894.
Cosman, P.H., Cregan, P.C., Martin, C.J., Cartmill, J.A.
2002. Virtual reality simulators: Current status in
acquisition and assessment of surgical skills. ANZ
Journal of Surgery. 72;30-34.
Conrad, J., Shah, A.H., Divino, C.M., Schluender, S.,
Gurland, B., Shlasko, E., Szold, A. 2006. The role of
mental rotation and memory scanning on the
performance of laparoscopic skills. Surg. Endosc.
20;504-510.
Feldman, L. 2004. Using simulators to assess laparoscopic
competence: ready for widespread use? Surgery.
135;28 – 42.
Gallagher, A.G., Satava, R.M. 2002.Virtual reality as a
metric for the assessment of laparoscopic psychomotor
skills. Surg. Endosc. 16;1746-1752.
Jordan, J.A., Gallagher, A.G., McGuigan, J., McClure, N.
2000. Virtual reality training leads to faster adaptation
to the novel psychomotor restrictions encountered by
laparoscopic surgeons. Surg. Endosc. 15;1080-1084.
Kneebone, R. 2003. Simulation in surgical training:
educational issues and practical implications. Med.
Educ. 37:267-277.
Madan, A. K., Frantzides, C. T., Park, W. C., Tebbit, C.
L., Kumari, N. V. A., O Leary, P. J. 2005. Predicting
baseline laparoscopic surgery skills. Surg.
Endosc.19;101–104.
Poulin, E.C., Gagne, J.P., Boushey, R.P. 2006. Advanced
laparoscopic skills acquisition: The case of
laparoscopic colorectal surgery. Surg Clin N Am.
86;987-1004.
Reznick, K. & MacRae, H. 2006. Teaching surgical skills
–Changes in the Wind. NEJM. 355;2664-2669.
Soper, N, J., Brunt, L. M., Kerbl, K. 1994. Laparoscopic
General Surgery. NEJM. 6;409-419.
Schjiven, M.P., Jakimowicz, J.J., Broeders, I.A., Tseng,
L.N. 2005. The Eindhoven laparoscopic
cholecystectomy training course-improving operating
room performance using virtual reality training. Surg.
Endosc.19;1220-1226.
Ström, P., Kjellin, A., Hedman, L., Johnson, E.,
Wredmark, T., Felländer-Tsai, L. 2002. Validation
and learning in the Procedius KSA virtual reality
surgical simulator: Implementing a new safety culture
in medical school. Surg. Endosc.17;227-231.
Villegas, L., Schneider, B.E., Callery, M.P., Jones, D.B.
2003. Laparoscopic skills training. Surg. Endosc. 17;
1879–1888.
CSEDU 2009 - International Conference on Computer Supported Education
284
