
STUDY OF CLINICAL WORKFLOW AND INFORMATION
FLOW OF A BREAST CARE UNIT
Vítor Silva
1
, Maria João Cardoso
2
, João Fonseca
3
and Ricardo Cruz-Correia
3
1
Magnetic Resonance Department, Hospital São João, Oporto, Portugal
Center for Research in Health Technologies and Information Systems (CINTESIS), Portugal
2
Breast Center, Hospital São João, Oporto, Portugal
INESC, Breast Research Group, Portugal
Faculdade de Medicina da Universidade do Porto (FMUP), Oporto, Portugal
3
Center for Research in Health Technologies and Information Systems (CINTESIS), Portugal
Faculdade de Medicina da Universidade do Porto (FMUP), Oporto, Portugal
Keywords: Clinical protocols, Information flows, Processes, Breast diseases, Hospital communication systems.
Abstract: Introduction. The study of the clinical workflows and information flows in healthcare institutions is of vital
importance to improve its effectiveness and efficiency. At Hospital São João, Oporto – Portugal, a
Diagnostic Breast Unit (DBU) was recently created. The implementation of a new Electronic Patient Record
(EPR) called Breast.Care triggered the need to better understand the DBU processes and suggest
improvements. Aim. To describe clinical workflows and information flows in DBU, detect problems and
propose solutions for better communication among different actors. Methods. The study started with a direct
observation period with a total of 24 hours. The observed processes and flows were transcribed into free text
and then into structured text, tables and Unified Modeling Language (UML) diagrams (activity and
partition-activity). The structured text and diagrams were analysed to find possible improvements. Results.
Seven main processes were identified representing how different actors (humans and computers) work
together. Three communication process improvements between humans were detected (e.g. changing timing
of patient data insertion to facilitate reading access to others), three human–machine improvements (e.g.
changing computer medical forms) and one between machines (creating specific links between information
systems). Discussion. Analysing workflow and information flow in DBU allowed the detection of
communication problems and the improvement of those through changes in EPR and in DBU current
processes.
1 INTRODUCTION
The Diagnostic Breast Unit (DBU), a part of the
Hospital Breast Center was created to improve
health care delivery to patients with breast problems
at Hospital São João (HSJ). A team of experts on
breast diseases work together in the Unit optimizing
the diagnosis of breast problems. The Unit provides
an integrated monitoring of patients, creates greater
comfort and prevents increase of hospital patient’s
visits, greatly reducing the waiting time to diagnosis.
This unit aims at being credited by the European
Society of Mastology (EUSOMA) and therefore
meets all the requirements needed. As a new unit
within the community hospital and having their own
team of experts, problems and difficulties on
communication and information flow patterns with
the “outside world”, including other hospital
departments, are to be expected.
Managing the diversity of medical data and its
communication in DBU, is not an easy task, due to
the existence of many heterogeneous processes.
Understanding those processes, workflows and its
information flows is of vital importance to improve
its effectiveness and efficiency. Currently, most of
clinical data are handled by software applications,
which are known to become the engine of data
management (Keizer 2005) (Oroviogoicoechea
2007).
Often the terms process and workflow are used
as synonyms or side by side without any distinctive
differences (Knolmayer 2000) (Reijers 2003). In
294
Silva V., João Cardoso M., Fonseca J. and Cruz-Correia R. (2010).
STUDY OF CLINICAL WORKFLOW AND INFORMATION FLOW OF A BREAST CARE UNIT.
In Proceedings of the Third International Conference on Health Informatics, pages 294-301
DOI: 10.5220/0002744502940301
Copyright
c
SciTePress

this paper, the following definitions will be used: a)
Process - a way for an enterprise to organize work
and resources (people, equipment, information,
computer applications, etc.) to accomplish its aims.
Nowadays, organizations try to arrange work and
resources to achieve a specific output – a result – for
a specific costumer. It can be simply defined as a
collection of interrelated work tasks, initiated in
response to an event, that achieve a specific result
for the process’ costumer (Sharp 2001); b)
Workflow
- simply refers to tasks, resources and
triggers associated with a specific process. It is
dependent on the process and contains the sequence
of tasks and information about data and facilities the
execution of functions (Becker 1999); c)
Information flow
- can be defined as a serie of
successive events, between the generation of
information from a source of information and
acceptance by a receiver. It is designed to promote
some kind of change (Silva 2008). With the advance
of information technologies, information flows tend
to be a multifocal and multioriented. All
organizations need systematic and consistent efforts
to influence and monitor all their information flow
by promoting strategies for that purpose (Krovi
2003). The retrieve of information flow is essential
to recognize its efficiency (Jacoski 2005).
Numerous authors have discussed the theoretical
benefits of a well established clinical workflow
(Duitshof 1995; Holland 2006; Becker 2007;
Malhotra 2007). It leads to detailed, organized,
formalized, communicated, managed and
streamlined processes. The workflow becomes clear
and potentiates process efficiency, better
organization, improved quality and better
identification and characterization of possible
medical errors (Becker 2007; Malhotra 2007; Peleg
2007).
In healthcare today we are faced with the
problem of departmental applications that support
specific functions and limited workflow. Most of the
data captured by these systems reside within the
application and are not easily retrieved and made
available to other processes that may require them
(Berg 1999; Nielsen 2000; Lorenzi 2003).
Delivering healthcare today is a complex task
often undertaken by multidisciplinary teams, whit
the obvious output of a great amount of information.
Additionally organizations have complex
infrastructures with poor communication between
different departments and staff. To optimize
operational efficiencies they require means to
automate and manage these processes making sure
that the right information is made available to the
right individual at the right time. An established
workflow can support such care processes by
executing agreed models of care (Berg 1999;
Nielsen 2000; Lorenzi 2003).
For information management and
communication with other healthcare institutions
(e.g. hospitals or primary care) and other hospital
departments (e.g. radiology or pathology), DBU
uses the following computer applications: a)
SONHO – the ADT (Admission-Transfer-
Discharge) system of the hospital, which
manipulates administrative data (e.g. demographic
patients’ data); b) SAM (Portuguese initials for
Medical Support System) - the outpatient medical
scheduling system and multipurpose hospital
patient; c) Siima (Portuguese initials for Clinical
Imaging Management System) - the imaging system
responsible for the record and visualizing of
mammography and ultrasound exams at DBU; d)
Breast.Care - a specific departmental electronic
patient record built for the DBU, to record and
analyse clinical data from patients with breast
problems; and e) Alert P1 – a system that receives
requests for consultation from primary care
physicians (this system is not available on DBU).
All described applications help in the integration
of outside and inside information contributing to
improve its efficiency and effectiveness
(Ammenwerth 2004; Keizer 2005).
2 AIM
To describe and analyse clinical workflows and
information flows in DBU, detect problems in the
system and propose solutions for better
communication among different actors, thereby
trying to improve performance.
3 METHODS
Study Design. This study was undertaken in
different days totalising a 24 hours period of
participant, direct and semi-structured observation
during January 2009.
Study Participants. Participants were all potencial
users of computer applications existing in the DBU.
Data Method Collection. The main data collection
method used was direct observation. This method
allowed a thorough analysis of clinical workflows
and information flows between different actors.
STUDY OF CLINICAL WORKFLOW AND INFORMATION FLOW OF A BREAST CARE UNIT
295
During a 24 hours period, one researcher (the
first author of this paper) observed interactions,
information flow, clinical workflow and processes
between different actors, in different offices
(consultation rooms, waiting rooms, main reception
areas, and technical work areas). Information was
gathered while shadowing study participants. During
this process, open-ended questions were asked to
develop insights about how events happened,
experienced and reported. In this phase extensive
field notes were collected.
Variables Description. Free-text was used to
extract the following variables: i) local of
observation; ii) actors observed; iii) stage of clinical
workflow; iv) software applications used.
Data Analysis. Data were collected through
observation method with field notes. The gathered
notes were then passed into structured text to allow
better analysis and comprehension. That structured
text described and analysed the different clinical
workflows and information flows in DBU. UML
diagrams, like activity and partition activity
diagrams, and tables were used and constructed.
4 RESULTS
We identified various types of clinical processes
(n=7) with different actors and corresponding
workflow (Table 1). Data about, where, how and
when they occurred was registered. Multiple actors
were present in all processes.
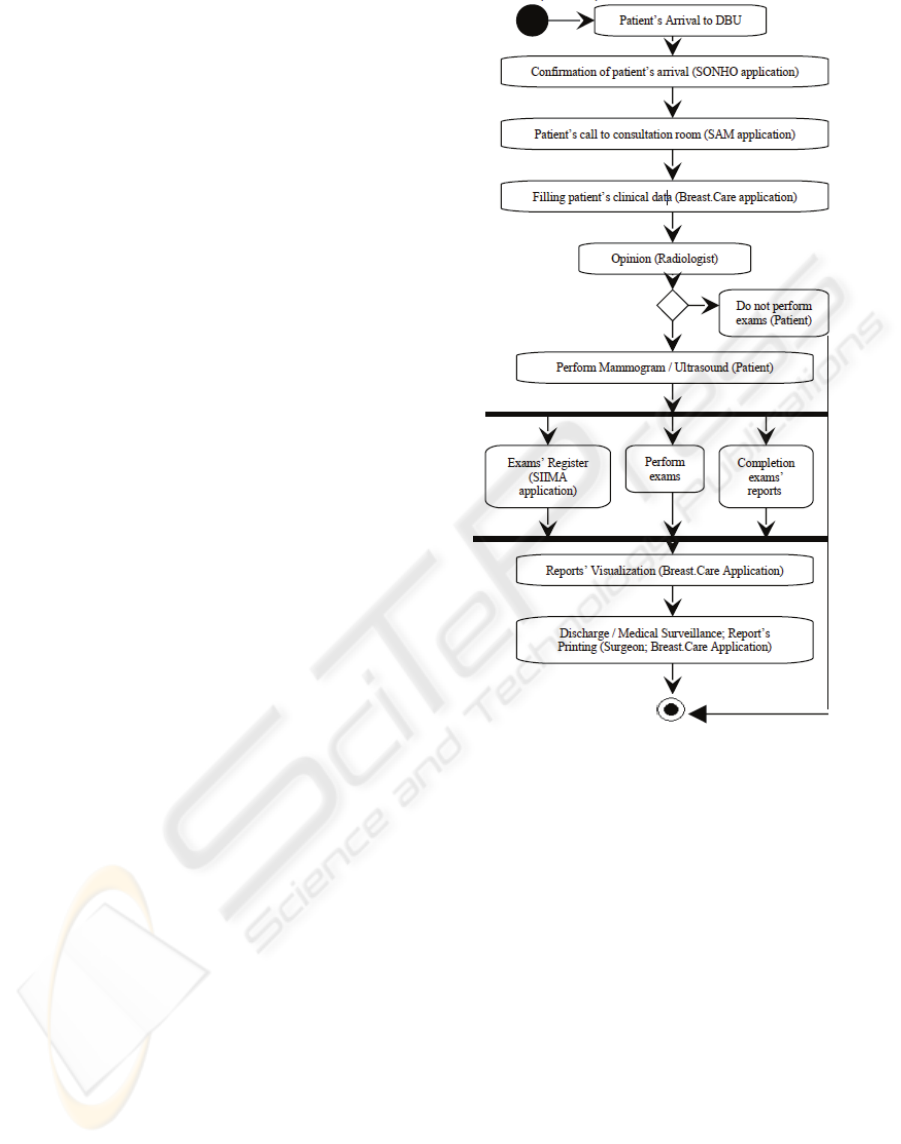
UML diagrams were used to analyse and
illustrate all processes. As an example, Figure 1
represents an activity diagram of Process I described
on Table 1. Table 2 shows the different types of
information flows that exist in the DBU. To clarify
some existing information flow described above, we
used UML partition activity diagrams. The first
partition diagram (see Figure 2) describes when the
surgeon goes directly to the radiologist to know his
opinion about a patient’s case (communication
between humans). The second diagram (see Figure
3) is related to radiologist performing examination
reports in Breast.Care application and copying and
pasting them to SIIMA application (communication
between humans and computers). After analysing
the processes, we have detected several possible
improvements to information flows. Improvements
were grouped together based on the type of actors
involved (Table 3).
Figure 1: UML activity diagram of Process I (Table 1) -
Patients (first consultation), do not perform invasive
exams and are discharged from the Unit in the same day.
Figure 1 is an activity UML diagram that is
recognized as the most suitable for modeling the
functional vision of a system, because describes the
logic of procedures or duties(Silva 2005).
These two tables show the most important clinical
workflows and information flows that occur in
DBU. Table 1 has seven processes with all
description, the different actors involved and how,
where and when they interact. Table 2 shows some
information flows associated to clinical workflows
and processes described on table 1, describing all
information flow and the sequence of actors.
Figures 2 and 3 show two UML partition activity
diagrams, which include division lines (called swim
lanes), that describe in greater detail and specificity
certain classes or subsystems, in this case actors
during information flows.
HEALTHINF 2010 - International Conference on Health Informatics
296
Table 1: Description of the different processes in DBU.
N Description Actors How Where When
I Patients
(first
consultation)
do not
perform
invasive
exams and
are
discharged
from DBU
same visit.
Patient,
Administra
tive staff,
Surgeon,
Radiologist
,
Radiograph
er
Patient arrives at DBU, gives all documents to administrative
staff, who confirms the patient’s arrival on SONHO application.
Reception Patient’s
arrival
Surgeon, through SAM application, confirms arrival and calls
patient to consultation room. Next he starts Breast.Care
application to introduce demographic and clinical data. Surgeon
performs clinical breast exam on patient.
Consultation
Room
Surgeon’s
interview
and exam
Surgeon observation of patients previous imaging exams.
Discussion and observation of exams with Unit Radiologist.
Lecture
Room
After
consultation
Radiologist could have two opinions: i) the patient doesn’t need to
perform any exam and is discharged from consultation; ii) patient
needs to perform some extra non-invasive diagnostic exams,
which will be reported through Breast.Care application.
Imaging
Rooms
At imaging
Patient is informed by surgeon of normal or benign results.
Discharge and reference to attending physician.
Consultation
Room
End of
consultation
I
I
Patients
perform
invasive
studies
(breast
biopsy) and
have a
subsequent
visit for
results.
Patient,
Administra
tive staff,
Surgeon,
Radiologist
,
Radiograph
er,
Pathologist
Similar to first 3 steps of process I. Reception,
Consultation
Room
Patient’s
arrival, at
consultation
A guided breast biopsy (imaging rooms) and a histological exam
will be undertaken (pathology department).
Imaging
Rooms
Pathology
Department
At imaging
At pathology
after
specimen
prepared
Patient informed of another visit date for results by the
administrative staff.
Consultation
Room
At
consultation
I
I
I
Patients
come to be
informed of
biopsy
result.
Surgeon,
Patient
The biopsy’s result can be benign (with or without surgery) or
malignant (surgery or primary non surgical treatments). If results
are benign, patients may be discharged from consultation and be
followed by attending physician. In some cases, surgery is advised
or desired.
Consultation
Room
At
consultation
I
V
Patients
scheduled
for surgical
intervention.
Surgeon,
Patient
All these patients must have a surgery scheduled in SAM
application (national waiting list). In some cases where primary
treatment is decided before surgery patient must be referred to
oncologist. Surgery is schedulled subsequentially (7 months later).
Consultation
Room
At
consultation
V Patients who
are referred
for a
Genetics
consultation.
Surgeon,
Patient,
Nurse in
charge of
genetics
consultatio
n
Patients, who have high risk for breast cancer (e.g. family
history), are referred to Genetics consultation in DBU, which
currently only occurs on Fridays. Surgeon refers those patients
directly to nurse in charge of genetics appointments.
Consultation
Room
DBU
At
consultation
V
I
Patients who
will be
followed in
DBU
(patients
with breast
cancer that
have already
been treated)
Surgeon,
Patient,
Administra
tive staff
Patient arrives to DBU, gives and the administrative confirms the
patient’s arrival on SONHO application.
Reception Patient’s
arrival
Surgeon, through the SAM application, sees that the patient has
arrived and calls him into consultation room. A clinical
questionnaire and physical examination completes patient’s
clinical data into the Breast.Care application. Patients are referred
for an outpatient consultation in HSJ. The surgeon usually uses
SAM application to record and print drugs prescription.
Consultation
Room
At
consultation
V
I
I
Diagnosis
Multidiscipli
nary Team
Meeting
Surgeon,
Radiologist
,
Pathologist
All cases of patients who were submitted to biopsy are discussed
in a diagnosis multidisciplinary team meeting.
Lecture
Room
Periodically,
proportional
to number of
biopsies
STUDY OF CLINICAL WORKFLOW AND INFORMATION FLOW OF A BREAST CARE UNIT
297
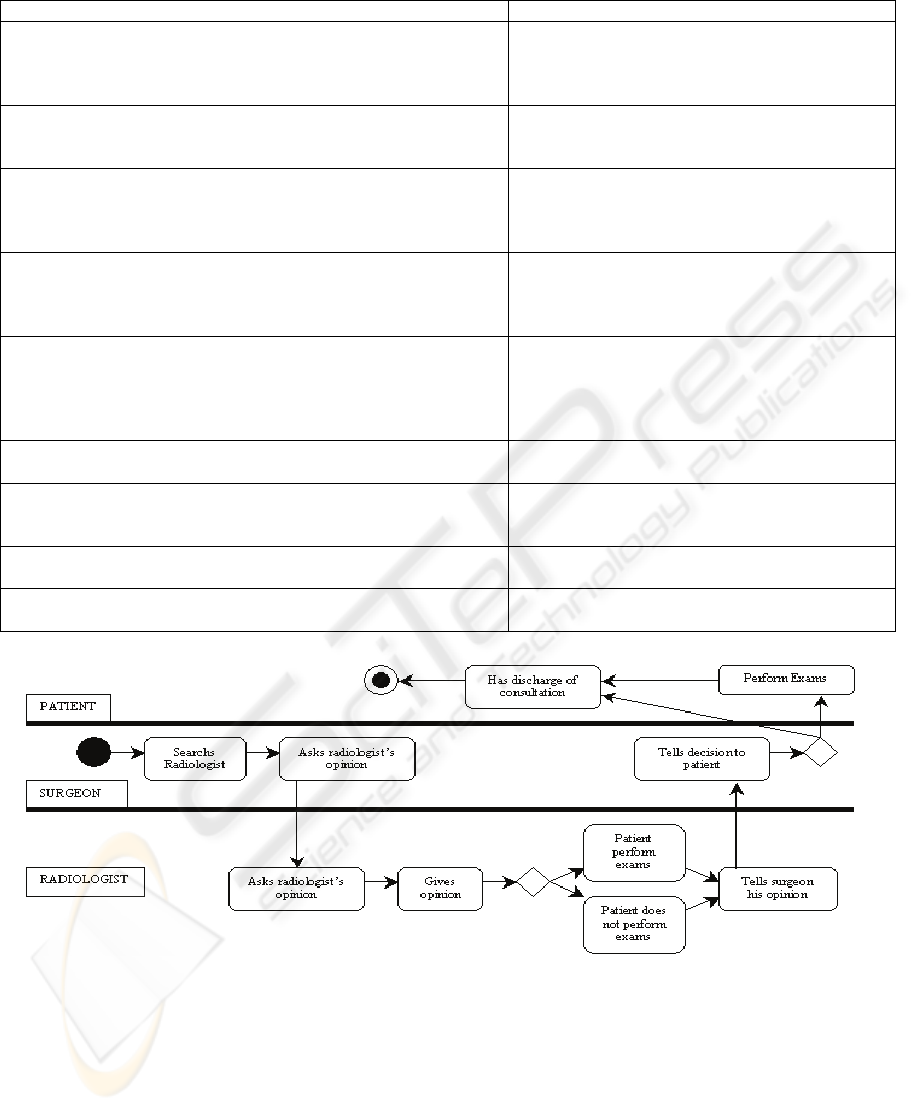
Table 2: Different types of information flow and actors that exist in DBU.
Information Flow Actors
Surgeon searchs and requests, directly and personally, radiologist
opinion about patient case. Radiologist reads patient’s exams and
informs surgeon. Surgeon informs patient (to perform or not to
further exams).
Surgeon → Radiologist → Surgeon → Patient
Patient is referred to genetics consultation. Surgeon refers patient
directly to nurse in charge of those consultations, who makes an
appointment. Patient will receive notification at home.
Surgeon → Patient → Nurse → Patient
Patients need to perform a breast MRI (Magnetic Ressonance
Imaging) to better characterize or stage the lesion. Surgeon informs
patient of the decision and requests exam at SAM application. MRI
unit receives that request, appoints it and notifies patient.
Surgeon → Patient → MRI Unit → Patient
Patient has benign breast disease and no need for further
intervention she will be referred to her attending physician.
Surgeon informs patient of decision and prints a report that will be
delivered by hand to attending physician.
Surgeon → Patient → Attending Physician
Majority of requests for first appointment in DBU are requested by
Alert P1 (system is not available directly in DBU). Surgeon in
charge prints breast referrals from general surgery department and
brings them to DBU. A classification of urgent, medium and non-
urgent priority is done based on attending physician information.
Surgeon → Surgery Unit → Surgeon
(Requests)
Radiographer knows of patient arrival, when personally warned by
administrative staff.
Patient → Administrative → Radiographer
During consultation, surgeon fills data relative to that episode in
Breast.Care application. It will create a PDF document with this
data in SAM application.
Surgeon → Breast.Care Application → SAM
Application
Radiologist has to copy and paste imaging reports in Breast.Care
application to SIIMA application.
Radiologist → Breast.Care Application → SIIMA
Application
Administrative staff takes patient information on printed sheets to
surgeon.
Administrative (information in paper) → Surgeon
Figure 2: Partition Activity Diagram of an information flow in which the surgeon goes personally to know the radiologist’s
opinion about a patient.
HEALTHINF 2010 - International Conference on Health Informatics
298
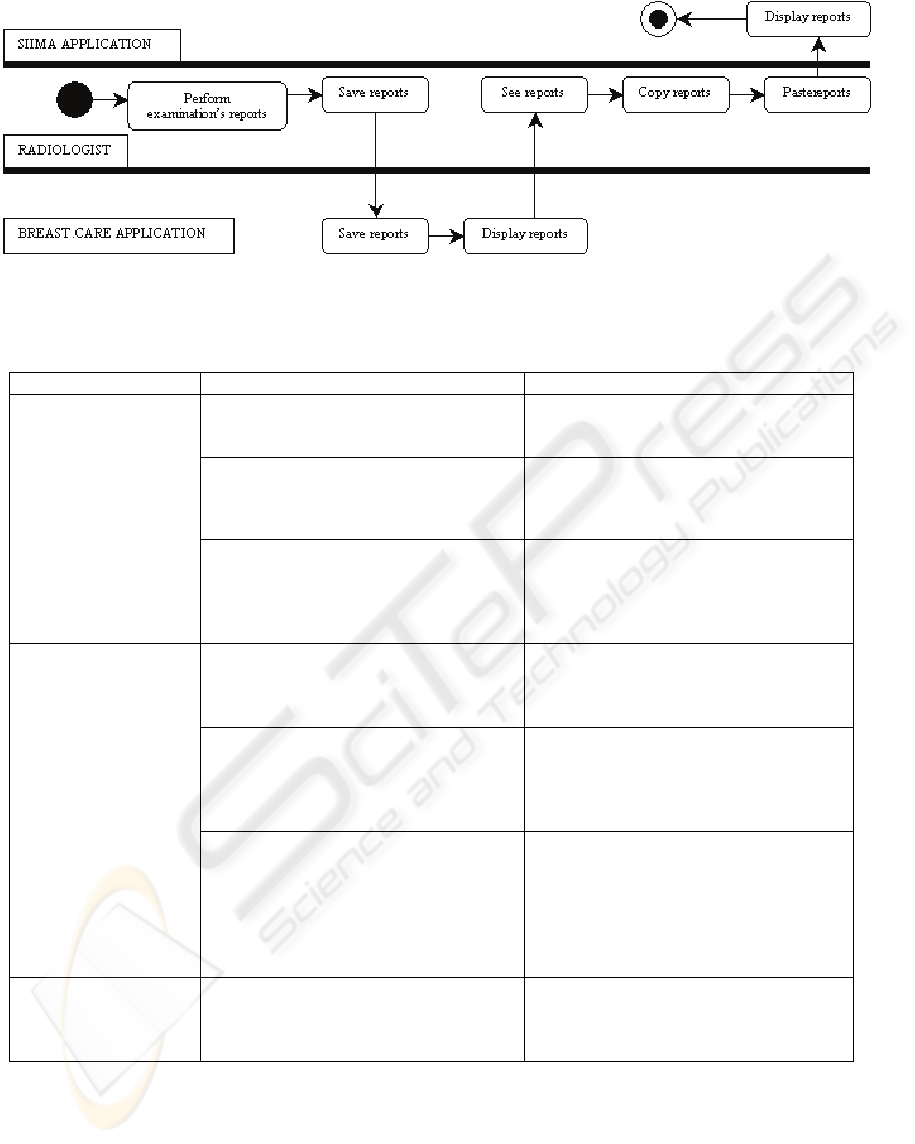
Figure 3: Partition Activity Diagram of an information flow in which the radiologist fills the report in Breast.Care
application and has to copy and paste that report to another computer application (SIIMA).
Table 3: Suggested Improvements on communication processes.
Current Suggested Improvement
Communication
between humans
Normally information related to patient is
printed to attending physician.
Deliver all patient information in
electronic format through one of the
currently available systems.
Radiographer only knows of patient
arrival to DBU when administrative staff
warns him personally.
Administrative staff could insert a
patient’s arrival hour at DBU, in SIIMA
application.
Surgeon has to search and ask, personally
radiologist’s opinion about a patient’s
case.
Surgeon’s clinical evaluation is reported
in Breast.Care, Radiologist could access
all abstract and patient’s exam over the
same application. Radiologist would write
his report back in Breast.Care.
Communication
between human-
machine
Alert P1 system is not available in DBU. Information on Alert P1 system should be
available to DBU users. This would avoid
going to another department and also
avoid printing requests.
Surgeon has to print reports to patient.
He has to go to reception room to get
those reports.
Some printers could be available in some
key-places, like in consultation rooms.
Printed reports could be mailed in
envelopes by administrative staff to
handle to patients on their way out.
Surgeons filling Breast.Care forms using
free text components.
Implement sctrutured forms that force a
logical sequential order (according to
consultation progress).
This modification in the software was
suggested to Breast.Care development
team and it is already implemented in
DBU.
Communication
between machines
(Integration of IS)
Radiologist has to copy and paste all
examination reports from Breast.Care to
SIIMA application.
A link should be available in Breast.Care
application connecting it to SIIMA
application.
STUDY OF CLINICAL WORKFLOW AND INFORMATION FLOW OF A BREAST CARE UNIT
299

5 DISCUSSION
This method allowed detailed description of
workflows and information flows, and also the
detection of communication problems, suggesting
some improvements. We feel that this methods
when properly applyed provide useful results for
improvement of information flow. With good
observational methods, we can also identify
appropriate and inappropriate patterns of
communication (Caris-Verhallen 2004; Unertl
K.M. 2006; Ash 2007). Through this method, we
can analyse various information flows in a health
unit, in order to develop general models of
workflow for the improvement of process
automation (Unertl K.M. 2006).
This study identified many processes involved
in the unit that showed the high diversity and
quantity of information that staff and computer
applications deal with. This fact reinforces the
need for well established clinical workflows and
information flows, in order to provide better
healthcare.
With suggested improvements, costs could be
reduced (e.g. reducing the need to print in paper)
and also additional time spared (e.g. the time
needed for the radiologist to fill the examination
reports in SIIMA and Breast.care software
applications). Simple information flows would
allow also avoid unnecessary participant travels
between rooms.
With observation method, authors were able to
see how doctors filled patients’ data into
Breast.Care application and thereby suggest some
changes. Based on those suggestions, Breast.Care
development team created a sequential method to
enter patients’ data in Breast.Care. This change
affected positively DBU doctors’ team, by
fastening data entering into the application.
Future research will use other methods of data
collection, like interviews and focus groups and
computer systems log analysis, aiming at enriching
the quality and quantity of data, and enable a
process of triangulation when analysis the
processes of the DBU (Bottorf 1993; Hewinson
1995; Ash 2007; Lessard-Hébert 2008).
ACKNOWLEDGEMENTS
We are grateful to all DBU staff for all the help
and availability provided.
REFERENCES
Ammenwerth, E., Brender J., Nykanen P., Prokosch HU,
Rigby M., Talmon J. (2004). "Visions and strategies to
improve evaluation of health information systems.
Reflections and lessons based on the HIS-EVAL
workshop in Innsbruck." International Journal of
Medical Informatics 73: 479-491.0
Ash, J., Guappone, K. (2007). "Qualitative evaluation of
health information exchange efforts." Journal of
Biomedical Informatics 40: S33-S39.
Becker, J., Jamiesch, C. (2007). Resctrictions in Process
Design: A Case Study on Workflows in Healthcare. 5th
International Conference on BPM, Australia.
Becker, J., zur Mulhen, M. (1999). Towards a Classification
Framework for Application Granularity in Workflow
Management Systems. Proc. 11th International
Conference on Advanced Information Systems
Engineering (CAiSE).
Berg, M. (1999). "Patient care systems and healthcare work:
a socialtechnical approach." Int J.Med.Inf. 55: 87-101.
Bottorf, J. L. (1993). "The use and meaning of touch in
caring for patients with cancer." Oncol Nurs Fórum 20:
1531-8.
Caris-Verhallen, W., Timmermans, L., van Dulmen, S.
(2004). "Observation of nurse-patient interaction in
oncoloy: review of assessment instruments." Patient
Education and Counseling 54: 307-320.
Duitshof, M. (1995). Workflow Automationin Three
Administrative Organizations. Department of Computer
Science – Section Information Systems. Twente,
University of Twente - The Netherlands. Masther's
Thesis.
Hewinson, A. (1995). "Nurses’ power in interactions with
patients." J Adv Nurs 1995 21: 75-82.
Holland, M., Young, J. (2006). "Improving clinical
workflow through effective context and identity
management." Health Industry Insights.
Jacoski, C. (2005). Peculiaridades do fluxo de informações
em pequenos escritórios de projeto de edificações. V
Workshop Brasileiro da Gestão do Processo na
Construção de Edifícios, Brazil.
Keizer, N., Ammenwerth, E. (2005). "The effects and
quality of IT evaluation studies: Trends in 1982-2002."
AMIA Annu Symp Proc.: 186-90.
Knolmayer, G., Endl, R., Pfahrer, M. (2000). Guidelines for
Business Process Modeling. Business Process
References 315 Management. Berlin, Springer-Verlag.
1806: 16-29.
Krovi, R., Chandra, A., Rajagolapan, B. (2003).
"Information Flow Parameters for Managing
Organizational Processes." Communications of the
ACM 18(3): 286-292.
Lessard-Hébert, M., Goyette, G., Boutin, G. (2008).
Investigação Qualitativa Fundamentos e Práticas,
Instituto Piaget.
Lorenzi, N., Riley, R. (2003). "Organizational issues =
changes." International Journal of Medical Informatics
69: 197-203.
HEALTHINF 2010 - International Conference on Health Informatics
300

Malhotra, S., Jordan, D., Shortliffe, E., Patel, V. (2007).
"Workflow modelling in critical care: Piecing
together your own puzzle." Journal of Biomedical
Informatics 40(2): 81-92.
Nielsen, P., Thomson, B., Jackson, R., Kosman, K.,
Kiley, K. (2000). "Standard Obstetric Record
Charting System: Evaluation of a New Electronic
Medical Record." Obstet & Gynecol 96: 1003-8.
Oroviogoicoechea, C., Elliott, B., Watson, R. (2007).
"Review: evaluating information systems in
nursing." J Clin Nurs. 17: 567-575.
Peleg, M. (2007). Guidelines and Workflow Models.
Clinical Decision Support, The Road Ahead: 281-
306.
Reijers, H. (2003). Design and Control of Workflow
Processes. Germany, Springer.
Sharp, A., McDermott, P. (2001). Workflow Modelling
– Tools for Process Improvement and Application
Development. London, Artech House.
Silva, A., Videira, C. (2005). UML Metodologias e
Ferramentas CASE. Portugal, CentroAtlantico.PT.
Silva, J., Oliveira, A., Costa, J.A., Lima, J.E., Penha, R.
(2008). Fluxo da Informação, a partir dos
prontuários, para a gestão das organizações em
saúde: um estudo de Caso na Liga Norte
Riograndense Contra o Câncer. XI SEMEAD –
Seminários em Administração FEA-USP, Brazil.
Unertl K.M., W. M. B., Johnson K.B. (2006). Applying
Direct Observation to Model Workflow and Assess
Adoption. AMIA 2006 Symposium Proceedings.
STUDY OF CLINICAL WORKFLOW AND INFORMATION FLOW OF A BREAST CARE UNIT
301
