
DESIGNING
A PHYSICIAN-FRIENDLY INTERFACE FOR AN
ELECTRONIC MEDICAL RECORD SYSTEM
Donald Craig and Gerard Farrell
eHealth Research Unit, Faculty of Medicine, Memorial University of Newfoundland, St. John’s, Canada
Keywords:
Electronic health record, User interface design, Data visualization, Physician workflow, Knowledge manage-
ment, Usability, Medical chart.
Abstract:
An Electronic Medical Record (EMR) system enables a physician to record patients’ health information, re-
quest reports from third partly health care providers and retrieve these reports when they are ready. Despite
the numerous benefits of EMRs, several factors have inhibited their widespread adoption. An underappreci-
ated but critical factor has been the proliferation of inferior user interfaces which are confusing to navigate
and disruptive to a physician’s workflow. To be useful, an EMR must allow physicians to record and query
information in a natural manner that accommodates the non-linear nature of their workflow. In particular,
an interface must permit a physician to record the minutiae of a patient’s condition while at the same time
preserving the physician’s overview of a patient’s record so that any aspect of the patient’s health can be ef-
fortlessly queried and inspected. This paper proposes an interface design that attempts to address several of
the usability deficiencies associated with current electronic medical record systems in use today.
1 INTRODUCTION
Electronic Medical Record (EMR) systems (Carter,
2008) are providing an increasingly viable mecha-
nism for physicians to record and retrieve patient re-
lated information. The potential benefits of such sys-
tems are well documented in the literature: a properly
designed EMR can help reduce medical errors, en-
hance communication between physicians and health
care providers and provide a more readily accessible
and comprehensive integration of several aspects of a
patient’s health record (Cimino and Shortliffe, 2006).
Unfortunately, despite the benefits of EMR sys-
tems, their rate of adoption has been slow relative
to the integration of information technology tools
into other occupations (Thompson and Dean, 2009).
The challenges encountered when deploying EMRs
in medical practices are numerous and varied (Baron
et al., 2005). Several reasons have been offered to ex-
plain the poor penetration of technology in the health
care sector. According to a recent study (Jha et al.,
2009), various financial and administrative issues are
often cited by hospitals as reasons for the poor adop-
tion of electronic medical record systems.
Surprisingly, this study also showed that physician
resistance is stronger in hospitals that have adopted
an EMR system than in hospitals without an EMR.
This suggests that current EMR technology may be
at best inadequate and at worst counter-productive in
addressing the needs of physicians. Indeed, techni-
cal issues related to the usability of EMRs have been
cited as a reason for the low acceptance rates of EMRs
in hospitals and clinics (Miller and Sim, 2004). Given
this, instead of capital investments in systems which
have a high risk of physician resistance and rejec-
tion, it may be wiser to investigate alternative inter-
face technologies that are more amenable to physi-
cians’ practices and workflows.
The interface design proposed by this paper al-
lows for a natural recording of patient related infor-
mation while simultaneously permitting seamless re-
quest and retrieval of reports from a variety of sources
related to a patient’s broader electronic health record.
This is done without having to navigate a myriad of
menu items and to tediously fill numerous data entry
fields presented in pop-up modal dialog boxes. By
streamlining the interface in this manner, we believe
that physicians will become less reticent to adopting
EMRs.
This paper is organized as follows: Section 2 gives
an overview of the challenges associated with the de-
sign of user interfaces for EMR systems and describes
324
Craig D. and Farrell G. (2010).
DESIGNING A PHYSICIAN-FRIENDLY INTERFACE FOR AN ELECTRONIC MEDICAL RECORD SYSTEM.
In Proceedings of the Third International Conference on Health Informatics, pages 324-329
DOI: 10.5220/0002746003240329
Copyright
c
SciTePress

some of the problems encountered by physicians as
they use the systems currently available. Section 3
presents the proposed interface design, which repre-
sents the primary contribution of this paper. Section 4
provides a discussion of some of the issues regarding
the interface design and presents opportunities for fu-
ture work. Finally, conclusions are presented in Sec-
tion 5.
2 EMR USER INTERFACE
ISSUES
The user interface of a viable EMR should provide
a portal through which all aspects of patients’ health
record can be seamlessly and accurately recorded and
retrieved. Moreover, the EMR interface must permit
requisition of orders and the subsequent reception of
results from a wide variety of healthcare sources. All
this information must then be made easily accessible
to the physician and presented in a meaningful way
by the EMR.
The literature suggests two aspects that are par-
ticularly important with respect to the usefulness of
an EMR to physicians: the recording of information
into the EMR and the navigation of the interface itself.
The goal of this paper is to present an EMR design
that makes it easier for the physician to accomplish
these tasks. The challenges associated with these is-
sues are discussed in the following subsections.
2.1 Recording Patient Information
Paper records offer physicians enormous flexibility
when documenting and annotating patient informa-
tion (Reuss et al., 2007). Unfortunately, the inter-
face for many electronic health record systems em-
phasize capturing patient data in a highly structured
or restricted coded form. In recent studies, it has been
shown that some physicians regularly eschew coded
data entry, opting instead to record patient informa-
tion in free-form text (Zheng et al., 2009). Providing
physicians the ability to record free-form text offers
them the flexibility to enter information in an order
and manner which is most appropriate to their per-
sonal workflow and style.
While coded and/or structured data can be useful
for clinical decision support and administrative pur-
poses such as report generation, forcing a physician
to pigeon-hole clinical observations may result in in-
formation critical to patient care being omitted from
the patient’s health record or recorded in the wrong
“box.” Information which is outside the domain cov-
ered by the restricted coded data of the required by the
software may subsequently be forgotten or not com-
municated to relevant parties.
During an encounter, patients often communicate
their complaints and symptoms to the physician in the
form of a story. For many physicians, accurately cap-
turing these stories (also known as patient narratives),
is essential to patient care (Walsh, 2004). An EMR
designer must appreciate the physician’s need to cap-
ture all aspects of the patient’s narrative during the en-
counter and allow the physician to construct the nar-
rative in a natural manner. Allowing the physician
to enter information using free-text offers more flex-
ibility over more restrictive structured or coded data
entry. As a result, the method of data entry becomes
more fluid and accommodating for the physician.
Ultimately, an EMR must never force the physi-
cian to forget that he or she is recording information
from a patient and not just recording information to a
database. By making the entry of patient information
more natural to the physician, the disruption to com-
munication between the physician and patient is kept
at a minimum.
2.2 Workflow and Interface Navigation
The importance of document management and the
clerical tasks implicitly performed by physicians must
be acknowledged in the design of an EMR interface.
In particular, patient information must be immedi-
ately accessible and not hidden within a labyrinth of
windows or dialog boxes (Rose et al., 2005). For ex-
ample, navigating between physician orders and their
associated results should be seamless and natural.
Physicians often complain about the “loss of
overview” as they navigate an EMR interface (Ash
et al., 2004). This loss of overview can be caused or
exacerbated by the plethora of pop-up windows or di-
alog boxes that are used by some EMRs to present
or request information or to alert physicians about
exceptional circumstances such as potentially seri-
ous drug-drug interactions (Grossman et al., 2007).
Sometimes, these dialog boxes are implemented as
“modal windows” which prevent the physician from
continuing until the event has been addressed. Such
modal dialog boxes are distractive and have been
shown to introduce inefficiencies in a physician’s
workflow (Belden et al., 2009).
The navigation of an EMR interface should be
very accommodating to a physician’s unique style and
needs. Retrieval of relevant information from a vari-
ety of sources should be efficient and tasks such as or-
ders and requisitions should be performed with a min-
imal number of steps. The numerous health events
that occur during the care of a patient must be pre-
DESIGNING A PHYSICIAN-FRIENDLY INTERFACE FOR AN ELECTRONIC MEDICAL RECORD SYSTEM
325

sented in a way that is contextually meaningful but
without overwhelming the physician or cluttering the
user interface. Details regarding these events and their
interactions with one another must be made readily
available by the interface.
Some of the inefficiencies associated with EMR
navigation may be attributed to fundamental aspects
of the underlying EMR architecture bubbling up to
the interface itself. When EMRs allow database ab-
stractions and other low-level implementation details
to bleed into the user interface, a physician may be-
come infected by technical considerations that are un-
related to the immediate care of his or her patients.
These artifacts can cause a physician to lose overview
during the assessment and planning phases of a pa-
tient’s treatment; patient care may degrade as a result.
By reducing or eliminating conventional user-
interface elements such as modal pop-up windows,
pull-down menus, buttons, checkboxes, lists, etc., a
more streamlined interface that offers free-text entry
and easier navigation can be developed. The basic
foundation for this interface is proposed in the next
section.
3 INTERFACE DESIGN
To address the issues described in the previous sec-
tion, the proposed interface design presents to physi-
cians a pane-based view of the patient record, as
shown in Figure 1. This interface is designed to of-
fer physicians a broad overview of the patient record
while allowing them to quickly focus on smaller de-
tails as the need arises.
As the physician records and retrieves clinical in-
formation to and from the EMR during the patient en-
counter, the interface does not change considerably
from one view to the next. No disruptive or obstruc-
tive pop-up windows are ever displayed by the inter-
face. In particular, the physician is not required to
navigate an abundance of windows and dialog boxes
in order to record or retrieve information to and from
the EMR, regardless of whether the information being
retrieved is local or remote. In addition to offering a
more natural workflow, this interface may help reduce
the loss of overview for the physician. The compo-
nents of the interface are described in further detail in
the following subsections.
3.1 Demographics Pane
The Demographics pane at the top of the window sim-
ply contains generic information about the patient,
such as name, age, date of birth and address. Unlike
other panes, the demographic pane cannot be resized
or closed — it is always present so that that the physi-
cian never loses focus of the patient currently being
treated. This helps to maintain overview, as described
in the Section 2.2.
The demographics pane can also be used to navi-
gate to other patients. As data is entered in the various
fields of this pane, the contents of the Viewer pane
below it will contain a list of patients that satisfy the
supplied criteria. Patients can then be selected from
this list and their associated details will be presented
in the Events pane.
3.2 Events Pane
The Events pane provides a segregated, time-ordered
view of a single patient’s health events (Bui et al.,
2007). This puts the entire patient’s history in tem-
poral context and offers the physician a “big picture”
view of the patient’s general history. This user inter-
face element is the primary vehicle used for navigat-
ing the patient chart and for maintaining a physician’s
overview of the patient record. As shown in Fig-
ure 1(b), this pane is divided into subpanes, each of
which correspond to various domains of health infor-
mation. There are five broad domains containing the
Notes
recorded by the physician,
Lab reports
,
X-ray
reports
,
Prescriptions
and
Correspondences
related to
the patient. Each of these subpanes can be expanded,
collapsed, zoomed and scrolled to reveal more or less
information as required by the physician.
Events are represented by small squares (colloqui-
ally referred to as rhondots) within the subpane. The
horizontal position of each event represents the date
the event took place, whereas the vertical placement
indicates the time of day the event occurred.
Events that are related to one another can be
connected by arrows, thereby making it clear which
events were triggered by an initiating event. This
would enable a threaded event viewer across several
provider domains, making it relatively easy to find the
originating order for a given lab result, for example.
Such a feature would rely upon the underlying com-
munication infrastructure using consistence reference
identifiers to relate the events together.
Colours and other visual attributes can be used
to indicate the urgency of the events. For example,
green could be used to represent normal events, while
blue and red could be used to represent abnormal and
critical/important events, respectively. Unread events
can be represented by a square; events that have been
viewed by the physician can be changed to circles.
More details on each event can be viewed by drag-
ging its square to the Viewer pane. An event can be
HEALTHINF 2010 - International Conference on Health Informatics
326
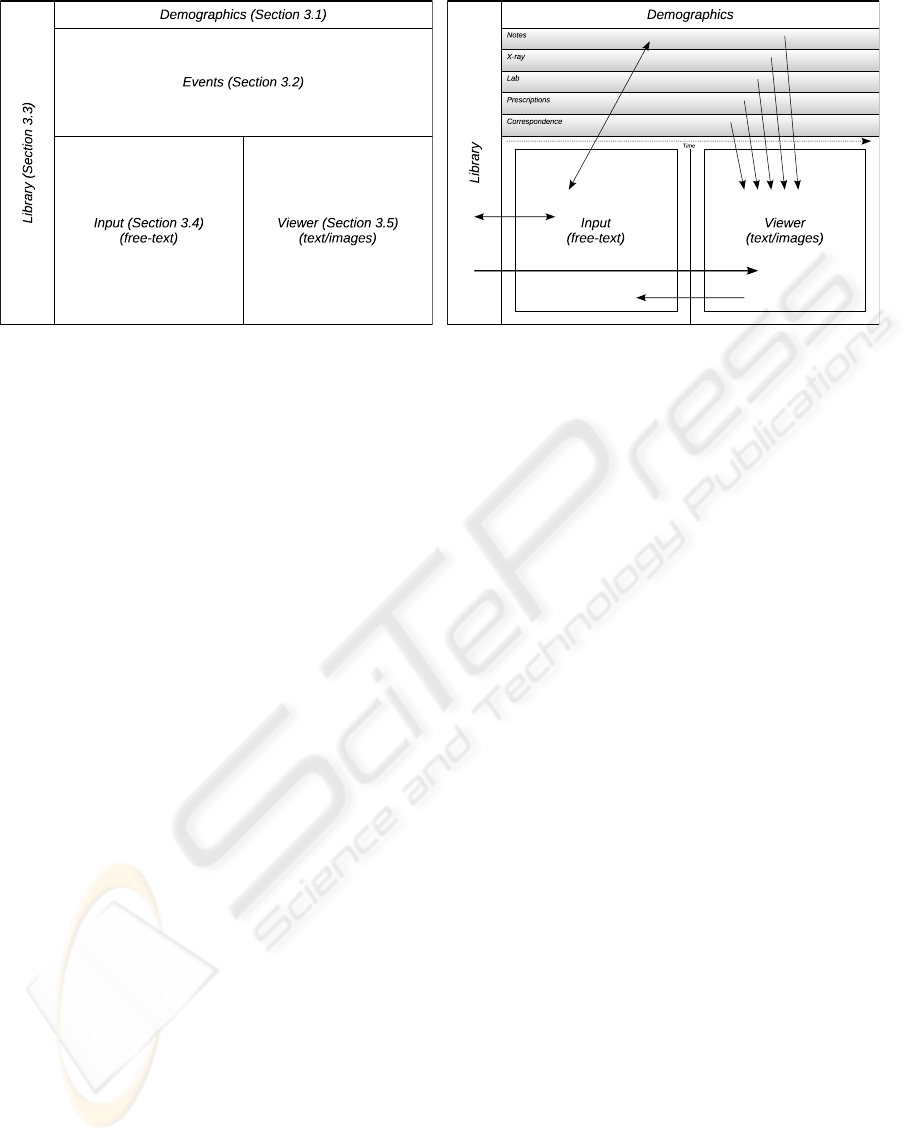
(a) Main Layout (b) Events Subpanes and Workflow
Figure 1: Interface Design Layout. The topmost pane shown in 1(a) contains patient demographics. The pane immediately
below contains a graphical representation of all the patient’s health events. To the left is a pane containing a generic library of
resource materials that can be queried by the physicians during input. Finally, the two panes at the bottom are used to record
and display detailed patient information. Figure 1(b) shows the collection of subpanes within the Events pane that contains
clinical data from a variety of sources. This pane of panes provides the physician with a broad, time-ordered overview of all
the patient’s information currently available to the physician from a variety of sources. Each event would be represented by
squares or dots (not shown). The arrows represent the general workflow that occurs between the panes.
annotated by dragging it to the Input pane, adding the
annotation, and dragging it back to the event pane; a
new note linked with the original event will then be
created in the
Notes
subpane. Context menus (acti-
vated by right clicking the mouse in the subpane) can
be used to select and plot various quantifiable data
items extracted from the events contained in that sub-
pane. An Events subpane can be expanded, if neces-
sary, to make the plots easier to read.
3.3 Library Pane
The Library pane is a vertical container along the
left hand side of the display which acts as a repos-
itory for a generic collection of clinical practice
guidelines, templates, formularies, patient educa-
tional pamphlets, diagnostic checklists, requisitions,
etc. Each element in the library has a title and a body
of associated text. The titles are arranged in alpha-
betical order in the pane. To prevent titles from over-
lapping, only frequently referenced titles are initially
displayed and accessible inside the pane. Dragging
these to the Input or Viewer panes will cause the ti-
tle’s corresponding body of text to be placed in the
appropriate pane. As with the subpanes in the Events
pane, the library pane can be zoomed and scrolled as
needed.
In addition to dragging information out of the Li-
brary pane, the contents of this pane can be queried
directly as information is entered in the Input pane.
The physician can add new resources to the li-
brary simply by writing text in the Input pane and then
dragging it to the Library pane. The first line of the
text can be used as the title. A body of medically re-
lated information can be programmatically imported
into the library, if necessary, as part of the installa-
tion procedure of the EMR in the physician’s office.
The Library pane may also contains documentation
related to the usage of the EMR itself, which can be
requested by making queries in the Input pane (see
below).
3.4 Input Pane
All information that the physician wishes to record in
the EMR is done via the Input pane. All progress and
SOAP notes as well as requisitions, prescriptions and
correspondences are created here in a relatively free-
text manner. Once the note is finished, it is dragged to
the Events pane where it will automatically be stored
in the
Notes
subpane. Generic information not par-
ticular to any patient can also be created here and
dragged to the Library, as described above.
The objective of the Input pane is to provide the
physician more flexibility when recording patient in-
formation than is offered by traditional EMRs that
may require a large amount of structured or coded
data entry. This pane is intended to serve the same
purpose as the blank piece of paper in a traditional
chart — the physician has the ability to record un-
structured text to capture the patient narrative in a way
most natural to his or her style.
DESIGNING A PHYSICIAN-FRIENDLY INTERFACE FOR AN ELECTRONIC MEDICAL RECORD SYSTEM
327

As the physician types the note, dynamic analy-
sis of the text and data extraction takes place. This
means that as characters are typed, words and phrases
can automatically change colour to inform the physi-
cian that something of interest has been understood
by the EMR. This provides the physician with instant
feedback that the EMR has successfully extracted in-
formation from the note. For example, quantitative
data such as heart rate and blood pressure could be
identified, provided a consistent syntax is used.
Notes are traditionally subdivided into coarse sec-
tions. For example a SOAP note has subjective, ob-
jective, assessment and plan sections. As various sub-
section heading text is entered by the physician, the
editor would enter different contextual modes of op-
eration which would affect the dynamic analysis of
the following text.
Ideally, all prescriptions and requisitions for lab
work or diagnostic could be made inside the Input
pane. This makes prescriptions and requisitions pos-
sible without having to navigate through numerous
pop-up screens and meticulously enter coded data
along the way (possibly losing patient overview in
the process). Any incomplete or erroneous requisi-
tions and dangerous prescription interactions could be
detected dynamically and reported in an unobtrusive
manner to the physician by turning the background
colour of the text red with an annotation indicating
the problem, for example.
The success of this Input pane interface depends,
in large part, on how well the dynamic text processing
algorithm can glean the intentions of the physician as
they construct their patient notes and requisitions (Ja-
gannathan et al., 2009). By having physicians adopt
modest syntactic conventions as part of their note tak-
ing, we believe that it will be possible to construct a
text processor that will be able to provide the physi-
cian with useful real-time feedback during the note
taking process.
3.5 Viewer Pane
The Viewer pane is used to display a wide variety
of data related to the patient chart. Events from the
Events pane can be dragged and dropped onto this
pane and the pane will render the contents of the event
in a human readable format. The contents could be
either text, images or a combination of both. Annota-
tions of the event can be made by dragging the event
to the Input pane, making the annotation, then drag-
ging it back to the Events pane.
4 DISCUSSION AND FUTURE
WORK
A prototype of this EMR is under development. The
current plan is to develop a web-based application
so as to ensure easy deployment across a wide va-
riety of computing platforms. The Bespin project
from Mozilla labs
(https://bespin.mozilla.com/)
im-
plements an editor component that may be useful for
entering medical notes in the context of the Input pane
described in Section 3.4.
The true measure of viability of the EMR inter-
face design described by this paper can only be made
once the construction of a working prototype that im-
plements the design is complete. Initially, it is ex-
pected that preliminary implementations of the EMR
will be used by medical school students in their first
or second year as an elementary training tool. Vari-
ous surveys and evaluations will be conducted on both
the students and their instructors for the purposes of
gathering feedback regarding the usefulness of the ap-
plication and to obtain suggestions for potential im-
provements. The remainder of this section describes
some of the problems that are anticipated and pro-
vides some possible mitigations.
Due to the free-text nature of the input, much work
remains in defining all the necessary syntactic clues
that would be used in the Input pane to allow the
physician to intuitively record and query patient in-
formation. For example, the exact details of the query
syntax and the format of the CPOE and prescription
sections of a note need to be addressed. When design-
ing the grammatical and syntactic format for these el-
ements, care must be taken to make the input as natu-
ral as possible so as not to make the EMR frustrating
or cumbersome to use by the physician.
The user interface should allow the partitioning of
events that are displayed in the Events pane accord-
ing to a patient’s specific problem. For example, it
should be possible to isolate those medical events per-
taining to a patient’s cancer treatment, while ignor-
ing events related to her broken hip. This would re-
duce the amount information presented to the physi-
cian and allow him or her to focus on a specific condi-
tion. A syntactically consistent textual tagging mech-
anism used within the free-text note may be helpful in
this regard.
Finally, the current web-based design of the in-
terface is somewhat unconventional in that it does
not present the physician with a traditional pull-down
menu system common in other traditional computer
applications. Furthermore, requiring all data be en-
tered as free-text may impose a burden on physi-
cians who are accustomed to having their notes tran-
HEALTHINF 2010 - International Conference on Health Informatics
328

scribed by someone else. However, many students
currently entering medical school are already familiar
with many web-based applications and have superior
keyboarding skills, making this less of an issue.
5 CONCLUSIONS
This paper proposes an interface design for an elec-
tronic medical record system that attempts to rectify
many of the problems encountered by physicians us-
ing existing EMRs to enter and query patient data.
The interface provides a more natural and less restric-
tive method of data entry by allowing the physician to
enter free-form text that undergoes dynamic extrac-
tion of quantifiable data and orders. Furthermore, by
making the navigation of various components of the
patient more efficient, we believe that the design of-
fers a fluid interface which is amenable to a physi-
cian’s workflow. As such, the work represented here
is still in progress — during the upcoming implemen-
tation and survey phases of this research, shortcom-
ings in this design will be uncovered and addressed,
along the lines as described in Section 4.
While this interface will require training in or-
der to use effectively, we believe that it can help in-
crease the productivity of a physician once this learn-
ing curve has been conquered. While this particu-
lar interface may not be suitable for all physicians,
we believe that the design presents a novel means
of interacting with a patient chart that may appeal to
physicians who have rejected such systems in the past,
thereby helping to increase EMR adoption.
ACKNOWLEDGEMENTS
The authors would like to thank the members, past
and present, of the Medical Informatics Group at
Memorial University whose ideas and suggestions
helped form the basis of the design work presented
in this paper.
REFERENCES
Ash, J. S., Berg, M., and Coiera, E. (2004). Some Un-
intended Consequences of Information Technology in
Health Care: The Nature of Patient Care Information
System-related Errors. Journal of the American Med-
ical Informatics Association, 11(2):104–112.
Baron, R. J., Fabens, E. L., Schiffman, M., and Wolf, E.
(2005). Electronic health records: Just around the cor-
ner? Or over the cliff? Annals of Internal Medicine,
143(3):222–226.
Belden, J. L., Grayson, R., and Barnes, J. (2009). Defin-
ing and testing EMR usability: Principles and pro-
posed methods of EMR usability evaluation and rat-
ing. HIMSS EHR Usability Task Force.
Bui, A., Aberle, D., and Kangarloo, H. (2007). Timeline:
Visualizing integrated patient records. IEEE Trans-
actions on Information Technology in Biomedicine,
11(4):462–473.
Carter, J. H., editor (2008). Electronic Health Records,
second edition. American College of Physicians,
Philadelphia, PA, USA.
Cimino, J. J. and Shortliffe, E. H., editors (2006). Biomed-
ical Informatics: Computer Applications in Health
Care and Biomedicine, third edition, chapter 2, pages
46–79. Springer-Verlag New York, Inc., Secaucus,
NJ, USA.
Grossman, J. M., Gerland, A., Reed, M. C., and Fahlman,
C. (2007). Physicians’ experiences using commercial
e-prescribing systems. Health Affairs, 26(3):w393–
404.
Jagannathan, V., Mullett, C. J., Arbogast, J. G., Halbritter,
K. A., Yellapragada, D., Regulapati, S., and Bandaru,
P. (2009). Assessment of commercial NLP engines for
medication information extraction from dictated clin-
ical notes. International Journal of Medical Informat-
ics, 78(4):284–291.
Jha, A. K., DesRoches, C. M., Campbell, E. G., Donelan,
K., Rao, S. R., Ferris, T. G., Shields, A., Rosenbaum,
S., and Blumenthal, D. (2009). Use of electronic
health records in U.S. hospitals. New England Journal
of Medicine, 360(16):1628–1638.
Miller, R. H. and Sim, I. (2004). Physicians’ use of elec-
tronic medical records: Barriers and solutions. Health
Affairs, 23(2):116–126.
Reuss, E., Naef, R., Keller, R., and Norrie, M. C. (2007).
Physicians’ and nurses’ documenting practices and
implications for electronic patient record design. In
Holzinger, A., editor, HCI and Usability for Medicine
and Health Care, volume 4799 of Lecture Notes in
Computer Science, pages 113–118. Springer-Verlag
New York, Inc.
Rose, A. F., Schnipper, J. L., Park, E. R., Poon, E. G., Li,
Q., and Middleton, B. (2005). Using qualitative stud-
ies to improve the usability of an EMR. Journal of
Biomedical Informatics, 38(1):51–60.
Thompson, S. M. and Dean, M. D. (2009). Advancing in-
formation technology in health care. Communications
of the ACM, 52(6):118–121.
Walsh, S. H. (2004). The clinician’s perspective on elec-
tronic health records and how they can affect patient
care. British Medical Journal, 328(7449):1184–1187.
Zheng, K., Padman, R., Johnson, M. P., and Diamond, H. S.
(2009). An interface-driven analysis of user interac-
tions with an electronic health records system. Jour-
nal of the American Medical Informatics Association,
16(2):228–237.
DESIGNING A PHYSICIAN-FRIENDLY INTERFACE FOR AN ELECTRONIC MEDICAL RECORD SYSTEM
329
