
INFORMATION SYSTEMS HETEROGENEITY
AND INTEROPERABILITY INSIDE HOSPITALS
A Survey
Lucas Ribeiro
1,2
, João Paulo Cunha
3
and Ricardo Cruz-Correia
1,4
1
Center for Research in Health Technologies and Information Systems (CINTESIS)
Faculdade de Medicina da Universidade do Porto (FMUP), Porto, Portugal
2
Centro Hospitalar de Trás-os-Montes e Alto Douro, Portugal
3
Instituto de Engenharia Electrónica e Telemática de Aveiro (IEETA), Universidade de Aveiro, Aveiro, Portugal
4
Serviço de Bioestatística e Informática Médica da FMUP, Porto, Portugal
Keywords: Electronic Health Record, Integration, Information System Interoperability, Heterogeneity.
Abstract: This paper presents a study of the heterogeneity and interoperability of Information Systems (IS) that exist
in Northern Portuguese Hospitals. Structured interviews to each Hospital CIO were performed regarding
their opinions, existing IS and integrations. The number of IS is exponentially related of the dimension of
the hospital (number of beds), and the relation between the number of IS and the number of integrations
follows an exponential model. The ratio between the number of effective integrations and the total
possibilities is very low and follows a quadratic model, indicating that the energy spent grows rapidly with
the increase of IS number and with poor results. Admission/discharge/transfer and drug related IS are
installed more often, and therefore are better candidates for a regional network. Despite numerous efforts to
develop standards, it seems that there is a large gap between their development and their applicability.
Interoperability inside organizations is a crucial first step, looking for the goal of achieving regional and
national EHR. Standardization is vital considering the number of IS and multitude of organizations
involved.
1 INTRODUCTION
It is currently agreed that interoperability in
healthcare is a matter of great importance, but also
of great complexity. The major challenge is to find a
way to allow interoperability between different
Information Systems (IS) in order to share
information and resources. Interoperability promises
a positive effect in the quality of care and also
economic advantages (Maldonado et al., 2003, Lenz
and Reichert, 2005, Walker et al., 2005, Uslu and
Stausberg, 2008).
Several solutions coexist with the aim of
facilitating the integration of a growing volume of
data, using different standards and technologies.
After many years of development in IS, the majority
of the healthcare organizations unfortunately are still
far beyond achieving open architectures that would
allow harmonious integration of computer
applications. The creation of a cohesive and
integrated Electronic Healthcare Record (EHR) is a
more complicated task than initially expected with
several obstacles (Zviran et al., 1998, Kitsiou et al.,
2006). Consistently combining data from different
sources takes a great deal of effort because the
individual systems usually differ in several aspects,
such as semantics, data representation, functionality,
presentation and terminology (Lenz, Blaser et al.
1999; Lenz and Kuhn 2002; Kitsiou, Manthou et al.
2006). In addition, several architectural mismatches
exists in the majority of the organizations, bringing
additional problems (Land and Crnkovic, 2003).
Interoperability of EHR is on the agenda of the
European Union (e.g. EPSOS and Calliope), of
many national governments (e.g. MedCom at
Denmark, RSEpt at Portugal) and regional initiatives
(e.g. RTS at the region of Aveiro in Portugal
(Cunha, 2007)). A summary of relevant patient data
has been seen as the most appropriate approach for
establishing EHR interoperability (Shabtai et al.,
2007). Nevertheless, to obtain the full advantages of
information sharing (either for patient care,
337
Ribeiro L., Cunha J. and Cruz-Correia R. (2010).
INFORMATION SYSTEMS HETEROGENEITY AND INTEROPERABILITY INSIDE HOSPITALS - A Survey.
In Proceedings of the Third International Conference on Health Informatics, pages 337-343
DOI: 10.5220/0002749003370343
Copyright
c
SciTePress

management or research), it is necessary to share
much more data than just a summary. The European
Union in the January 2009 report says that achieving
full interoperability across the entirety of healthcare
would be a lengthy, expensive and possibly
unattainable goal (Veli N. Stroetmann (Ed.) and Karl
A. Stroetmann, 2009).
It is also known, that in order to obtain a regional
or national patient record it is first crucial to achieve
interoperability inside each healthcare organization
(Cotter, 2007). The integration maturity model
proposed by Schmidt includes four levels of
integration (inexistent, point to point, processes and
external); it should be noticed that only in this final
step is interoperability among different institutions
considered (Schmidt, 2000).
This paper describes the heterogeneity and
interoperability of IS existing in Northern
Portuguese Hospitals, aiming to foresee the
integration difficulties in creating a complete
regional or national patient record.
2 METHODS
2.1 Study Participants
The participants of this study are all hospitals in the
northern region of Portugal (n=34). The hospitals are
represented in this study by their Chief Information
Officer (CIO).
In the scope of this study we have just
considered clinical IS. We have not considered
integrations with any medical device.
2.2 Design Study
This is a cross-sectional study representing the
reality found in these Portuguese hospitals in the
first semester of 2009.
2.3 Data Collection Methods
ARS Norte (Administração Regional de Saúde do
Norte – Northern Regional Health Administration)
was asked permission to facilitate data collection for
the study. After their support it was sent a request
for cooperation to each Hospital. Then, the authors
sent an email to each hospital CIO involved in the
study with the questionnaire attached.
After the CIO returned the questionnaire a
process of double validation of the results was
performed: (1) the first author of this work, made a
phone interview with CIO to confirm the answers
given; (2) then the data was sent by e-mail to every
CIO so that the results of each interview were
validated by them.
2.4 Variable Description
The main variables of the questionnaire can be
grouped into CIOs opinions and the reality existing
inside their institutions. Variables about opinions:
How important is interoperability between IS
What plans for interoperability exist for your
institution
Do you trust the security of the already
existing integrations regarding information
confidentiality, integrity and availability
Are there monitoring mechanisms to detect
integration errors
Does the hospital have a plan regarding IS
If a plan exists, how does it refer to
interoperability issues
Is it better to buy most of IS to one single
vendor, or to buy best-of-breed departmental
IS from multiple vendors
Should there be regulation and certification to
the IS market regarding integration issues
Between which stakeholders (e.g. different
hospital departments, hospital and social
institutions, hospital and primary care) should
data exchange be a priority
Variables about reality inside hospitals:
What IS exist in the hospital
For each IS:
What is the scope (Global or Departmental;
the classification of the departmental
systems was made based on the list of
medical specialties of the National Board of
Physicians);
Supplier;
Relational database management system
(RDBMS);
Compliance with Architecture Standards.
Classification Adapted from (Blobel, 2006)
Terminology and Ontology Standards.
Classification Adapted from (Blobel, 2006)
What integrations exist between IS
For each integration:
I1. The level of the integration. Classification
adapted from (Schmidt 2000)
I2. Type of integration;
I3. Type of error detection (none, log, log and
automatic alert);
I4. Communication Standards. Classification
Adapted from (Blobel, 2006).
HEALTHINF 2010 - International Conference on Health Informatics
338
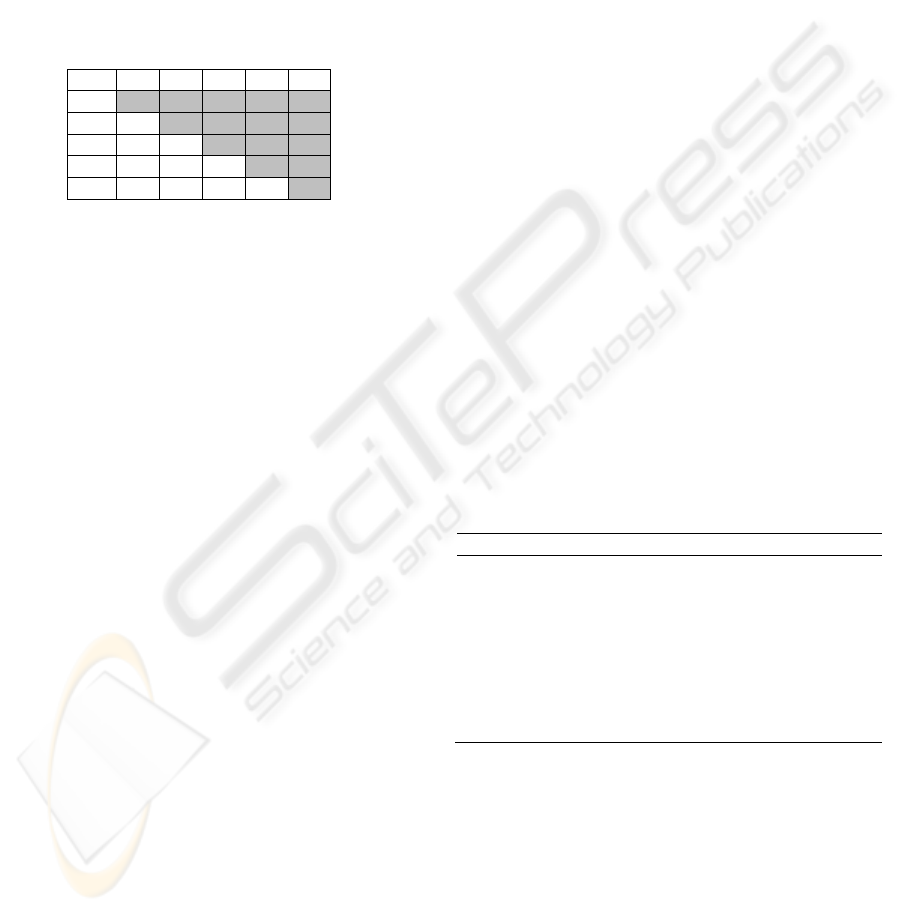
Four matrixes were built per hospital (one for each
variable regarding each integration, from I1 to I4).
Data from all arrays were stored in a relational
database, built on MS Access. Finally, we grouped
all the matrixes of all hospitals. An example of such
matrixes is illustrated in Table 1. Then some data
was exported to SPSS for statistical analysis.
Table 1: Example of possible integration matrix between 5
different systems (A to E) regarding variable I1. The letter
“d” means integration at the data level; “p” means
integration at the presentation level and “l” integration at
the logical level.
A B C D E
A
B d
C l d
D - - -
E d - p -
3 RESULTS
In this region there are 34 hospitals, most of them
are grouped in centers with financial autonomy (24
hospitals are grouped in 9 centers). As for the others,
7 are alone and 3 are grouped in 2 local units of care
(local units of care include hospitals and primary
care centers). The 7 ungrouped hospitals are either
very small or specialized hospitals. To our analysis
the number of different institutions considered is 18
(9 centers + 7 individual hospitals + 2 local units of
care). The number of beds per hospital varies
between 50 and 1083, with a median of 428 beds.
3.1 CIO Opinions
All CIOs (n=18) believe that interoperability is a big
issue in the future (72.2% of the responsible state it
is a very important issue and of urgent resolution,
responding the remaining 27.8% this is a very
important issue but not priority at the moment).
Most responsible for the IS have answered they
already have projects being implemented or plans to
soon begin interventions in IS integration (66.6%).
Most CIO (61.1%) stated that the hospital has a
plan for IS. The percentage of respondents who said
that the plan addresses the integration of IS in a
superficial way is 54.5% other 45.5% respond that
the issue is discussed in detail, with definition of the
requirements for interoperability.
The vast majority of respondents (72.2%)
believe that regarding the architecture of hospital IS
the best policy is to have multiple suppliers even
with the need for integrating them. The remaining
27.8% of respondents argue that the best policy is to
have a single provider that includes all clinical areas
thus ensuring a simple integration between all
modules. As for those responsible for hospitals with
500 beds or more none advocate that the best policy
is to have a single supplier.
The vast majority of CIO’s (88.9%) believe that
there should be regulation and certification of
software because without that interoperability will
hardly be effective, though the organizations should
be autonomous in the choices they make. The
percentage of those who argues that the Ministry of
Health should impose the solutions to organizations
is only 11.1%.
The three most frequently mentioned reasons, by
the eighteen respondents, to justify the lack of
interoperability that exists in the IS are: (1) existing
solutions are obsolete (66.7%), (2) the services tend
to behave as "islands" (61.1%) and (3) IS
architecture is poorly defined (50.0%).
Table 2 presents the results given, when asked to
choose from three options, as for between which
stakeholders should data exchange be a priority,
Although most respondents believe that the
integration between different IS is sufficiently
secure, they expressed some distrust in the three
areas under review (confidentiality of information
exchanged, data integrity and availability).
Table 2: Opinions of CIOs (n=18) regarding the question
about between which stakeholders should data exchange
be a priority.
Type of data exchange N %
Between each hospital department 18 100
Between hospital and primary care 18 100
Between hospital and patient 8 44
Between hospital and pharmacies 5 28
Between hospital and social security 4 22
Between hospital and private hospitals 1 6
Between hospital and insurance companies 0 0
Between hospital and patient transportation
companies
0 0
3.2 Reality Inside Hospitals
3.2.1 Existing Information Systems
We found a total of 416 different installations
resulting in 127 different IS (ratio 3.3). There are
organizations that sometimes have the same IS
installed more than once, usually as a result of the
creation of Hospital Health Centres, thus without
complete consolidation of all its IS to date. There are
three organizations in this situation (40 installations).
INFORMATION SYSTEMS HETEROGENEITY AND INTEROPERABILITY INSIDE HOSPITALS - A Survey
339
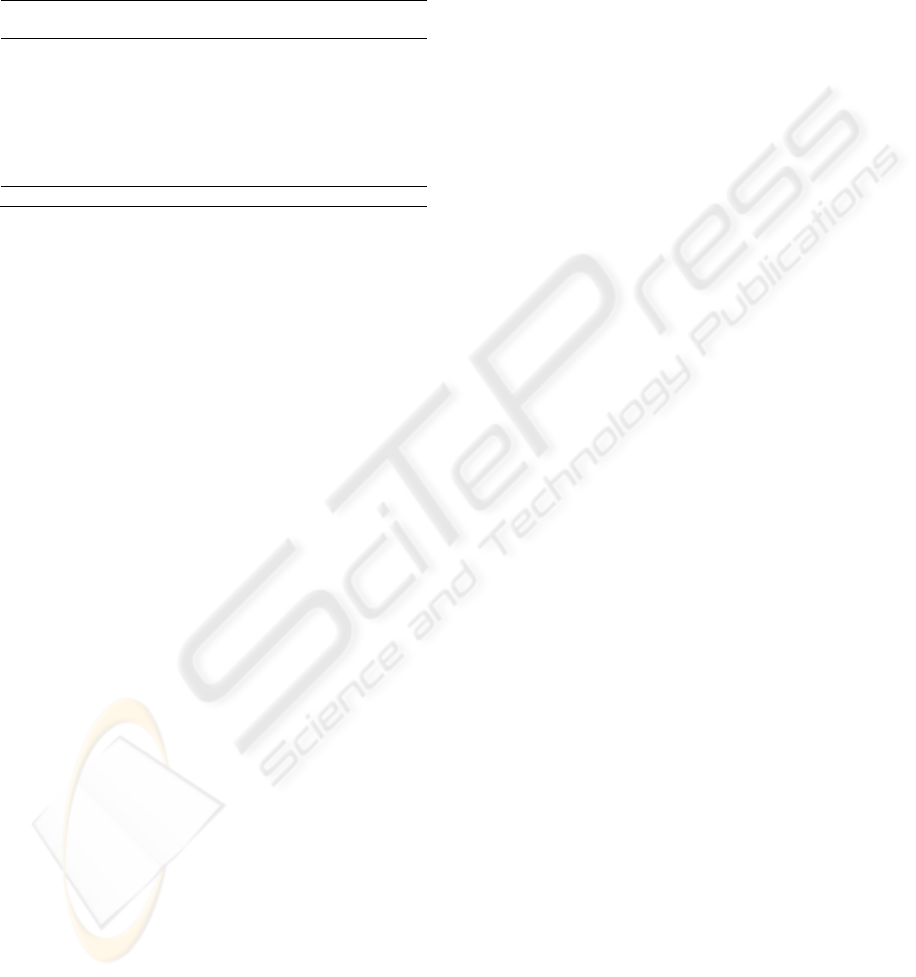
Table 3 shows the number of installations, number
of different existing systems and their ratio grouped
by the types of installed IS.
Table 3: Type of installed IS, number of installations,
number of different existing systems and their ratio. The
Departmental type IS are subdivided in subgroups.
Type of IS Installations Different IS Ratio
N % N %
ADT or EPR 67 16 8 8.4
Departmental 349 84 119 2.9
Laboratory IS 58 14 22 2.6
Imaging (RIS
and PACS)
41 10 17 2.4
Prescribing and
dispensing drugs
34 8 6 5.7
Others 216 52 74 2.9
Total 416 127 3.3
In terms of distribution of suppliers of IS by country
of origin, the country with the highest expression is
Portugal (58.3%). For the other supplier countries, it
is also worth mentioning, Spain (12.5%) and the
United States of America (10.4%), other five
countries represent the remaining 18.8%. For the
RDBMS used, the vast majority of facilities use
Oracle (77.9%) followed by SQL Server (10.3%)
and in 11.8% others.
The number of IS by organization follow a
normal distribution. The majority of organizations
(66.7%) have up to twenty two distinct IS. The
average of IS per Hospital is 20.9 (SD 9.1) with a
minimum 7 and maximum 41. If we consider the
total number of installations (including repetitions)
the average hospital installations rises up to 23.1.
No IS found follows any standard of information
architectures.
As for terminologies, 67.7% of IS don’t use any
specific terminology, LOINC is used by 11.02%;
ICD by 9.45%; SNOMED by 7.87% and others in
3.94%.
The analysis of the relationship between the
variables: number of IS (IS Nº) and number of beds
(Nº Beds); number of IS and number of effective
integrations (
Nº Integrations) and number of possible
(Pi) and effective integrations, was tested in three
models (linear, quadratic an exponential) to search
for the model that best fit the data. The quality of the
adjustment was analyzed with the F test.
There is a high positive association between the
number of beds and the number of IS (R
2
= 0.65).
The exponential equation better relates the number
of IS with the number of beds. The equation is as
follows:
IS Nº = 10.78
×
e
0.001 x Nº Beds
3.2.2 Existing Integrations
In the total 18 organizations (34 hospitals) we found
629 integrations. The number of integrations per
organization does not follow a normal distribution.
The median is 27.5 (minimum 7 and maximum 88
integrations).
There is a high positive association between the
number of IS and the number of integrations (R
2
=
0.66). In this case, 66% of the variation in the
number of integrations (Nº integrations) is explained
by the number of IS (IS Nº). The equation that better
represents the relationship is exponential. The
equation is as follows:
Nº Integrations = 9.15× e
0.06 x IS Nº
The total possibilities of integration (Pi), based on
the number of existing systems (IS Nº), is as
follows:
Pi= IS Nº [(IS Nº/2)-(1/2)]
The mean percentage of effective integrations
(existing integrations) versus the number of total
possible integrations is 15.8% (SD 7.6).
The graphic (scattered plot Figure 1) shows the
results regarding the number of effective
integrations and total possible integrations using the
3 models (linear, exponential and polynomial).
After analyzing the three models, we conclude
that the quadratic is the more adequate. The equation
that demonstrates this relation is as follows:
Nº Integrations=16,59+0,02 × Nº Pi+(7 × 10
-5
) × Nº Pi
2
The number of integrations for application layer
(data, logic, presentation) is as follows: data
(83.8%), presentation (14.9%) and logic (1.3%). In
the data layer most common integrations types are:
DB Link (35.0%) and Shared Database (30%). The
use of FTP is used asynchronously at 4.1% of cases.
In only 3.5% of cases messages are used via sockets
directly by applications. Message Oriented
Middleware (MOM) is used in 11% of cases
(Biztalk 60%; Iguana 14.3%; Mirth 7.1%; Ensemble
5.7%; Apache Service Mix 4.3%, Merge 4.3%,
Mitra 2.9% and Hermes 1.4%).
When MOM is used, the same IS uses the same
MOM in the totality of the cases. In some cases in
the same single integration is used more than one
MOM.
In the logic layer, Web Services is the only
method used. In the presentation layer all
integrations are Web based.
In the majority of the integrations no semantic
protocol is used (87.1%). In the remaining (12.9%)
the only used is HL7 V2.X. Where HL7 is used, in
80.2% cases, MOM is used in the integration.
HEALTHINF 2010 - International Conference on Health Informatics
340
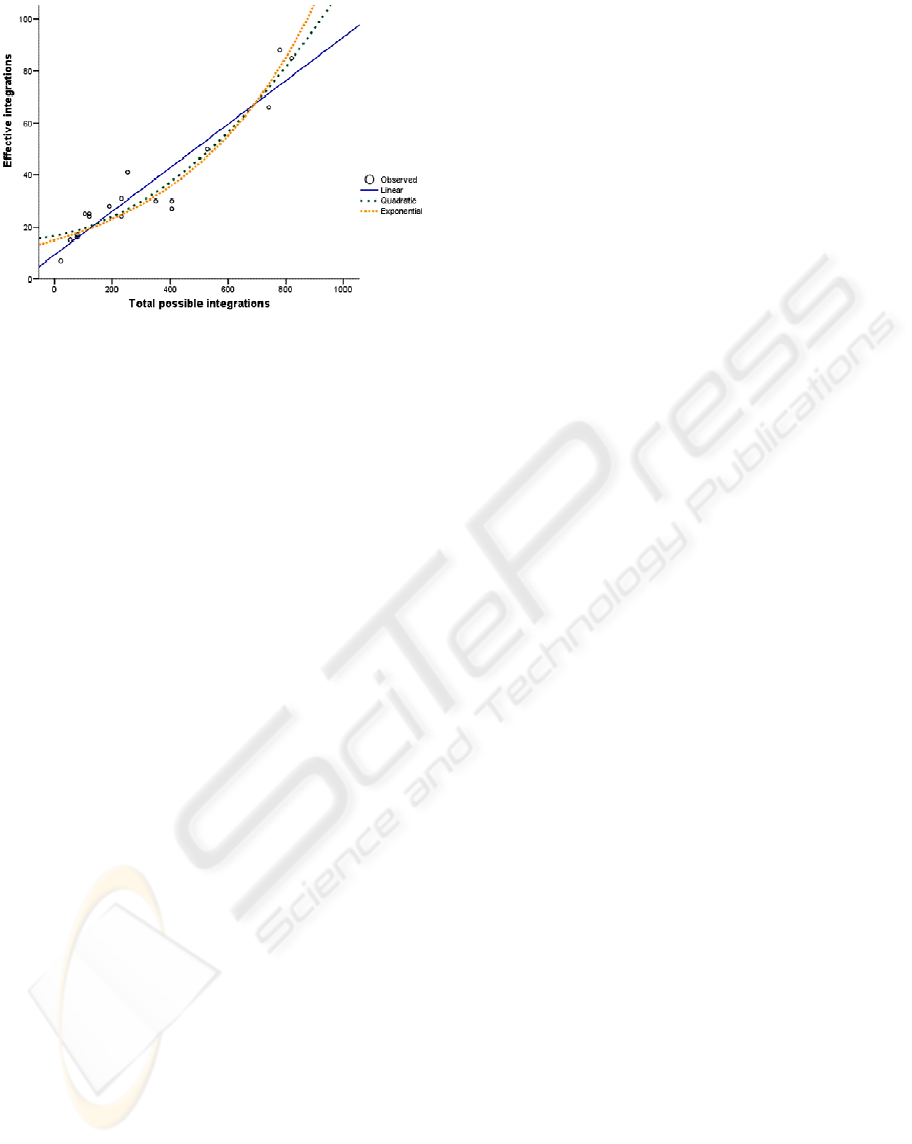
Figure 1: Number of effective integrations versus number
of total possible integrations.
In most cases there is no mechanism for detecting
errors (51.5%). In 33.7% there is only log record,
and in only 14.8% of cases there are record and
alarm mechanisms for abnormal situations.
4 DISCUSSION
Numerous authors point to interoperability as crucial
for achieving gains in health, by improving the
quality of care, allowing greater convenience, cost
reduction, improvements in research, public health
and decision support, among many others. Our
results show that the CIO's of the studied hospitals
somehow support these points of view as they
attribute great importance to interoperability.
The vast majority of CIO's believe that it is not
possible to build an EHR using just a single supplier,
and so there is the need of interoperability between
existing solutions. In our opinion, this reinforces the
need for governmental regulation agencies to
facilitate the interoperability between stakeholders.
Our study concludes that there is a multiplicity of
IS, probably too many. Some are very specialized
and so very difficult to become part of a single
monolithic IS. In addition to the hospital wide IS,
the most prevalent are those related to the
laboratories, medical imaging, and drugs prescribing
and dispensing.
The number of different IS versus the number of
installations show us that global systems have the
best ratio (8.4 installations per IS), followed by drug
related IS (5.7 installations per IS). In our opinion
these are the best candidates for early multi-
institution integrations as the existing heterogeneity
is lower. The remaining IS types (Laboratory,
Imaging and others) have very similar ratios (2.6,
2.4 and 2.9 respectively) and so are more difficult to
be integrated as more different IS have to be
included.
The number of IS per organization is closely
related to the hospital dimension (number of beds),
following an exponential relationship.
The number of integrations per hospital is
closely related to the number of IS, following an
exponential relationship.
A high ratio between the real and the possible
number of integrations is more easily achieved in
small hospitals. In larger hospitals this is more
difficult to achieve since the number of IS is higher,
and although the number of integrations rise, the
total proportion is lower, because the number of
possible integrations grows faster. This means that
the energy to integrate the existing systems rises
very fast when the dimension of the hospital rises
with poor results.
We have witnessed in the last 15 years a change
of paradigm of IS "data-aware" to "process-aware”,
where organizations are increasingly focusing on the
business processes (Van der Aalst et al., 2007). SOA
and BPM promise making systems flexible and
agile. For this reasons, SOA is the “state of the art”
technology in the sector (Kuhn et al., 2007). The
adoption of SOA in health is the natural course, this
new approach will force us to rethink architecture
and how we developed the IS for the health sector
(Mykkänen et al., 2007). However, our results show
that almost all the integrations are in the data and
presentation layer, not sharing functionalities and
not taking advantage of the potential of SOA and
BPM technologies. This can possibly be explained
either by the age of these technologies, younger than
the age of the existing IS, or by the resistance to
change that sometimes characterizes the health
sector.
Despite numerous efforts to develop standards, it
seems that there is a large gap between their
development and their application in these hospitals.
No IS follows a standard information architecture,
and in 12.9% of cases the only standard of
communication found was HL7 v2.x. Interesting fact
is that HL7 is used almost always in association with
middleware (80.2%), leading us to conclude that the
IS that implement HL7 directly is very low. HL7
v2.x is the most widely implemented standard in the
world today (Cruz-Correia et al., 2007). However,
the fact that an IS is compliant with HL7 version 2,
does not imply direct interoperability between
applications, since this version has no precisely
defined underlying information model, allowing
vague definitions with a multitude of optional data
INFORMATION SYSTEMS HETEROGENEITY AND INTEROPERABILITY INSIDE HOSPITALS - A Survey
341

models. In this context, although there is great
flexibility, it is necessary bilateral agreements
between the parties involved to be able to achieve
interoperability. To solve this problem a new version
of HL7 (version 3) is developing based on a
reference model called Reference Information
Model (RIM) (Eichelberg et al., 2005). For this
reason, in the totality of the cases we studied it is
necessary bilateral agreements, even when HL7 is
used.
From a management perspective integration is
not valued as a global centralized activity. Our
results show that it is possible to find in the same
hospital technological overlapping approaches. Also,
the same IS uses the same MOM everywhere, and
therefore we conclude that the MOM is imposed by
the supplier, probably because is much faster and
easier to build the integrations with the same product
everywhere.
The construction of regional or national EHR,
are in the centre of attention today, by the potential
benefits involved. However, to make this possible,
first there must be local interoperability at each
health organization so that patient data can be seen
in a comprehensive way when it is accessed from
other institution. Interoperability inside hospitals is
weak, for the reasons presented above, thus
undermining the project of regional and national
EHR, as well as creating enormous obstacles within
organizations.
Our results also show that CIOs are reluctant
regarding the safety of the exchanged data, as in the
majority of cases (51.5%) there is no control
mechanism for the integration.
In the scope of this study we have just
considered clinical IS, and we have not considered
integrations with medical devices. If the analysis is
extended the complexity of the problem is even
greater.
A limitation of our study is the inexistence of
other similar studies for comparison. However it is
our impression that this reality will be identical in
many other regions.
Another important finding relates to the
difficulty on getting the data, due to the lack of
documentation regarding existing systems and their
integrations. In the majority of the cases getting the
data from the healthcare was hard. We have reasons
to believe that being the main author of the paper
also a CIO and therefore a colleague of the
interviewed has helped gathering the data.
5 CONCLUSIONS
Our study concludes that there is a multiplicity of IS,
probably too many. The number of IS per
organization is closely related to the hospital
dimension and the number of integrations is
exponentially related with the number of IS. The
energy necessary to integrate the existing systems
grows rapidly when the dimension of the hospital
increases, with poor results.
Almost all integrations are in the data and
presentation layer, not sharing functionalities and
not taking advantage of the potential of SOA and
BPM technologies
Despite numerous efforts to develop standards, it
seems that there is a large gap between their
development and their application in these hospitals.
To our knowledge, the situation in Portugal
seems even worse as not many (if any) people work
in international standards bodies. We intend to
present these results to national institutions aiming at
raising global awareness on our current situation.
Interoperability inside hospitals is weak, thus
undermining the project of regional and national
EHR, as well as creating enormous obstacles within
organizations.
ACKNOWLEDGEMENTS
The authors acknowledge the help provided by ARS
Norte and also the contribution provided by Drª
Filipa Gomes in the statistical analysis.
REFERENCES
Blobel, B. (2006) Advanced And Secure Architectural Ehr
Approaches. International Journal Of Medical
Informatics, 75, 185-190.
Cotter, C. M. (2007) Making The Case For A Clinical
Information System: The Chief Information Officer
View. Journal Of Critical Care, 22, 56-65.
Cruz-Correia, R. J., Vieira-Marques, P., Ferreira, A.,
Almeida, F., Wyatt, J. & Costa-Pereira, A. (2007)
Reviewing The Integration Of Patient Data: How
Systems Are Evolving In Practice To Meet Patient
Needs. Bmc Medical Informatics And Decision
Making, 7, 14.
Cunha, J. P. (2007) Rts Network: Improving Regional
Health Services Through Clinical Telematic Web-
Based Communication System. Ehealth 2007
Conference. Berlin.
Eichelberg, M., Aden, T., Riesmeier, J., Dogac, A. &
Laleci, G. B. (2005) A Survey And Analysis Of
HEALTHINF 2010 - International Conference on Health Informatics
342

Electronic Healthcare Record Standards. Acm
Computing Surveys (Csur), 37, 277-315.
Kitsiou, S., Manthou, V. & Vlachopoulou, M. (2006) A
Framework For The Evaluation Of Integration
Technology Approaches In Healthcare. Proceedings
Of The Ieee In Information And Communication
Technologies In Bioinformatics, 28–30.
Kuhn, K. A., Giuse, D. A., Lapao, L. & Wurst, S. H.
(2007) Expanding The Scope Of Health Information
Systems-From Hospitals To Regional Networks, To
National Infrastructures, And Beyond. Methods Inf
Med, 46, 500-2.
Land, R. & Crnkovic, I. (2003) Software Systems
Integration And Architectural Analysis-A Case Study.
Lenz, R. & Reichert, M. (2005) It Support For Healthcare
Processes. Lecture Notes In Computer Science, 3649,
354.
Maldonado, J. A., Robles, M. & Crespo, P. (2003)
Integration Of Distributed Healthcare Records:
Publishing Legacy Data As Xml Documents
Compliant With Cen/Tc251 Env13606. Computer-
Based Medical Systems, 2003. Proceedings. 16th Ieee
Symposium, 213-218.
Mykkänen, J., Riekkinen, A., Sormunen, M., Karhunen,
H. & Laitinen, P. (2007) Designing Web Services In
Health Information Systems: From Process To
Application Level. International Journal Of Medical
Informatics, 76, 89-95.
Schmidt, J. (2000) Enabling Next-Generation Enterprises.
Eai Journal, 7, 8.
Shabtai, I., Leshno, M., Blondheim, O. & Kornbluth, J.
(2007) The Value Of Information For Decision-
Making In The Healthcare Environment. Stud Health
Technol Inform, 127, 91-7.
Uslu, A. M. & Stausberg, J. (2008) Value of The
Electronic Patient Record: An Analysis of The
Literature. Journal Of Biomedical Informatics, 41,
675-682.
Van Der Aalst, W. M. P., Benatallah, B., Casati, F.,
Curbera, F. & Verbeek, E. (2007) Business Process
Management: Where Business Processes and Web
Services Meet. Data & Knowledge Engineering, 61, 1-
5.
Veli N. Stroetmann (Ed.), D. K., Pierre Lewalle, Alan
Rector, Jean M. Rodrigues, & Karl A. Stroetmann, G.
S., Bedirhan Ustun, Martti Virtanen, Pieter E. Zanstra
(2009) Semantic Interoperability For Better Health
And Safer Healthcare. European Commission I N Fo
Rma T I O N S O C I E T Y A N D M E D I A.
Walker, J., Pan, E., Johnston, D., Adler-Milstein, J., Bates,
D. W. & Middleton, B. (2005) The Value Of Health
Care Information Exchange And Interoperability.
Health Affairs.
Zviran, M., Armoni, A. & Glezer, C. (1998) His/Bui: A
Conceptual Model For Bottom-Up Integration Of
Hospital Information Systems. Journal Of Medical
Systems, 22, 147-159.
INFORMATION SYSTEMS HETEROGENEITY AND INTEROPERABILITY INSIDE HOSPITALS - A Survey
343
