
SMART COLLATERAL LIGAMENT BALANCER FOR
INTRA- AND POSTOPERATIVE MEDIOLATERAL BALANCE
Shaban Almouahed
1,2
, Chafiaa Hamitouche
1,2
, Eric Stindel
1,3,4
and Christian Roux
1,2
1
LATIM – INSERM U650, Brest, France
2
TELECOM Bretagne – Institut TELECOM, Brest, France
3
Université de Bretagne Occidentale, Brest, 29200, France
4
CHU Brest, Service d’Orthopédie-Traumatologie, Brest, France
Keywords: Total knee arthroplasty, Collateral ligament balance, Knee balancer.
Abstract: The poor ligament balance performed at the time of total knee arthroplasty (TKA) can cause postoperative
instability and consequently early loosening of the prosthetic knee. The improper intraoperative assessment
of ligamentous balance is due to the use of an accurate surgical instrument which tenses the medial and
lateral collateral ligaments in uncontrolled way. A smart ligament balancer is proposed in this paper to
assess and perform ligament balancing intra- and postoperatively. A detailed three-dimensional model of the
prototype is developed using CAD software in order to discuss the operation of this device. The
intraoperative use of this balancer could allow to accurately reestablish a rectangular tibiofemoral gap with
symmetric mediolateral load distribution across the whole range of knee flexion. On the other hand, the
implanted balancer could be used postoperatively to assess ligamentous balance and to correct it when
needed.
1 INTRODUCTION
In most arthritic knee joints undergoing total knee
arthroplasty (TKA), some degree of collateral
ligament imbalance exists (Griffin, 2000). The
ligament imbalance could be present in the form of
instability, deformity, or a combination of these two
elements. The importance of acquiring proper
ligament balance at the time of TKA is well
recognized (Insall, 1993). Many techniques have
been used to assess ligament imbalance including
knee tensioning devices (Laskin, 1989), spacer
blocks (Insall, 1984), and manual distraction
instruments. The aforementioned techniques balance
the medial and lateral collateral ligaments by loading
them with maximally or in uncontrolled way. If the
resultant gap is trapezoidal, then the ligaments are
imperfectly balanced. Moreover, the traditional
tensors are unable to accurately assess the
ligamentous balance because of the discrete
measurement of tibiofemoral forces (Attfield, 1994).
A robotized distractor (Marmignon, 2004) has been
developed to assess soft-tissue balance. This
distractor consists of a base plate which is connected
with two independent and parallel trays. The upper
trays support the condyles and can be lifted by
means of a jack and a cable or thanks to two
inflatable rubber bladders. The disadvantage of the
first approach is that the device is not powerful
enough (maximal force is equal to 100 N), while the
disfavor of the second is that the parallelism of
upper trays could not be assured, which influences
the right functioning of the device. A force-sensing
device (Crottet, 2005) has been developed to
intraoperatively enhance the ligament balancing
procedure. This device has two sensitive plates to
support the two femoral condyles, a tibial base plate
and a set of different size spacers to fit the apparatus
thickness to the patient-specific tibiofemoral space.
Each of the two sensitive plates is instrumented with
three deformable bridges. Each bridge is equipped
with thick-film piezoresistive sensor to ensure the
accurate measurement of the amplitude and location
of tibiofemoral contact forces. The soft-tissue
imbalance is then assessed by the net varus-valgus
moment. The major limitation of this device is that
the application of load is manually performed by
stressing the lower limb, thus load is difficult to be
accurately applied. Moreover, the augmentation of
tibiofemoral gap height and consequently ligament
tension must be achieved by inserting different size
spacers, which increases the time and complexity of
TKA.
139
Almouahed S., Hamitouche C., Stindel E. and Roux C. (2010).
SMART COLLATERAL LIGAMENT BALANCER FOR INTRA- AND POSTOPERATIVE MEDIOLATERAL BALANCE.
In Proceedings of the Third International Conference on Biomedical Electronics and Devices, pages 139-142
DOI: 10.5220/0002757501390142
Copyright
c
SciTePress
To address the aforementioned shortcomings, a
smart ligament balancer is proposed to assess and
balance the collateral ligaments intra- and
postoperatively and to correct the imbalance when
needed.
2 MATERIAL AND METHODS
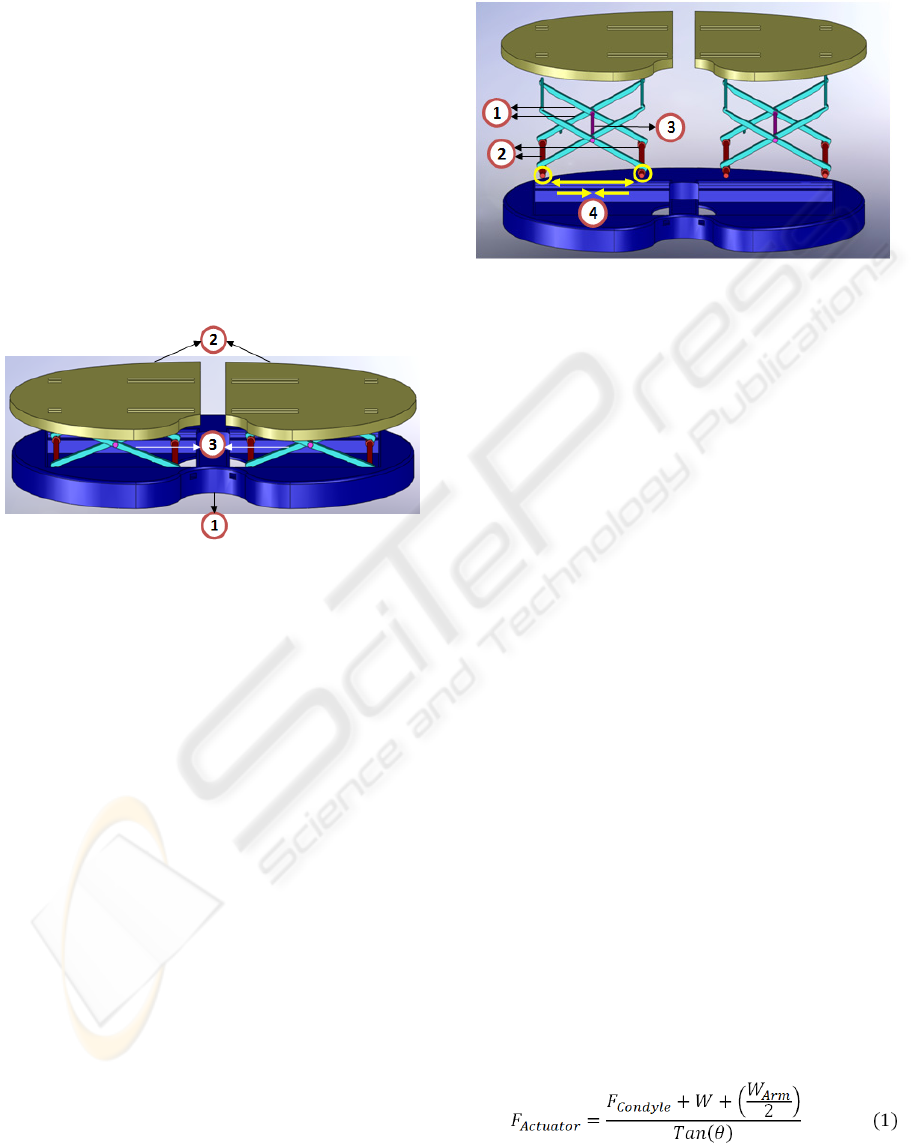
A detailed three-dimensional model (Fig. 1) of the
device is designed using CAD software in order to
describe the functionality of this device. The
proposed device consists of a fixed base plate and
two mobile plates. The lower base plate is separately
connected to each of the top plates by a scissor
mechanism operated by a miniature linear actuator.
Figure 1: An Isometric view of the smart ligament
balancer: 1. the fixed tibial base plate, 2. the two mobile
plates, and 3. the two scissor mechanisms.
The actuator located at the bottom of base plate
compartment drives one sliding shaft away from the
other in order to move the upper plate downward
and vice versa (Fig. 2). The two actuators are
automatically driven by a microcontroller in
response to the command signals sent by the surgeon
and to the force and position values measured by
adequate sensors embedded into the device. The
device is equipped with force and position sensors.
Three force sensors are embedded within each
mobile plate to continuously measure the amplitude
and location of the corresponding compartmental
contact force. One position sensor is embedded into
each compartment of the base plate to accurately
measure the distance between both the upper plates
and the lower plate at any time of the balancing
procedure.
In our study, the perfect ligament balance is
defined by a rectangular tibiofemoral gap and a
symmetric distribution of compressive load between
the medial and lateral compartments of knee at both
full extension and at 90° of flexion. The purpose of
this study is to assess the soft tissue balancing per-
and postoperatively for the full range of knee motion
and to rectify the imbalance when existed by means
of smart knee balancer.
Figure 2: Exploded view of the smart ligament balancer: 1.
the scissor arms, 2. the sliding shafts, 3. the pivot shaft,
and 4. the distraction and contraction of the actuator.
The immobile lower base plate of smart ligament
balancer is positioned onto the proximal cut of the
tibia while the two mobile upper plates are in contact
with the corresponding femoral condyles. The
balancer must be introduced into the tibiofemoral
space after the tibial osteotomy is performed and
before the femoral cuts are made. Measurement
must be made at full extension with the smart
balancer fixed onto the proximal tibial cut and acting
against the distal femoral condyles and at 90° of
flexion using the posterior femoral condyles and the
proximal tibial surface.
After the tibial cut is made, the smart ligament
balancer must be positioned within the knee. The
surgeon must send a command signal in order to
expand the balancer with a predetermined tension on
both medial and lateral sides until both mobile plates
are in full contact with distal femoral condyles and
the predetermined tension of collateral ligaments is
sensed by the force transducers embedded within the
upper plates. If the medial and lateral gaps are not
equal, a ligament release needs to be carried out in
order to rectify the mediolateral imbalance until the
flexion and extension spaces seem to be symmetric
and the collateral ligaments are once again well-
balanced (Fig. 3).
The relationship between the force measured on
the upper surface of mobile plate and the force
exerted by the actuator to expand or collapse the
scissor mechanism and consequently the balancer is
given by the following equation:
BIODEVICES 2010 - International Conference on Biomedical Electronics and Devices
140
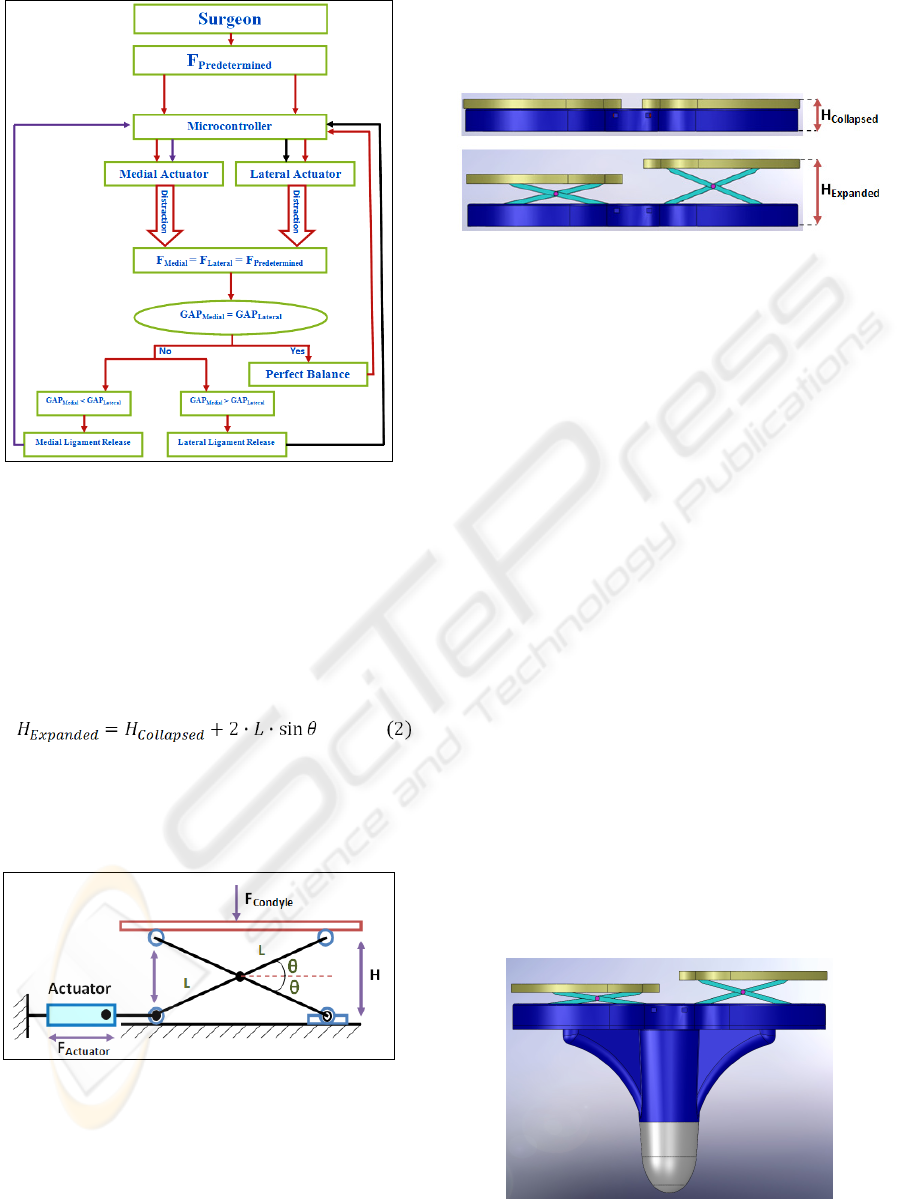
Figure 3: A schematic diagram of ligament balancing
procedure using the smart knee balancer.
Where F
Actuator
is the force provided by the actuator
arm, F
Condyle
is the force applied to the upper plate by
the corresponding femoral condyle, W is the weight
of the mobile plate and W
Arm
is the combined weight
of the two scissor arms (Fig. 4). The collapsed
height of the smart ligament balancer is 5 mm while
the expanded height is given by the next equation:
Where H
Expanded
is the expanded height of the
balancer, H
Collapsed
is the collapsed height of the
balancer, L is the length of scissor arm and θ is the
angle between the horizontal and scissor arm.
Figure 4: Scissor lift jack.
The starting angle is equal to 0° to allow the
balancer to be completely collapsed with initial
height of 5 mm (Fig. 5) and the ending angle must
not exceed 30° in order to maintain the parallelism
of the upper plates and to ensure their stability in the
transversal plane. Since the length of the scissor arm
equals 25 mm. Consequently and according to the
equation (2), the balancer can expanded from 0 mm
to 25 mm in a continuous movement.
Figure 5: The collapsed height of the balancer (H
Collapsed
=
5 mm) and the expanded height (H
Expanded
= 30 mm).
3 CONCLUSIONS
Tibiofemoral mechanical malalignment and
collateral ligament imbalance can result in a
postoperative instability of the prosthetic knee which
is a major complication after total knee arthroplasty
(Fehring, 1994). Since surgeons strive for perfection
in ligament balance, an accurate ligament balancer
(Fig. 6) is indispensable to prevent postoperative
complications such as instability. The importance of
postoperative assessment of ligament imbalance is
due to the fact that the mediolateral laxity of
prosthetic knee can change and increase after total
knee arthroplasty without resulting in postoperative
tibiofemoral mechanical malalignment but
increasing coronal ligament imbalance and
consequently knee instability. The primary cause of
postoperative ligament imbalance is that the
intraoperative ligamentous balance couldn’t be
perfectly achieved at the time of surgery, even with
considerable release of one of the two collateral
ligaments. This might be due to the absence of
adequate assessment of ligament balance during
surgery. Furthermore, the mediolateral ligament
balance varies postoperatively even if proper
balance is performed intraoperatively.
Figure 6: In vivo ligament balancer embedded onto the
tibial component of knee prosthesis.
SMART COLLATERAL LIGAMENT BALANCER FOR INTRA- AND POSTOPERATIVE MEDIOLATERAL
BALANCE
141

To the best of our knowledge, the smart ligament
balancer proposed in this study is the first one that
could quantitatively assess the mediolateral balance
of collateral ligament intra- and postoperatively in
both extension and flexion. In addition, this balancer
could allow a continuous assessment of ligament
imbalance over the whole range of flexion while
most balancing instruments assess this balance at
full extension and 90° of flexion and don’t allow
measurements at other positions of flexion (Attfield,
1996).
Since the medial and lateral collateral ligaments
of knee are of different cross-section, length and
shape and do not represent extensile strings, but
viscoelastic, extendible structures, the ligament
imbalance could not be constant at different
separation gaps and depends on the compressive
tension used to distract the bones. Therefore,
ligament imbalance must be quantified at different
distraction gaps by tensing the knee by equal forces
both medially and laterally but with different force
at each time. This is completely possible by means
of our smart knee balancer given that the ligament
imbalance is quantified by measuring the difference
in height between the medial and lateral sides of a
trapezoidal tibiofemoral gap produced when
identical tensions are applied to both medial and
lateral ligaments of the knee. In addition, the
parallelism of the upper trays is perfectly ensured by
the use of scissor mechanism instead of inflatable
rubber bladders (Marmignon, 2004). Furthermore,
the continuous movement of the upper tray ensures a
continuous augmentation of the gap height rather
than the discrete movement achieved by inserting
spacer blocks (Crottet, 2005), which decreases the
time and complexity of knee surgery.
REFERENCES
Attfield, S. F., Warren-Forward, M., Wilton,
T., Sambatakakis, A., 1994. Measurement of soft
tissue imbalance in total knee arthroplasty using
electronic instrumentation, Medical Engineering and
Physics, 16(6):501–505.
Attfield, S. F., Wilton, T. J., Pratt, D. J., Sambatakakis A.,
1996. Soft tissue balance and recovery of
proprioception after total knee replacement, Bone and
Joint Surgery, 78(4):540–545.
Crottet, D., Maeder, T., Fritschy, D., Bleuler, H., Nolte,
L.P., Pappas, I.P., 2005. Development of a force
amplitude- and location-sensing device designed to
improve the ligament balancing procedure in TKA,
IEEE Transactions on Biomedical Engineering,
52(9):1609–1611.
Fehring, T. K., Valadie, A. L., 1994. Knee instability after
total knee arthroplasty, Clinical Orthopaedics and
Related Research, 299:157–162.
Griffin, F., Insall, J., Scuderi, G., 2000. Accuracy of soft
tissue balancing in total knee arthroplasty,
Arthroplasty, 15(8):970–973.
Insall, J.N., 1984. Surgery of the Knee, Chapter: Total
knee replacement, Churchill Livingstone, 1
st
edition.
Insall, J.N., 1993. Surgery of the Knee, Chapter: Surgical
techniques and instrumentation in total knee
arthroplasty, Churchill Livingstone. 2
nd
edition.
Laskin, R.S., Riegèr, M.A., 1989. The surgical technique
for performing a total knee replacement arthroplasty,
The Orthopedic Clinics of North America, 20(1):31–
48.
Marmignon, C., Leimnei, C., Cinquin, P., 2004. Robotized
distraction device for knee replacement surgery,
Computer Assisted Radiology and Surgery, 1268:638–
643.
BIODEVICES 2010 - International Conference on Biomedical Electronics and Devices
142
