
FR
OM STORED CLINICAL DATA TO INTEROPERABLE
CLINICAL KNOWLEDGE
Idoia Berges, Jes
´
us Berm
´
udez, Alfredo Go
˜
ni and Arantza Illarramendi
University of the Basque Country, Paseo Manuel de Lardizabal 1, Donostia-San Sebasti
´
an, Spain
Keywords:
Semantic Interoperability, Electronic Health Records.
Abstract:
Health Information Systems deal with a great volume of digital clinical data. Although this management
has brought several advantages to the healthcare domain, a more intelligent management of those stored data
can provide further benefits. In this paper we present a proposal which introduces two main new advantages
to those Health Information Systems: First, the possibility of a semantic interoperability among them and
second, the ability to share the medical knowledge generated by each system—or by specialized organizations.
Our proposal makes use of an ontology to describe the terms used by the different Electronic Health Record
standards and the terms used by specific Health Information Systems (not forcing them to use a fixed standard),
and a reasoner that allows to interpret on the fly the data of a particular Health Information System by another
one, even when they use different data representations. Moreover, our solution provides a rule-based formalism
for representing medical knowledge of each system. Thanks to this representation, one system can benefit from
the knowledge which is stored on other systems and that was not initially aware of.
1 INTRODUCTION
The use of Electronic Health Records (EHRs) has
brought multiple advantages to the healthcare do-
main. The problem of poor legibility that might occur
when using handwritten paper records is avoided.
Moreover, decision support can be added to the med-
ical systems to help the professionals in the decision
process as well as to detect possible inconsistencies.
These advantages lead to less error-prone systems
which undoubtedly increase the quality of healthcare.
Another benefit of using information technologies
in this area is the possibility of exchanging EHRs
between different organizations. Over his lifetime,
a patient is likely to receive medical attention from
several institutions, and it seems reasonable for each
institution to have access to the previously recorded
data of the patient. Nowadays, however, this interop-
erability is still hard to achieve. Health Information
Systems used within the organizations have been
independently developed, which results in a high
number of heterogeneous models for representing
and recording EHRs.
In order to try to solve this situation, several
standards have arisen to represent EHRs. Most of
them follow a dual model approach, which separates
the information level from the knowledge level. The
information level is represented by the Reference
Information Model (RIM), which contains the
generic classes and properties that allow the writing
of any clinical annotations. For example, the classes
representing Tables, Lists and Entries will be found
at this level. The RIM is considered a stable model
that is not expected to change. Since the RIM is
composed of a small number of classes and they are
too general to describe the semantics of the clinical
terms, archetypes are used in the knowledge level
to create those descriptions. Archetypes impose
restrictions over the classes of the RIM to create new
clinical terms. These terms can be linked to clinical
terminologies, such as SNOMED (SNOMED, 2009)
or LOINC (LOINC, 2009) in order to represent their
meaning. For example, the term “Blood Pressure
Reading” could be described by an archetype.
The best known EHR standards are
openEHR(openEHR, 2009), CEN13606(CEN-
13606, 2007) and HL7 CDA(HL7-CDA, 2009).
The openEHR standard has been developed by the
openEHR Foundation, an international not for profit
foundation that aims at improving healthcare by
developing specifications, software and knowledge
resources with the purpose of achieving EHR in-
355
Berges I., Bermúdez J., Goñi A. and Illarramendi A. (2010).
FROM STORED CLINICAL DATA TO INTEROPERABLE CLINICAL KNOWLEDGE.
In Proceedings of the Third International Conference on Health Informatics, pages 355-360
DOI: 10.5220/0002758003550360
Copyright
c
SciTePress

teroperability. It follows the aforementioned dual
model approach and has already done a major work
in designing archetypes and templates (compositions
of archetypes). CEN 13606 is the proposal of the
European Committee for Standardization to represent
EHRs. It follows also the dual model approach
and provides by now a quite simple RIM and few
archetypes based on those of openEHR. Finally, HL7
CDA has been developed by HL7 and provides a
RIM and a draft template specification, which in this
standard represents the same idea of the openEHR
archetypes. For example, let us suppose that the
archetypes for representing the concept of “Risk
Score”(RS) are described as in Fig. 1 for openEHR
and CEN13606, respectively. Notice that some of the
classes to build the archetypes are different in both
standards (e.g. Observation vs. Entry in Fig. 1).
However, none of these standards has been
universally adopted, so the interoperability problem
remains unsolved. Moreover, as most medical
organizations in the world have their own developed
EHR models, it would be too expensive and time
consuming to change all their Health Information
Systems, migrating the stored data instances to the
new specifications, and training the medical staff to
use the new system. We advocate for another solution
which is transparent to the medical staff and where
only the essential information is transformed into
another representation. This solution goes far beyond
the use of XML for the interchange of data—because
even if it has been proved relevant for this issue, it
does not deal with the semantics of the exchanged
data(Hefflin and Hendler, 2000). On the contrary,
our proposal benefits from emerging semantic web
technologies, and more specifically ontologies ,
which can play a relevant role in the development
of frameworks to facilitate semantic interoperation
between heterogeneous Information Systems(Obrst,
2003).
In this paper we present a framework that favours
the semantic interoperability between heterogeneous
Health Information Systems. Two main research
issues are tackled by the proposal: the query inter-
pretation problem (Sections 2 and 3) and the clinical
knowledge sharing (Section 4). Considering the first
one, we have built an ontology, named EHRONT, in
which the RIMs and archetypes from the EHR stan-
dards and specific EHRs are described. This ontology
has been build following well-known methodologies
for building ontologies (Corcho et al., 2003). Thanks
to the ontological axioms defined between the terms
of different standards, and those between terms of
standards and terms of specific EHRs, a record of a
specific Health Information System
A
(corresponding
to a particular patient) will be interpreted on the fly
by another specific Health Information System B.
With regard to the second issue, our approach allows
the sharing of medical knowledge between systems
by using Semantic Web rules.
Achieving real interoperability among EHRs is
a research issue into which great effort is being put
((European Community, 2009), (Hoffman, 2009)).
Among the related works closer to our proposal, the
following ones can be mentioned: (Kilic and Dogac,
2009) provides a solution that uses ontological
reasoning. In this case, communication between
systems that follow different standards under the
same RIM (HL7-RIM) is supported, but commu-
nication between systems that use their proprietary
EHR specifications is not considered. Moreover,
in the transformation process of an instance of a
source archetype Arch
A
, the target archetype must
be explicitely declared, which requires the sender
to know specific knowledge about the receiver. In
(Mart
´
ınez-Costa et al., 2009) a software architecture
is presented for transforming a source ADL archetype
description that follows openEHR into a target ADL
description that follows UNE-EN 13606. Ontologies
describing archetype models of both standards, in
addition to an integrated ontology, are used in the
process. Notice that neither of both works considers
the feature of knowledge sharing.
2 THE EHRONT ONTOLOGY
The EHRONT ontology is the central element of the
framework and it is essential to achieve semantic in-
teroperability between heterogeneous EHR systems.
The terms of the EHRONT ontology are described as
classes and properties using the Web Ontology Lan-
guage, OWL(OWL, 2009), and more precisely, OWL-
DL. EHRONT is composed of two interrelated lay-
ers (standards layer and application layer) that clas-
sify the EHR contents regarding different levels of ab-
straction, being the standards layer the most general
and the applications layer the most concrete. Each
Health Information System will have its own version
of the EHRONT ontology. The standards layer will be
the same for all versions, while the applications layer
will be proper to each system. In the standards layer,
the classes and properties (RIM) that are specific to
each EHR standard are specified, as well as their
archetypes. Up to now, the terms of openEHR RIM,
CEN13606 RIM and HL7-CDA and their archetypes
belong to this level.
Following, a fragment of the logical representa-
HEALTHINF 2010 - International Conference on Health Informatics
356
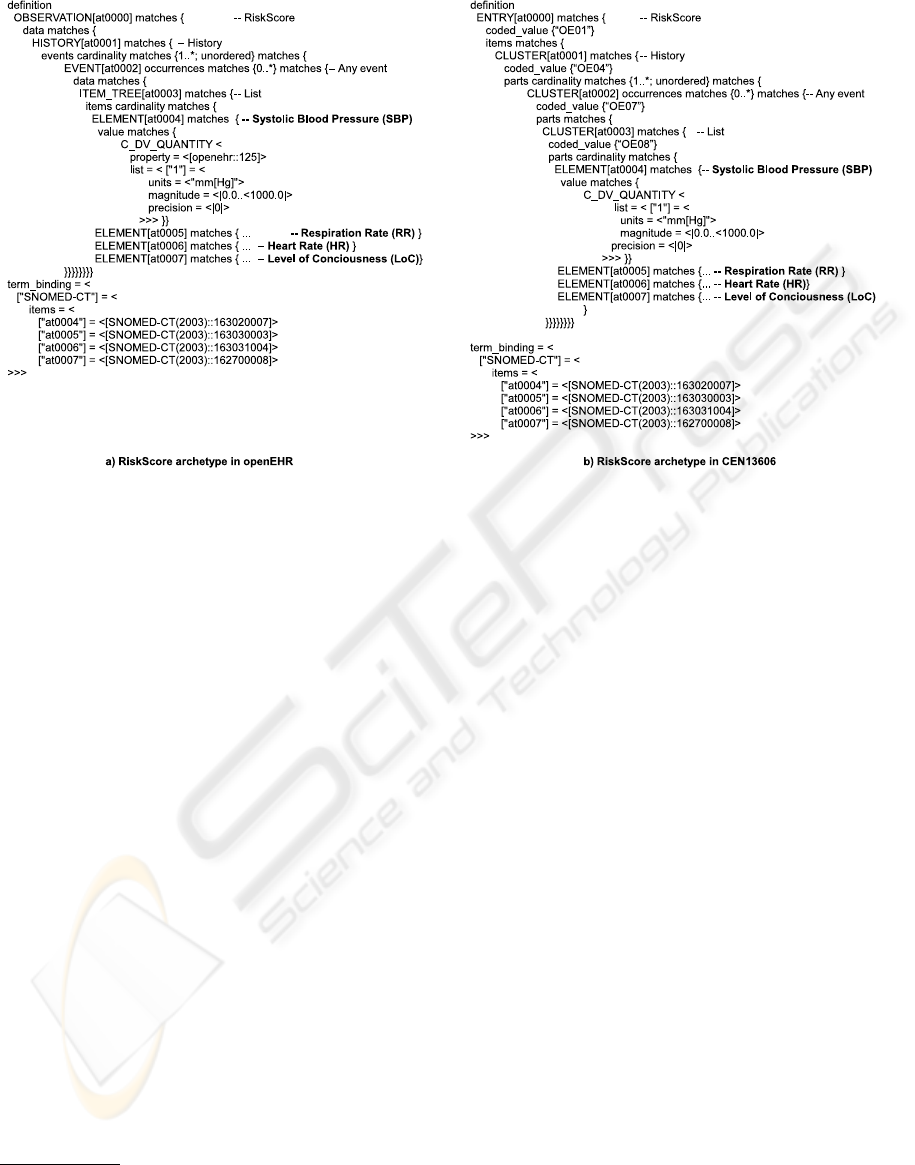
Figure 1: Archetypes for representing the Risk Score.
tion of archetypes in Fig. 1 can be found
1
.
oe:RS
≡
oe:Observation
u ∃
oe:hasObsData.oe:RSHistory
oe:RSHistory
≡
oe:History
u ∃
oe:hasHistoryEvent.oe:RSEvent
oe:RSEvent
≡
oe:Event
u ∃
oe:hasEvent.oe:RSData
oe:RSData
≡
oe:ItemTree
u ∃
oe:hasItem.oe:SBP
u∃
oe:hasItem.oe:RR
u ∃
oe:hasItem.oe:HR
u∃
oe:hasItem.oe:LoC
oe:SBP
≡ ∃
oe:hasSNOMEDCode.
{
‘‘163030007’’
}
u∃
oe:units.
{
‘‘mmHg’’
} u ∃
oe:magnitude
cen:RS
≡
cen:Entry
u ∃
cen:codedV.
{
‘‘OE01’’
}
u∃
cen:items.cen:RSHistory
cen:RSHistory
≡
cen:Cluster
u ∃
cen:codedV.
{
‘‘OE04’’
}
u∃
cen:parts.cen:RSEvent
cen:RSEvent
≡
cen:Cluster
u ∃
cen:codedV.
{
‘‘OE07’’
}
u∃
cen:parts.cen:RSData
cen:RSData
≡
cen:Cluster
u ∃
cen:codedV.
{
‘‘OE08’’
}
u∃
cen:parts.cen:SBP
u ∃
cen:parts.cen:RR
u∃
cen:parts.cen:HR
u ∃
cen:parts.cen:LoC
cen:SBP
≡ ∃
cen:SNOMEDCode.
{
‘‘163030007’’
}
u∃
cen:units.
{
‘‘mmHg’’
} u ∃
cen:magnitude
Moreover, relationships between terms of the dif-
ferent standards are defined in this layer. These rela-
1
We prefer this logical notation instead of the more ver-
bose RDF/XML syntax. Terms belonging to the openEHR
standard are prefixed by oe:, while terms belonging to the
CEN13606 standard are prefixed by cen:
tionships are essential to achieve interoperability be-
tween medical systems based on different EHR stan-
dards.
oe:Observation
≡
cen:Entry
u ∃
cen:codedV.
{
‘‘OE01’’
}
oe:History
≡
cen:Cluster
u ∃
cen:codedV.
{
‘‘OE04’’
}
oe:Event
≡
cen:Cluster
u ∃
cen:codedV.
{
‘‘OE07’’
}
oe:ItemTree
≡
cen:Cluster
u ∃
cen:codedV.
{
‘‘OE08’’
}
∃
oe:hasObsData
≡ ∃
cen:items
∃
oe:hasHistoryEvent
v ∃
cen:parts
∃
oe:hasEvent
v ∃
cen:parts
∃
oe:hasItem
v ∃
cen:parts
∃
oe:hasSNOMEDCode
≡ ∃
cen:SNOMEDCode
∃
oe:units
≡ ∃
cen:units
∃
oe:magnitude
≡ ∃
cen:magnitude
The application layer extends the level above with
classes and properties that are specific to each Health
Information System. All these classes can be defined
as subclasses of the terms in the standards layer of
the EHRONT ontology. Semantic Web Rules can
be added to enrich instance relationships. Obviously,
the more relationships and rules are defined with the
terms of the standards layer, the easier it will be to
achieve interoperability among systems. Moreover,
we propose a module that explores a schema of a par-
ticular system and extracts all its information (fields,
datatypes, restrictions, etc.) to create a new class in
the application layer of the EHRONT used by that
FROM STORED CLINICAL DATA TO INTEROPERABLE CLINICAL KNOWLEDGE
357
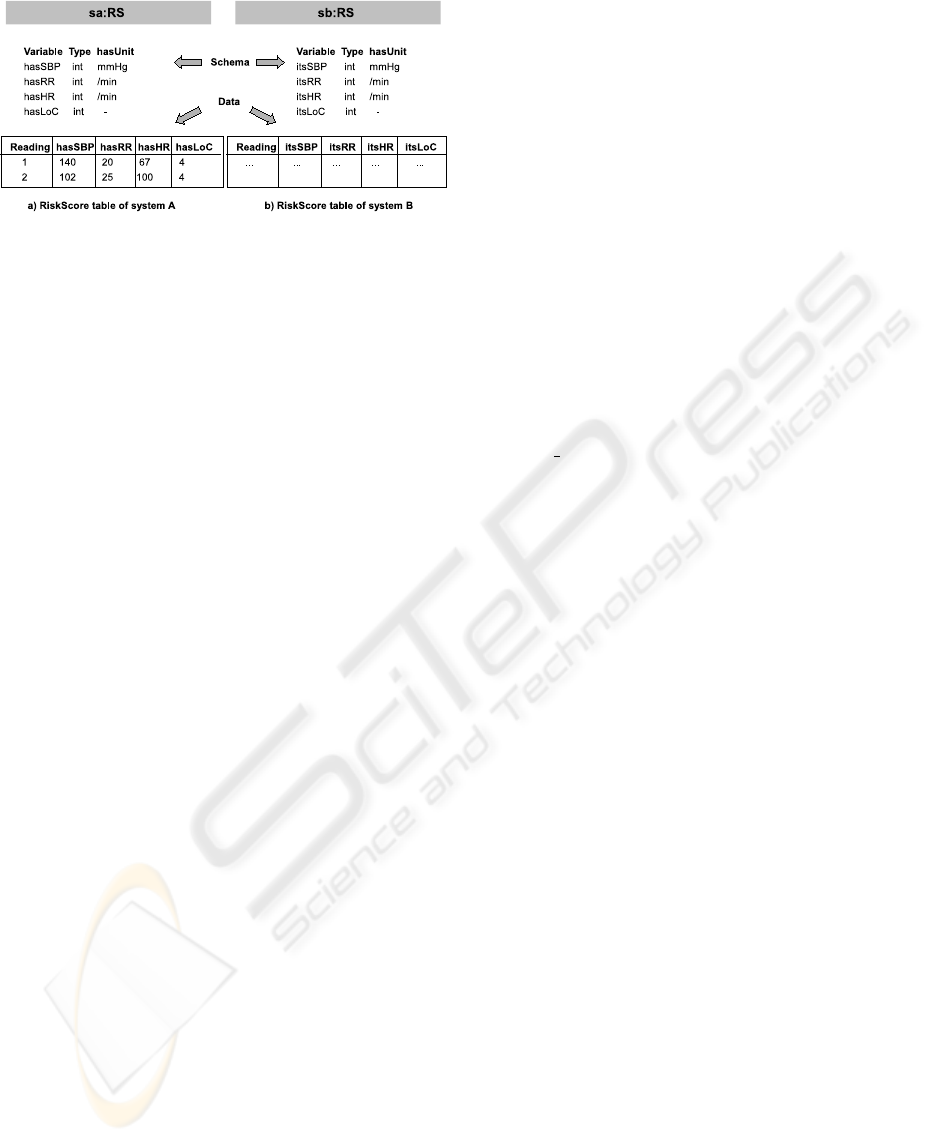
Figure 2: Risk Score tables of particular systems.
system. This new class is indeed the definition of
an archetype. Let us imagine a Health Information
System A whose table for storing Risk Score read-
ings is the one in Fig. 2a. The representation of this
archetype in the application layer of the EHRONT on-
tology, using OWL, could be the following:
sa:RS
≡
oe:Observation
u ∃
sa:hasSBP.sa:SBP
u∃
sa:hasRR.sa:RR
u ∃
sa:hasHR.sa:HR
u∃
sa:hasLoC.sa:LoC
sa:hasUnit
v
oe:units
sa:hasMagnitude
v
oe:magnitude
sa:hasSnomedCode
v
oe:hasSNOMEDCode
sa:SBP
≡ ∃
sa:hasUnit.
{
‘‘mmHg’’
}
u∃
sa:hasSnomedCode.
{
‘‘163020007’’
}
In order to map instances of this archetype to, for
example, the Risk Score archetype of the openEHR
standard, the following SWRL(SWRL, 2009) rule
must be used, because the openEHR Risk Score
archetype is much more complex than this one.
sa:RS(?x)
∧
sa:hasSBP(?x,?y)
∧
sa:hasRR(?x,?z)
∧
sa:hasHR(?x,?a)
∧
sa:hasLoC(?x,?b)
∧
swrlx:createOWLThing(?x,?c)
∧
swrlx:createOWLThing(?x,?d)
∧
swrlx:createOWLThing(?x,?e)
→
oe:RS(?x)
∧
oe:RSHistory(?c)
∧
oe:RSEvent(?d)
∧
oe:RSData(?e)
∧
oe:hasObsData(?x,?c)
∧
oe:hasHistoryEvent(?c,?d)
∧
oe:hasEvent(?d,?e)
∧
oe:hasItem(?e,?y)
∧
oe:hasItem(?e,?z)
∧
oe:hasItem(?e,?a)
∧
oe:hasItem(?e,?b)
3 INSTANCE
INTEROPERABILITY
The first contribution provided by our proposal is the
capability of a particular system B to interpret infor-
mation sent by another system A on the fly.
Let T
1
(i) be a tuple stored on the T
1
table of a
database of system A. Let T
2
be a table of a database
of system B. Let A and B the versions of EHRONT
ontologies used by systems A and B respectively. In
addition, let us assume that the module mentioned in
the previous section has converted the table schema
from T
1
to an OWL archetype class in the applica-
tion level of A , creating the class A :appT
1
. In the
same way, the table schema from T
2
has been con-
verted to an OWL archetype class in the applica-
tion level of B, creating the class B :appT
2
. Fur-
themore, specialization relationships have been cre-
ated between A :appT
1
and the standard level class
A:openehrT
1
and between B :appT
2
and the standard
level class B:cenT
2
. Finally, in the standards level re-
lationships have been defined between A:openehrT
1
and B:cenT
2
.
The process that needs to be carried is composed
of several steps:
1. One specific module is used in system A to
convert T
1
(i) into an individual of the class A :appT
1
,
namely A :appT
1
(i). In our example, if the second
tuple of the table in Fig. 2a is to be migrated, individ-
ual sa:rs 2 is created. Moreover, the following OWL
assertions will be created, among others:
(sa:rs-2 is-a sa:RS)
(sa:rs-2 is-a oe:Observation)
(sa:rs-2 sa:hasSBP sa:sbp-1)
(sa:sbp-1 sa:hasUnit "mmHg")
(sa:sbp-1 sa:hasMagnitude 102)
(sa:sbp-1 sa:hasSnomedCode "163020007")
2. At this point, with the help of an OWL rea-
soner, all the information related to A :appT
1
(i) is
extracted and converted into a set of OWL asser-
tions. Thanks to the specialization relationships and
rules that have been defined between the application
layer class A:appT
1
and the standards layer class
A:openehrT
1
(i) of the A ontology, A:appT
1
(i) will
be also related to the terms of the standards layer.
More precisely, it will also be an individual of the
A:openehrT
1
class. In our example, thanks to the rule
described in the previous section, the following asser-
tions will be created:
(sa:rs-2 is-a oe:RS)
(sa:rs-2 oe:hasObsData oe:rs-hist-1)
(oe:rs-hist-1 is-a oe:RSHistory)
(oe:hist-1 oe:hasHistoryEvent oe:rs-event-1)
(oe:rs-event-1 is-a oe:RSEvent)
(oe:rs-event-1 oe:hasEvent oe:rs-data-1)
(oe:rs-data-1 is-a oe:RSData)
(oe:rs-data-1 oe:hasItem sa:sbp-1)
(sa:sbp-1 is-a oe:SBP)
(sa:sbp-1 oe:units "mmHg")
(sa:sbp-1 oe:magnitude 102)
(sa:sbp-1 oe:hasSNOMEDCode "163020007")
3. The OWL assertions are sent to system B and
asserted into the B ontology. Again, with the help of
a reasoner, new information is obtained. Thanks to
the horizontal relationships defined in the standards
HEALTHINF 2010 - International Conference on Health Informatics
358

layer of the EHRONT ontology, the A :appT
1
(i) indi-
vidual is transformed into an individual of the stan-
dards layer class B :cenT
2
. Moreover, thanks to the
specialization relationships defined between the stan-
dards and application layers of the EHRONT ontol-
ogy, A:appT
1
(i) will become also an individual of the
B:appT
2
class.
In our example, let us imagine that in system B,
the Risk Score table is the one in Fig. 2b and that
there is a description of its archetype in the applica-
tion layer in the same way that has been done in sec-
tion 2 for the table of system A. Among others,the
following assertions will be inferred:
(sa:rs-2 is-a cen:RS)
(sa:rs-2 cen:items oe:rs-hist-1)
(oe:rs-hist-1 is-a cen:RSHistory)
(oe:hist-1 cen:parts oe:rs-event-1)
(oe:rs-event-1 is-a cen:RSEvent)
(oe:rs-event-1 cen:parts oe:rs-data-1)
(oe:rs-data-1 is-a cen:RSData)
(oe:rs-data-1 cen:parts sa:sbp-1)
(sa:sbp-1 is-a cen:SBP)
(sa:sbp-1 cen:units "mmHg")
(sa:sbp-1 cen:magnitude 102)
(sa:sbp-1 cen:SNOMEDCode "163020007")
Furthermore, thanks to the rules that may be de-
fined to relate the standards layer classes with the ap-
plication layer, the following assertions are created:
(sa:rs-2 is-a sb:RS)
(sa:rs-2 sb:hasSBPReading sa:sbp-1)
(sa:sbp-1 is-a sb:SBPReading)
(sa:rs-2 sb:itsUnit "mmHg")
(sa:rs-2 sb:itsMagnitude 102)
(sa:rs-2 sb:itsSNOMEDCode "163020007")
4. As A :appT
1
(i) is now an individual of the class
B:appT
2
, one specific module can be used to convert
the individual to an instance of the T
2
table.
Notice that thanks to the relationships that have
been defined in the EHRONT ontology, a tuple of a
table of a particular system has been interpreted by
another system.
4 KNOWLEDGE SHARING
EHRs hold great potential for clinical decision sup-
port, for example by translating practice guidelines
into automated reminders and actionable recommen-
dation. Usually, medical experts are in charge of
those translation tasks. An additional advantage pro-
vided by our proposal is the possibility of defining
and sharing obtained medical knowledge, expressed
as rules, between Health Information Systems. In
order to define the knowledge rules we have chosen
again SWRL, because it uses the declarative form to
Table 1: Expected values for the variables of the Risk Score.
Variable Min. value Max. value
Systolic Blood Pressure (SBP) 91 199
Respiration Rate (RR) 8 30
Heart Rate (HR) 50 119
Level of Conciousness (LoC) 4 4
express rules (which is suitable for obtaining conclu-
sions from a set of data) and moreover it is thought to
be used along with the OWL language.
For example, SWRL rules can be used to calculate
the Risk Score(RS) value of a given patient once the
Risk Score variables are registered. Table 1 shows the
values that are considered as normal for each variable.
If any of the variables is outside its limits, there is
an anomaly with that patient. For each anomaly that
is detected, the Risk Score value increases by 1. The
only good Risk Score for a patient is to have value 0.
Otherwise, there is some risk and medical staff must
be warned.
The knowledge could be expressed at the standard
level using SWRL rules similar to the following ones.
From this moment on, those rules can be shared with
other systems.
•
oe:RSData(?x)
∧
oe:hasItem(?x,?y)
∧
oe:SBP(?y)
∧
oe:magnitude(?y,?a)
∧
swrlb:lessThan(?a,91)
→
oe:hasRS-SBP(?x,1)
•
oe:RSData(?x)
∧
oe:hasRS-SBP(?x,?y)
∧
oe:hasRS-RR(?x,?z)
∧
oe:hasRS-HR(?x,?a)
∧
oe:hasRS-LoC(?x,?b)
∧
swrlb:add(?c,?y,?z)
∧
swrlb:add(?d,?c,?a)
∧
swrlb:add(?e,?d,?b)
→
oe:hasRS(?x,?e)
5 CONCLUSIONS
Although great efforts are being made in order to
achieve interoperability between Health Information
Systems, in our humble opinion there is still much
work to be done. Our approach takes into account
the real problem of systems that were not devel-
oped under EHR standards and integrates them into
a semantic-based framework. This framework al-
lows interoperability of EHR records (supported by a
reasoning process that decreases human intervention)
and, additionally, the shareability of encoded knowl-
edge about clinical processes. As future work we plan
to precisely identify the types of queries that can be
totally or partially interpreted on the fly.
FROM STORED CLINICAL DATA TO INTEROPERABLE CLINICAL KNOWLEDGE
359

REFERENCES
CEN-13606 (2007). EN 13606-1: Electronic Health Record
Communication.
Corcho,
´
O., Fern
´
andez-L
´
opez, M., and G
´
omez-P
´
erez, A.
(2003). Methodologies, tools and languages for build-
ing ontologies: Where is their meeting point? Data
and Knowledge Engineering, 46(1):41–64.
European Community (2009). Semantic Interoperability for
Better Health and Safer Healthcare. Research and De-
ployment Roadmap for Europe. ISBN-13: 978-92-79-
11139-6.
Hefflin, J. and Hendler, J. (2000). Semantic Interoperabil-
ity on the Web. In Proceedings of Extreme Markup
Languages 2000, pages 111–120. Graphic Communi-
cations Association.
HL7-CDA (2009). Available at http://www.hl7.org.
Hoffman, L. (2009). Implementing Electronic Medical
Records. Communications of the ACM, 52(11):18–20.
Kilic, O. and Dogac, A. (2009). Achieving Clinical State-
ment Interoperability using R-MIM and Archetype-
based Semantic Transformations. IEEE Transactions
on Information Technology in Biomedicine, to appear.
LOINC (2009). Available at http://loinc.org.
Mart
´
ınez-Costa, C., Men
´
arguez-Tortosa, M., Valencia-
Garc
´
ıa, R., Maldonado, J., and Fern
´
andez-Breis, J. T.
(2009). Transformaci
´
on Autom
´
atica de Arquetipos
UNE-EN 13606 y openEHR para Facilitar la Inter-
operabilidad Sem
´
antica. In Inforsalud 2009, Madrid,
Spain.
Obrst, L. (2003). Ontologies for Semantically Interop-
erable Systems. In Proceedings of the 2003 ACM
CIKM International Conference on Information and
Knowledge Management, pages 366–369, New Or-
leans, Louisiana, USA. ACM.
openEHR (2009). Available at http://www.openehr.org.
OWL (2009). Available at
http://www.w3.org/2001/sw/WebOnt/guide-
src/Guide.html.
SNOMED (2009). Available at
http://www.ihtsdo.org/snomed-ct/.
SWRL (2009). Available at
http://www.w3.org/Submission/SWRL/.
HEALTHINF 2010 - International Conference on Health Informatics
360
