
IN-VEHICLE MONITORING OF AFFECTIVE SYMPTOMS FOR
DIABETIC DRIVERS
In-vehicle Hypoglycemia Alerting System in EU Project METABO
Jonghwa Kim
Institute of Computer Science, University of Augsburg, Universit
¨
atsstr. 6a, D-86159 Augsburg, Germany
Alessandro Ragnoni
FERRARI Spa, via Abetone Inferiore 4, 41053 Maranello (Mo), Italy
Jacopo Biancat
S.A.T.E. S.r.l., Santa Croce 664/a, 30135 Venezia, Italy
Keywords:
Diabetes mellitus, Hypoglycemia, Emotion recognition, Biosensors, Pattern recognition.
Abstract:
Can self-management of emotion help on safety driving of diabetic patients? Fluctuant emotions in driving
can lead to very critical situations. In particular for diabetic drivers experiencing hypoglycemic events it is
inevitable to provide an intelligent alerting/recommendation system that assesses continuously driver’s affec-
tive and metabolic states and predicts sudden hypoglycemic events, in order for avoiding dangerous situations
during driving. In this paper we introduce an innovative approach to in-vehicle emotion monitoring system
conceived in the EU project METABO. The system aims for providing the drivers a self-management oppor-
tunity to monitor/control their emotional states and apt recommendations according to detected hypoglycemic
symptoms.
1 INTRODUCTION
Emotions affect perception, action and internal pro-
cesses of which the person having the emotion may
not be aware. This unawareness is then very danger-
ous for drivers, since safe driving activity demands
various types of driver’s abilities simultaneously such
as psychomotor skills, visuospatial functions, vigi-
lance and rapid information processing and judge-
ment. Actually, it is reported that the inability to
manage one’s emotions during driving is identified as
one of major causes of road traffic accidents (James,
2000). This is even more critical due to the fact that
drivers often lack the ability to calm themselves their
negative emotions, for instance, when they are an-
gry or frustrated. There are a number of research re-
sults in literature that support the importance of the
emotional state of drivers for traffic safety. Lajunen
and Parker (Lajunen and Parker, 2001) established
the links between anger, aggression and reported acci-
dents. Anxious may impair driver’s capability to deal
with a complex situation that occurs unexpectedly be-
cause anxiety narrows attentional focus, leading to
misinterpretation (
¨
Ohman, 2000). Furthermore, in the
work (Armitage et al., 1999) it is claimed that posi-
tive moods promote risky decision making and more
heuristic strategies, whereas negative moods instigate
a more problem-focussed approach.
The role of fluctuant emotions in driving is more
critical for diabetic drivers who suffer from hyper-
/hypoglycemia accompanying extremely unsteady af-
fective symptoms. Acute hypoglycemia, the most
common side effect of insulin therapy, may com-
promise driving skills. Functions that are most af-
fected by hypoglycemia include crucial abilities for
safe driving such as rapid judgement, attention, anal-
ysis of complex visual stimuli, memory and process-
ing of information and hand-eye coordination. Such
dysfunctions cause problem with contrast sensitiv-
ity and increased irritability and promote anger and
mood changes. Particularly, it is important to note
that the patients who lose their ability to recognize
the early signs of hypoglycemia, called hypoglycemia
unawareness, suffer from at least ten times higher risk
367
Kim J., Ragnoni A. and Biancat J. (2010).
IN-VEHICLE MONITORING OF AFFECTIVE SYMPTOMS FOR DIABETIC DRIVERS - In-vehicle Hypoglycemia Alerting System in EU Project
METABO.
In Proceedings of the Third International Conference on Health Informatics, pages 367-372
DOI: 10.5220/0002759703670372
Copyright
c
SciTePress
for severe hypoglycemia than that of patients with-
out this hypoglycemia unawareness. The impaired
awareness of hypoglycemia is associated with more
profound cognitive dysfunction, which takes longer to
recover after acute hypoglycemia than is experienced
by individuals with normal awareness (Deary, 1999;
Gold et al., 1995).
All these findings call to mind the need for in-
vehicle emotion monitoring system that observes pa-
tient’s emotional state during driving, reminds patient
to manage his affective state himself, predicts/alerts
forthcoming hypoglycemia events and recommends
needed activity. Recently many works on auto-
matic emotion recognition using physiological mea-
surements have been reported especially in advanced
human-computer interaction (HCI) (Kim and Andr
´
e,
2008). However, as emotion is a function of time,
context, space, culture, and person, it’s intensity and
effect may also widely differ from user to user and
from situation to situation. For diabetes mellitus, it
needs to pay a special attention to the fact that apply-
ing of emotion recognition systems developed based
on healthy people might result in a risky situation.
This is because of the fact that origin stimuli caus-
ing actual emotional state can hardly be traced for
diabetes patient, due to mutual interaction between
emotional change and the glucose level, which can be
described in the form of a vicious circle (i.e. cause-
result-cause).
In this paper, we present a design of in-
vehicle emotion monitoring system using multichan-
nel biosensors. First we briefly introduce the EU
project METABO where we develop the monitoring
system as a part of the project. Then we move to sum-
marize the concept of in-vehicle hyperglycemia alert-
ing system and describe our systematical approach to
the in-vehicle emotion monitoring system.
2 PROJECT METABO
The METABO
1
(Controlling Chronic Diseases re-
lated to Metabolic Disorders) is an european collab-
orative project funded by European Commission and
started in January of 2008 by 22 partners from 9 EU
member states.
2.1 Objective of METABO
The aim of METABO is to set up a comprehen-
sive platform, running both in clinical settings and
in every-day life environments, for continuous and
1
EU FP7-ICT-2007-1-216270, www.metabo-eu.org
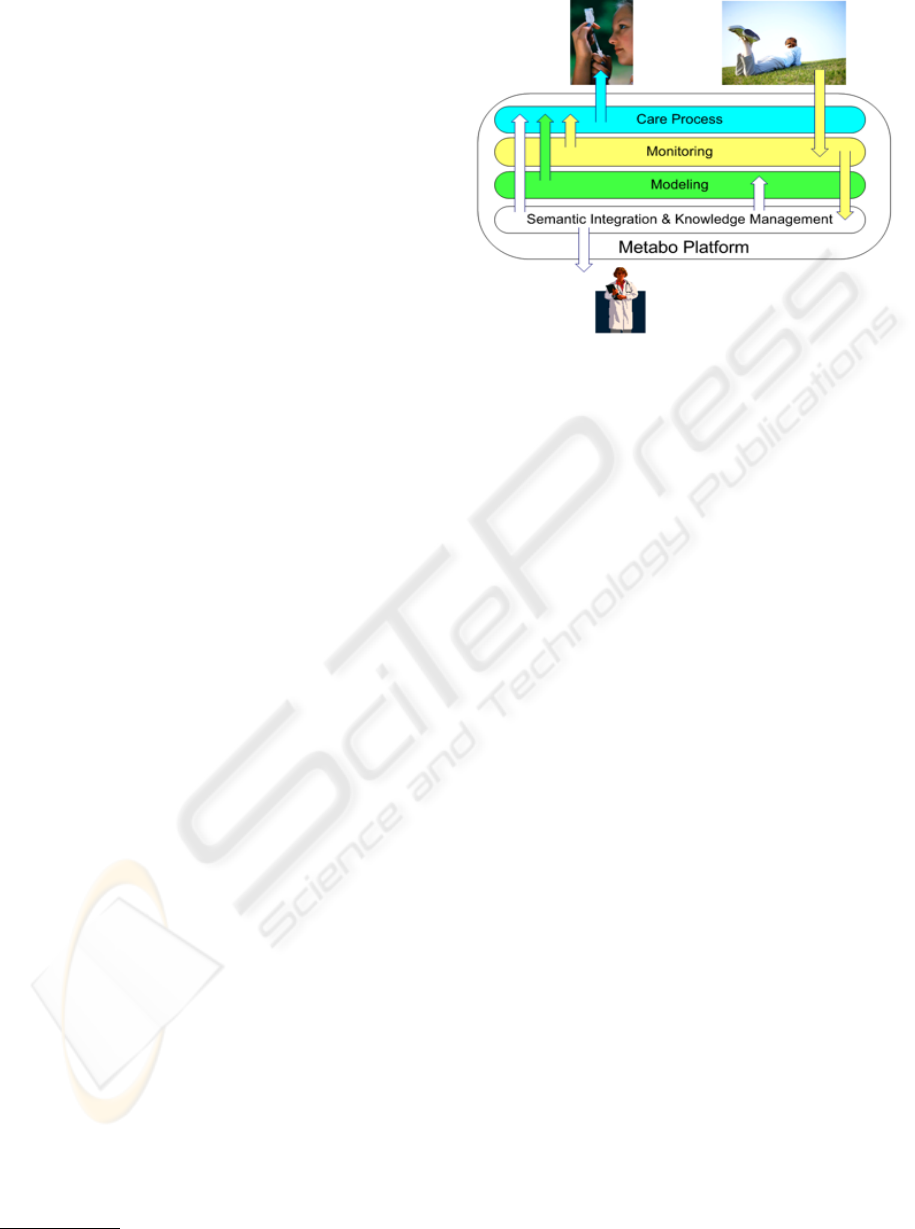
Figure 1: The concept of the METABO (after METABO
Annex I ”Description of Work”).
multi-parametric monitoring of the metabolic status
in patients with, or at risk of, diabetes and associ-
ated metabolic disorders. The type of parameters that
will be monitored, in addition to ”traditional” clinical
and biomedical parameters, will also include subcuta-
neous glucose concentration, dietary habits, physical
activity and energy expenditure, effects of ongoing
treatments, and autonomic reactions. The data pro-
duced by METABO will be integrated with the clini-
cal data and the history of the patient and will be used
in two major interrelated contexts of care:
1. Setting up a dynamic model of the metabolic be-
havior of the individual to predict the influence
and relative impact of specific treatments and of
single parameters on glucose level.
2. Building personalized care plans integrated in the
current clinical processes linking the different ac-
tors in primary and secondary care and improving
the active role of the Patient.
3. The combined use of tools for predictive mod-
elling and for the personalisation of the individ-
ual process of care will close the loop between
the Patients, the Professionals involved and the
Health Organisation. Mining the data produced
by METABO will allow the identification of pat-
terns and trends that will allow the fine tuning of
the model and the prompt adjustment of the pro-
cess of care.
METABO consists of a global platform that col-
lects and processes data coming from the patient and
the physicians’ tools (a mobile device for the patients
to acquire data from user and sensors and a web ap-
plication for the physicians to present them all data
collected and analyzed) and works as an information
exchange bridge between physicians and patients. On
HEALTHINF 2010 - International Conference on Health Informatics
368
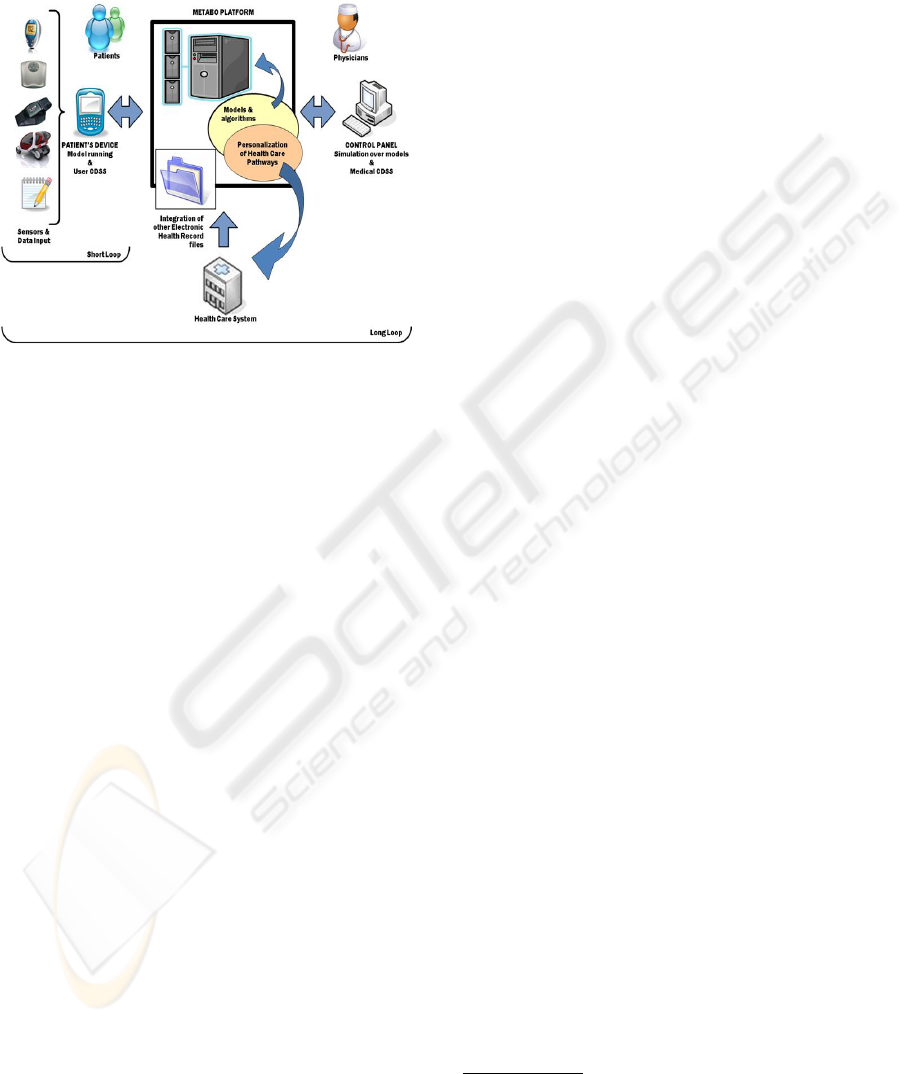
top of this, the system provides both groups of users
with decisions support systems to give them recom-
mendations in a personalized short loop and an inte-
grated long loop Figure 2.
Figure 2: Diagram of METABO Platform (after METABO
Annex I ”Description of Work”).
2.2 In-vehicle Hypoglycemia Alerting
System
In-vehicle hypoglycemia alerting system (IHAS) is a
special case-study in the METABO, which aims at de-
signing and building an in-vehicle version of the sys-
tem to provide metabolic monitoring and preventive
support to drivers, especially to those suffering from
sudden and/or unaware hypoglycemia. This research
is innovative in that it aims to measure and predict
hypoglycemia events indirectly by using physiologi-
cal sensors and by analyzing driver’s behavior behind
the wheel and the change of emotional states. The hy-
pothesis is that hypoglycemia will affect the both the
bio-profile of the patient and his/her driving behavior.
The IHAS consists of four subsystems, i.e. behavioral
monitor, emotive monitor, healthcare state and physi-
ological state:
Behavioral Monitor. This subsystem measures
driving-relevant signals such as steering wheel an-
gle, vehicle speed, lateral and longitudinal accelera-
tion, brake usage, etc. These will then be used to
develop a module able to evaluate driver’s behav-
ior. The final scope will be to identify pattern and
trends in these signals which can be correlated to hy-
poglycemic events in order to alert the driver to the
forthcoming hypoglycemia.
Input: car signals available on the CAN networks.
Output: indexes quantifying driver behavior focusing
on those behaviors.
Emotive Monitor. This subsystem is responsible
for recognizing driver’s emotional states by using
multichannel physiological signals and visual infor-
mation. This task includes to verify predictability of
glucose level changes based on actual emotional state
under the condition of a short-term observation and
to provide the driver a possibility of emotion manage-
ment training through biofeedback. Main challenge
of the system is to find interferential correlation be-
tween driver’s emotional state and the change of glu-
cose level.
Input: multichannel physiological signals and visual
information.
Output: driver’s emotional states and prediction of
hypoglycemic events.
Healthcare Monitor. This subsystem analyzes di-
etry, physical activity, treatment, and glycemic data
and predicts the metabolic status of the diabetic driver
in the short- and medium run. The data will be col-
lected by using patient’s mobile device (PMD) and
continuous glucose monitoring system (CGMS).
Input: treatment history, blood glucose values, insulin
intake, food intake, physical activity
Output: predicted blood glucose level and recommen-
dations.
Physiological Monitor. This module analyzes the
same physiological signals used for emotive monitor
in order for assessing the physiological state of the
driver. Particularly, it mainly focuses on extracting
cardiac features from electrocardiogram and blood
pressure.
Input: multichannel physiological signals
Output: drivers physiological states focusing on hy-
poglycemia detection.
3 IN-VEHICLE EMOTION
MONITORING
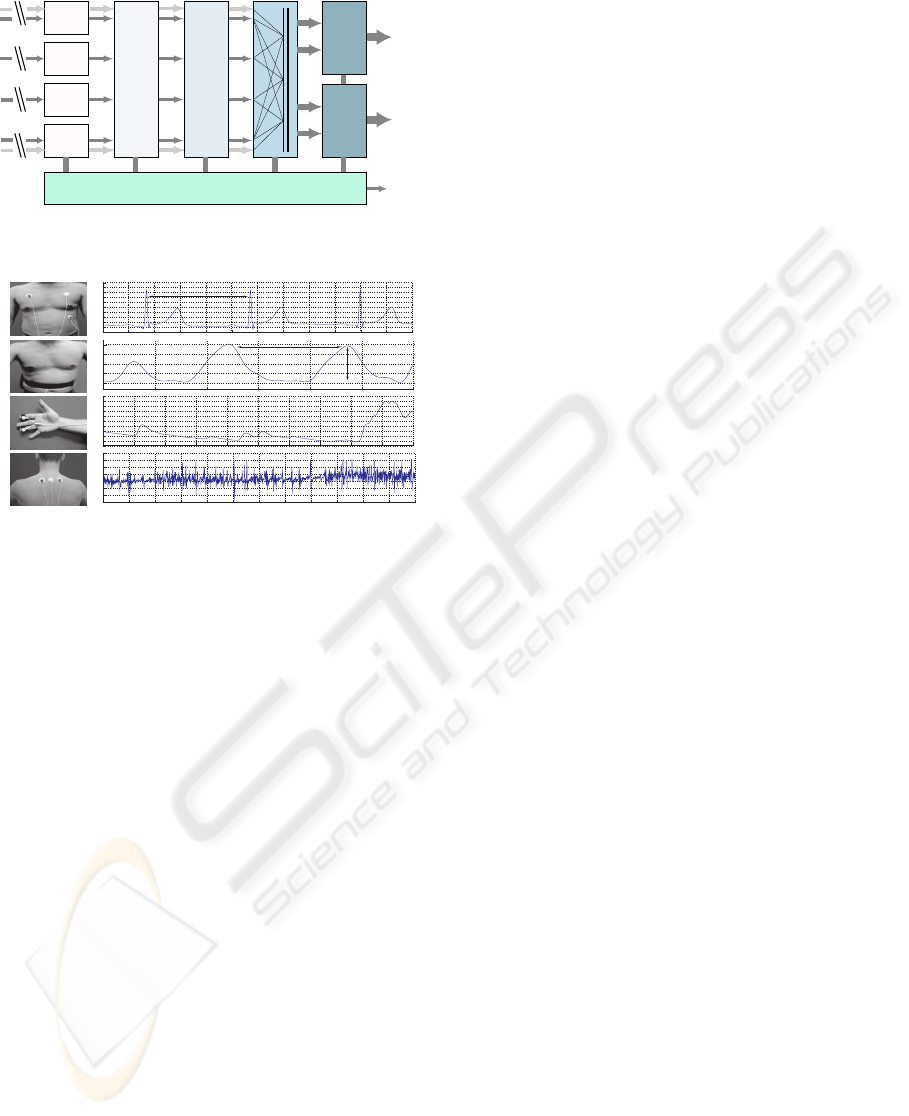
Figure 3 shows the frame work of in-vehicle emotion
monitoring (IEM) system.
3.1 Biosensors
We collect the physiological signals by using the
ME6000
2
with four biosensors, electromyogram
(EMG), skin conductivity (SC), electrocardiogram
(ECG), and respiration (RSP). The typical waveforms
and sensor positions are illustrated in Figure 4.
2
This is an 16 channel multi-modal Biofeedback sys-
tem with 14 bit resolution in sampling rate of 2000 Hz.
www.megaemg.com
IN-VEHICLE MONITORING OF AFFECTIVE SYMPTOMS FOR DIABETIC DRIVERS - In-vehicle Hypoglycemia
Alerting System in EU Project METABO
369
ACQUIRE
PREPROCESS
ANALYSE
FUSION
MAPPING
Rule-based
Mapping
Statistical
Classifier
ECG
HR
GSR
ST
EMG
RSP
Knowledge Bases:
sensor priority, calibration profile, context data, hypoglycemia symptoms
wireless
Behavioral/physilogical
hypoglycemia symptoms
General
affective states
Meta
information
Noise Reduction
Lowpass and Bandpass Filtering
Spectral Analyse, Discrimination
Feature, Pattern Extraction
Figure 3: Framework of physiological emotion recognition.
!""#
$"""#
!%""#
!"""#
##%""#
#%$&'#
#%$&(#
#%$&)#
#%$&*#
#%$&%#
####!+#
$*""# #
$,""# #
$$""# #
$"""# #
####!$#
####!!#
####!"#
######'#
######(#
######"#
#-%""#
"# $""# +""#
+""#
$%""#
*"""#%"""#,"""#+"""#$"""#!"""#"#
$"""#!%""#!"""#%""#"#
$%"#$""#!%"#!""#%"#"#
,""# %""# *""#
./0#
.10#
.20#
.30#
Position Typical Waveform
Interbeat Interval
Interbeat Interval
Breath Amplitude
Figure 4: Position and typical waveforms of the biosensors:
(a) ECG, (b) RSP, (c) SC, (d) EMG.
3.2 Feature Extraction
In offline condition, we have a variety of choices
for applying signal analysis techniques to obtain rele-
vant features. In the previous work (Kim and Andr
´
e,
2008), we proposed a wide range of physiological fea-
tures from various analysis domains including time,
frequency, entropy, geometric analysis, subband spec-
tra, multiscale entropy, and HRV/BRV in order to
search for the best emotionrelevant features. In the
work, we achieved an average recognition accuracy
of 95% from a naturalistic dataset obtained from a
reliable experiment using a musical induction, which
was not based on any lab setting or any deliberate in-
structions for evoking certain emotions. The recog-
nition accuracy of 95% for four emotions (joy, anger,
sadness, pleasure) connotes more than a prima facie
evidence that there are some ANS differences among
emotions.
For online systems, the choice of features is re-
stricted to those that can be calculated possibly in re-
altime or near realtime at least. Therefore the effec-
tive use of feature selection and realtime signal pro-
cessing techniques plays an important role. Based on
the features in the previous work, we select diabetes-
specific features for the IEM system.
3.3 Mapping Features with Emotions
In addition to the typical driving-relevant emotions
such as anger, stress, anxiety, exciting etc., we
classify physiological and behavioral symptoms of
hypoglycemic events. Driving-relevant emotional
states and hypoglycemic symptoms can be summa-
rized as follows:
Driving-relevant emotions:
- Anger: leads to horn-honking, rapid steering and
accelerating
- Stress (in multiple levels): related to traffic situa-
tion (e.g. rush hour) and other road user.
- Anxiety, calm, excitation etc.
Diabetes-specific emotions:
- Stress: blood sugar release is symptomatic of
stress
- Fear of hypo-/hyperglycemia
- Depression: possibly because of imperfect rela-
tionship between self-care & health, or combina-
tion of acute & chronic stressors.
- Anger, nervous, anxiety
Signs of hypoglycemia:
- Mild: tremor, sweating, tachycardia, nervousness,
heart palpitations, hunger
- Moderate: shaking, dizzy, headache, confusion,
numbness of lips or extremities, cold, clammy
skin, slurred speech, hyperventilation or shortness
of breath
- Severe: disorientation, seizure, coma, uncon-
scious
Based on these factors, we consider a novel emotion
model combined with hypoglycemic symptoms (Fig-
ure 5) for the IEM system.
In addition to the statistical classifiers such as sup-
port vector machines, k-nearest neighbor, neural net-
works, etc. that are commonly used in pattern recog-
nition, we develop a rule-based mapping method
in which we generate rules for mapping particular
features linearly to the change of certain emotional
states. We employ this method especially for recog-
nition of hypoglycemic symptoms, such as shaking,
sweating, cold, tremor, rapid breathing and tachycar-
dia, which can directly be detected by analyzing linear
variation of related biosignals, for example, sweating
by GSR, rapid breathing by RSP, tremor by EMG,
etc. Therefore, the rule-based mapping algorithm can
easily be implemented for realtime system without
HEALTHINF 2010 - International Conference on Health Informatics
370

!"#$%&'($)*+,-./'-
.#,+&')'0&1$)*+,-./'-
#&0#*$('2+$)
)'3*$('2+$)
.'+&/&%"*%$)"41"
4"0$/&%"*%$)"41"
!"#$#%!&
!'&()%*+
#($%,-.#&()/%*+
(*+&#
)(0/10(#,%(
023,
02*)&*)4&*)
)%#&,
!3&&$%*&!!
0(34
521
!/(6%*+
)#&42#
7&(#
,&$#&!!%2*
(*8%&)1
!)#&!!
980%)&4&*)
Figure 5: Discrete emotion model combined with hypo-
glycemia symptoms.
training a classifier. For the other emotions such as
stress, joy, anger, and neutral, the recognition system
needs to be learned from cross-correlated behavior of
features from multichannel biosignals and requires a
training dataset for supervised machine learning. As
a result, we will need to develop a combined classifi-
cation scheme of both rule-based mapping and super-
vised classification in order for recognizing multiple
symptoms and emotional states. An ensemble method
can also be considered for improved recognition ac-
curacy, e.g. classifier ensemble method in which we
classify by using different classifiers and combine the
results from each classifier by using decision-level fu-
sion algorithms such as majority voting, Borda count,
and boosting.
Main challenge in the IEM system is overcoming
possibly overlapping physiological reactions between
hypoglycemic events and common emotional states
and calibrating the biosensors in driving situation.
4 DISCUSSION: IMPACT OF
EMOTIONS ON DIABETES (&
VICE VERSA)
Patient’s emotional needs and problems are an impor-
tant component of treatment and integral component
of diabetes management. The role of emotions in dia-
betes management was observed as early as the seven-
teenth century, when British physician Thomas Willis
noted that diabetes first appeared among patients who
had experienced significant life stresses.
Recently it is widely recognized that negative
emotions such as stress, anxiety, fear, depression,
and sorrow affect the blood glucose level (Surwit and
Schneider, 1993). Patients experiencing such negative
emotional states may have greater difficulty in con-
trolling blood glucose compared to those not suffer-
ing emotional problems. Depression, for example, is
not generally listed as complication of diabetes. How-
ever, it can be one of the most common and dangerous
complications. More importantly, depression under-
mines the motivation of patient to maintain diabetic
management. Diabetics with major depression have a
very high rate of recurrent depressive episodes within
the following five years (Lustman et al., 1997b). In
the study of (Lustman et al., 1997a) it is proven that
effective treatment of depression can improve diabetic
control. Stress can also readily elevate blood glucose
and affects the autonomic nervous system, which in
turn affects the secretory rate of insulin and glucagon
and finally disrupts metabolic control. Stabler and
colleagues (Stabler et al., 1987) found that children
judged to have a ”Type A” personality structure had
an increased blood glucose elevation in response to
stress and children with a calmer disposition had a
smaller glucose rise when stressed. Several studies
have demonstrated a relationship of stress to glycemic
control in samples of patients with Type 1 diabetes
(Inui et al., 1998; Viner et al., 1996). Stress can
be managed, for example, by using behavioral stress
management program such as progressive muscle re-
laxation (PMR), or the administration of anxiolytic
medications. Recently, the study in (Surwit et al.,
2002) supported the efficacy of outpatient stress man-
agement training for the improvement of glycemic
control in patients with Type 2 diabetes. For stress
management training, they used the PMR and medi-
cation instruction methods complementarily. The re-
sult of their experiment showed that at the end of a
1-yea follow-up period, patients who received train-
ing in stress management skills demonstrated approx-
imately a 0.5% reduction in HbA1c relative to control
patients. While positive emotions such as laughter
have been reported to modify the levels of neuroen-
docrine factors involved in negative emotions and to
modulate immune function (Berk et al., 1989; Taka-
hashi et al., 2001), less attention has been so far paid
to impact of positive emotions on diabetes. Through
the observation in (Hayashi et al., 2003) it is firstly
elucidated that laughter can suppress the elevation of
blood glucose level. From their 2-day experiment, it
turned out that the patients with Type 2 diabetes had
a smaller rise in post-meal blood glucose when they
watched a comedy show than when they listened to a
humorless lecture.
IN-VEHICLE MONITORING OF AFFECTIVE SYMPTOMS FOR DIABETIC DRIVERS - In-vehicle Hypoglycemia
Alerting System in EU Project METABO
371

5 CONCLUSIONS
Research on the role of emotions in diabetes is still
challenging work, because literature so far offers
ideas rather than well-defined solutions. In this paper
we presented conceptual scheme of in-vehicle emo-
tion monitoring system for diabetic drivers. Many
works remain to be done in the project METABO.
To achieve our goals in this new area we conceived,
it requires not only a methodological, technical in-
novation but also conceptual changes with workable
thoughts focusing on specific contexts of medical ap-
plications.
ACKNOWLEDGEMENTS
The work described in this paper is funded by the EU
under research grant ICT-216270-METABO.
REFERENCES
Armitage, C. J., Conner, M., and Norman, P. (1999). Dif-
ferential effects of mood on information processing:
evidence from the theories of reasoned action and
planned behaviour. European Journal of Social Psy-
chology, 29:419–433.
Berk, L., Tan, S., Fry, W., Napier, B., Lee, J., Hubbard, R.,
Lewis, J., and Eby, W. (1989). Neuroendocrine and
stress hormone changes during mirthful laughter. Am.
J. Med. Sci., 298(390–396).
Deary, I. (1999). Symptoms of hypoglycaemia and ef-
fects on mental performance and emotions. In Fisher,
B., editor, Hypoglycaemia in Clinical Diabetes, pages
29–54. Chichester, U.K., Wiley.
Gold, A., MacLeod, K., Deary, I., and Frier, B. (1995).
Hypoglycemia-induced cognitive dysfunction in dia-
betes mellitus: effect of hypoglycemia unawareness.
Physiol. Behav., 58:501–511.
Hayashi, K., Hayashi, T., Iwanaga, S., Kawai, K., Ishii, H.,
Shoji, S., and Murakami, K. (2003). Laughter lowered
the increase in postprandial blood glucose. Diabetes
Care, 26:1651–1652.
Inui, A., Kitaoka, H., Majima, M., and et al. (1998). Effect
of the kobe earthquake on stress and glycemic control
in patients with diabetes mellitus. Arch. Intern. Med.,
158:274–288.
James, L. (2000). Road Rage and Aggressive Driving.
Amherst, NY: Prometheus Books.
Kim, J. and Andr
´
e, E. (2008). Emotion recognition based on
physiological changes in music listening. IEEE Trans.
Pattern Anal. and Machine Intell., 30(12):2067–2083.
Lajunen, T. and Parker, D. (2001). Are aggressive peo-
ple aggressive drivers? a study of the relationship
between self-reported general aggressiveness, driver
anger and aggressive driving. Accident Analysis and
Prevention, 33:243–255.
Lustman, P., Griffith, L., Clouse, R., and et al. (1997a). Ef-
fects of nortryptiline on depression and glycemic con-
trol in diabetes: Results of a double-blind, placebo-
controlled trial. Psychosomatic Medicine, 59(3):241–
250.
Lustman, P., Griffith, L., Freedland, K., and Clouse, R.
(1997b). The course of major depression in diabetics.
Gen. Hosp. Psychiatry, 19(2):138–143.
¨
Ohman, A. (2000). Fear and anxiety: Evolutionary, cog-
nitive and clinical perspectives. In Lewis, M. and
Haviland-Jones, J. M., editors, Handbook of Emo-
tions. The Guilford Press, New York.
Stabler, B., Surwit, R., Lane, J., and et al. (1987). Type a
behavior pattern and blood glucose control in diabetic
children. Psychosomatic Medicine, 49:313–316.
Surwit, R. and Schneider, M. (1993). Role of stress in the
etiology and treatment of diabetes mellitus. Psycho-
som. Med., 55:380 –393.
Surwit, R., Tilburg, M. V., Zucker, N., and et al. (2002).
Stress management improves long-term glycemic
control in type 2 diabetes. DIABETES CARE, 25(1).
Takahashi, K., Iwase, M., Yamashita, K., Tatsumoto, Y.,
Ue, H., Kuratsune, H., Shimizu, A., and Takeda, M.
(2001). The elevation of natural killer cell activity in-
duced by laughter in a crossover designed study. Int.
J. Mol. Med., 8:645–650.
Viner, R., McGrath, M., and Trudinger, P. (1996). Family
stress and metabolic control in diabetes. Arch. Dis.
Child., 74:418–421.
HEALTHINF 2010 - International Conference on Health Informatics
372
