
AN AUTONOMIC COMPUTING FRAMEWORK FOR
SELF-MANAGED EMERGENCY DEPARTMENTS
Serene Almomen and Daniel Menascé
Volgenau School of Information Technology and Engineering, George Mason University
4400 University Drive, Fairfax, VA 22030, U.S.A.
Keywords: Autonomic Computing, Healthcare, Emergency Department, Quality of Service, Self-Managed System.
Abstract: The delivery of cost-effective and quality Emergency Department (ED) services remains an important and
ongoing challenge for the healthcare industry. ED overcrowding has become a common problem in
hospitals around the world, threatening the safety of patients who rely on timely emergency treatment.
Despite numerous advances in medical procedures and technologies, EDs continue to experience
overcrowding problems. The combination of increased demand and diminished resources makes optimizing
emergency departments a difficult problem for healthcare decision makers. We examine this problem by
applying an autonomic computing framework for self-managed emergency departments to maintain optimal
Quality of Service (QoS) during its operation. Our work has potential implications in guiding a hospital’s
effort to optimize their emergency department system.
1 INTRODUCTION
In hospitals all over the country, healthcare
emergency departments (ED) are severely
overcrowded resulting in delays in care, difficulty in
providing quality care, patient discomfort and
dissatisfaction, and higher service cost. In addition,
overcrowding also leads to staff burnouts and
inefficient utilization of resources. Many ED nurses
leave for other departments or units as a result of
getting overwhelmed with the ED workload (ACEP,
2010).
The challenges of the ED, including
overcrowding and boarding, have been a subject of a
great deal of discussion. Several meetings, reports,
and research studies have been conducted to
understand the causes, implications and possible
solutions to ED overcrowding and boarding issues.
The ED is one of the most critical units in any
healthcare organization. Consequently, improving
performance of this unit is vital to the success of the
healthcare organization.
Due to the dramatic increase in the cost of
healthcare over the past few decades, researchers
and healthcare professionals examined new ways to
improve efficiency and at the same time reduce
healthcare costs. Simulation tools have assisted
healthcare decision-makers in this endeavour
(Hashimoto & Bell, 2007). Another attempt to
improve the ED system relies in capturing ED
workflow patterns and analyzing these patterns to
create an automated and enhanced ED system design
(Moss & Xiao, 2004). Another approach discussed
the use of workflow technologies and web services
to automate emergency healthcare processes
(Poulymenopoulou, Malamateniou, &
Vassilacopoulos, 2008). That work discussed the
need to provide an appropriate technological
infrastructure for automating and managing the
emergency healthcare processes in both intra- and
inter-organizational services. The implementation of
this approach involves capturing process logic
requirements for healthcare workflow systems with
a view to design a system that is easily adjustable to
process changes and to evolving organizational
structures. Some tools have also been developed for
hospital capacity planning simulation to conduct
both process flow analysis and capacity forecasting
(Mengwasser & Berger, 2009).
The dynamic nature of the ED adds to the
complexity of the problem. Sudden changes to the
workload due to emergencies such as fire, natural
disasters, and terrorist attacks are difficult, if not
impossible, to predict.
Furthermore, the ED environment is complex in
nature. ED systems are composed of a collection of
52
Almomen S. and Menascé D..
AN AUTONOMIC COMPUTING FRAMEWORK FOR SELF-MANAGED EMERGENCY DEPARTMENTS .
DOI: 10.5220/0003138200520060
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 52-60
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

resources including both humans (e.g., doctors,
nurses, and technicians) and equipments (e.g., X-ray
machines and CT-Scan). ED systems also involve
human processes and decision making where
humans in the loop determine how the application
evolves based on their awareness of the situation and
infrastructure. Consequently, there is a need for self-
managing EDs. We examine this problem by
applying an autonomic computing framework for
self-managed EDs to maintain optimal operational
Quality of Service (QoS). Our work has potential
implications in guiding a hospital’s effort to
optimize their emergency department systems.
The rest of the paper is organized as follows.
Section 2 discusses background information on the
proposed approach. Section 3 discusses the
environment of EDs. The next section describes the
autonomic computing framework for EDs. Section 5
discusses different implementation techniques for
the autonomic framework. Finally, Section 6
presents some concluding remarks.
2 BACKGROUND
Computing systems have reached a level of
complexity where traditional IT support that
involves human effort to maintain the systems and
keep them operational is becoming increasingly
challenging. A similar problem was experienced in
the 1920s in telephony before automatic branch
exchanges were introduced to eliminate human
intervention (Mainsah, 2002).
Autonomic computing seeks to enhance the
performance or QoS and at the same time minimize
human intervention. The autonomic computing
paradigm has been inspired by the autonomic
function of the human central nervous system
(Kephart & Chess, 2003). It is the body’s master
controller that monitors changes inside and outside
the body, integrates sensory inputs, and effects
appropriate response (Ashby, 1960). Autonomic
controls in the human body use motor neurons to
send indirect messages to organs at a sub-conscious
level. These messages regulate temperature,
breathing, and heart rate without conscious thought
(Ashby, 1960). The implications for computing are
immediately evident; a network of organized, smart
computing components that give us what we need,
when we need it, without a conscious mental or even
physical effort (IBM, 2010).
Autonomic computing attempts to intervene in
computing systems in a similar fashion to its
biological counterpart. There has been significant
research to create autonomic systems. An example
of such effort is IBM’s MAPE-K (Monitor, Analyze,
Plan, Execute, Knowledge) reference model
(Huescher & McCann, 2008). A similar model is
proposed by Russel and Norvig (2003) in which an
intelligent agent monitors its environment through
sensors and uses the collected data to determine
actions to be performed in the environment (Russel
& Norvig, 2003).
In either model, an autonomic system has a
managed element (such as software or hardware
resources), the organ in the human body, that is
given an autonomic behaviour and an autonomic
manager, the nervous system in the human body,
that monitors the managed element and specifies
actions to be executed by the managed element
(Huescher & McCann, 2008) (Russel & Norvig,
2003). There have been several different
implementations of the MAPE-K model including
autonomic toolkit, ABLE, Kinesthetics eXtreme
(KX), and self-management tightly coupled with
application. The latter implementation is closely
related to the proposed approach discussed in this
paper. Such implementation involves either using an
autonomic middleware framework that offers self-
management properties to applications built on top
of this middleware or through encapsulating tasks in
components and defining self-management and
adaptation in terms of these components (Huescher
& McCann, 2008).
IBM also portrayed four fundamental properties
of self-management: self-configuration, self-
optimization, self-healing, and self-protection.
Briefly, these properties mean that an autonomic
computing system configures itself according to
high-level goals, optimizes its use of resources,
detects and diagnose problems, and protects itself
against malicious attacks and end users who
inadvertently make changes to the system
components such as its software (Huescher &
McCann, 2008). Consequently, any implementation
of autonomic computing systems should realize
these properties.
In addition, studies in the autonomic systems
field describe approaches to plan the changes or
actions to be effected on the managed element of an
autonomic system. Some propose policy-based
adapting planning, architectural models, or process-
coordination approach (Sloman, 1994) (Wise, Cass,
Lerner, Call, Osterweil, & Jr., 2000) (Huescher &
McCann, 2008).
With recent advances in embedded computing,
networking, and related information technologies, it
is now feasible to deploy a variety of sensing
AN AUTONOMIC COMPUTING FRAMEWORK FOR SELF-MANAGED EMERGENCY DEPARTMENTS
53

devices, communication networks and IT services in
the real world. These physical spaces include a
variety of sensors such as optical sensors, RFIDs, as
well as specialized sensors such as people-counters
and load-cells that enable monitoring the state of the
physical world and its activities. These sensors are
connected to communication networks such as
Ethernet, cellular, Bluetooth, and WiFi. (Kim, et al.,
2008). These sensors provide a mechanism to
monitor the different resources of a system. Such
technology makes it even easier to implement
autonomic computing systems in real world
environments.
Another concept that can facilitate the
implementation of autonomic systems in real world
environments is utility functions. Utility functions
express the usefulness of a system to one or more
stakeholders as a function of the attributes of a
system. The concept of utility is one of the methods
used to represent Knowledge in autonomic systems.
A utility function is written as follows:
U = f (x
1
, x
2
, ..., x
n
) (1)
where x
1
, …, x
n
are attributes and the function f
combines these attributes in way that expresses the
usefulness of a system as a function of these
attributes. In general, utility functions are
normalized in the [0,1] range with zero representing
the lowest utility and one representing the highest
utility. It is generally easier to specify a utility
function as a function of several utility functions,
one for each attribute. An example would be where
(2)
the global utility function is a weighted sum of all
the individual utility functions.
Autonomic computing systems use utility
functions as the goal to be optimized. The attributes
in this case are several Quality of Service (QoS)
metric of interest such as response time, throughput,
and availability of the computing resources
(Menasce, Bennani, & Ruan, 2005). As failures and
performance degradations occur, the autonomic
computing system automatically changes its
configuration parameters in a way that maximizes
the utility function for the system. Consequently, the
utility function of an autonomic system can be
written as follows:
U = f (QoS
1
, QoS
2
, ...QoS
n
) (3)
where both the utility function and QoS metrics are
defined by domain experts.
3 EMERGENCY DEPARTMENT
ENVIRONMENT
We interviewed a Director of Emergency Services
and a staff nurse at a Pediatric Emergency
Department to gain a better understanding of the ED
environment. Our findings are summarized in what
follows.
The ultimate goal of an ED is patient
satisfaction, which is normally measured by the
length of stay at the ED. ED length of stay is the
patient time in the ED as follows (Welch, Augustine,
Camargo, & Reese, 2006):
For admitted patient: arrival time to
conversion time
For discharged patients: arrival time to
discharge time
For transferred patients: arrival time to
transfer conversion time
Many QoS metrics are collected and analyzed at
EDs to determine areas of improvement that are
necessary to meet this goal. These QoS metrics can
be time measures or proportion measures (Welch,
Augustine, Camargo, & Reese, 2006). The time
measures include arrival time to first seen by a
doctor, doctor to discharge time, doctor to decision
to admit time, arrival time to rooming, disposition to
discharge, and many others. The proportion
measures include number of patients who left before
they were supposed to, complaints, hospital
diversion, and ED patient flow to name a few. These
measures are commonly referred to as Core
Measures and are often specified by a healthcare
governing body serving local or nationwide
hospitals. These Core Measures data are saved in an
advanced analytical tool where comparative reports
taking into account national averages can then be
generated allowing hospitals to proactively assess
performance and identify opportunities for quality
improvement including potentially preventable
readmissions and complications. These Core
Measures also depend on several Census and
utilization metrics including pediatric patients per
day, high-acuity patients per day, number of self-
paid patients, medication doses administered per 100
patients seen, and service hours per day of
physicians.
There are many critical issues in EDs that
contribute to an unsatisfactory level of these QoS
metrics, many of which are demography-dependent.
Inadequate patient beds always lead to long arrival
to discharge time for example. The lack of an
ultrasound machine may also be critical in an ED
U = w
i
i=1
n
∑
U
i
(x
i
)
HEALTHINF 2011 - International Conference on Health Informatics
54

that expects many pregnancy-related emergencies.
This is an example of a demography-related issue.
Other issues include lack of outpatient psychiatric
service and lack of outpatient programs for referral.
However, we found that lack or resources,
specifically nurse shortage, is a major contributor to
not meeting the overall goal of quick patient
turnaround.
There are compelling reasons to collect and
control ED QoS metrics. Regulatory burdens, ED
operations management, and ED body of knowledge
expansion are some (Welch, Augustine, Camargo, &
Reese, 2006). The Joint Commission on
Accreditation of Healthcare Organizations
(JCAHO), for example,
is pursuing clinical quality
improvement (QI) data in the form of Core
Measures. Any facility that does not have in place
the infrastructure to track these data risks its
accreditation.
In addition, to determine whether ED
process innovations are effective, quality measures
will be required. To date, much QI work goes
unpublished, and therefore ED QI workers are
failing to build a body of research that is pertinent to
operational efficiency.
In an effort to control QoS metrics within an
acceptable range, hospitals in collaboration with
nurse and the physician groups document their ED
standard processes, treatment protocols, and
regulations and orient new staff on them. The
processes take into account national averages of ED
patients’ length of stay and try to stay within or
below that range. In addition, these processes are
evaluated often to accommodate technology
changes, equipment increase, and changes in
practices. Pilots and time audits are sometimes used
to determine the compliance to those processes and
protocols.
To maximize efficiency at the ED, the
Emergency Severity Index (ESI) to classify patients
coming into the ED is used. ESI is a five-level
emergency department (ED) triage algorithm that
provides clinically relevant stratification of patients
into five groups from 1 (most urgent) to 5 (least
urgent) on the basis of acuity and resource needs.
The Agency for Healthcare Research and Quality
(AHRQ) funded initial work on the ESI (AHRQ,
2010).
A triage nurse is responsible for ESI level
assignment to ED patients. The ESI level determines
the waiting time of patients. ESI level 1 patients
have no waiting time for example. In addition, EDs
are divided into care areas or zones based on the
severity of the case treated. Consequently, the ESI
level also determines the zone the patient will
occupy. Level 4-5 patients are often assigned to the
‘fast track’ zone since they usually do not require
many resources before they can be discharged. The
triage nurse is also responsible for zone assignments.
A charge nurse uses the ESI level and zone
assignment for each patient in the ED to determine
the most efficient workflow of the ED. The charge
nurse’s role, consequently, is to run the ED as
efficiently as possible to help minimize patients’
length of stay. In the EDs we visited, the charge
nurse uses a computer application that collects the
QoS metrics as well as patient status to assist in
making decisions on the most efficient workflow at
the ED at any given time. These decisions may
include changing a nurse’s assignment to balance the
workload of ED nurses, task a nurse to dispense
medication if a doctor’s order is ready, start the
hospital admission process for a patient after
doctor’s diagnosis is complete, and request an on-
call nurse to come to the ED if the workload is high.
The staff nurses are assigned patients and take care
of patients once they are in a room at the ED.
It is also important to note that there is no cost
constraint that limits the operation of an ED. In other
words, no patient will ever be turned away because
of insufficient resources. EDs normally have
working agreements with other hospitals in their
area where they can quickly transfer patients to due
to heavy workload or resource shortage. EDs also
use what they call a ‘float pool’ of nurses who can
be used to staff EDs if needed. Nevertheless,
maximizing the efficiency of an ED does reduce the
cost of service.
4 AN AUTONOMIC COMPUTING
FRAMEWORK FOR ED
Our framework involves developing an autonomic
computing system or a self-managed ED system that
can regulate and maintain itself without human
intervention. This is ideal in an ED environment
since the goal is to create a system that will be able
to adapt to a constantly changing environment (such
as patient flow, workload, and resource availability)
in a way that preserves given operational goals (such
as performance goals or QoS goals).
To achieve that, the proposed approach attempts
to implement the MAPE-K (Kephart & Chess, 2003)
model in an ED environment. Within the ED
context, autonomic managers define a control loop
(MAPE-K loop), as shown in Figure 1. Changes are
made through action operations. Sensors look at the
AN AUTONOMIC COMPUTING FRAMEWORK FOR SELF-MANAGED EMERGENCY DEPARTMENTS
55
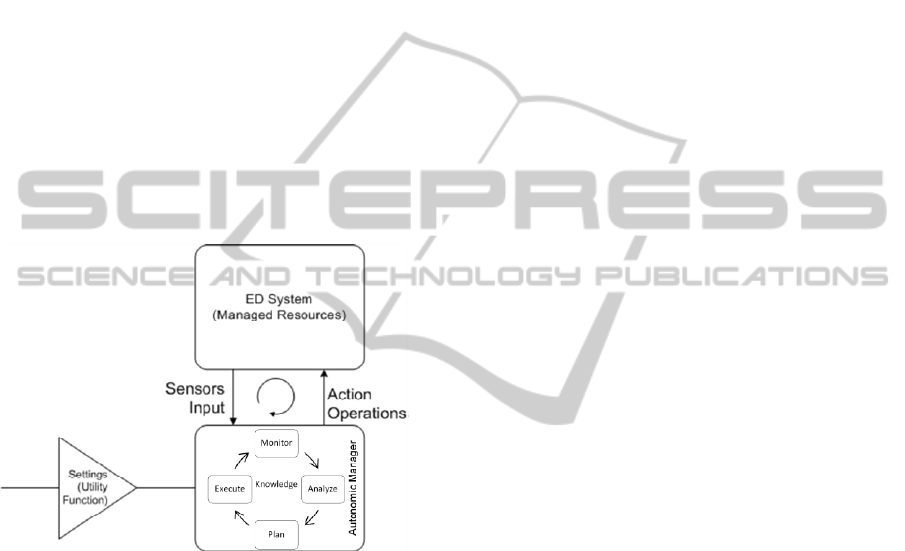
state of the managed ED resources, and action
operations can change the current state. The entire
ED environment is a set of managed resources.
Autonomic managers, just like a charge nurse,
continuously monitor the system and handle events
that need action to be taken. They monitor the ED
environment using inputs from the sensors installed
in the environment and analyze what is found. Based
on the defined utility function of the ED, the
autonomic manager then plans and executes any
specific actions needed to maximize the utility
function. The steps of monitoring, analyzing,
planning, and executing may be executed
concurrently. For example, if the X-ray machine in
an ED is experiencing high utilization, the system
could decide to provision an additional machine.
The system can then return to monitoring, and if
utilization drops, the X-ray machine can be
deprovisioned and made available to other
departments in the hospital.
Figure 1: Autonomic Computing Model for ED.
The ED system depicted in Figure 1 can have a
variety of architectures. It can consist of integrated
applications or components within the ED such as
the pharmacy dispensing application, the scheduling
application, and the resource allocation application.
We also consider a cyber-physical ED system as
including smart devices such as patient wrest
sensors, nurse PDAs, bed sensors, and other devices.
Our approach to self-managed ED systems does
not address the various ED system architectures.
Rather, it assumes a cutting edge system such as a
cyber-physical environment that collects data or
metrics through different sensors and devices to send
to the autonomic manager. Contrary to common
systems in the autonomic computing environments,
the ED system in the diagram consists of human
resources in addition to the hardware and software
resources. This means that doctors and nurses are
considered resources of the system as well as CT-
Scan, X-ray machines, bed sensors, and pharmacy
dispensing application for example.
The ED autonomic manager attempts to optimize
pertinent QoS metrics. One of the metrics, called
wait time ratio and defined as W/T, combines the
average length of stay (T) with the average time (W)
spent by the patient in the waiting area. Other
relevant metrics are patient throughput (X
0
), and
resource utilization (U
i
) for resource i.
The values of these QoS metrics depend on
several of the census and utilization parameters
discussed in section 3 which can be categorized as
workload intensity parameters (e.g., the arrival rate
of patients of a given group) and the service
demands parameters of each group at each resource
(e.g., the average time spent by a patient using the
CT-Scan).
The goal of the ED autonomic system is to find
settings of the managed resources that optimize a
given utility function provided by the domain expert,
which depends on the values of several QoS metrics.
This is important in order to realize the self-
optimization property of an autonomic system. The
autonomic manager uses the provided utility
function to plan appropriate changes or actions to be
effected on the managed resources of the ED. As
mentioned before, utility function may be obtained
by combining utility functions for the different QoS
metrics, such as:
Utility function for the throughput of the ED:
U
X
(X
ED
)
Utility function for the average length of stay,
T, in the ED: U
T
(T)
Utility function for the average time spent by
a patient waiting in the ED: U
W
(W)
Utility function for the wait time ratio W/T:
U
W/T
(W/T)
As an example, Figure 2 shows two utility
functions: one for U
W/T
(W/T) in Figure 2(a) and the
other for U
X
(X
ED
) in Figure 2(b). A global utility
function U
g
is a function of the individual utility
functions U
X
(X
ED
), U
T
(T), U
W
(W), and U
W/T
(W/T):
U
g
= f (U
X
(X
ED
), U
T
(T), U
W
(W),
U
W/T
(W/T)).
(4)
HEALTHINF 2011 - International Conference on Health Informatics
56
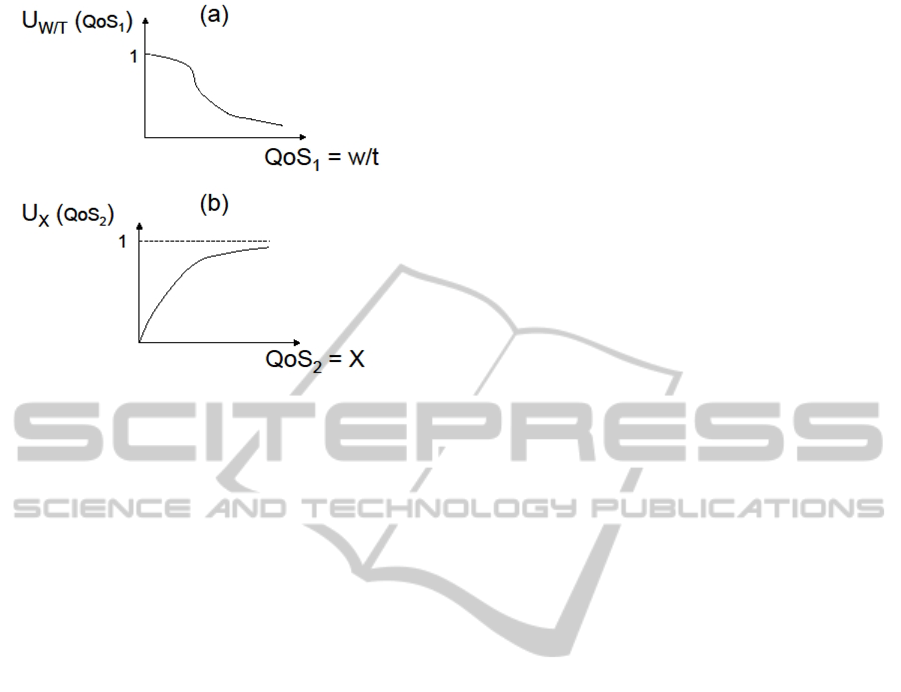
Figure 2: Example of Utility Functions.
5 IMPLEMENTATION
TECHNIQUES
There are two main approaches to implementing
autonomic computing systems; model-driven based
on system performance models and data-driven
based on reinforcement learning. In what follows,
we describe the two approaches to autonomic
computing implementation and illustrate how one
model-driven technique, the queuing-theoretic
model, can be applied in the context of the ED.
5.1 Model-driven Approach
The model-driven approach relies on being able to
build models that can be used to predict the values
of a system’s QoS metrics as a function of its
configuration parameters and resource sharing
policies. Parameter and policy optimization
techniques need to be defined in this approach. The
parameter and policy optimization techniques map
system states to action operations, hence, are used to
plan the changes to the autonomic system to
maximize its utility function (Gracanin, Bohner, &
Hinchey, 2004).
Model-driven approaches focus on algorithms
that make use of explicit system performance
models such as queuing-theoretic or control-
theoretic models.
Using a model-driven approach to autonomic
computing makes it possible to generate run-time
models that reflect the current state of the system
without the unnecessary dependency on the system
platform (Rohr, Boskovic, Giesecke, & Hasselbring,
2006). This capability makes this approach possible
to adapt in implementing dynamic and complex
autonomic systems such as the ED system.
However, the design and implementation of accurate
performance models of complex computing systems
can be highly knowledge-intensive and labour-
intensive and may require original research
(Tesauro, Jong, Das, & Bennani, 2006).
5.2 Data-driven Approach
The data-driven approach focuses on knowledge-
free trial-and-error methodology in which a learner
tries various actions in numerous system states, and
learns from the consequences of each action
(Tesauro, Jong, Das, & Bennani, 2006). This
approach is also referred to as Reinforcement
Learning (RL). RL has successful applications in
Markov Decision Process (MDP) in which RL can
potentially learn decision-theoretic optimal policy in
dynamic environments where the effects of actions
are stationary and history-independent. RL has
successful implementation in real-world problems
such as helicopter control and financial markets
trading (Tesauro, Jong, Das, & Bennani, 2006).
Contrary to the model-driven approach, RL does
not require an explicit model of the computing
system. In addition, RL has the capability to
properly react to dynamical phenomena in an
environment due to its roots in sequential decision
theory. Other methods tend to treat dynamical
effects only approximately or ignore them all
together, or deal with the decision making problem
as a series of unrelated instantaneous optimization
(Tesauro, Jong, Das, & Bennani, 2006). Thus, RL is
a possible implementation approach in autonomic
computing.
The use of RL in real-world applications such as
an ED system, however, can suffer from poor
scalability in large state spaces since a lookup table
is used to store a separate value for every possible
state-action pair. The size of such a table increases
exponentially with the number of state variables of
the system making it challenging to use in real
applications (Tesauro, Jong, Das, & Bennani, 2006).
In addition, poor performance in live systems
implementing this approach can be observed due to
the long learning periods that may be necessary.
AN AUTONOMIC COMPUTING FRAMEWORK FOR SELF-MANAGED EMERGENCY DEPARTMENTS
57
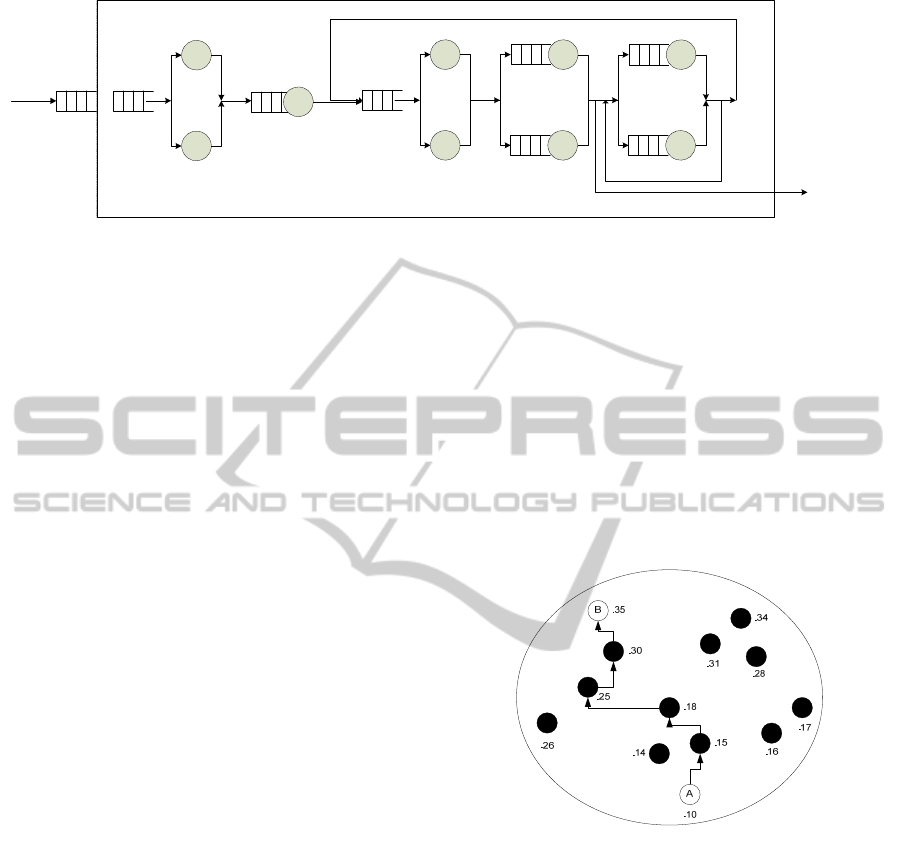
Figure 3: Example of ED QN Model.
5.3 Model-driven Implementation
in the ED
The work by Menascé and Bennani (2003) describes
creating autonomic computing models for computer
systems based on the notion of queuing network
(QN) models (Menascé & Bennani, 2003). Much
like computer systems, an
ED has many shared
resources (e.g., beds, X-ray machines, doctors, and
nurses). The performance of such a system can,
hence, be conveniently represented by a Queuing
Network (QN) model that represents the flow of
patients and their contention for these resources.
When a patient arrives at the ED for treatment, the
patient alternates using the different resources in the
ED such as the nurse, bed, and X-ray machine, quite
likely more than once. At any point in time, a patient
can be treated by a nurse and another using the X-
ray machine, while other patients are waiting to be
treated by the nurse or use the X-ray machine. Thus,
the nurse and X-ray machine can each be
characterized as a queue with a waiting line. An
example of a QN model of an ED system is
illustrated in Figure 3. In the diagram, the different
resources of the system are represented by queues.
This is a common representation in computer
systems that our approach may adapt for self-
managed ED systems including humans as
resources. For example, nurses, doctors, and X-ray
technicians are resources used by patients who flow
through the system as indicated in Figure 3. The
flow of a patient from one resource to another gives
this model the network nature.
Some parameter and policy optimization
approaches commonly used for QN models are hill
climbing and beam-search algorithm among others.
These approaches are referred to as combinatorial
search techniques. The use of exhaustive searches of
all possible configurations of the ED system is not
feasible due to the complexity of such systems.
Consequently, using a combinatorial search
technique will find a close-to-optimal configuration
so that the utility function of the new configuration
is as close as possible to the desired QoS level
(Babaoglu, et al., 2005) (Menasce, Bennani, &
Ruan, 2005). In this case, the ED autonomic
manager will use combinatorial search techniques
such as hill-climbing to find the close-to-optimal
configuration. A state space represents possible
configurations of the system, as shown in Figure 4.
Each point in the space represents a configuration of
controlled parameters and the numerical value
associated with each point represents the value of
the utility function.
Figure 4: Example of State Space Search.
The figure shows that the current configuration is
point A with value .10, which is obtained by
computing the utility function using the
measurements obtained from the sensors in the ED
system. Through hill-climbing search, all
‘neighbour’ configurations are examined and a new
configuration with the highest value of the utility
function is selected. The search is repeated at each
new point visited until either the value of the QoS
does not improve, or a threshold on the number of
points traversed has been exceeded. Through hill-
climbing, a new close-to-optimal configuration,
point B with value .35, is found. The value of any
point in the search space can be computed through
the use of QN models that can predict the value of
the ED QoS metrics for configurations different than
1
K
1
M
1
N
………….
………….
………….
Doctor
X-ray
Technician
Discharge
Staff Nurse
Waiting Area
Emergency Department
1
Triage Nurse
Charge Nurse
1
J
………….
HEALTHINF 2011 - International Conference on Health Informatics
58

the current one. The QoS values are then used to
compute the value of the utility function for that
point in the search space.
The configuration parameters for each point in
the space can be represented as v=(v
1
, …,v
m
). As an
example, in the ED, possible configuration
parameters to be changed by the autonomic
controller are: the maximum number of doctors
(M
D
), the maximum number of nurses (M
N
), the
queuing discipline at the X-ray machine (d
X-ray
), and
the queuing disciplines at the CT-Scan (d
CT-Scan
).
Thus, the configuration point can be defined as
v=(M
D
,
M
N
, d
X-ray
,
d
CT-Scan
). Based on these
parameters, the combinatorial search technique of
choice will start at the current configuration C
0
,
examine all the neighbour configurations to C
0
and
move to the one with the highest QoS value. A
neighbour configuration is defined as one in which
the parameters values of M
D
, and M
N
changes by ±1
and the parameter values of d
X-ray
, and d
CT-Scan
changes from First Come First Served (FCFS) or
Priority Queuing, for example. The search is
repeated at each new point until either the value of
utility function does not improve, or a threshold on
the number of points traversed has been exceeded.
The autonomic manager will then send an action
operation comprised of the new optimal
configuration to the ED system to change the ED’s
current configuration in order to achieve improved
operations and decreased service cost.
6 CONCLUDING REMARKS
Inspired by biology, autonomic computing has
evolved as a discipline to create software systems
and applications that self-manage in an attempt to
overcome the complexities and inability to maintain
current and emerging systems effectively.
The implementation of autonomic computing has
been increasingly emerging in fields including
power management, data centers, clusters, and
GRID computing systems, and ubiquitous
computing. These applications are already
demonstrating their feasibility and value (Huescher
& McCann, 2008). However, there is no evidence
that autonomic computing has been implemented in
healthcare Emergency Department (ED) systems
where not only hardware and software comprise the
system resources, but also human beings. Our
framework extends the autonomic computing
concepts to create a self-managed ED system to
reduce the dependency on human intervention to
maintain such a complex system, thus, improve the
ED operations, and decrease the ED service cost.
We are currently in the process of investigating a
live implementation of the framework proposed in
this paper in an ED environment. Specifically, we
plan to compare the results on an ED with and
without an autonomic computing system in order to
investigate whether performance and cost
improvements can be obtained.
REFERENCES
ACEP, 2010. Meeting the Challenge of Emergency
Department Overcrowding/Boarding. Washington:
American College of Emergency Physicians.
AHRQ. (2010). Emergency Severity Index, Version 4.
Retrieved October 20, 2010, from Agency for
Healthcare Research and Quality: http://
www.ahrq.gov/research/esi/esi1.htm
Ashby, W. R., 1960. Design for a Brain. Chapman & Hall
Ltd.
Babaoglu, O., Jelasity, M., Montresor, A., Fetzer, C.,
Leonardi, S., Moorsel, A. v., et al., 2005. Self-Star
Properties in Complex Information Systems. Springer
Verlag: Lecture Notes in Computer Science.
Gracanin, D., Bohner, S. A., & Hinchey, M., 2004.
Towards a Model-Driven Architecture for Autonomic
Systems. Proc. 11th IEEE Intl. Conf. Engineering of
Computer-Based Systems, (pp. 500-505).
Hashimoto, F., & Bell, S., 2007. Improving Outpatient
Clinic Staffing and Scheduling with Computer
Simulation. Journal of General Internal Medicine ,
182-184.
Huescher, M. C., & McCann, J. A., 2008. A survey of
Autonomic Computing—Degrees, Models,and
Applications. New York: ACM.
IBM, 2010. Autonomic Computing - The Solution.
Retrieved June 30, 2010, from Autonomic Computing:
http://www.research.ibm.com/autonomic/index.html
Kephart, J., & Chess, D. (2003). The Vision of Autonomic
Computing. IEEE Internet Computing , 41-50.
Kim, M., Massaguer, D., Dutt, N., Mehrotra, S., Ren, S.,
Stehr, M.-O., et al. (2008). A Semantic Framework for
Reconfiguration of Instrumented Cyber Physical
Spaces. St. Louis: IEEE.
Mainsah, E., 2002. Autonomic computing: The next era of
computing. Electronic Communications Engineering
Journal , 14, 1, 2–3.
Menascé, D. A., & Bennani, M. N., 2003. On the Use of
Performance Models to Design Self-Managing
Computer Systems. Computer Measurement Group
Conference. Dallas: Computer Measurement Group.
Menascé, D. A., Bennani, M. N., & Ruan, H., 2005. On
the Use of Online Analytic Performance Models in
Self-Managing and Self-Organizing Computer
Systems. Springer Verlag: Lecture Notes in Computer
Science.
AN AUTONOMIC COMPUTING FRAMEWORK FOR SELF-MANAGED EMERGENCY DEPARTMENTS
59

Menascé, D., Almeida, V., & Dowdy, L., 2004.
Performance by Design: Computer Capacity Planning
by Example. Upper Saddle River: Pearson Education,
Inc.
Mengwasser, M. J., & Berger, M. A., 2009, February.
Hospital Capacity Planning Model. Noblis Sponsered
Research Projects , pp. 20-21.
Moss, J., & Xiao, Y., 2004. Improving Operating Room
Coordination: Communication Pattern Assessment.
The Journal of Nursing Administration , 93-100.
Poulymenopoulou, M., Malamateniou, F., &
Vassilacopoulos, G., 2008. Emergency healthcare
process automation using workflow technology and
web services. Athens: Informatics for Health and
Social Care.
Rohr, M., Boskovic, M., Giesecke, S., & Hasselbring, W.,
2006. Model-driven Development of Self-managing
Software Systems. Proc. 9th Intl. Conf. Model-Driven
Engineering Languages and Systems. Springer.
Russel, S., & Norvig, P., 2003. Artificial Intelligence: A
Modern Approach 2nd Ed. Prentice Hall.
Sloman, M., 1994. Policy driven management for
distributed systems. J. Netw. Syst. Manag.
Tesauro, G., Jong, N. K., Das, R., & Bennani, M. N.,
2006. A Hybrid Reinforcement Learning Approach to
Autonomic Resource Allocation. 3rd IEEE
International Conference on Autonomic Computing
(ICAC), (pp. 65-73). Dublin, Ireland.
Welch, S., Augustine, J., Camargo, C. A., & Reese, C.
(2006). Emergency Department Performance
Measures and Benchmarking Summit. Academic
Emergency Medecine , 1074–1080.
Wise, A., Cass, A. G., Lerner, B. S., Call, E. K.,
Osterweil, L. J., & Jr., S. M., 2000. Using Little-JIL to
coordinate agents in software engineering. Automated
Software Engineering. ASE.
HEALTHINF 2011 - International Conference on Health Informatics
60
