
TISSUE HEATING DUE TO ENDOCARDIAL LEADS DURING
MRI SCANS
Numerical Models and Experimental Validation
Eugenio Mattei, Giovanni Calcagnini, Michele Triventi, Federica Censi, Pietro Bartolini
Italian National Institute of Health, Department of Technology and Health, Rome, Italy
Veronica Piacentini and Stefano Pisa
Department of Electronic Engineering, Sapienza University of Rome, Rome, Italy
Keywords: Endocardial Leads, Magnetic Resonance Imaging, Heating, Numerical Models.
Abstract: Magnetic Resonance Imaging (MRI) tissue heating due to implanted leads represents a major concern for
the safety of patients bearing metallic devices. In this work temperature measurements were performed to
validate the typical solutions adapted as endocardial lead models, that are a thin bare metal wire and an
insulated one. Both experimental and numerical analysis was performed in the frequency range between
10kHz and 128MHz ( frequencies of the gradient and RF fields of MRI systems). We found that the bare
wire is not a reliable model to study the RF heating locally induced at the lead tip. At low frequencies
(<1MHz), the PM lead can be properly modelled as an insulated thin metal wire, providing that the actual
resistivity of the lead is also modelled. As frequency increases, such a model becomes less accurate and
different solutions must be adopted.
1 INTRODUCTION
In the last years the number of patients with
implantable devices, such as pacemakers (PM),
cardioverter/defibrillators (ICD), deep brain
stimulators (DBS) has notably increased. These
patients are today considered strongly
contraindicated to undergo magnetic resonance
imaging (MRI) examinations. This is mainly due to
the hazards that the radiofrequency (RF) field and
the gradient field may represent for the implanted
patient. The energy of the MRI field can couple into
conductive leads, like that used for implantable
devices, in two major ways: 1) the conductive lead
acts as an antenna capable of receiving and
supporting the field, and this mechanism can create
the resonant waves (Pisa et al, 2008); 2) the implant
acts as an electrical ‘short circuit’ to the electrical
potentials induced within the body by the RF field
(Konings et al, 2000). Each of these effects may
create at the lead-tissue interface high electrical
current density which, combined with the high
electrical resistance of most of the biological tissues,
can cause local resistive heating. This power
deposition in tissues, that results in an increased
local absorption rate (SAR) and consequently in
temperature growing, is potentially harmful to the
patient; an excessive temperature growth may bring
living tissues to necrosis and to death. In addition,
the induced currents that flow from the implant into
the body may cause unwanted stimulation of
excitable tissues, such as muscles or nerves. In this
field, in-vivo studies are difficult to carry out for
practical and ethical reasons, whereas computational
techniques represent a favourable choice for testing
the safety of implantable devices within an MRI
environment. However, numerical studies often
implies some simplifications of the actual physical
model that is studied, which may affect the validity
and generality of the results. For this reason,
numerical studies always need to be firmly
anchored in reality and have to be validated by
experimental measurements. The aim of this paper is
the validation, through experimental measurements
of the induced heating, of the model of an
endocardial lead. The analysis was performed in the
RF range between 10kHz and 500kHz (frequencies
of the MRI gradient fields), between 32MHz and
378
Mattei E., Calcagnini G., Triventi M., Censi F., Bartolini P., Piacentini V. and Pisa S..
TISSUE HEATING DUE TO ENDOCARDIAL LEADS DURING MRI SCANS - Numerical Models and Experimental Validation.
DOI: 10.5220/0003163503780381
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2011), pages 378-381
ISBN: 978-989-8425-37-9
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

128MHz (frequencies of the MRI RF fields). The
most commonly used lead models, as thin bare metal
wire or thin insulated metal wire, are first
considered. In addition, since in clinical practice
endocardial leads may not always have a negligible
resistive impedance, a new model that takes into
account a finite electrical conductivity of the lead is
proposed.
2 METHODS AND MATERIALS
The RF behaviour of an endocardial lead was first
validated in terms of induced heating at the tip
versus the two typical models used to represents
leads in numerical studies: a thin bare metal wire
and an thin insulated metal wire. The same structure
has been considered both numerically and
experimentally. This provided us with a direct mean
for validating the results of the numerical analysis,
thus reducing the number of variables typically
involved in other validation procedures. Due to the
wide frequency range covered by the analysis
(10kHz-128MHz), two experimental set-ups were
designed and then reproduced as numerical models:
a low-frequency (LF) set-up and a high-frequency
(HF) set-up.
2.1 Experimental Setups
2.1.1 LF setup (10kHz, 100kHz, 500kHz)
The lead was placed inside a 20cm x 14cm x 30cm
PVC box filled with gelled saline material (HEC
2%, NaCl 0.16%) that mimics the electrical and the
thermal properties of human tissues at the
considered frequency. The measured conductivity
for the gel was 0.2 S/m. A density of 1006 kg/m
3
, a
thermal conductivity equal to 0.2 W/(m·K) and a
specific heat of 4178 J/(kg·K) have been provided
by the HEC manufacturer.
The current was injected directly into the lead
by applying a voltage gap between one end of the
lead and a metallic electrode placed on a wall of the
PVC box. The temperature increase caused by the
current at the lead tip-gel interface was measured by
using a fluoroptic® thermometer (Luxtron model
3100) with SMM probes placed in transversal
contact with the lead tip (Mattei et al, 2007). These
plastic fiber probes (1mm diameter) have an
accuracy of 0.1°C and operated at 8 samples per
second. Temperature measurements were performed
at the tip of a PM unipolar lead (Hepta 2, Sorin
Biomedica) and at the tip of the two simplified lead
models: a 20-cm long thin bare metal wire
(radius=1 mm) and the same wire but with an
insulation sheath. A constant current of 40 mA rms
was injected in the leads at the different frequencies
of interest (10kHz, 100kHz, 500kHz), for a period
of 300s. The amplitude of the current as well as the
voltage at the gap between the lead and the
electrode on the box was measured in real-time
during the experiments.
2.1.2 HF setup (32 MHz, 64MHz, 128MHz)
For the higher frequencies we designed an
experimental set-up that allowed us to measure the
RF current all along the lead. The three leads were
placed inside a PVC tube (radius=2cm;
height=30cm) filled with the same gel previously
described, but with a conductivity of 0.6 S/m. The
RF signal, was applied between the lead and an
electrode placed on one end of the PVC tube, at the
frequency of 32MHz, 64MHz, 128MHz. The current
flowing inside the lead and the gel was measured by
using a clamp current probe (BCP512, A.H. System,
CA). This set-up allows to test the lead in a
condition similar to the implant, but since the current
probe is not submersible, we were forced to measure
the total current crossing a section containing the
lead and the surrounding gel. The temperature
increase was measured with the amplitude of the RF
signal set to have always the same current value of
40mA rms at the lead tip. In addition, we measured
the current amplitude in seven positions along the
tube (at 0cm, 5cm, 10cm, 15cm, 20cm, 25cm - lead
tip, 30cm), so to have an estimation of the current
amplitude distribution at the frequencies of 1MHz,
32MHz, 64MHz, 128MHz. Finally, temperature VS
current curves were calculated for the PM lead and
the two simplified models, in order to relate the
temperature increase measured at the led tip to the
amount of current flowing into the tissue.
2.2 Numerical Models
2.2.1 LF setup (10kHz, 100kHz, 500kHz)
Numerical simulations have been performed using a
commercial software, CST studio 2008, based on the
Finite Integral Technique. The experimental set-ups
were faithfully reproduced in the numerical
environment: the bare wire was modelled as a metal
thin conductor (radius=1mm), while the insulated
wire was modelled as the same wire with a rubber
insulation (thickness=1mm). In order to define a
new model that could better reproduce the behaviour
of an actual endocardial lead, we measured the
TISSUE HEATING DUE TO ENDOCARDIAL LEADS DURING MRI SCANS - Numerical Models and Experimental
Validation
379
electrical parameters of the PM lead with an LCR
meter and we found an impedance of about 50 Ohm.
This impedance is likely to be localized at the lead
tip, that is generally made of conductive ceramic
materials. For this reason, the insulated wire was
modified by adding at its end a cylindrical tip with
radius and height both of 1mm and with electric
conductivity σ=6.37 S/m. It results in a resistance of
about 50 Ohm. The same voltage measured in the
experimental tests was applied in the model, to
ensure the comparability between experimental and
numerical data.
2.2.2 HF set-up (32MHz, 64MHz, 128MHz)
As for the LF measurements, also the HF
experimental set-up was faithfully reproduced in the
CST environment. In this case, the excitation was
applied in terms of current injected into the leads.
The amplitude of the current was chosen to match
the experimental value measured at one end of the
lead when the current at the tip was 40 mA rms.
3 RESULTS
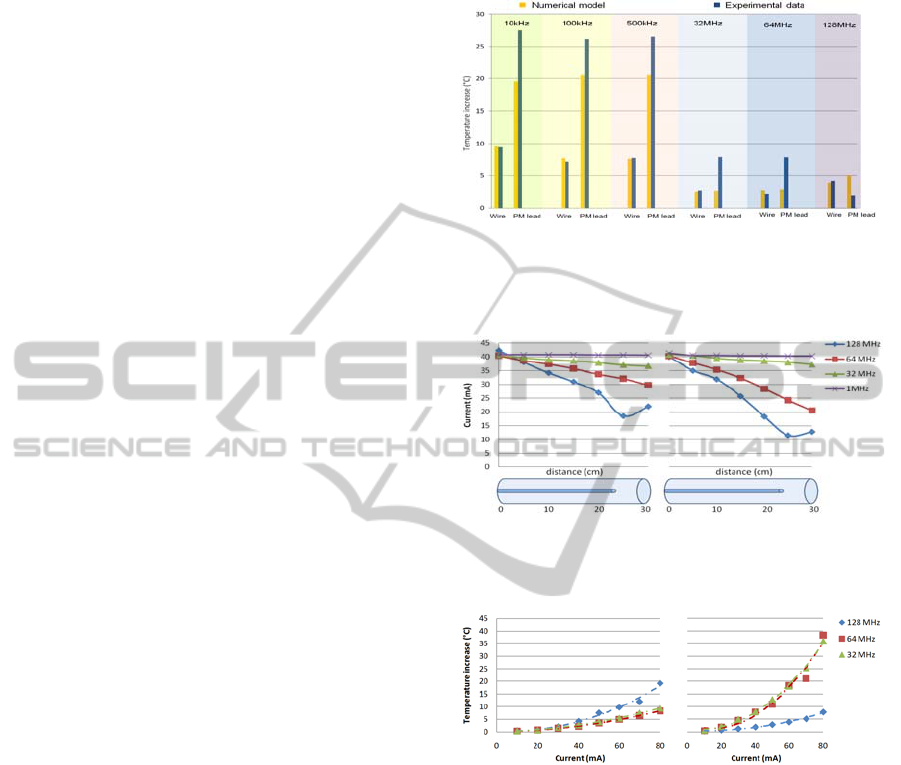
Both in experimental and simulated measurements,
the bare wire showed temperature increases at its tip
comparable with the resolution of the Luxtron
thermometer (0.1°C). The temperature increments
obtained from experimental and simulated data are
reported in Figure 1, both for LF and HF. For each
frequency, two couples of bars are reported: the first
one compares the heating at the tip of the insulated
wire, (experimental versus numerical); the second
one compares the temperature increase measured at
the tip of the PM lead (experimental) to that of the
50 Ohm-tip insulated wire (numerical). Figure 2
shows the current distributions measured along the
PVC tube used for HF experiments. Up to 32MHz,
no significant changes in the current amplitude were
observed from the beginning of the tube to its end.
At higher frequency, a downward trend is noticed,
so that the current at the tip is much smaller than the
one applied at the other end of the lead. At 128
MHz, the minimum for the current amplitude was
observed at 25 cm from the tube end (position of the
lead tip), afterwards the current start increasing. The
same behaviour was observed both for the PM lead
and the insulated wire, even if the decrease in
current amplitude as frequency increases was more
evident for the former than the latter. In Figure 3 the
current VS temperature curves are reported. The
current amplitude reported on the X-axis is
measured at the lead tip. As expected from the
relation between SAR and E field, a quadratic trend
was found (R
2
>0.95).
Figure 1: Comparison between experimental an numerical
temperature increases measured at the tip of the insulated
metal wire and of the PM lead. The numerical model of
the PM lead refers to the 50Ohms insulated wire.
Figure 2: Current amplitude distribution along the PCV
tube used for HF temperature measurements. Left panel:
insulated metal wire. Right panel: PM lead.
Figure 3: Current VS Temperature curves for the insulated
metal wire (left panel) and the PM lead (right panel).
Current values were measured inside the PVC tube, at the
section corresponding to the lead tip.
4 DISCUSSION
The bare wire represents the simplest way to model
an endocardial lead. However, our data show that it
cannot be considered a reliable solution to
investigate the RF induced heating in human tissues.
The absence of an insulation sheath produces a more
uniform power deposition along the wire, so that the
local heating at the lead tip becomes not significant.
A thin metal wire insulated by a rubber sheath is the
typical solution adopted both in experimental and
numerical studies dealing with RF induced heating
BIODEVICES 2011 - International Conference on Biomedical Electronics and Devices
380

on implanted leads (Bassen et al, 2007). We
compared this model with an actual PM lead. First
of all, we compared the temperature increase
measured at the tip of an insulated metal wire with
its equivalent numerical model: very good
agreement between simulated and experimental
results was found, for all the frequencies of interest
(10kHz-128MHz). In the LF range, temperature
increases measured at the tip of the PM lead are
much higher than for the insulated wire (more than
three times higher), for the same excitation
conditions. Numerical simulations show that an
improvement of the lead model can be achieved
considering the actual resistivity of the lead: when
modelling a wire with a finite-conductivity tip, the
gap from the real PM lead becomes significantly
lower (<28% respect to the experimental value). The
lead impedance is a characteristic that can sensibly
vary from lead to lead, mainly depending on the
properties of the tip material, When it is made of
ceramic components (such us pyrolitic carbon), the
resistivity is close to 50 Ohm, whereas, in case of
metallic materials, it goes down to few Ohm or even
less. In any case the lead manufacturers should
indicate the value of the impedance in the technical
notes of their products; thus, it should be an easy
element to take into account. At higher frequencies
(32MHz, 64MHz, 128MHz), marked differences
between the PM lead and its numerical model are
observed, even when modelling the finite-
conductivity tip wire. In particular, at 128MHz, the
temperature increase at the PM lead tip, which up to
64MHz is always higher than the insulated wire,
becomes lower. It suggests that at higher frequencies
other mechanisms play an important role in the heat
generation process, that the simple model of an
insulated wire cannot take into account. To better
understand this aspect, we measured the current
peak distribution along the lead. The higher is the
frequency, the closer is the length of the lead to the
theoretical resonance value inside the gel. At
128MHz the theoretical resonance length is about
23cm for a dipole inside a dielectric mean with a
permittivity of about 25. In such conditions, a kind
of resonant wave can be supposed inside the lead. A
resonance phenomenon in various kinds of linear
structures (e.g. catheters used in interventional
radiology) has been hypothesized also by other
groups (Nitz et al, 2001). Heating induced by the
same current measured at the section of the tip
shows opposite trend with increasing frequency in
the insulated wire and in the PM lead. This is a
further confirmation that, at high frequencies, the
simplified model of the insulated wire moves far
from the actual behaviour of the PM lead. Thus, in
order to obtain reliable results new and more
realistic models must be developed. For example, as
already proposed by some groups (Helfer et al,
2006, Neufeld et al, 2009), a model able to
reproduce the actual inductance of the lead may
represent a substantial improvement of the analysis.
5 CONCLUSIONS
Our study reveals that at frequency below 1 MHz,
the RF–induced heating on endocardial leads can be
properly evaluated by modelling the lead as an
insulated wire. It is however necessary to take into
account the resistivity of the lead, in particular the
resistivity of the tip. At higher frequencies this
model becomes less reliable and new solutions
which consider also other aspects, such as the lead
inductance, must be adopted.
REFERENCES
Bassen H., Kainz W., Mendoza G., Kellom T. MRI-
induced heating of selected thin wire metallic
implants-- laboratory and computational studies--
findings and new questions raised. Minim Invasive
Ther Allied Technol. 2006;15(2):76-84.
Helfer J. L., Gray R.W., MacDonald S.G., Bibens T.W..
Can pacemakers, neurostimulators, leads, or guide
wires be MRI safe? Technological concerns and
possible resolutions. Minim Invasive Ther Allied
Technol. 2006;15(2):114-20.
Konings M. K., Bartels L. W., Smits H. F., Bakker C. J..
Heating around intravascular guidewires by resonating
RF waves. J Magn Reson Imaging. 2000 Jul;12(1):79-
85.
Mattei E., Triventi M., Calcagnini G., Censi F., Kainz W.,
Bassen H. I., Bartolini P. Temperature and SAR
measurement errors in the evaluation of metallic linear
structures heating during MRI using fluoroptic®
probes. Physics in Medicine and Biology, 2007 Mar
21;52(6):1633-46.
Neufeld E, Kühn S., Szekely G., Kuster N. Measurement,
simulation and uncertainty assessment of implant
heating during MRI. Phys Med Biol. 2009 Jul
7;54(13):4151-69.
Nitz W. R., Oppelt A., Renz W., Manke C., Lenhart M.,
Link J. On the Heating of linear conductive structure
as Guide Wires and Catheters in Interventional MRI,
Journal of Magnetic Resonance Imaging 2001, 13
105-114.
Pisa S., Calcagnini G., Cavagnaro M., Piuzzi E., Mattei E.,
and Bernardi P, "A study of the interaction between
implanted pacemakers and the radio-frequency field
produced by magnetic resonance imaging apparatus",
IEEE Trans. Electromag. Compat., vol. 50, no. 1, pp.
35-42, February 2008.
TISSUE HEATING DUE TO ENDOCARDIAL LEADS DURING MRI SCANS - Numerical Models and Experimental
Validation
381
