
THE NATURE OF MEDICAL DEVICE SERVICES
A Multiple-case Study
Christian Mauro, Helmut Krcmar
Information Systems, Technische Universität München, Boltzmannstr. 3, 85748 Garching, Germany
Jan Marco Leimeister
Information Systems, Universität Kassel, Nora-Platiel-Str. 4, 34127 Kassel, Germany
Keywords: Service Oriented Device Architecture, SODA, Service Oriented Architecture, SOA, Medical Devices.
Abstract: The integration of medical devices into the IT infrastructure of hospitals is still a major challenge. Recent
research tries to adapt service oriented concepts to the field of medical devices in order to achieve an easier
and better integration. However, no generalized framework for this kind of integration exists. The purpose
of this paper is to identify the characteristics (the nature) of medical device services. The results were
achieved by conducting a multiple-case study with three cases on two university hospitals. As a result, we
identified twelve specific integration issues of medical devices and deduced eight characteristics. This paper
contributes to the design of a generalized framework for the service oriented integration of medical devices.
The identified characteristics can be interpreted as requirements to such a framework.
1 INTRODUCTION
The integration of medical devices into the IT
infrastructure of hospitals is still an open issue
(Lesh, Weininger, Goldman, Wilson, & Himes,
2007). There is a huge gap between reality and the
vision of seamless healthcare with horizontally and
vertically integrated healthcare processes enabled by
seamless IT support (Schweiger, A., Sunyaev, A.,
Leimeister, J. M., & Krcmar, H., 2007). In order to
bridge this gap several research projects are
exploring the concept of service oriented device
integration. The idea of this concept is the
encapsulation of devices as services, analogous to
enterprise services in service oriented architectures
(SOA) (de Deugd, Carroll, Kelly, Millett, & Ricker,
2006).
As we showed with a literature analysis, some first
prototypical implementations achieved promising
results (Mauro, C., Sunyaev, A., Leimeister, J. M.,
& Krcmar, H., 2009). However, we also revealed
that there is a lack of generalized concepts. In
particular, a general framework for the service
oriented integration of medical devices is missing.
Following a design science approach (according
to Hevner, March, Park, and Ram (2004)), the aim
of our research is to design, implement and evaluate
such a framework. This paper presents an important
step of this research, the exploration of the
characteristics (the nature) of medical device
services. This list of characteristics can be
interpreted as requirements to the integration
framework.
2 SERVICE ORIENTED
INTEGRATION OF LEGACY
SYSTEMS AND DEVICES
From an integration point of view, legacy systems
and medical devices have some common
characteristics (cf. Bennett (1995, p. 19), Bisbal,
Lawless, Bing, & Grimson (1999, p. 103), and Lesh,
et al. (2007)):
Slow hardware doesn’t allow the use of
modern software communication frameworks.
A lack of clean interfaces complicates the
integration with other systems.
A difficult (or impossible) expandability
doesn’t allow modifications of insufficient
interfaces.
250
Mauro C., Krcmar H. and Leimeister J..
THE NATURE OF MEDICAL DEVICE SERVICES - A Multiple-case Study.
DOI: 10.5220/0003172002500255
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2011), pages 250-255
ISBN: 978-989-8425-37-9
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
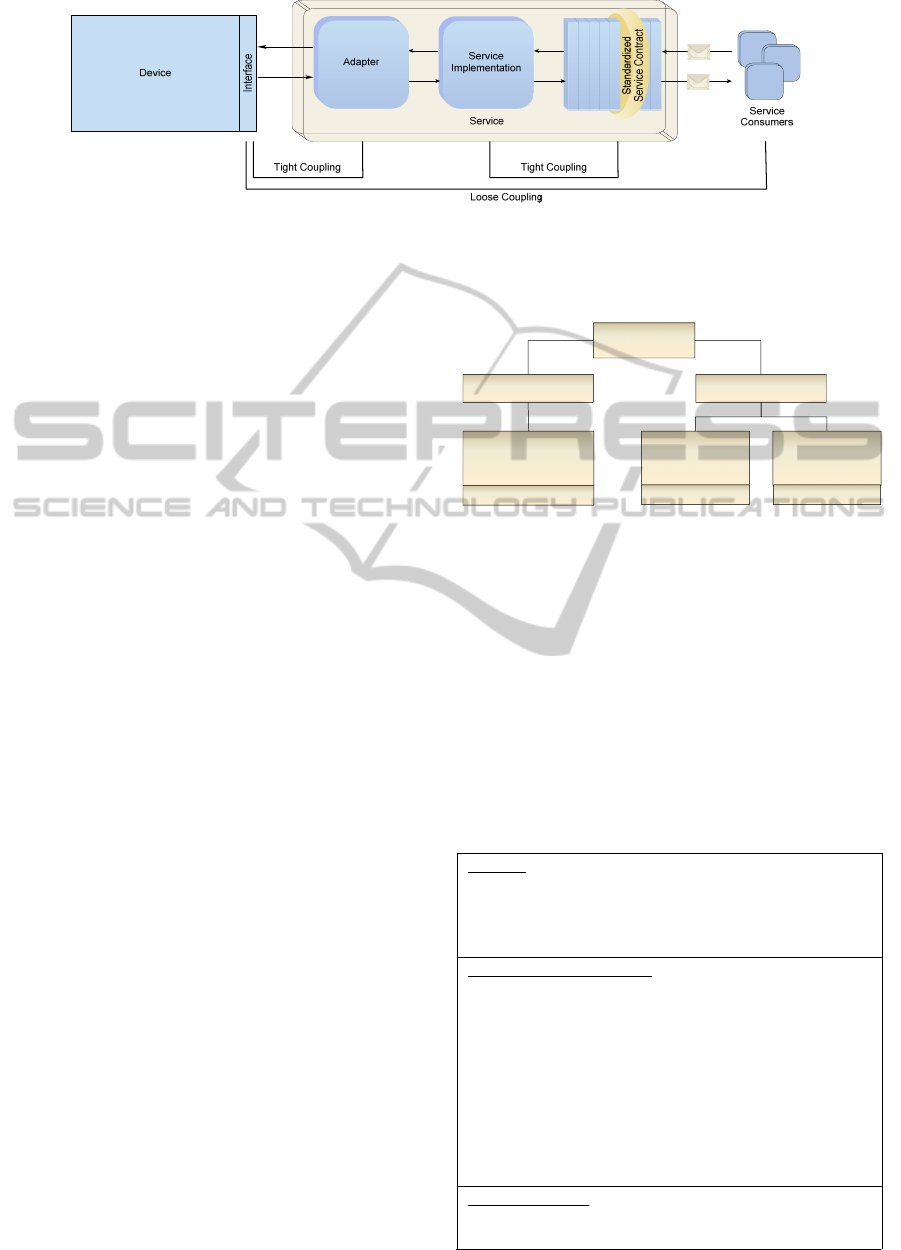
Figure 1: Service oriented integration of devices (according to Mauro et al. (2010)).
To overcome the integration issues of legacy
systems a lot of publications and products are
successfully using service oriented concepts (e.g.,
Siebenhaar, Lehrig, Braun, and Görge (2008)). In
recent research, these concepts are adapted to
devices (SODA, Service Oriented Device
Architecture, cf. de Deugd et al. (2006)). Figure 1
shows a conceptual perspective view of the service
oriented integration of devices. Following the
contract-first principle (Erl, 2009), the starting point
is the definition of the service contract followed by
its implementation. An adapter component is
necessary to handle the connection to the proprietary
device interface. The strength of the concept is the
loose coupling of service consumers to medical
devices (Mauro, C., Leimeister, J. M., & Krcmar,
H., 2010). In this paper we use the term “medical
device services” for services that encapsulate
medical devices.
From a static point of view, the concept of the
service oriented integration of legacy systems can
directly be applied to medical devices. However,
from a dynamic point of view we expect additional
integration issues due to the characteristics of
medical devices (e.g., mobility) and therefore of
medical device services. With the following
multiple-case study we try to identify the
characteristics (the “nature”) of medical device
services.
3 CASE STUDY DESIGN
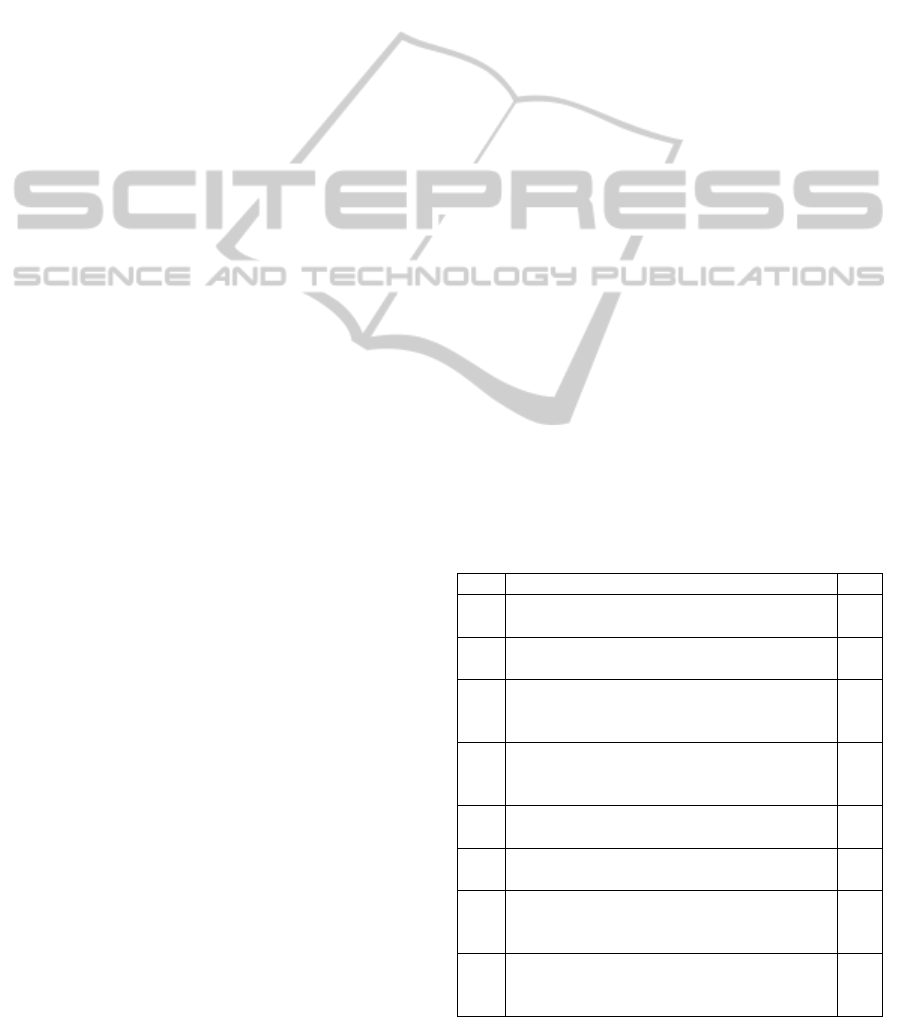
The multiple-case study is composed of three single
cases conducted at two university hospitals (Figure
2). The cases were selected because of their different
disciplines and our access to the field.
We use case studies for the exploration of the nature
of medical device services due to the fact that
different aspects (e.g., processes or the type of data
provided by the devices) have to be considered. The
handling of different kind of sources (observations,
documents, interviews, etc.), as necessary for such
an exploration, is a considerable strength of case
studies (Yin, 2009, p. 11).
Figure 2: Multiple-case study with three cases.
Following Yin (2009, p. 27), the design of a case
study consists of several elements. Table 1 shows
these elements and how they are implemented in our
case study. The strategy used for interpreting the
data is implicit contained in the explanations of
section 4.
Following the process proposed by Yin (2009, p.
57) we write an individual report for each case and
present our cross-case conclusions in another
section.
Table 1: Case study design.
Purpose
Exploring the reasons for the complexity of the
integration of medical devices in order to draw
conclusions regarding the nature of medical device
services
Research Questions (RQ)
RQ1: How many systems might use the data provided
by medical devices?
RQ2: Which processes complicate the integration of
medical devices?
RQ3: Which legal restrictions complicate the
integration of medical devices?
RQ4: What kind of capabilities and data is provided by
the interfaces of medical devices?
RQ5: How are the grade of standardization and the
complexity of the interfaces of medical devices?
Units of analysis
All electronic medical devices of the respective
institution
Multiple-Case
Study
Intensive Care Unit 2
of the Neuro Head
Center
University Hospital I University Hospital II
Ophthalmic
Clinic
Case Study 1
Case Study 2
Neurological
Clinic
Case Study 3
THE NATURE OF MEDICAL DEVICE SERVICES - A Multiple-case Study
251

Table 1: Case study design. (cont.)
Collected data and their link to the research questions
RQ1,
RQ2
Processes using medical devices or data
provided by medical devices
(Source: Observation, interviews)
RQ3 Regulatory
Framework
(Source: literature)
Intended use of the
device interfaces
(Source: specificati-
ons and manuals)
RQ4 Kind of hardware
interfaces
(Source: on-site
analysis and
specifications
Complexity of
software interfaces
(Source: Protocol
specifications)
Kind of data
provided by
software interfaces
(Source: Protocol
specifications)
Capabilities of
software interfaces
(Source: Protocol
specifications)
Grade of standardization of the software
interfaces
(Source: Protocol specifications)
4 CASE STUDY RESULTS
4.1 Case Study 1 – Intensive Care Unit
4.1.1 Medical Devices and their Interfaces
At the Intensive Care Unit 2 (ICU2) the number of
different devices is small. Basically, an intensive
care bed is equipped with four types of devices:
Infusion pumps (B. Braun Infusomat® Space),
Syringe pumps (B. Braun Perfusor® Space),
Respirator (Dräger Evita XL or Evita 4), and Patient
monitor (GE Datex-Ohmeda).
B. Braun infusion and syringe pumps are inserted
into a rack, the B. Braun SpaceStation. An optional
module – the B. Braun SpaceCom – acts as a single
access point for all pumps of a bed. This module has
a number of standard hardware interfaces: Wireless
LAN, Ethernet RJ45, PS/2 for barcode scanner, RS-
232 serial, and USB master/slave. Over these
hardware interfaces three software interfaces are
provided: a) A web server to configure the system
and to access infusion data over a web browser, b)
the medium complex proprietary BCC protocol,
which can be used to access infusion data, and c) the
simple XML based proprietary proposal data
protocol, which can be used to send up to 24
medications to the pumps.
The Dräger Evita XL and Evita 4 respirators
provide a serial RS-232 hardware interface for data
export. The software interface is the proprietary and
very complex Dräger MEDIBUS protocol. It
supports a real time mode, which can be activated by
using specific commands in order to support a
continuous fast data flow.
Unfortunately, we didn’t get access to the GE
Datex-Ohmeda interface specification so far. Instead
of that we analyzed the specification of a
comparable patient monitor, the Dräger Infinity®
Delta. This monitor provides two protocols: a) The
medium complex proprietary RS-232 Export
Protocol (via serial interface), which can be used to
export several vital signs and alarms, and b) the
medium complex proprietary Infinity® protocol (via
LAN or wireless LAN), which provides monitoring
data over network.
4.1.2 Legal Restrictions
In Europe the Medical Device Directive is the most
important legal basis. From an integration point of
view, the two most important aspects are the
upcoming norm IEC 80001, which defines
regulations for the interconnection of medical
devices, as well as the intended use of the device
interface specified by the manufacturer (Mauro, C.,
Sunyaev, A., Dünnebeil, S., Leimeister, J. M., &
Krcmar, H., 2009). If the interface of a device is
used in a way that is not intended by the
manufacturer, the user (i.e., the hospital) is
responsible for all resultant damages to the patient or
other persons.
The intended use of all analyzed devices does not
include the use of the provided data for diagnostic or
therapeutic decisions. In addition, the SpaceCom
specification prohibits a monitoring of alarms only
on the basis of the data provided by the interface.
These restrictions must be taken into consideration
when connecting the devices to other systems.
4.1.3 Process Analysis
By observing the processes at the ICU2 we
identified a number of (future) systems that could
use the data provided by the medical devices:
documentation systems (vital signs, care
documentation, medication documentation, etc.),
therapy planning systems, clinical trial systems,
score calculation system (for the purpose of
accounting a score value is calculated for each
patient), IT supported ward rounds, and the medical
technology database. We also identified a number of
aspects that further complicate the integration of
medical devices:
Linking medical data to patients: Data provided
by medical devices must be correctly linked to a
BIODEVICES 2011 - International Conference on Biomedical Electronics and Devices
252

patient. Linking data to the wrong patient could
result in misinterpretations.
Mobility of medical devices: Some devices are
mobile in order to provide continuous care to the
patient. As a consequence, devices may not be
connected to the network at all times.
Replacement of medical devices: If a device is
defective (or needs to be maintained) it may
dynamically be replaced by another one (other
model, other manufacturer, etc.).
Operation mode of medical devices: Devices can
be switched on/off at any time, e.g., if a
medication is stopped, the corresponding
infusion pump may be switched off.
4.1.4 Conclusion
We conclude each case study with a reflection of the
case study’s research questions:
RQ1: Several systems (we identified six useful
integration scenarios) may be interested in the data
provided by medical devices (cf. section 4.1.3).
RQ2: The linking of medical data to patients as well
as the mobility and replacement of devices are
critical aspects. Another challenge is the fact that
medical devices may be switched on/off at any time
(cf. section 4.1.3). RQ3: The upcoming norm IEC
80001 must be taken into consideration. In addition,
the data provided by the analyzed medical devices
must not be used for diagnostic or therapeutic
decisions. In addition, the monitoring of alarms only
on the basis of the data provided by the device
interfaces is not allowed (cf. section 4.1.2). RQ4:
The devices provide current vital signs and
information about the current therapy by request or
as continuous data flow. In addition, medications
can be sent to the B. Braun pumps (cf. section 4.1.1).
RQ5: The devices provide standardized hardware
interfaces. However, all software interfaces are
proprietary. The complexity of the protocols ranges
from simple to very complex (cf. section 4.1.1).
4.2 Case Study 2 – Ophthalmic Clinic
4.2.1 Medical Devices and their Interfaces
In this clinic we found 42 different (total number:
49) medical devices of 25 manufactures. Due to the
great number of different devices we will not
explain each device type in detail but summarize the
most important results. Our analysis showed that the
devices are of two kinds: a) Devices with no IT
interface or with printer only (13), and b) devices
that need special software (running on a internal or
external computer) with a graphical user interface in
order to analyze raw data and generate findings (29).
From an integration point of view, devices of the
first category are quite unfavorable. There might be
the possibility for some devices to redirect the
printout into a file. However, e.g., for integrated
thermal printer this is not possible at all. Devices of
the second category cannot be directly integrated
with other systems. Instead of that the corresponding
software has to be integrated. Our analysis showed
that about 50% of these software systems are
supporting standards like DICOM (Digital Imaging
and Communications in Medicine), GDT
(Gerätedatentransfer, a common German standard)
or HL7 (Health Level 7). The other half is providing
proprietary interfaces and data formats.
Due to the specific discipline of the clinic the
majority of the medical devices are producing image
data. Therefore, the size of a dataset of one medical
examination can be up to 200 megabyte.
4.2.2 Legal Restrictions
We couldn’t found any specific legal restrictions in
the documents of the software systems. However,
being software for the purpose of diagnostic the
software itself might be (in future versions of the
software: must be) a class IIa medical device due to
the legal regulations (Mauro et al., 2009). Thus, the
IEC 80001 must be taken into consideration when
integrating such software systems (cf. section 4.1.2).
4.2.3 Process Analysis
The number of systems that may be interested in the
data produced by the medical devices is very
limited. In general, the generated findings are
printed out and put into a paper-based medical
record. Thus, after integrating the devices, the
findings could directly be imported to an electronic
medical record. Another system to be integrated may
be the medical technology database (cf. section
4.1.3). Again, we identified a number of aspects that
may complicate the integration of the devices:
Linking medical data to patients: The linking of
the data is not as difficult as in case study 1.
Administrative patient data (as name, gender,
birthday, etc.) can be entered into the software.
However, this manual step is error-prone, patient
data may be entered incorrect.
Operation mode of medical devices: This aspect
is not as critical as in case study 1 because the
software systems do not expect any requests.
They may receive administrative patient data
from the hospital information system, but such
THE NATURE OF MEDICAL DEVICE SERVICES - A Multiple-case Study
253
transfers are initiated by the user itself.
The mobility of medical devices is not relevant
in case study 2. Only three of the analyzed devices
are used mobile. None of these devices has an IT
interface, findings can only be printed. Also the
replacement of a device could not be observed in
this case study.
4.2.4 Conclusion
RQ1: Only a small number of systems (we identified
two useful integration scenarios) may be interested
in the data provided by medical devices (cf. section
4.2.3). RQ2: The administrative patient data should
be imported from hospital information system to
avoid manual mistakes. The fact that medical
devices may be switched on/off at any time should
be kept in mind (cf. section 4.2.3). RQ3: Medical
software may be a medical device in the sense of the
Medical Device Directive. In this case, the norm
IEC 80001 has to be taken into consideration (cf.
4.2.2). RQ4: 31% of the analyzed device types do
not provide an IT interface. The remaining 69%
need special software in order to provide findings of
an examination. This includes a textual report as
well as different kind of data, e.g., numeric values or
images up to 200 MB (cf. 4.2.1). RQ5: The software
interfaces are about 50% standardized and 50%
proprietary. The complexity of the protocols ranges
from simple to very complex (cf. 4.2.1).
4.3 Case Study 3 – Neurological Clinic
4.3.1 Medical Devices and their Interfaces
In this clinic we found 26 different (total number:
38) medical devices of 17 manufactures. The results
are very similar to case study 2. To avoid redundant
explanations we will refer to case study 2 at some
places.
Our analysis showed that all devices (except one
device that only has printing capabilities) need
special software (running on an internal or external
computer) with a graphical user interface in order to
analyze raw data and generate findings. Thus, as in
case study 2, the devices cannot be directly
integrated with other systems. Instead of that the
corresponding software has to be integrated.
Again, about 50% of these software systems are
supporting established standards. We also identified
again a number of systems that produce a great
amount of data (up to 400 megabyte when saving
electrocardiogram video sequences).
4.3.2 Legal Restrictions
Regarding legal restrictions our findings of case
study 3 match with the findings of case study 2.
4.3.3 Process Analysis
Regarding the process analysis our findings of case
study 3 match with the findings of case study 2. The
only difference is that the mobility of the medical
device is an important aspect. 15 of the analyzed
medical devices are used mobile and therefore may
be offline or appear in different network segments.
4.3.4 Conclusion
The results of case study 3 are very similar to the
results of case study 2. Thus, we only list the
differences: a) In addition to images also video data
up to 400 MB are provided, b) only one of the
analyzed device types does not provide an IT
interface. All remaining devices need special
software in order to provide findings of an
examination, and c) 58% of the analyzed devices are
used mobile.
4.3 Cross-Case Conclusions
In this section we provide cross-case conclusions in
the form of a consolidated list of reasons for the
complexity of the integration of medical devices.
We compare these reasons with the integration
issues of legacy systems (Table 2).
Table 2: Integration obstacles of medical devices.
Nr. Reason Description LS
1
Several systems may have to be integrated
with the medical device.
X
2
Data provided by medical devices must be
correctly linked to a patient.
3
Medical devices may be mobile and
therefore are not connected to the network
at all times.
4
Medical devices (and with it the device’s
hardware and software interfaces) may
dynamically be replaced by another one.
5
Medical devices can be switched on/off at
any time.
6
Due to legal restrictions the interface of a
medical device cannot be changed.
X
7
A risk management (IEC 80001) must be
conducted when connecting medical
devices with other systems.
8
The interface of a medical device is only
allowed to be used as intended by the
manufacturer.
BIODEVICES 2011 - International Conference on Biomedical Electronics and Devices
254
Table 2: Integration obstacles of medical devices.(Cont.)
9
Medical devices may provide streaming
data.
10
Medical devices may provide huge image
or video files.
X
11
Medical devices often provide proprietary
and complex interfaces.
X
12
Medical devices do not provide modern
communication frameworks.
X
Nr.= Reason Number, LS = Legacy System,
X = Analogous also valid for legacy systems
5 DEDUCING THE NATURE OF
MEDICAL DEVICE SERVICES
Based on the identified reasons presented in the
previous section we deduced the characteristics of
medical device services. The following list presents
the characteristics as well as the references to the
reasons they were deduced from. Medical device
services
correctly link their medical data to patients
(Reason 2),
dynamically appear and disappear at the network
(Reasons 3, 4, and 5),
automatically publish themselves (as a
consequence of Reasons 3, 4 and 5),
dynamically communicate with different
hardware interfaces and complex low-level
device interfaces (Reasons 4, 6, 11, and 12),
have passed a IEC 80001 risk management
process (Reason 7),
respect the intended use of the device interfaces
(Reason 8),
may provide streaming data (Reason 9), and
may provide huge amount of data (Reason 10).
Reason 1 doesn’t result in an item of this list.
Services are intended to be used by several other
systems so this aspect is not a characteristic of
medical device services.
6 CONCLUSIONS AND FUTURE
RESEARCH
In this paper we presented the nature of medical
device services in the form of a list of eight
characteristics. The results were deduced by
conducting a multiple-case study comprised of three
cases at two university hospitals. This list of
characteristics can be considered as a list of
requirements to a service oriented integration
framework for medical devices. Such a concept must
support / realize all items of the list. Thus, our next
step will be designing a service oriented integration
framework for medical devices based on existing
SOA design patterns / SOA best practices. Finally,
we will implement and evaluate the created
framework.
REFERENCES
Bennett, K. (1995). Legacy Systems: Coping with
Success. IEEE Software, 12(1), 19-23.
Bisbal, J., Lawless, D., Bing, W., & Grimson, J. (1999).
Legacy information systems: issues and directions.
IEEE Software, 16(5), 103-111.
de Deugd, S., Carroll, R., Kelly, K. E., Millett, B., &
Ricker, J. (2006). SODA: Service Oriented Device
Architecture. Pervasive Computing, IEEE, 5(3), 94-96.
Erl, T. (2009). SOA Design Patterns. Boston: Prentice
Hall International.
Hevner, A. R., March, S. T., Park, J., & Ram, S. (2004).
Design Science in Information Systems Research. MIS
Quarterly, 28(1), 75-105.
Lesh, K., Weininger, S., Goldman, J. M., Wilson, B., &
Himes, G. (2007). Medical Device Interoperability –
Assessing the Environment. Paper presented at the
Joint Workshop on High Confidence Medical Devices,
Software, and Systems and Medical Device Plug-and-
Play Interoperability.
Mauro, C., Leimeister, J. M., & Krcmar, H. (2010).
Serviceorientierte Integration medizinischer Geräte –
ganzheitliche IT-Unterstützung klinischer Prozesse.
Informatik-Spektrum, Online First.
Mauro, C., Sunyaev, A., Leimeister, J. M., & Krcmar, H.
(2009). Service-orientierte Integration medizinischer
Geräte - eine State of the Art Analyse. Paper presented
at the Wirtschaftsinformatik 2009 - Business Services:
Konzepte, Technologien und Anwendungen.
Mauro, C., Sunyaev, A., Dünnebeil, S., Leimeister, J. M.,
& Krcmar, H. (2009). Mobile Anwendungen im
Kontext des Medizinproduktegesetzes. Paper
presented at the Informatik 2009 - Im Focus das
Leben.
Schweiger, A., Sunyaev, A., Leimeister, J. M., & Krcmar,
H. (2007). Toward Seamless Healthcare with Software
Agents. Communications of the Association for
Information Systems (CAIS), 19, 692-709.
Siebenhaar, M., Lehrig, T., Braun, J., & Görge, T. (2008).
Entwicklung einer SOA-basierten Webanwendung zur
Buchung und Verwaltung von Segeltouren:
Proprietäre Software vs. Open Source
Wirtschaftsinformatik, 50(4), 325-329.
Yin, R. K. (2009). Case study research: design and
methods (4 ed.). California: SAGE Publications.
THE NATURE OF MEDICAL DEVICE SERVICES - A Multiple-case Study
255
