
ON THE USE OF openEHR IN A PORTABLE PHR
Cândido Santos
1,2
, Tiago Pedrosa
1,3
, Carlos Costa
1
and José Luís Oliveira
1
1
DETI/IEETA, Universidade de Aveiro, Aveiro, Portugal
2
DEE, Instituto Superior de Engenharia de Coimbra (ISEC), Coimbra, Portugal
3
IPB, Instituto Politécnico de Bragança, Bragança, Portugal
Keywords: Personal health record, Electronic health record, openEHR, Privacy, Security.
Abstract: Quality medical acts rely on patient medical information. With paper records, the responsibility of gathering
the disparate information and making it available to the caregivers, falls exclusively upon the patient. This
still is, to great extent, the case with electronic health documents. The consensus is that the advantages of
patient involvement in his own health are numerous. With the advent of recent technologies and their
deployment in healthcare, new ways of involving the patient and making him an active part of his own
health are possible. Electronic Health Records (EHR) and specially Personal Health Records (PHR) are
important tools for patient empowerment but data population and management through non-intuitive
structured forms is time consuming, takes a great amount of effort, and can be deterring specially for people
that are not very computer-oriented. PHRs can be simple and scalable applications that the patient uses to
get started and afterwards evolve towards complexity. In any case, compliance with standards must be
accomplished. In this paper we present a PHR simple to use, implemented on a USB Flash pen for mobility,
and compliant with the openEHR specification. Our model builds on openEHR and adds security and
privacy features, allows patient data management and can work as an information repository.
1 INTRODUCTION
Healthcare is currently undergoing profound
changes. New diagnose and treatment techniques
make possible to address more conditions thus
increasing personal life quality but also the number
and severity of illnesses per patient. People pay an
increasing attention to their own health, demanding
for quality healthcare. Population ageing leads to an
increase in the number and seriousness of medical
conditions per patient, and to continuous and
integrated healthcare.
All the aforementioned factors result in an
increase in the number of medical acts, their
improved quality, the rise in health costs, and the
exponential escalation of the amount of existing
information per patient. Of special interest to us is
the latter.
Personal Health Information (PHI) is typically
generated in many different places making its
collection and management difficult for the patient.
With great amounts of PHI to process, existence
doesn’t necessarily mean availability and availability
doesn’t necessarily mean usability. Information can
exist and not be available to the professional
caregiver, or it can be available but take too much
time to browse through.
It is common sense that involving patients in
their own healthcare is positive. The more involved
and informed a patient is, the more useful
information he will supply and more informed
medical decisions will be made by healthcare
professionals.
Information technologies bring new possibilities
to PHI management through the use of computerized
medical records that can assume many forms. The
deployment of Electronic Health Records (EHR) in
general replaces with advantages the paper-based
records. Personal Health Records (PHR) are an
important factor contributing for patient
empowerment.
Patient management of PHI through the use of a
PHR can be daunting, specially for people not very
familiar with computers. Meticulous, regular and
timely data input by the patient is undoubtedly
clinically relevant and helpful. But most
implementations force the use of complex and user-
unfriendly screen forms. Thus, instead of acting as
351
Santos C., Pedrosa T., Costa C. and Luís Oliveira J..
ON THE USE OF openEHR IN A PORTABLE PHR .
DOI: 10.5220/0003173203510356
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 351-356
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

positive factors in involving the patient in his own
health, these implementations can easily deter an
individual away from technology, accomplishing
exactly the opposite objective they were designed
for.
We share the vision that PHRs are an important
factor in positive patient involvement in his own
health, and ultimately in total patient empowerment.
But we take a simplistic approach and propose that
complicated computerized PHI management
schemes can be more prejudicial than beneficial.
Instead, a minimal PHR, conformant with current
standards, and easy to use can serve as an entry point
specially for users that are not too computer-skilled.
If, later on, those users decide they want extra
features in their PHR, more complex
implementations are available.
In this paper we review the current situation
concerning patient’s medical records and advocate
steps towards patient empowerment through PHRs.
Considering that a) A great percentage of data
that is accessible to patients consists of
Complementary Diagnose Tests (CDT), mostly in
paper format; b) When converted into electronic
format, this data will also be responsible for the
greatest demands in terms of storage and
management needs; c) The open source standard
specification openEHR allows integration with
legacy systems (assumed to be professionally
managed); a simple system for the patient to perform
that integration and PHI management at a personal
level is worthy of attention.
Most PHR proposals state that it must be patient-
centric, but that usually just means that the health
information revolves around the patient. We propose
a PHR that is patient-centric in information terms,
and that is also user-centric in terms of easiness.
2 BACKGROUND
One way of making the patient a more active
participant in the healthcare services he seeks
throughout his lifetime is by allowing him to
responsibly manage his own PHI. Population ageing
is changing some paradigms in healthcare, making it
more patient-centric and increasingly relying on the
patients’ responsible actions in the management of
their own conditions like diabetes, for example.
With the objective of giving the patient some
form of access to his health information, some PHI
management schemes have been proposed, namely
through the use of EHRs and PHRs operated on
servers, personal computers and mass storage
devices and accessed locally or remotely via smart
cards, as proposed by Costa (2003) and Costa (2004)
and other portable devices like USB pens.
2.1 Patient Empowerment
Anderson and Funnel (2009) argue that patient
empowerment in healthcare can be conceived as the
capacity of patients to think critically and make
autonomous decisions. In order to achieve this, the
patient must have access to a comprehensive set of
his own PHI and be capable of managing that data in
the way he sees fit. To achieve this goal, the control
of the medical information has to fall under the full
responsibility of the patient, i.e. the patient must
have physical possession of all the data pertaining to
his health.
When considering PHI management through the
use of information technologies, different levels of
computer knowledge have to be considered since
some people are not technology-oriented. A scalable
solution adaptable to different user technology
awareness is a major advantage.
2.2 EHRs and PHRs
PHI management is achieved through EHRs and
PHRs but various problems presently afflict this
technological field, in particular the lack of data
representation and data transfer standards widely
accepted, the non-agreement on the basic data fields
that make up an EHR/PHR, the varying definitions
of EHRs and PHRs, and legal issues concerning data
ownership.
There are no generally accepted definitions for
EHRs and PHRs but most of the literature seems to
agree at least on one basic difference between them:
an EHR contains PHI and is usually stored and
managed by a healthcare institution for the use of
healthcare professionals, while a PHR consists of a
set of PHI (that might be the same or different from
the data set contained in the EHR) that is usually
stored under the patient’s ownership and
management, and for his own use.
Of special concern to us is the concept of PHR.
According to Tang et al (2006) a PHR is more than a
simple means to gather all the scattered information,
it encompasses a set of data, knowledge and
applications that allow the patient to become
actively involved in his health by providing a set of
functionalities. Kaelber et al (2008) have presented a
general description of most of the work that remains
to be done in the field of PHRs.
HEALTHINF 2011 - International Conference on Health Informatics
352

One of the problems that face developers is the
right choice of model to work with. Given the
present interest surrounding this theme, it’s only
natural that various classifications arise. For
example, Kaelber and Pan (2008) classified PHRs
according to their degree of interconnectivity as a)
Stand-alone; b) Tethered. The later being subdivided
in provider-tethered, payer-tethered, third-party-
tethered and interoperable.
The stand-alone model has the advantage of
being non-biased in terms of the focus it presents
towards parts of the data contained in the PHR but
the disadvantage of having to be bought, while the
tethered models tend to be offered as fidelity factor
or, at least, to be less expensive. Another important
factor to have in mind is the record data population
method.
The tethered models present the advantage of
being frequently given by institutions free of charge
and being already populated with some information.
But also have the disadvantage of each particular
type of PHR being too focused on the type of
information more relevant to that institution.
Tang et al (2006) consider that the most
promising architecture for a PHR is the one that
integrates with an existing EHR. According to the
classification presented this corresponds to the
tethered-interoperable model.
From the perspective of patient empowerment
data ownership and management assume a crucial
importance. Maloney and Wright (2010) classify
PHRs in four categories: a) self-contained EHR,
maintained and controlled by the patient; b) self-
contained EHR, maintained by a third-party such as
a web service provider; c) component of an
integrated care EHR maintained by a health provider
(e.g. a general practitioner) and controlled at least
partially by the patient; d) component of an
integrated care EHR but maintained and controlled
by the patient.
2.3 PHRs in Portable Devices
Smart Cards (SC) are very secure authentication
tokens and some of them have very useful
cryptographic capabilities, thus providing very
interesting characteristics when deployed in
healthcare in general namely as remote PHI access
tokens. Some of the proposed models of PHR in
smart cards are remote information aggregation
tokens that allow the patient to visualize some of his
PHI contained elsewhere and to manage some of
that information in a necessarily limited manner.
Some countries are shifting from traditional
paper-based national identification cards and
passports towards smart cards. This evolution
towards a technological overlap between
identification, health information access, and
management makes possible to envision many forms
of integration.
The storage capacity of smart cards is on the
constant rise but more so is the amount of medical
information generated per patient that can nowadays
take some gigabytes of storage space, and this is an
important limitation at the moment. For all their
security features, SC’s are undoubtedly a type of
device to keep under close observation in search of
future developments.
Among the logical candidates for storage devices
capable of holding a PHR under the patient’s
responsibility are external hard drives, CDs, DVDs,
and USB flash pens. According to Srinivasan and
Datta (2007), because of issues like physical
resistance to damage, better performance under
electromagnetic fields, the fact that they have no
moving parts, don’t need any additional hardware,
are not susceptible to dust, and that can come in a
variety of shapes and forms, the USB pens are the
most advantageous of them.
On top of all those advantages, there are now a
number of portable applications described by
PortableApps (2010) and Pendriveapps (2010) that
don’t need installation and can be executed from the
pen, an additional security factor.
2.4 Standards
In this field of work the lack of widely accepted
standards is a reality, there is no shortage of
proposed standards, the shortage is at the acceptance
level. At the core of data representation, structure
and storage there are three well positioned
candidates: openEHR as described by openEHR
(2007); HL7-CDA (Health Level 7 – Clinical
Document Architecture), described by Dolin et al
(2006); and CCR (Continuity of Care Record)
described by Ferranti et al (2006). At the
communication level, HL7 seems to hold the
advantage at the moment. We will not get into an in-
depth analysis of these standards and will focus our
attention on the openEHR specification mainly
because it is open source and attempts to comply
both with HL7 and HL7-CDA.
OpenEHR is a set of specifications for an EHR
focusing mainly on structure and content. An EHR
compliant with openEHR consists of a logically
organized structure of folders, each containing
ON THE USE OF openEHR IN A PORTABLE PHR
353

versioned healthcare events. Versioning is
accomplished through recording every data change
in special data structures (Contributions).
All the interaction with data is achieved through
the use of Archetypes and Templates. An archetype
is a component that allows standardization by
mapping each medical event into pre-agreed
individual fields of information (Entries) forming a
Composition. A Template serves both as a
messaging standardization structure and is closely
related to screen forms. It aggregates one or usually
more archetypes.
An archetype can be used to manage data
referring, for example, to a blood pressure
monitoring event, that are mapped into various
information fields (date, systolic, diastolic,
respective values, etc), forming a Composition, e.g.
“blood pressure measurement”. A Template can be
an aggregate of information, e.g. “discharge
summary” that manages the information relative to
various healthcare events, each one of them created
through a particular archetype.
Archetypes are meant to be created by other
parties, namely in close collaboration with medical
experts, and Templates are mostly to be developed
by local implementations. Archetypes are also the
structures that allow the use of terminologies.
OpenEHR’s main focus is on components
instead of documents and its main specification is
the openEHR EHR Reference Model, namely its
EHR Information Model described by Beale et al
(2008). An openEHR system is composed of an
EHR Repository, an Archetype Repository,
Terminology, and Demographic or identity
information. A high-level openEHR EHR structure
consists of Contributions, EHR_id, EHR_Access,
EHR_Status, Directory, and Compositions.
3 A PORTABLE PHR openEHR-
Compliant
The basic paradigm of the Portable PHR (p.PHR) is
simplicity in order to attract users to the world of
PHRs. The best way to start is by allowing
individuals to scan their current paper records,
mostly CDTs and to provide a simple means to
store, organize and manage that information that will
be kept in a USB flash pen for total portability. The
proposed model also accommodates a workflow
similar to the paper-based but in which CDTs are
handed to the patient in electronic format both by e-
mail and in physical presence.
In another work (Santos et al, 2010), we
proposed a p.PHR, implemented on a USB flash
pen, based on secure virtual containers with
characteristics briefly summarized below. In this
paper we present the necessary steps to make it
compatible with the openEHR specifications.
One of the key concepts of the previously
proposed PHR model is the existence of five
different conceptual data types implemented through
individual document classification or by placing the
documents in different data storage areas or virtual
containers: a) Confidential Data (extremely
sensitive); b) Normal Data (disclosed to health
professionals); c)Transfer Data (recently entered the
PHR); d) Prescription Data; e) Emergency Data.
This model allows patient mobility, provides an
emergency data repository, and can be used, by a
patient with just basic computer skills, as a passive
information repository to be carried between
healthcare facilities, thus mimicking the existing
social habit with paper-based records.
In order to achieve this, the p.PHR’s structure
needs to be secure and to allow for different data
storage areas depending on the degree of
confidentiality the patient deems the particular data
items that make up his PHR. The information
contained in the p.PHR is controlled, managed, and
made available to third parties by the patient and
only under his explicit consent.
In order to allow the patient to both manage the
PHI contained in the p.PHR and to make it available
to other actors in a scalable manner, various
operating modes are available upon patient’s option.
These operating modes are shown in figure 1.
Upon receiving the p.PHR in the respective
device, the patient authenticates himself for account
provisioning. The device is supplied with a master-
password that will be used for the initial setup of
p.PHR native applications and for the creation of a
working-password (password). When the patient
accesses the p.PHR an operating mode is selected.
Each actor in healthcare delivery has different
information access needs, therefore with different
access privileges to each data type. Figure 1 shows
these data types in usage context.
Although an EHR is conceptually different from
a PHR, the openEHR specification can be deployed
for data structure. In terms of data, the EHR
openEHR-compliant’s structure can be deployed
with the added feature of the secure virtual
containers (containing the classified compositions)
reflected at the openEHR directory level.
In terms of the overall system the EHR
repository
will be reduced to just one PHR and the
HEALTHINF 2011 - International Conference on Health Informatics
354
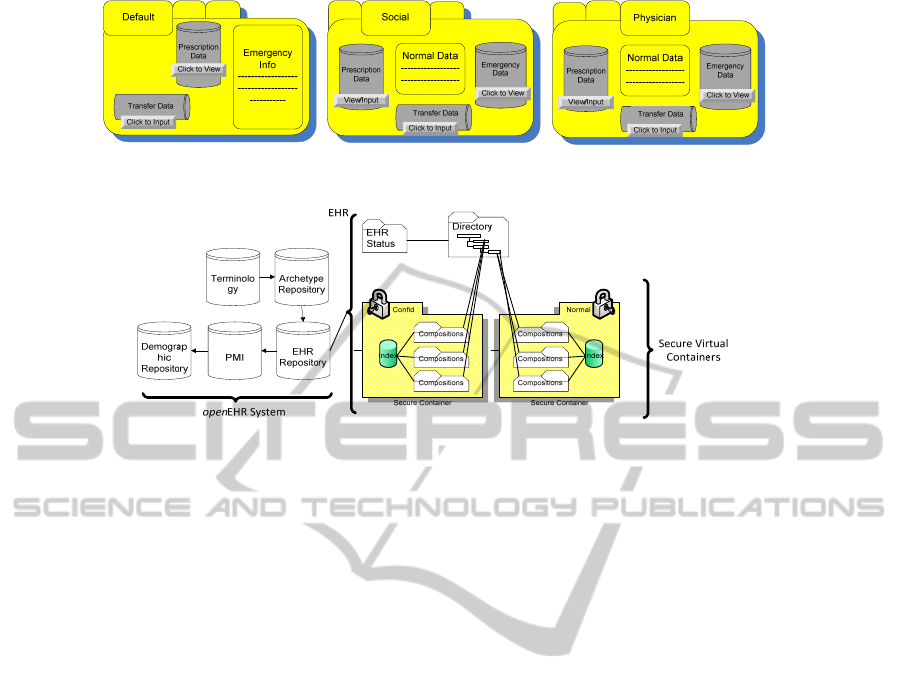
Figure 1. p.PHR data and user-access.
Figure 2. Containers, EHR, and HER system.
demographic repository will also be reduced to just
the individual’s information. There is no need for a
Patient Master Index (PMI) since there is only one
patient in the PHR system. The same applies to the
EHR_id data structure since there is no need to make
the p.PHR a part of any uniquely identifiable
scheme. The Archetype Repository, residing outside
any secure virtual container, is populated with the
necessary Archetypes on a needed basis. Outside
any container is also the EHR_Status data structure.
This Architecture is depicted in figure 2.
Inside each secure container there are openEHR
compositions, that are data previously instantiated
by the Archetypes, optionally including, or
referencing, CDT multimedia files, and the virtual
container File Indexing Database that references all
documents in the container.
The openEHR specification is directed towards
various users creating data and populating the
record. In our p.PHR implementation, the patient is
the only data creator who shows different views of
his PHI to various users, this fact carries some
implications. There is no need to implement a heavy
access control strategy and we can rely on the
password-protected secure virtual containers for
different user-access. The data structure
EHR_ACCESS provided by openEHR is not used in
our implementation. The versioning supported by
openEHR can be discarded in favor of simplicity
since there aren’t many data alterations that can be
foreseen. There is no internal electronic signature
scheme for information integrity although, in the
case of externally generated electronic data items
should be signed by the respective institutions that
generated them by their own software.
The data management functionality is
implemented as document classification through the
use of Archetypes, e.g the openEHR-EHR-
CLUSTER.exam-generic.v1 that is simultaneously
generic and allows for the storage of a multimedia
file, which is very useful for CDT management.
Medication and allergies lists are entered through
openEHR-EHR-COMPOSITION.medication-list.v1
and openEHR-EHR-EVALUATION.adverse.v1
Archetypes.
The pPHR is completely pen-resident and
consists of a stand-alone application with various
management functionalities allowing access to a
virtual container where the various data items are
stored. The virtual container is implemented in a zip-
like manner (ZipArchive) with compression and file
encryption via a soft-coded encryption key. AES
encryption algorithm and the fact that, upon access
by the application, the files are decompressed to
computer RAM memory only, are important features
contributing for enhanced security. Encryption
capabilities are allowed by openEHR.
The access to any individual file stored inside a
virtual container is subject to authentication and the
decompression of the files is made to computer’s
memory. The fact that decompressed data is not
written to hard disk or even to the USB pen is an
increased security feature.
ON THE USE OF openEHR IN A PORTABLE PHR
355

4 CONCLUSIONS
PHRs are a way of involving patients in their own
healthcare but complex implementations can turn
those users with just the basic computer knowledge
away from technology.
An individual’s PHI is at present generated
dispersedly and is stored in many different locations
under many physical formats. The responsibility of
collecting it and making it available to the healthcare
professionals falls upon the patient.
Our approach to PHRs is a simplistic one
providing an implementation that can be a point of
entry for the patient. Later he will be given the
chance of more functional implementations and
consequently more complex to use.
A portable PHR in a USB pen device can be
envisioned as a complement, rather than a
replacement for existing PHI management systems,
such as EHRs. The p.PHR intends to be the initial
step in letting the patient assume the responsibility
of managing his own PHI, thus contributing for
patient empowerment. The medical data pertaining
to a patient and maintained in the p.PHR is kept
under his direct control, allows patient mobility, and
provides an emergency data repository. The patient
decides which data becomes part of the record and
who, and under what circumstances, has access to it.
Data is kept in conceptually different data
containers and is controlled, managed, and made
available to third parties by the patient and only
under his explicit consent. Any access to the p.PHR
and the data within depends exclusively on patient’s
authorization.
Standard conformity is achieved through the
deployment of the openEHR specifications and their
generic, multi-user, and EHR-oriented, adaptation to
our specific, single-user, PHR needs.
Security features are added through the use of
password-protected virtual containers.
Privacy concerns are addresses by different data
containers and data-classification.
REFERENCES
Anderson, R.M & Funnell, MM 2009, Patient
empowerment: Myths and misconceptions. Patient
Educ Couns.
Beale, T et al 2008, EHR Information Model - Revision
5.1.1. The openEHR Foundation.
Costa, C 2004, Doctoral Thesis: A Security Dynamic
Model for Healthcare Information Systems.
Departamento de Electrónica e Telecomunicações,
Universidade de Aveiro.
Costa, C et al 2003, A New Concept for an Integrated
Healthcare Access Model. The New Navigators: From
Professionals to Patients. Proceedings of MIE2003.
Dolin, RH, et al 2006, HL7 Clinical Document
Architecture, Release 2. J Am Med Inform Assoc,
13(1): p. 30-9.
Ferranti, JM et al 2006, The clinical document
architecture and the continuity of care record: a
critical analysis. J Am Med Inform Assoc, 13(3): p.
245-52.
Kaelber, D et al 2008, A Research Agenda for Personal
Health Records (PHRs). JAMIA.
Kaelber, D & Pan, EC 2008, The value of personal health
record (PHR) systems. AMIA Annu Symp Proc, p.
343-7.
Maloney, FL & Wright, A 2010, USB-based Personal
Health Records: An analysis of features and
functionality. Int J Med Inform.
openEHR 2007, Introducing openEHR - Revision 1.1. The
openEHR Foundation.
Pendriveapps.com 2010, Portable applications that can be
run from a usb device [Online]. (Accessed 2010-02-
10).
PortableApps.com 2010, Portable Aplications - Your
Digital Life Everywhere
TM
[Online]. (Accessed 2010-
02-10).
Santos, J et al, 2010, Modelling a Portable Personal
Health record. Proceedings of the International
Conference on Health Informatics (HealthInf 2010).
Valencia, Spain. p. 494-498.
Srinivasan, U & Datta, G 2007, Personal Health Record
(PHR) in a Talisman: An Approach to Providing
Continuity of Care in Developing Countries Using
Existing Social Habits. 9th International Conference
on e-Health Networking, Applications and Services, p.
277-279.
Tang, PC et al 2006, Personal health records: definitions,
benefits, and strategies for overcoming barriers to
adoption. JAMIA 13(2): p.121-6.
HEALTHINF 2011 - International Conference on Health Informatics
356
