
iTrem
Robert Delano, Brian Parise and Leanne West
Georgia Tech Research Institute, 925 Dalney St., Atlanta, Ga, U.S.A.
Keywords: iPhone, Essential tremor, Parkinson’s, Mobile phone, Human-computer interaction.
Abstract: iTrem is an iPhone application that uses the phone’s built-in accelerometers to collect frequency and
amplitude data of hand tremor in people with Essential Tremor, Parkinson’s Disease, and other neurological
conditions. iTrem makes it possible to take frequent tremor data samples from a subject and communicate it
in real time to a doctor or researcher independent of the subject’s location. Aggregating the tremor data
collected by iTrem provides a way for patients, doctors and researchers to collaborate on a grand scale,
possibly shedding light on new avenues of treatment and therapy.
1 INTRODUCTION
Essential Tremor and Parkinson’s disease are the
most common neurological conditions defined by
tremor and collectively affect 5 to 10 million people
in the U.S. (Boelen, 2009). Parkinson’s kills one
person every 26 minutes in the U.S. alone (Xu,
Kochanek, Murphy, and Tejada-Vera, 2007)! There
is no definitive diagnosis for either condition; both
are a clinical diagnoses based on symptoms and
response to medication (Anwar and Sweeny, 2010).
Very little data about tremor is available to track the
effectiveness of medication and therapy over time.
Essential Tremor affects nearly 1 out of 5 people
over 65 and is usually progressive (Beers and Jones,
2005). Commonly beginning in young adulthood,
Essential Tremor becomes more obvious with age,
usually resulting in some degree of disability.
Originally called “The Shaking Palsy”,
Parkinson’s is a progressive disorder of the central
nervous system caused by a loss of Dopamine in the
brain. The patient experiences four primary
symptoms: tremor, rigidity, slow movements, and
loss of balance. One of the most common
neurological disorders 5 to 10 percent of people with
Parkinson’s present will symptoms before the age of
forty (Grimes, 2004).
Dopamine replacement is the “gold standard” for
treating Parkinson’s disease. Patients experience
what doctors refer to as “on/off” times with the
medication refer to. On is when there is some
symptom relief and off is when the symptoms return.
To sustain a therapeutic effect it is crucial to
anticipate the off times and take medication in
advance to reduce the occurrence of off times. Some
patients take medication every two hours and others
just a few times daily. Being able to track the
severity of symptoms throughout the day will help
patients and doctors define an optimum daily
medication schedule.
Tremor is the most common movement disorder
and is defined as an involuntary, rhythmic,
oscillating movement of nearly constant amplitude
(Anwar and Sweeny, 2010). The amplitude of a
tremor determines the severity of the disability
where the frequency can be characteristic of a
specific disorder (see Table 1).
There are three categories of tremor, resting,
postural, and kinetic or intention tremor. Resting
tremor occurs when the body is at rest and supported
against gravity. Postural tremor occurs when holding
any intentional posture, such as the arms out
stretched. Kinetic or intention tremor may appear
during any voluntary movement. Many patients
experience a combination of all three types of
tremor. (DeMeyer, 2004).
There are three categories of tremor, resting,
postural, and kinetic or intention tremor. Resting
tremor occurs when the body is at rest and supported
against gravity. Postural tremor occurs when holding
any intentional posture, such as the arms out
stretched. Kinetic or intention tremor may appear
during any voluntary movement. Many patients
experience a combination of all three types of tremor
(DeMeyer, 2004).
115
Delano R., Parise B. and West L..
iTrem.
DOI: 10.5220/0003177701150118
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 115-118
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

Table 1: Tremor Frequencies (Rohkamm, 2004).
Frequency Disorder
2.5-5 Hz Cerebellar tremor, Holmes tremor
3-6 Hz Parkinsonian tremor
7-9 Hz Essential tremor, postural tremor in parkinsonism
7-12 Hz Physiological tremor, exaggerated physiological
tremor
12-18 Hz Orthostatic tremor
The severity of tremor is most often determined
by a subjective clinical observation made by a
Movement Disorder Specialist (MDS). The doctor or
patient bases medication and therapy choices on an
observed response to medication.
Reproducible objective tremor data, as is
collected by the iTrem application, will provide
doctors with more information when choosing daily
medication schedules and types of therapy. With a
larger quantity of reliable data, researchers will have
another avenue to spot trends in therapy. Actively
involving the patient may also provide some level of
comfort for the patient, increased communication
with the doctor, and more satisfaction with the care
provided (Sheldon and Kaplan, 1985).
2 TREMOR MEASUREMENT
The cost and challenge of gathering frequent tremor
data discourages the collection and aggregation of
data. In many cases, therapy choices are based solely
on the subjective clinical observation of a doctor.
These observations could work in conjunction with
objective data collection, thereby creating a
multidimensional approach towards the treatment of
tremor (Tarsy, Vitek and Lozano, 2003).
2.1 Clinical Rating Scales
Most tremor rating scales are based on a simplistic
rating score of 0 to 4, with 0 being no detectable
tremor. Although still used, many scales have not
been validated or found to be reliable. The
Washington Heights-Inwood Tremor Rating Scale is
the only validated clinical tremor rating scale (Chen
and Swope, 2010).
The Washington Heights-Inwood Tremor Rating
Scale first has the patient hold his/her arms in front
with wrists pronated and then in a “wing” position.
The patient is also asked to pour water from one cup
into another, use a spoon to drink water, perform
finger to nose movements, and draw Archimedes
spirals. Tremor is rated on a scale 0 to 3, with 0
being normal. Although, this technique has been
validated, a scale of 0 to3 does not allow for subtle
differences in frequency and amplitude. The
Washington Heights-Inwood Tremor Rating Scale is
also not designed for the testing of resting tremor
(Tarsy, Vitek and Lozano, 2003).
2.2 Professional Measurement Systems
The expense and time required for doctors to use
electronic-physiologic methods like the EEG and
EMG usually discourages the use of these devices.
By attaching 16-20 electrodes to a patients scalp, an
Electroencephalography (EEG) can record the
electrical activity along the scalp caused by the
firing of neurons in the brain (Niedermeyer and da
Silva, 1999).
An electromyography EMG uses a very thin
needle electrode that is placed through the skin into
the muscle. The electrode then picks up the electrical
activity produced by the muscles. An EMG may
cause mild discomfort where the electrodes are
inserted and may leave the tested muscle tender
afterwards.
Both EEG and EMG are expensive and time
consuming. An average EMG takes around 15-20
minutes to complete and may cause discomfort. An
EEG can last about 1-½ hours. EEG and EMG
procedures also require the patient to be on location.
iTrem is affordable, mobile and painless.
2.3 Off-the-shelf Measurement Systems
Although off-the-shelf products are available for
tremor measurement, there are no devices that
collect and store tremor data for review and
research. They also require that the patient and
doctor be in the same location.
Two examples of off-the-shelf tremor
measurement devices are the Tremorometor
(www.managingtremor.com) and the Stressometer
(www.tnr.fr). Designed to test for tremor in an office
or clinic, the Tremorometer® provides acceleration
measurements by taping a sensor to the patient’s
index finger for 15-second tests. The Stressometer
has the ability to measure tremor caused by
neurological disorders, but instead focuses on the
microscopic tremors of the nervous system as they
relate to stress.
HEALTHINF 2011 - International Conference on Health Informatics
116
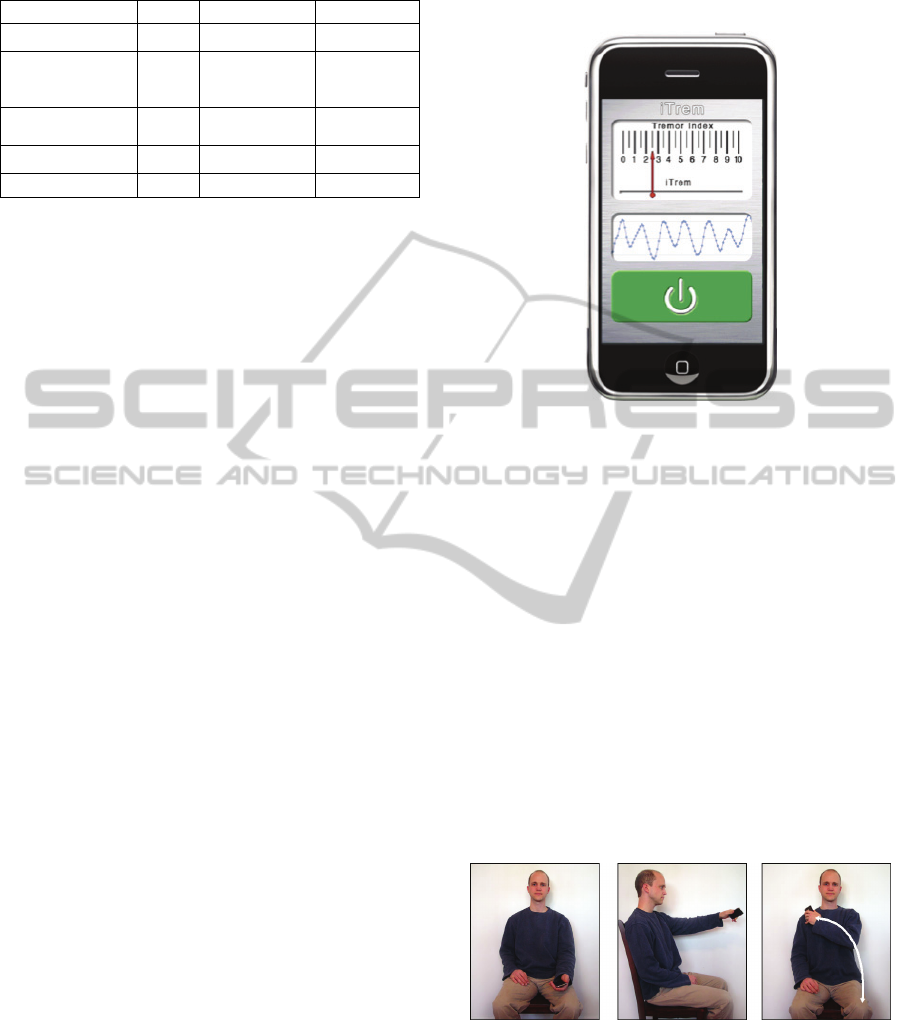
Table 2: Feature comparison.
Feature iTrem
Tremorometer Stressometer
Measure tremor Yes
Yes Yes
Real-time
patient doctor
communication Yes No No
Aggregate patient
data Yes No No
Expandable Yes No No
Hardware Cost >=$199 $595 ~$650
3 iTrem
Both a phone and a breakthrough Internet device, the
iPhone garnered over 25 percent of the mobile
market by the end of 2009 (Tabini, 2010). The
iPhone’s sensitive accelerometers, Internet access,
and popularity made it an ideal hardware choice for
creating an application to track tremor and
communicate that data instantaneously to doctors.
iTrem is a newly developed mobile iPhone
application that provides an affordable and easy
method to collect reproducible, objective tremor data
(See Figure 1). Resting, postural, and intention
tremors can be measured with the iTrem system.
iTrem can connect the doctor, patient, and
researchers in real time without requiring them to be
in the same geographic location. Tremor data can be
transmitted to a web repository for doctor review or
aggregated for research. Through the patient’s web
profiles, doctors can remotely schedule tests, test
reminders, and medication reminders.
To collect data with iTrem, the patient holds the
iPhone and performs simple arm or hand movements
to test resting, postural, and action tremors (See
Figure 2) that are based on the movements that a
patient would perform in the Doctor’s office. To
collect data with iTrem, the patient holds the iPhone
and performs simple arm or hand movements to test
resting, postural, and action tremors (See Figure 2)
that are based on the movements that a patient would
perform in the Doctor’s office. The tests last 10 to
15 seconds each. Holding the iPhone during these
tests, the iTrem application measures tremor data,
including amplitude and frequency, using the
iPhone’s accelerometers.
To collect data with iTrem, the patient holds the
iPhone and performs simple arm or hand movements
to test resting, postural, and action tremors (See
Figure 2) that are based on the movements that a
patient would perform in the Doctor’s office. The
tests last 10 to 15 seconds each. Holding the iPhone
during these tests, the iTrem application measures
tremor data, including amplitude and frequency,
using the iPhone’s accelerometers.
Figure 1: Actual tremor index meter.
Doctors and researchers can program the phone
via the web server. Test schedules and
configurations are stored on the server and
synchronized to the phone periodically. The iPhone
will remind the patient when to take each test with
an alert or reminder. The phone will then briefly
instruct the patient as to what actions to perform for
each test including, resting, postural, and action.
The results of every test are stored in a Web
Repository.
After collection, patient data is uploaded to a
private profile on a secure web server. Doctors can
then review the objective data to assess medication
response, progression, and tremor severity. This
information will also help the patient and doctor
anticipate “off” times and adjust the daily
medication schedule accordingly.
Figure 2: Resting, postural and action tremor tests.
Access to the data is restricted to the patient and
their doctor. Researchers could have access to an
anonymized version of the entire patient databases
(See Figure 3). The tremor data will assist doctors in
diagnosis, as well as helping patients refine their
daily medication schedules to minimize “off” times.
iTrem
117
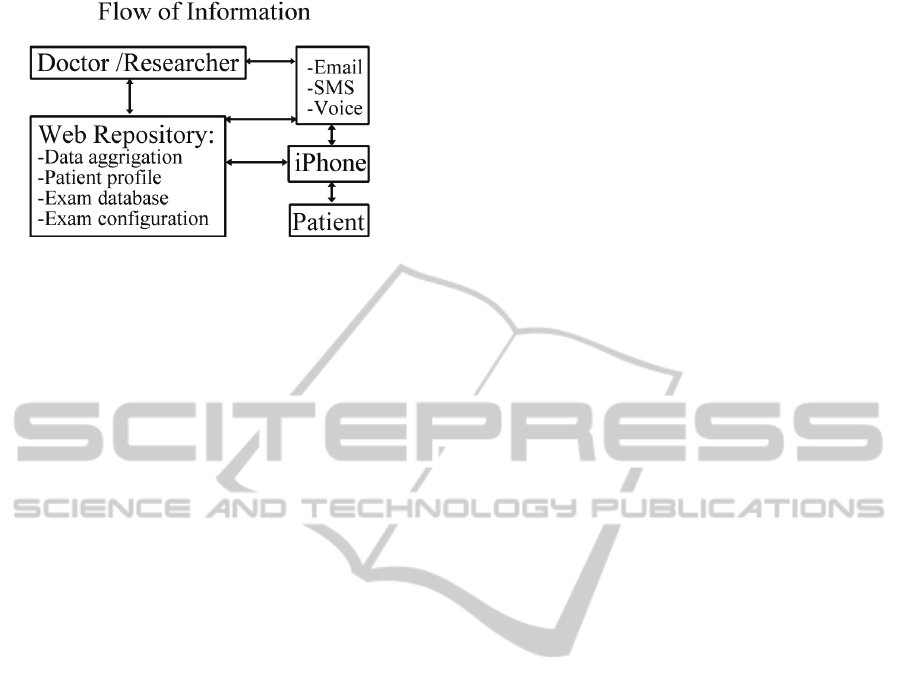
Figure 3: Flow of information.
3.1 Data Collection
Accelerometers inherently produce a small amount
of noise, and the iPhone accelerometer is no
different. iTrem compensates for with custom filters
and data smoothing algorithms. To date, the
collected data has been consistent. Validation has
been performed by comparing results from iTrem
with results gathered by the Mayo clinic using their
measurement instrumentation. More rigorous
validation will occur in the next phase of
development with the use of a motion capture
system. Using the high fidelity tracking capabilities
of the modern IR-based motion capture systems
iTrem will be able to measure in 3 dimensions hand
tremor displacement and compare that with the data
collected by the iTrem application.
4 FUTURE DEVELOPMENT
While continuing to develop the tremor tests the
iTrem team is now collaborating with a Movement
Disorder Specialist (MDS) and clinical researcher
whose specialty is the study and treatment of
Parkinson’s disease. The MDS has agreed to
determine the effectiveness of iTrem as a tool in the
exam room as well as the validity of the
measurements.
Simple games are also being developed to record
tremor data. The game is designed so that the motion
of the game play can be filtered out to reveal the
tremor data. Games also offer the capability to
gather baseline data from individuals without tremor
who are willing to play the game and contribute their
movements to the tremor database as well as allow
for the collection of data from patients who are
focusing on using tremor affect hands and arms to
perform tasks such as keep a character in the game
still.
ACKNOWLEDGEMENTS
Funding for this effort to date has been provided by
of the Georgia Tech Research Institute Electro-
Optical Systems Laboratory’s Landmarc Research
Center through Internal Research and Development
funding.
REFERENCES
Ahmed, Anwar, Sweeny, Patrick Tremor. Retrieved
March 2, 2010 from Cleveland Clinic:
http://www.clevelandclinicmeded.com/medicalpubs/di
sease management/neurology/tremors/.
Beers, Mark H. and Jones, Thomas V. The Merck Manual
of Health & Aging. Ballantine Books, New York,
2005. 357, 360.
Boelen, Miriam Health Professionals’ Guide to Physical
Management of Parkinson’s Disease. Human Kinetics,
Champaign, IL, 2009. 69.
Chen, Jack J. Swope, David M. Retrieved March 3, 2010
from Medscape: Essential Tremor: Disability
Associated with Essential Tremor: Clinical,
Functional, and Psychosocial. http://www.medscape.
com/viewarticle/461397_9.
Greenfield, Sheldon, M. D., Kaplan, Sherrie, Ph.D., M. P.
H; and Ware, John E., Jr., PhD Expanding Patient
Involvement in Care: Effects on Patient Outcomes.
Annals of Internal Medicine , April 1, 1985.
Grimes, David A. Parkinson’s: everything you need to
know. Firefly Books, Buffalo, New York, 2004.
DeMeyer, William Technique of the Neurologic
Examination. McGraw-Hill Companies, Inc., 2004.
347-348.
Rohkamm, Reinhard Color Atlas of Neurology. Thieme,
Stuttgart, Germany, 2004.
Niedermeyer, Ernst, da Silva, F. H. Lopes
Electroencephalography, 4th Ed., Lippincott Williams
& Wilkins, Philadelphia, PA 1999.
Stressometer: www.tnr.fr
Tabini, Marco comScore: Apple gained US smartphone
market share in December. Retrieved March 4, 2010
from MacWorld: http://www.macworld.co.uk/
Tarsy, Daniel, Vitek, Jerrold Lee, and Lozano, Andres M.
Surgical treatment of Parkinson’s disease and other
movement disorders. Humana Press Inc., Totowa,
New Jersey, 2003.
Tremorometer: www.managingtremor.com/.
Xu, Jiaquan, M. D., Kochanek, Kenneth, M. A., Murphy,
B. S. and Tejada-Vera, B. S. National Vital Reports.
U.S. Department of Health and Human Services,
Hyattsville, MD, 2007.
HEALTHINF 2011 - International Conference on Health Informatics
118
