
MOBILE TIMELINE EMR SYSTEM
Support System for Doctors’ Cognition/Analysis
Keisuke Ogawa, Kazunori Matsumoto, Masayuki Hashimoto, Tatsuaki Hamai
KDDI R&D Labs, Inc. 2-1-15 Ohara, Kamifukuoka, Saitama 356-8502, Japan
Yoshiaki Kondo
Tohoku University Graduate School of Medicine, Tōhoku, Japan
Wise Solutions, Inc., Plymouth, Michigan, U.S.A.
Keywords: Electronic medical records, Timeline, visualization of medical data, XEUS, Word completion, Adaptive
data mergence, Social patient list, Mobile, XML.
Abstract: In this paper, we propose a novel electronic medical record system (EMR) based on a brand new concept to
support doctors’ cognition and medical analysis wherever they are. Conventional EMR systems have the
advantage of helping doctors easily retrieve and manage mass medical records. On the other hand, medical
records have been expected to support doctors’ planning. Most conventional EMR systems don’t have an
appropriate function for such purpose, however. Because of its poor user interface, which is similar to
legacy medical records written on paper, they can’t help doctors analyze medical data that occurs
chronologically. To attain that purpose, the system has to have the ability to visualize medical data that
occurs over various time spans. This is because the relationship among the different medical data should be
observable when we look at it over various time spans. In addition, doctors aren’t always at their desks, so
they can’t always use EMR systems with a desktop PC. Therefore, in view of these problems, we propose a
system that has timeline interface which visualizes medical data that occurs over various time spans and its
client application works on a mobile device. In this manner, the system can support doctors’ cognition and
medical analysis wherever they are. In addition, we are verifying this system in the medical field.
1 INTRODUCTION
EMR systems are becoming popular in medicine
(A.L.Rector. 1996 , Anderson JD. 1999 , David W.
Bates et al. 2003 , Samuel J. Wang et al. 2003 , Jim
Johnson. 2010). This is because the system enables
doctors to manage mass medical data easily. As
represented by POMR (Weed LL. 1968), medical
record systems have been expected to support
doctors’ planning. But most of these EMR systems
are merely electronic data storage of legacy medical
records. For such purpose, the system has to have
the ability to visualize medical data that occurs over
various time spans. Because medical data often
occurs over various time spans, doctors have to
visualize it over various time spans for a medical
analysis. With these systems, doctors can look at
medical data for only a few days at most.
Accordingly, doctors can’t analyze medical data
effectively. In addition, there is another problem that
doctors don’t have much time to use the EMR at
their desks. As a result of these problems, doctors
desire a system that can support their cognition and
medical analysis anywhere. In view of these
problems, we propose a mobile timeline EMR
system that supports doctors’ cognition and medical
analysis. This system has the features listed below:
・ It has the ability to visualize medical data that
occurs chronologically over various time spans.
・ Its client application works on a mobile device
such as a mobile phone or a tablet PC.
・ In spite of the narrow bandwidth of wireless
mobile networks, the system responds quickly.
In this paper, we introduce the conventional EMR
systems in section 2 and reveal their problems. In
section 3, to solve these problems, we introduce the
mobile timeline EMR system and its technological
features.
405
Ogawa K., Matsumoto K., Hashimoto M., Hamai T. and Kondo Y..
MOBILE TIMELINE EMR SYSTEM - Support System for Doctors’ Cognition/Analysis.
DOI: 10.5220/0003287604050410
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 405-410
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
2 CONVENTIONAL EMR
SYSTEMS
In this section, we introduce the conventional EMR
systems. They can be divided into two types used in
medicine as listed below:
・ A system that has a user interface similar to
legacy medical records written on paper (type-1).
・A system that has a user interface that summarizes
the data of medical examinations over the last few
days (type-2).
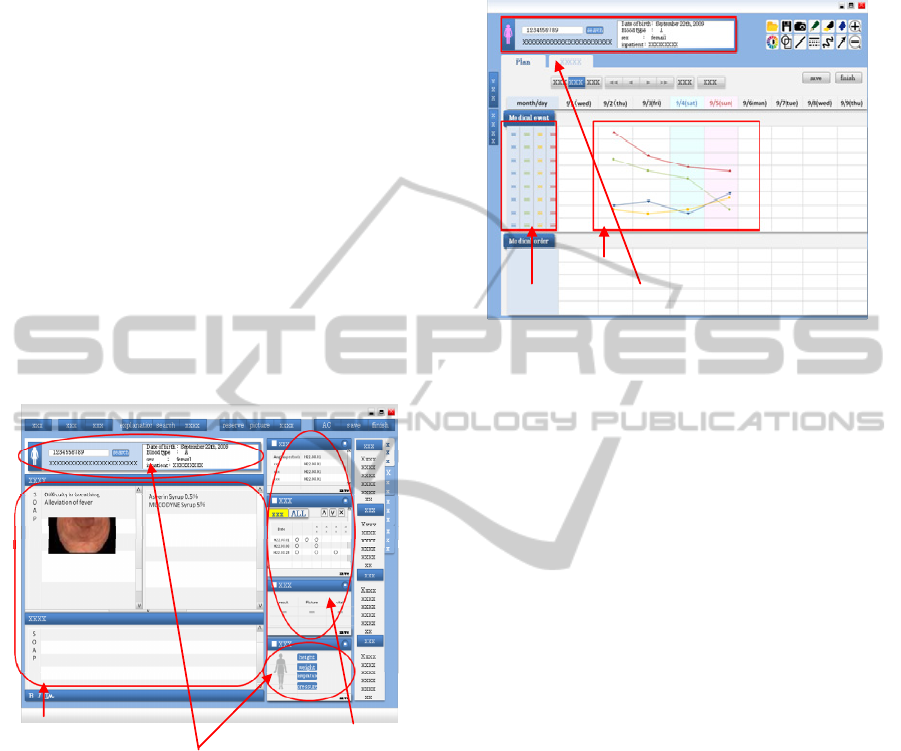
Figure1 shows the client application of a type-1
EMR system that displays SOAP information, the
patient’s information, and histories of medical
exams. With these systems, by treating medical data
as electronic data, doctors can search and manage
their patients’ medical data easily. This ability of
mass data management is a significant advantage
compared with legacy medical records.
Informationofthepatient
SOAP information
Historiesofmedicalexams
Figure 1: Conventional EMR system (type-1).
Figure2 shows the client application of a type-2
EMR system. It can display the data over the fixed
term. Due to the restriction of the size of the display,
in general, it displays the data over the short term.
However, there are various kinds of medical data
occurring over various time spans. So with these
systems, which can visualize medical data for only a
few days, doctors can’t always look at it and infer
the relationship among them. In other words, though
doctors can look at and understand the state of
patients who come two or three times with these
systems, they never can look at and understand the
state of patients who are suffering for years, such as
asthmatics, diabetics or patients suffering from
hypertension. Accordingly, these systems don’t
attain the purpose of supporting doctors’ analysis
and cognition.
InformationofthepatientMedicalEvents
Medicaldatainthefixedshortterm
Figure 2: Conventional EMR system (type-2).
3 MOBILE TIMELINE EMR
SYSTEM
As described above, in order to meet the demands of
supporting doctor’s cognition and medical analysis,
the system must have a function to visualize medical
data that occurs over various time spans and allow
doctors to look at medical data from any perspective.
So we introduced timeline interface to solve this
problem. Timeline interface visualizes the medical
data in chronological order. Timeline interface has a
multistage time scale such as years, months and days,
etc. With timeline interface, the system can visualize
chronological data over various time spans.
In addition, to meet the demands of mobility and
portability, we use a mobile device as a client of this
system. By adopting a mobile device, the system
gains a significant advantage in that doctors can
inspect and analyze the data anywhere, but mobile
devices have some problems as listed below:
(1) Difficulty with input and reading with a small
display
(2) Low data transmission rate through mobile
wireless network
To solve problem (1), we adopted the functions
listed below:
・ Advanced word completion using optimized
lexicon for each medical branch.
・ Social patient list that aims to reduce the input by
reusing the search histories in each medical branch.
HEALTHINF 2011 - International Conference on Health Informatics
406
For problem (2), we adopted the functions listed
below:
・ An Adaptive data mergence function that merges
neighboring data objects adaptively. This reduces
the amount of data transmitted.
・ An XML document encoding system that
reduces the amount of data transmitted by
transforming the XML plaintext to small binary data.
In this manner, we can realize the tool based on the
concept of supporting doctors’ cognition and
analysis wherever they are. These functions are
described below in detail.
3.1 Timeline Interface
Timeline interface is the most important part of this
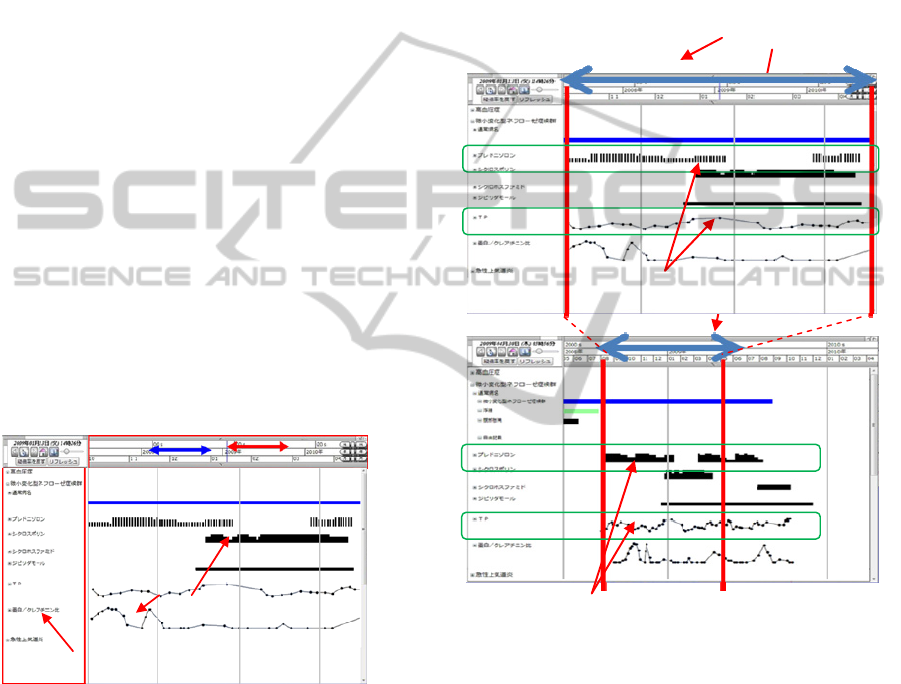
system. Figure3 shows it. Doctors can change the
time scale to various time units by controlling the
bar on the upper part. For example, by clicking the
bar, doctors can change the day unit time scale to the
month unit scale or the hour unit scale. By changing
the time scale to a smaller unit scale, doctors can
observe medical data over a short time span in detail.
Conversely, by changing the time scale to a bigger
unit scale, doctors can look at medical data over a
long time span. Also, we can change the length of
the time unit by pinch-in/pinch-out.
Wecanchangethetimescaleeasily.
Zoomout
Zoomin
Namesofmedicaleventssuchasmedication,
disease
,
ins
p
ectionandsoon
Dataobjectswhichstandfor
medicalevents
Figure 3: Timeline interface.
The reasons why we use this interface are described
below:
・ There are various kinds of medical data. They
occur chronologically and there are often several
relationships among them.
・ When there is a relationship among the different
data, the appropriate time scale to observe exists. By
selecting the time scale properly, the system can
visualize the relationship among the data.
For example, take the case where we can discover
the relationships when we observe the data over a
long time span, even if we can’t discover it over a
short time span. Conversely, we can’t discover it
with an overly long time span. Accordingly, the
system must have a function that allows users to
select the appropriate time scale.
With this timeline interface, doctors can change
the time scale as they wish. Therefore, doctors can
observe the various relationships between various
data. In other words, doctors can inspect medical
data from various points of view. Figure4 shows an
example of observable relationships.
Sametimespan
ValueB
MedicationA
Wecan’tobserveanyrelationshipswiththe
shorttimescale.
We can discover the relationships with the long time
scale.Inthiscase,we canobservea possibilityofthe
fact that stopping the” medication A” causes a
decreaseo
f
“
valueB”.
MedicationA
ValueB
Figure 4: Visualization of the relationships among medical
data.
In this manner, this system can be not only a
management tool for medical data, but also a tool for
supporting doctors’ cognition and medical analysis.
3.2 Word Completion using Lexicon
for Medical Data
The input method is not only an important factor that
decides the usability of the system on mobile
devices, but also a difficult problem. This is because
mobile devices only have poor input accessories
MOBILE TIMELINE EMR SYSTEM - Support System for Doctors' Cognition/Analysis
407
such as small touch panels and keyboards. In
particular, in EMR systems, doctors have to input
special characters for medical treatment using these
poor input devices to write down the SOAP
information or to search patients. To solve this, it is
common knowledge that the word completion
method using a lexicon of medical words is effective
(Laird S. Cermak et al 1992, C. G. Chute et al 1999,
Hiroyuki Komatsu et al 2001). However, the words
used in medicine differ significantly among each
branch. In other words, there is a problem that using
the same lexicon among all the branches is
insufficient. For example, the phrase nephrotic
syndrome is often used by pediatricians, but is rarely
used by ophthalmologists. Accordingly, we optimize
the lexicon for each branch. Simply put, we changed
the bias of the TRIE (Donald R. Morrison 1968)
structure of the lexicon for each branch. Then for
each branch, by summarizing and analyzing the
doctors’ input history commonly, the system
succeeded in improving the accuracy of word
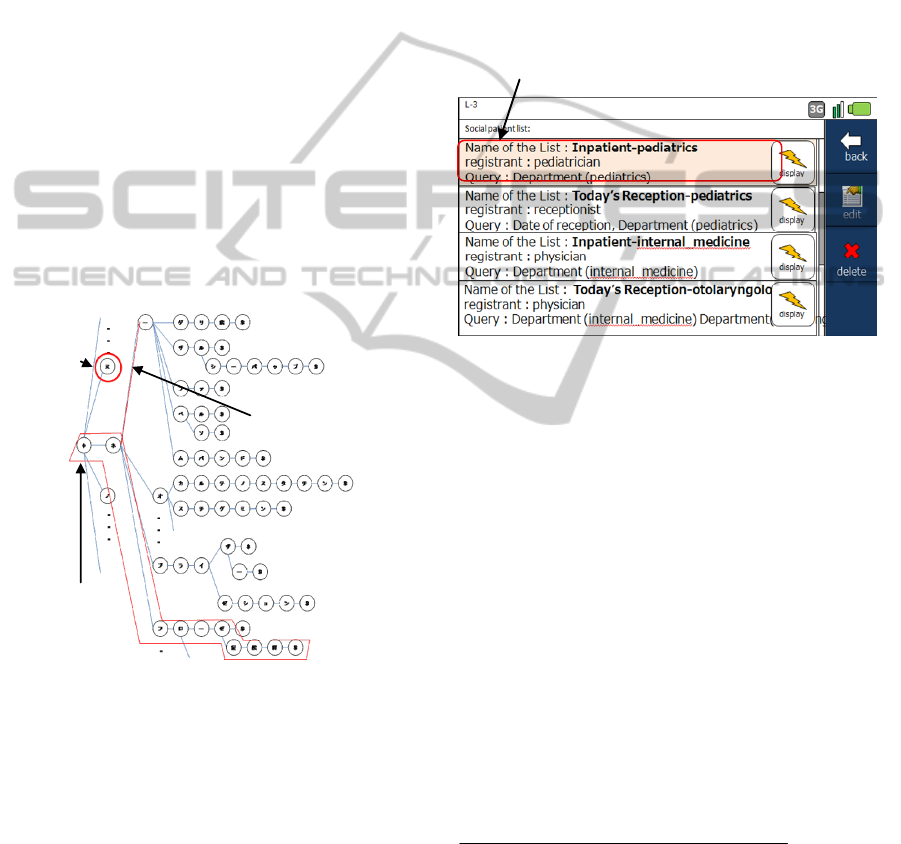
completion. Figure5 shows an example of the TRIE
structure in Japanese.
Oneletter
C
hangingtheweight
betweenletters
Onewor
d
Figure 5: TRIE structure for lexicon of medical words in
Japanese.
Here, we use φ for the head of the sentence and
$ for the tail of the sentence. By adding word
frequency of doctors’ own input history, word
frequency of other doctors’ input history in the same
branch and the cost of prediction to the tail of the
sentence, we can make the TRIE structures for each
branch.
3.3 Social Patient List
In this subsection, we introduce another function for
the purpose of reducing input, which is called the
social patient list in this system. By using the social
patient list, doctors can search for patients using
useful queries without using a keyboard that is
difficult to use. Social patient list is a function that
enables doctors to save search queries as a list of
patients and have them in common in each branch.
In other words, doctors in the same branch can
utilize the useful search histories of other doctors as
if they were their own. The figure presented below is
an example of a social patient list. By clicking the
display button, doctors can easily reuse the search
queries of other doctors.
Searchqueriesofotherdoctorsinthesamebranch
Figure 6: Social patient list.
3.4 Adaptive Data Mergence
The response speed of the system is a very important
factor for deciding the system’s usability. The
advantage of timeline interface is, as we described
above, the ability to visualize the relationships of
medical data with various time scales. If doctors
want to look at the data in the long time span, they
can enlarge the time scale as they wish. In this
manner, however, the system has to display a lot of
data objects at once. On the other hand, in this
system, since its client is a mobile device, the client
only has narrow wireless communication bandwidth.
In order to improve the response speed in this
system, we use adaptive data mergence. Adaptive
data mergence is a function that merges neighboring
data objects adaptively. We use the formula below
as a threshold to merge data objects.
___ ___
:
Start time of objectA end time of objectB
threshold x
timescale
−
<
As we described in Figure7, when doctors enlarge
the time scale, if the time gap of the data objects is
smaller than the threshold, the system merges the
objects to one object. In this manner, the system can
reduce the amount of data and improve the response
speed and usability.
HEALTHINF 2011 - International Conference on Health Informatics
408
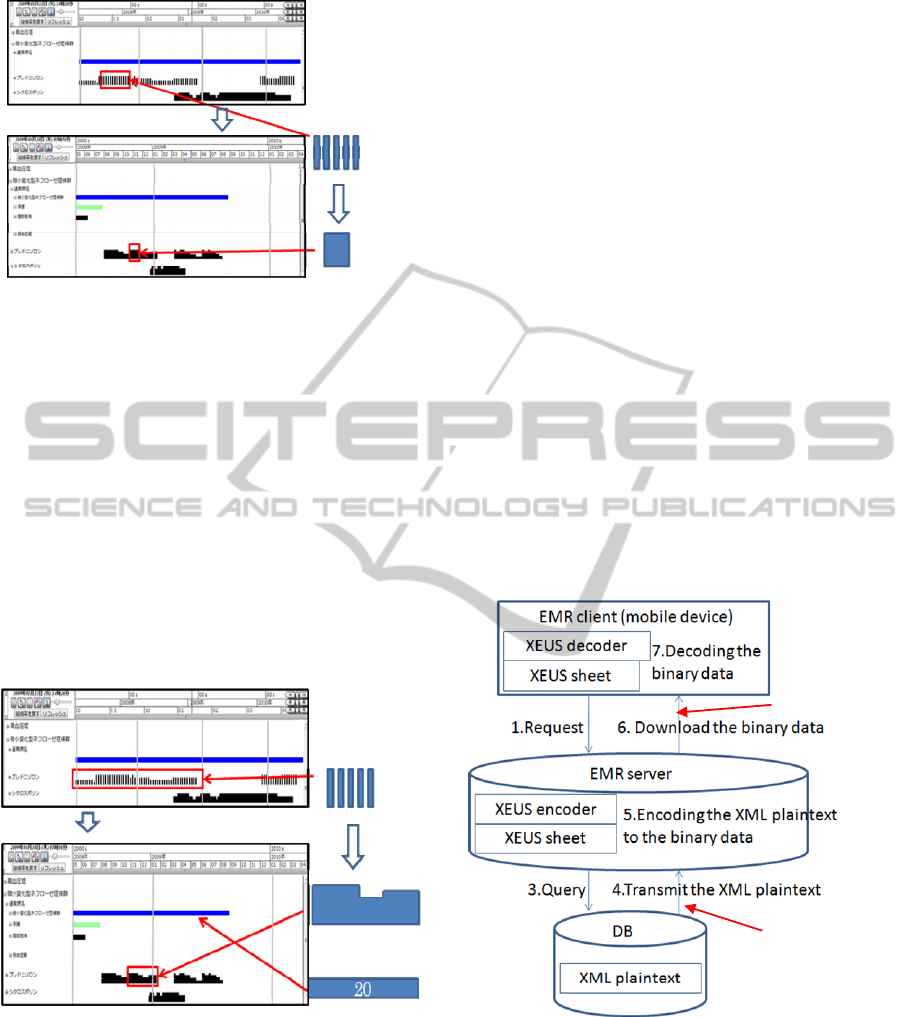
C
hangingthetimescale Somedataobjects
Representingasintegratedone
objectautomatically
Figure 7: Adaptive data mergence.
In addition, there are various types of graphs for
the data objects and the best graphs for the data
objects are different from each other. If doctors want
to observe the flow of medication data, a line graph
is the best representation. In another example, if
doctors want to look at the frequency of the
examination data, a histogram is the best
representation. Adaptive data mergence has the
ability to select the best representation automatically
by learning the history in the same branch. As
represented below in Figure8, the system has the
ability to change the representation depending on the
data.
Representingthenumberofobjects
Somedataobjects
Representingthefigure
C
hangingthetimescale
Figure 8: Various graph representations for data objects.
3.5 XML Document Encoding System
Recently, MML (Kenji Araki et al. 2000 , Jinqiu
Guo et al 2003), which is the standard data format to
transmit medical data between two different EMR
systems, has been proposed. MML is a format based
on XML. In addition, in this mobile timeline EMR
system, we use a data format based on MML. The
common XML document is the plaintext data, so it
provides the advantage of high readability and high
extensibility. XML also results in a disadvantage in
respect to data size, safety and parse processing load
in terms of data reception, however. Therefore, in
this system, we solve these problems by adopting the
XEUS (Kobayashi Arei et al. 2001) XML document
encoding system. XEUS is the abbreviation of XML
document Encoding Universal Sheet and a system
for encoding XML documents. Now, we describe
the procedure of the XEUS system.
1
st
step: Define the XEUS sheet which is a document
that has the logical structure and a table of the
encoding. The XEUS sheet is described by XML.
2
nd
step: By using this XEUS sheet in the encoder,
we can encode the large plaintext XML document
into a small binary document. This is because the
encoder can separate the plaintext XML document
into the logical structure and serialized data, and
transforms it into small binary data. Then in the
decoder, by using the same XEUS sheet, which
defines the logical structure, we can decode the
small binary document. Figure9 shows the concept
of the XEUS system.
Narrowbandwidth
Broadbandwidth
Figure 9: XEUS system.
In this mobile timeline EMR system, the EMR
server that has medical data has the encoder and the
mobile device that displays the EMR data has the
decoder. In general, XML documents result in the
data becoming one-fifth the original size. This is a
significant help for the client of this system, which
only has narrow wireless communication bandwidth.
MOBILE TIMELINE EMR SYSTEM - Support System for Doctors' Cognition/Analysis
409

4 CONCLUSIONS
In this paper, we proposed an EMR system based on
the brand new concept. This system has a significant
advantage to support doctors’ cognition and medical
analysis wherever they are. The system has the three
features described below.
・ Since this system has timeline interface, doctors
can look at and analyze medical data by using
various time scales. This is a significant help for
doctors’ cognition and analysis.
・ Since its client is a mobile device, the system can
support doctors’ cognition and medical analysis
wherever they are.
・ In spite of using a mobile device as a client, this
system guarantees ease of use as much as possible.
In addition to the features described above, making
use of the advantage of easy use, there is a
possibility that the doctors can use this system as an
educational tool.
REFERENCES
A. L. Rector., 1996. Computer-based Patient Records,
Yearbook of Medical Informatics, Section 2, 195-198.
Anderson J. D., 1999. Increasing the acceptance of clinical
information systems. MD Computing.16(1)62-5.
David W. Bates, Mark Ebell, Edward Gotlieb, John Zapp,
and H. C. Mullins., 2003. A Proposal for Electronic
Medical Records in U.S. Primary Care, J Am Med
Inform Assoc.
Samuel J. Wang, Blackford Middleton, Lisa A. Prosser,
Christiana G. Bardon, Cynthia D. Spurr, Patricia J.
Carchidi, Anne F. Kittlera, Robert C. Goldszer, David
G. Fairchild, Andrew J. Sussman, Gilad J. Kuperman,
David W. Bates,2003. A cost-benefit analysis of
electronic medical records in primary care. The
American Journal of Medicine.
Jim Johnson., 2010. Making A Successful Transition To
Electronic Medical Records. Healthcare Technology
Online.
Weed LL., 1968. Medical records that guide and teach.
New England Journal of Medicine 278:593-600.
Laird S. Cermak, Mieke Verfaellie, Marie Sweeney and
Larry L. Jacoby, 1992. Fluency versus conscious
recollection in the word completion performance of
amnesic patients, Brain and Cognition Volume 20,
Issue 2, Pages 367-377.
C. G. Chute, P. L. Elkin, D. D. Sherertz, and M. S.
Tuttle,1999. Desiderata for a clinical terminology
server, Proc AMIA Symp.
Hiroyuki Komatsu, Akira Takabayashi, Toshiyuki Masui,
2001. Predictive Text Input with Japanese Dynamic
Abbreviation Expansion Method “Nanashiki”, WISS.
Donald R. Morrison,1968. PATRICIA-Practical
Algorithm To Retrieve Information Coded in
Alphanumeric, jacm.
Kenji Araki, Katsuhiro Ohashi, Shunji Yamazaki,
Yasuyuki Hirose, Yoshinori Yamashita, Ryuichi
Yamamoto, Kazushi Minagawa, Norihiro Sakamoto
and Hiroyuki Yoshihara ,2000. Medical Markup
Language (MML) for XML-based Hospital
Information Interchange, Journal of Medical Systems.
Jinqiu Guo, Kenji Araki, Koji Tanaka, Junzo Sato,
Muneou Suzuki, Akira Takada, Toshiaki Suzuki,
Yusei Nakashima and Hiroyuki Yoshihara, 2003. The
Latest MML (Medical Markup Language) Version 2.3
XML-Based Standard for Medical Data
Exchange/Storage, Journal of Medical Systems.
Kobayashi Arei, Takagi Satoru, Muramatsu Shigeki, Baba
Akira, Matsumoto Kazunori, Inoue Naomi, 2001. The
general XML document encoding system "XEUS",
IEIC Technical Report. (Institute of Electronics,
Information and Communication Engineers).
HEALTHINF 2011 - International Conference on Health Informatics
410
