
*
Supported by the MEC-Spain under contract TIN2007-64974
AN AGENT-BASED DECISION SUPPORT SYSTEM
FOR HOSPITAL EMERGENCY DEPARTMENTS
*
Manel Taboada
1
, Eduardo Cabrera
2
and Emilio Luque
2
1
Tomas Cerda Computing Science School, Universidad Autonoma of Barcelona (UAB), Barcelona, Spain
2
Computer Architecture and Operating Systems Department (CAOS)
Universidad Autonoma of Barcelona (UAB), Barcelona, Spain
Keywords: Healthcare operational management, Agent-based modelling, Individual oriented simulation, Emergency
department, Decision support systems.
Abstract: Healthcare operational management provides many areas where modelling and simulation have been shown
to be useful tools, and within this field there is probably no area more fluid or dynamic than hospital
emergency departments (ED). This paper presents the results of an ongoing project that is being carried out
by Individual Oriented Modelling (IoM) research group of the UAB, with the participation of Hospital ED
Staff Teams. The general objective is creating a simulator that, used as decision support system (DSS), aids
the heads of the ED to answer both, “what if...” questions in order to make the best informed decisions
possible, and more complex questions involving the optimisation of the system. The defined ED model is a
pure Agent-Based Model, formed entirely of the rules governing the behaviour of the individual agents
which populate the system. Two distinct types of agents have been identified, active and passive. Active
agents represent human actors, meanwhile passive agents represent services and other reactive systems.
Active agents are described by Moore state machines extended to include probabilistic transitions. With the
aim of verifying the proposed model a simulation has been created using NetLogo.
1 INTRODUCTION
Healthcare is one of the most important services in
modern civilisation. In a hospital there are many
complex, independent, but interrelated departments
(Decker, 1998). The Emergency Department (ED)
may well be one of the most complex and fluid
healthcare systems that exists, consuming a large
portion of economic budgets for health services.
However, patients often feel neglected and that the
service is saturated.
The simulation of complex systems is of
considerable importance and is used in a broad
spectrum of fields such as engineering, biology,
economy and health care. There are no standard
models to describe these complex systems, but they
may share many common traits. Agent-Based
Modelling (ABM) is an efficient and well utilised
technique that has many advantages, amongst them
is increased detail in simulation based experiments,
a transparent learning process, and the ability to a
control and easily modify individual behaviour.
This paper presents the results of an ongoing
project that is being carried out by Individual
Oriented Modelling (IoM) research group of the
UAB, with the participation of the ED Staff Team of
the Hospital of Sabadell. Its general objective is
create a simulator that, used as decision support
system (DSS), aids the heads of the ED to allow
additional knowledge of patient admission
scheduling (Hutzschenreuter et al., 2008), physician
staff (Jones and Evans, 2008), resource optimisation,
and decreased patient waiting time (Laskowski and
Mukhi, 2008).
Following Macal and North (2006), and also
making use of the considerable expertise existing
within the IoM research group, a concrete and
continuous development methodology has been
devised for the construction of the tool, following an
iterative & spiral process. Each cycle involves 5
phases: 1) system analysis; 2) model design; 3)
simulator implementation; 4) simulator execution
and results analysis; 5) simulator validation. Once
417
Taboada M., Cabrera E. and Luque E..
AN AGENT-BASED DECISION SUPPORT SYSTEM FOR HOSPITAL EMERGENCY DEPARTMENTS.
DOI: 10.5220/0003291804170422
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 417-422
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

the first iteration has been completed, based on the
conclusions obtained during the analysis and
validation phase, the model is updated and a new
cycle is carried out. The process will be repeated
until the objectives are achieved.
An Agent-Based Model for Emergency
Departments is being designed, in which all rules
within the model concern the agents, no higher level
behaviour is modelled; it emerges as a result of local
level actions and interactions. This model describes
the complex dynamics found in a hospital ED,
representing each individual and system as an
individual agent. After ending the first cycle two
distinct kinds of agents have been identified, active
and passive. Active agents represent the individuals
involved in the ED, in this case all human actors,
such as patients, nurses or doctors. Passive agents
represent services and other reactive systems, such
as the information technology (IT) infrastructure or
central services used for performing tests.
In order to simulate the model state machines are
used to represent the actions of each agent and the
communication between agents. This takes into
consideration all the variables that are required to
represent the many different states that an individual
may be in throughout the course of their time in a
hospital emergency department, be that individual a
patient, a member of hospital staff, or any other role.
The change in these variables, invoked by an input
from an external source, is modelled as a transition
between states. The communication between
individuals is modelled as the inputs that agents
receive and the outputs they produce, both implicitly
and explicitly. In order to control the agent
interaction, the physical environment in which these
agents interact also have to be modelled, being
sufficient do it as a series of interconnected areas,
such as admissions, the waiting room, or
consultation suits.
In the next cycles new agents and state variables
will be added gradually, until the simulator behaves
as similar as possible to the real system, although
being less complex. After this, data assimilation and
optimisation techniques will be used for new
improvements of the tool. Parallel simulations with
different parameters will be performed, in order to
make adjustments to the model based on the
comparison of the results of these simulations with
data from real systems. High Performance
Computing will be necessary due to the high amount
of data and computation inherent to these both
phases.
The remainder of this article is organised as
follows; section 2 describes the related work in
healthcare operational management and simulation.
The proposed emergency department model is
detailed in section 3, while the corresponding
simulation is given in section 4. In section 5 the
future work is pointed out. Finally, section 6 closes
with conclusions.
2 RELATED WORK
The modelling and simulation of hospital emergency
departments sits at the intersection of a number of
distinct fields. In addition Agent-based techniques
have been used in the modelling of healthcare
operational management, but there are few pure
agent-based models to be found in the literature that
have been rigorously validated against their real
world counterparts.
Economics, biology, and social sciences are the
three fields in which agent-based models are most
utilised (Jones and Evans, 2008). Modelling
techniques using agents can bring the most benefit
when applied to human systems where agents
exhibit complex and stochastic behaviour, the
interaction between agents are heterogeneous and
complex, and agent positions are not fixed
(Bonabeau, 2002). In the particular case of social
sciences ABMs are used in situations where human
behaviour cannot be predicted using classical
methods such as qualitative or statistical analysis
(Norling and Sonenberg, 2000). Human behaviour is
also modelled with ABMs in the fields of
psychology (Smith and Conrey, 2007) and
epidemiology (Epstein, 2009) amongst others.
Agent technology is a useful tool when applied
to healthcare applications. Previous works modelling
healthcare systems have focused on patient
scheduling under variable pathways and stochastic
process durations, the selection of an optimal mix
for patient admission in order to optimise resource
usage and patient throughput (Hutzschenreuter et al.,
2008). Work has been performed using differing
degrees of agent-based modelling for evaluating
patient waiting times under the effects of different
ED physician staffing schedules (Jones and Evans,
2008) or patient diversion strategies (Laskowski and
Mukhi, 2008).
This proposal addresses many of the issues
surrounding the modelling and simulation of a
hospital emergency department using agent-based
technologies. The basic rules governing the actions
of the individual agents are defined, in an attempt to
understand micro level behaviour. The macro level
behaviour, which means the system as a whole,
HEALTHINF 2011 - International Conference on Health Informatics
418

emerges as a result of the actions of these basic
building blocks, from which an understanding of the
reasons for system level behaviour can be derived as
shown Staindsby, Taboada and Luque (2009).
3 EMERGENCY DEPARTMENT
MODEL
The Emergency Department model defined in this
work is a pure Agent-Based Model, formed entirely
of the rules governing the behaviour of the
individual agents which populate the system.
Through the information obtained during interviews
carried out with ED staff at the Hospital of Mataro
and the Hospital of Sabadell, two kinds of agents
have been identified; these are active and passive
agents. The active agents represent people and other
entities that act upon their own initiative (patients,
companions of patients, admission staff, sanitarian
technicians, triage and emergency nurses, staff
emergency doctors, specialists, and social workers).
The passive agents represent systems that are solely
reactive, such as the loudspeaker system, patient
information system, pneumatic pipes, and central
diagnostic services (radiology service and
laboratories).
This section is dedicated to describe the various
components of the general model in detail. Section
3.1 explains the manner in which active agents are
modelled. Passive agents are discussed in section
3.2. The communication model is defined in section
3.3. Finally in section 3.4 the details of the
environment where the agents move and interact are
outlined.
3.1 Active Agents
Active agents are described by state machines,
specifically Moore machines. A Moore machine has
an output for each state; transitions between states
are specified by the input. Considering this, the
current state of an active agent is represented by a
collection of “state variables”, known as the state
vector (T). Each unique combination of values for
these variables defines a distinct state. In each time
step the state machine moves to the next state as
defined by the current state and the input vector as
described below.
3.1.1 State Variables
In order for the state machine to function, all state
variables must be enumerable in some manner. This
may be discrete variables or variables representing
continuous quantities which have been divided into
ranges.
An initial set of state variables has been defined
through the round of interviews performed, based on
the minimum amount of information required to
model each patient and member of staff. Such state
variables are: name/identifier (for identifying each
individual), personal details (any individual
information which is important in relation with his
stay in the ED, such as age, medical history, origin,
etc.), location (the area of the ED where the
individual currently is), action (what the individual
in a particular state is doing), physical condition
(haemodynamic-constants and the degree of
dependence following the Barthel Index), symptoms
(healthy, cardiac/respiratory arrest, severe/moderate
trauma, etc. Information reported by the patient, and
classified by ED staff following the relevant triage
and acuity scale, the Canadian or the Andorran
scale, depending on the country of the Hospital),
communication skills (The time spent during the
process depends on the agent’s ability to
communicate. The possible values are low, medium
or high), and level of experience of the ED staff
(None, low, medium or high), which also influences
the processing time. Some of the state variables will
have a potentially very large set of possible values,
e.g. the symptoms or physical condition.
3.1.2 Inputs, Outputs & State Transitions
Upon each time step the state machine moves to the
next state. This may be another state or the same one
it was in before the transition. The next state the
machine takes is dependent on the input during that
state. The input may be more accurately described as
an input vector (I) that contains a number of input
variables, each one of which may take a number of
different values. As this is a Moore machine, the
output depends only on the state, so each state has its
own output, although various states may have
outputs that are identical.
Table 1: State transition table.
AN AGENT-BASED DECISION SUPPORT SYSTEM FOR HOSPITAL EMERGENCY DEPARTMENTS
419
Again, the output is more accurately described as an
output vector (O), a collection of output variables,
each with a number of defined possible values.
Transitions between states are dependent on the
current state at time t (St) and the input at time t (It).
Following the transition the state machine will be in
a new state (St+1). The state machine can be
represented as a state transition table, as shown in
Table 1, where each row represents a unique state
input combination, showing the output and the state
in the next time step (defined by the current state
and the input).
3.1.3 Probabilistic State Transitions
In dynamic and complex systems such as hospitals,
there exists the necessity for a model not to be
entirely deterministic. In these cases a state machine
can be modelled with more than one possible next
state given a current state and input combination.
Which transition is made is chosen at random at the
time of the transition, weights on each transition
provide a means for specifying transitions that are
more or less likely for a given individual. Each one
of the input variable of the input vector (I) may take
a number of different values. In these cases the state
transition table is defined with probabilities on the
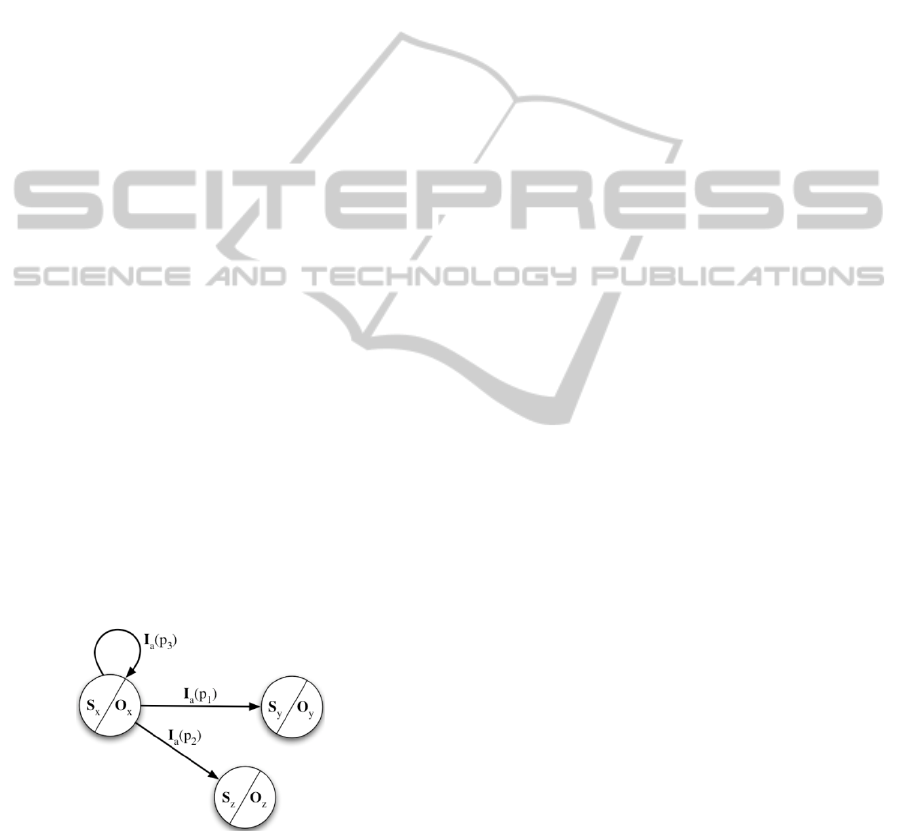
“effect” of the input. An agent in state S
x
receiving
input I
a
may move to either state S
y
, state S
z
, or
remain in the same state, with a probability of p
1
, p
2
,
and p
3
respectively. One of these transitions will
always occur, which is to say p
1
+ p
2
+ p
3
= 1.
Figure 1 shows the three different transitions for the
“current state-input” combination of this specific
example.
Figure 1: Probabilistic state transitions graph
representation.
The exact probabilities may be different for each
agent, in this way agent behaviour can be
probabilistically defined external to their state,
representing personality characteristics in different
people.
3.2 Passive Agents
Passive agents represent services within the hospital
system such as the IT infrastructure that allows
patient details to be stored, radiology services and
other laboratory tests as well as specialist systems
such as the pneumatic tube networks that some
larger hospitals use to quickly transfer samples from
one part of a building to another.
Not all passive agents are modelled using state
machines. In some cases this may be overly
complicated, due to systems with register like
memory capacities; in others a simple store and
forward messaging system is sufficient.
3.3 Communication Model
To model the interaction between agents 3 types of
communication are proposed:
1-to-1 between two individuals;
1-to-n is representing an individual addressing a
group;
and 1-to-location a type of communication
where an individual speaks to all occupants of a
specific area, for instance using a speaker
system.
Messages contain three parts. The message
source is the individual who is communicating,
speaking in many cases. The message destination
would then be to whomever this individual is
speaking to, and thirdly the content, what is being
said. These three parts form the message tuple
(<src>, <dst>, <content>). In the case of a 1-to-
location message, the destination of the message is
an entire location, so the content may need to
include the actual indented recipient of the message.
This could represent a patient’s name being called
over the loudspeaker system.
3.4 Environment
All actions and interactions modelled take place
within certain locations, collectively known as the
environment. The environment itself can be defined
to different levels depending on the positional
precision required of the model.
The environment in which the agents move and
interact is passive and discrete. There is little
distinction made between agents in the same
location. A patient in the waiting room does not
have any more specific sense of position than they
are in the waiting room. Certain locations may be
physically distinct, but functionally identical, for
instance there are usually a number of triage rooms,
HEALTHINF 2011 - International Conference on Health Informatics
420
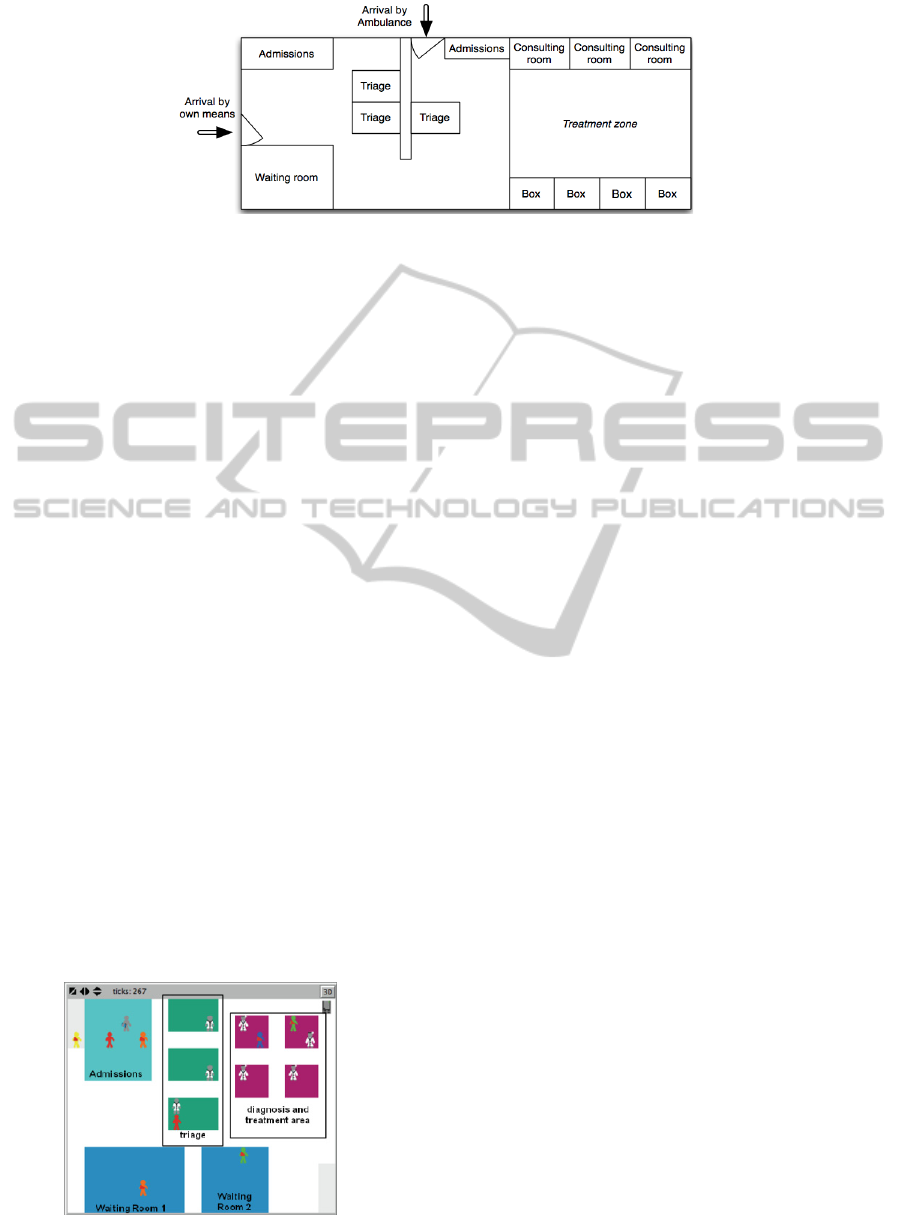
Figure 2: Simplified Emergency Department layout.
an agent in any one of these will act as if they are in
any triage room, however they Simplified ED layout
are distinct in order to represent that each available
room may only be used by one nurse-patient group
at a time.
The environment also contains representations of
the relative distances between different discrete
locations. Figure 2 shows a representation of
topographical distribution of the Emergency
Department.
4 SIMULATION
With the aim of verifying the proposed model
against real data sets from a hospital emergency
department a simulation has been created using the
agent based simulation tool NetLogo (Wilensky,
1999).
The tool initially uses a simplified set of patient
attributes and a less complicated patient flow in
order to make a preliminary demonstration of how
accurate a simulation can be produced using only
reduced parameters. The four primary areas are
accounted for: admissions, triage (3 boxes), waiting
rooms (one for patients before triage, and the second
for patients who have passed the triage process, and
are waiting for treatment), and diagnosis and
treatment areas conjoined (that include four boxes).
The types of individuals represented in this simula-
Figure 3: Simulation display in NetLogo.
tion are patients, admission staff, triage nurses, and
doctors.
In this model the patients are shown following
the same path through the ED, even though in reality
they are been treated differently depending on the
level of severity of their condition. The time spent at
each stage may also represent laboratory tests, which
are not shown explicitly.
Since a primary use of the simulation tool is to
garner feedback from the professionals who work in
emergency departments, a graphical representation
of the process is considered a very important aspect
of the simulation. NetLogo allows visualisations of
agent actions and interactions; a sparse patient load
is shown in figure
3.
There is further validation to be performed.
However initial tests using the simulation are
showing very promising results.
5 FUTURE WORK
Following the iterative & spiral process discussed in
the introduction, after this first cycle, the work will
continue with the purpose of improving the model
and the simulation, applying assimilation techniques
for that.
In the next iterations new agents and state
variables will be added gradually, until the simulator
behaves as similar as possible to the real system,
although being less complex. After this, parallel
simulations with different parameters will be
performed, in order to make adjustments based on
the comparison of the results obtained in these
simulations with data from real system.
Once the improving of the model achieves a
proper adjustment level, simulation will be used as
DSS, with the objective of answering “what if...”
questions in order to aid healthcare managers make
the best informed decisions possible. The tool will
let to divine what will happen to the system as a
whole if one or more changes are made to the
AN AGENT-BASED DECISION SUPPORT SYSTEM FOR HOSPITAL EMERGENCY DEPARTMENTS
421

parameters that define it. After additional definitions
of quantitative and qualitative indices, more
complex questions involving the optimisation of the
system could be evaluated. In these specific cases
simulation will be carried out with the objective of
minimising (patient waiting times, total service cost,
etc) or maximising (patient’s satisfaction) indices,
subject to specific constraints of human and material
resources available.
The distribution pattern of patients’ arrival to the
ED varies among the day, but also over a week or a
year. For this reason, and having into account the
objectives of the project, is desirable to run
simulations for an annual period of time. In addition,
as a result of the potential number of individuals to
include in the simulation and the number of states in
the state machine of each individual, a great amount
of values should be computed. Considering also the
parallel simulations that will have to be performed
during the adjustment process, it can be concluded
the need of using High Performance Computing.
6 CONCLUSIONS
A concrete example of an Agent-Based Model for
Hospital Emergency Departments has been
presented, which represents a hospital ED following
system analysis performed at a number of different
hospitals, under the advice of healthcare
professionals with many years of experience. The
model uses state machine based agents which act
and communicate within a defined environment,
providing the ability to study the dynamic of
complex systems without the difficulty of obtaining
exhaustive system descriptions required by other
modelling paradigms. An initial simulation has been
created in order to demonstrate the validity of the
model.
Future improvements of the model will be made
using data assimilation and optimisation techniques.
The former will involve performing parallel
simulations with different parameters, and after
comparing data from simulation and real system,
making the proper adjustments of the model. The
latter refers to optimisation through simulation runs
in order to minimise or maximise indices such as
patient waiting times, total service cost or patient
satisfaction, while adhering to constraints in the
number of doctors, nurses and hospital beds
available. In both parallelisation and High
Performance Computing will be necessary.
From this point, the simulation will be able to be
used as the core component of a decision support
system to aid hospital administrators make better use
of resources, achieving a more efficient and
improved patient care cycle. This in turn will allow
better management of dynamic patient flow, either
as a result of specific circumstances or seasonal
fluctuation.
REFERENCES
Bonabeau E., 2002. Agent-based modeling: Methods and
techniques for simulating human systems. In
Proceedings of the National Academy of Sciences.
Decker K, Li J., 1998. Coordinated Hospital Patient
Scheduling. In: Proceedings of the 3rd International
Conference on Multi Agent Systems. Washington, DC,
USA: IEEE Computer Society;
Epstein J. M., 2009. Modelling to contain pandemics. In
Nature, 460(7256):687.
Heath B, Hill R, Ciarallo F., 2009. A Survey of Agent-
Based Modeling Practices In Journal of Artificial
Societies and Social Simulation;12(4):9.
Hutzschenreuter A. K., Bosman P. A. N., Blonk-Altena I.,
van Aarle J., La Poutr´e H., 2008. Agent-based patient
admission scheduling in hospitals. In: Proceedings of
the 7th international joint conference on Autonomous
agents and multiagent systems. Richland.
Jones S. S., Evans R. S., 2008. An Agent Based
Simulation Tool for Scheduling Emergency
Department Physicians. In: AMIA Annual Symposium
proceedings,
Laskowski M., Mukhi S., 2008. Agent-Based Simulation
of Emergency Departments with Patient Diversion. In:
eHealth; p. 25–37.
Macal C., and North M., 2006. “Tutorial on agent-based
modeling and simulation part 2: how to model with
agents,” In: Proceedingsof the Winter Simulation
Conference, pp. 73 – 83.
Norling E., Sonenberg L., Ronnquist R., 2000. Enhancing
Multi-Agent Based Simulation with Human-Like
Decision Making Strategies. In: MABS; p. 214–228.
Smith E. R., Conrey F. R., 2007 Agent-Based Modeling:
A New Approach for Theory Building in Social
Psychology. In: Pers Soc Psychol Rev. 11(1):87–104.
Stainsby H., Taboada M., Luque E., 2009. Towards an
Agent-Based Simulation of Hospital Emergency
Departments. In: Proceedings of the 2009 IEEE
International Conference on Services Computing.
Washington, DC, USA: IEEE Computer Society
Wilensky U., 1999. NetLogo. Center for Connected
Learning and Computer-Based Modeling,
Northwestern University Evanston, IL.
HEALTHINF 2011 - International Conference on Health Informatics
422
