
Event-based Workflow Analysis in Healthcare
Eva Gattnar
1,2
, Okan Ekinci
1
and Vesselin Detschew
2
1
Clinical Competence Center Cardiology, Siemens Healthcare
Allee am Röthelheimpark 3a, 91052, Erlangen, Germany
2
Institute of Biomedical Engineering and Informatics, Ilmenau Technical University
POB 100565, 98684 Ilmenau, Germany
Abstract. Efficiency and high quality of care are nowadays demanded by
healthcare organizations. Clinical workflow analysis is an important element of
quality improvement efforts in hospitals. Standardized process models can
support process monitoring and mining in healthcare delivery. Therefore our
paper presents a promising approach for measuring Key Performance Indicators
(KPIs) in hospitals based on a newly developed clinical process model. In order
to measure process performance, it addresses the entire treatment process. As
standardized method, the model allows the evaluation and analysis of clinical
workflow metrics and thus forms the basis for continuous quality improvement.
For modeling purposes, we use Event-driven Process Chains (EPC), a common
process modeling notation, and the ARIS Toolset. Our process approach allows
the analysis and evaluation of specific clinical workflows and furthermore
forms the basis for continuous performance measurement, clinical quality
improvement and a sustainable risk reduction in health care.
1 Introduction
Clinical workflow analysis is an important element of clinical quality improvement
efforts. Optimization of clinical pathways and the management of time-critical
diseases such as heart attack and stroke – although highly standardized – can be more
or less time-consuming depending on the workflow bottlenecks in a particular health
care organization. To identify bottlenecks in a workflow that overall can be
accomplished within one or two hours, requires a thorough understanding of both
workflow and durations each of the sub-processes take. As process data are generated
by several hospital information systems, its extraction is problematically. Therefore
this investigation presents an event-based approach to standardized and automated
extraction of required process parameters. The aim is to determine process cycle times
as well as to optimize clinical pathways.
Clinical process quality means the way in which care is delivered and specific
clinical requirements are fulfilled. Standardized process models can support process
monitoring and quality controlling in healthcare delivery. Improving the effectiveness
and efficiency as well as optimization of clinical pathways regarding quality, time and
costs is one of the key management strategies of time-critical diseases such as heart
attack and stroke. To identify workflow bottlenecks in such acute processes requires a
Gattnar E., Ekinci O. and Detschew V..
Event-based Workflow Analysis in Healthcare.
DOI: 10.5220/0003587800610070
In Proceedings of the International Joint Workshop on Information Value Management, Future Trends of Model-Driven Development, Recent Trends in
SOA Based Information Systems and Modelling and Simulation, Verification and Validation (MSVVEIS-2011), pages 61-70
ISBN: 978-989-8425-60-7
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

thorough understanding about both the hospital information systems and the clinical
workflows.
We propose therefore a newly developed clinical process model for workflow
analysis, performance measurement and quality improvement in hospitals. For
modeling purposes, the Event-driven Process Chain (EPC), a process modeling
notation, and the ARIS Toolset, are used. In our approach process quality metrics,
based on established clinical guidelines, are considered as performance measures.
Furthermore, interoperability issues (i.e. the ability of an information system to
participate in a complex information management process in a concerted fashion with
a number of other information systems [1]), are also addressed. In order to analyze
process performance, our approach focuses the entire treatment process. As
standardized model, it allows the analysis and evaluation of specific clinical
workflows and furthermore forms the basis for continuous performance measurement,
clinical quality improvement as well as risk reduction. In health care delivery this
typically directly translates into an improved service and quality outcome for patients
as well as a reduction of treatment costs.
2 Event-driven Process Chains
Prerequisite for performance measurement is the knowledge of the processes. These
characteristic clinical processes are to be identified and brought together in a process
model including relationships and structures like sequence, parallelism, alternative
and loop. For modeling purposes, Event-driven Process Chain (EPC) is used as
process modeling language. The EPC is a methodology for a semi-formal description
of business processes and is central to a variety of reference models. The language has
been developed by SAP AG and IDS Scheer AG in a collaborative research project in
the early nineties [2]. IDS Scheer AG, a software and consulting company, has
furthermore developed the ARIS Toolset, a worldwide leading business process
modeling tool, which is very often used for reference modeling by means of EPC [3].
The method is characterized by clarity and an integrated tool support in practice. It is
one of the most commonly used methods in business modeling [4] as well as also
applicable as process modeling method in hospital domain [5]. An EPC represents the
temporal and logical dependencies of events and processes, and also allows the
explicit notation of events, where process performance measurements can be done.
For these reasons, the EPC is a suitable method for clinical process measurement
efforts. Furthermore, the clinical task-oriented EPC-notation enables non-technical
professionals like physicians or other clinical staff to understand the modeled clinical
process quickly and easily. On top of that, the ARIS toolbox support is an important
argument.
EPCs are used mostly at the lower levels of process hierarchy. This level of detail
is also necessary for performance measurement. On conceptual or technical level
other methods such as Business Process Modeling Notation (BPMN) [6], Unified
Modeling Language (UML) [7] or Business Process Execution Language (BPEL) [8]
are often used. EPC models consist of functions, events, process interfaces (paths),
control flows (connections resp. arrows), connectors and further informational and
organizational elements. Functions are active elements and represent the tasks or
62
activities in a process [3]. As passive elements, events describe process states and
have in contrast to functions no duration. Events trigger functions and are themselves
results of functions. Functions and events have to be connected and to alternate with
each other. Each EPC starts with at least one event and ends with at least one event. In
order to model sequences, branches and processing loops, logical connectors (AND,
OR, XOR) are used. They model thus joins and splits [3]. Process paths indicate
connections to other processes or sub-processes and partition processes at the same
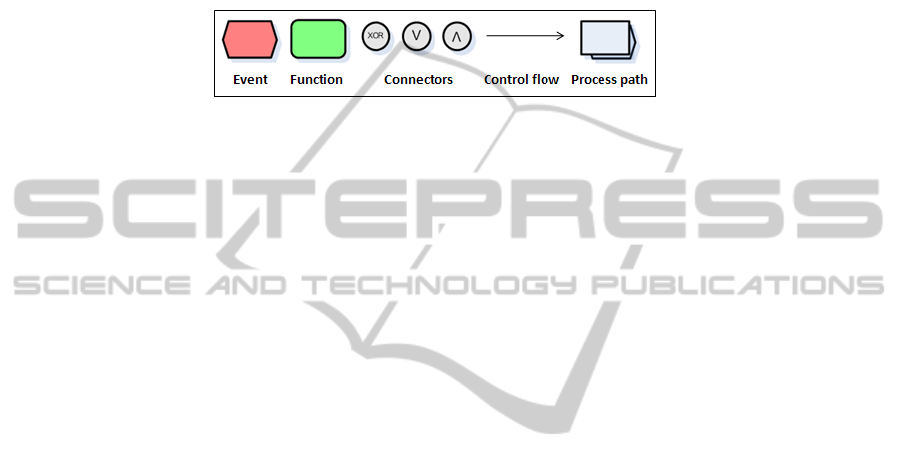
hierarchical level [9], [10]. Fig. 1 shows the EPC-elements used in this paper.
Fig. 1. Event-driven Process Chain (EPC)-Elements.
3 Clinical Quality Control and Assurance
3.1 Clinical Quality Dimensions and Medical Care Level
According to JCAHO (Joint Commission on Accreditation of Healthcare
Organizations), quality of care is the degree to which patient care services increase
the probability of desired outcomes and are consistent with current professional
knowledge. Quality can be furthermore classified according to A. Donabedian into
three quality dimensions: structural, process and outcomes quality [11]. This
internationally accepted classification is based on the assumption that all quality
dimensions are based on one another. Only the analysis of all three dimensions
simultaneously represents a holistic and integrated assessment of quality of care.
Structural quality thereby relates to the environment within care is delivered. These
includes the characteristics of a hospital, including both diagnostic and therapeutic
approaches, the technical equipment (rooms, medical devices, IT-systems and
infrastructure etc.), location, financial resources, the number and qualifications of
employees and the organization as well as the personnel structure. The way in which
care is delivered is related to process quality. This includes all operations relating to
the clinical workflow, therapeutic and nursing measures, and cooperation of the staff.
Clinical care often varies depending on the condition of the patient and disease
progression. In consequence, the quality of process has to be assessed individually. As
the evaluation of process quality is important for homogeneous groups of patients,
standardized clinical pathways and process models are often defined, to support
quality management efforts. The achievements of delivered care are finally focused
by outcomes quality. From a medical point of view the results of all diagnostic and
therapeutic efforts in treating a patient are referred. This includes measurable figures
such as procedural success, mortality and complications of treatment, and parameters
such as the rate of hospital infections, reinterventions etc. Fig. 2 schematically shows
the quality dimensions embedded in the health care process.
63
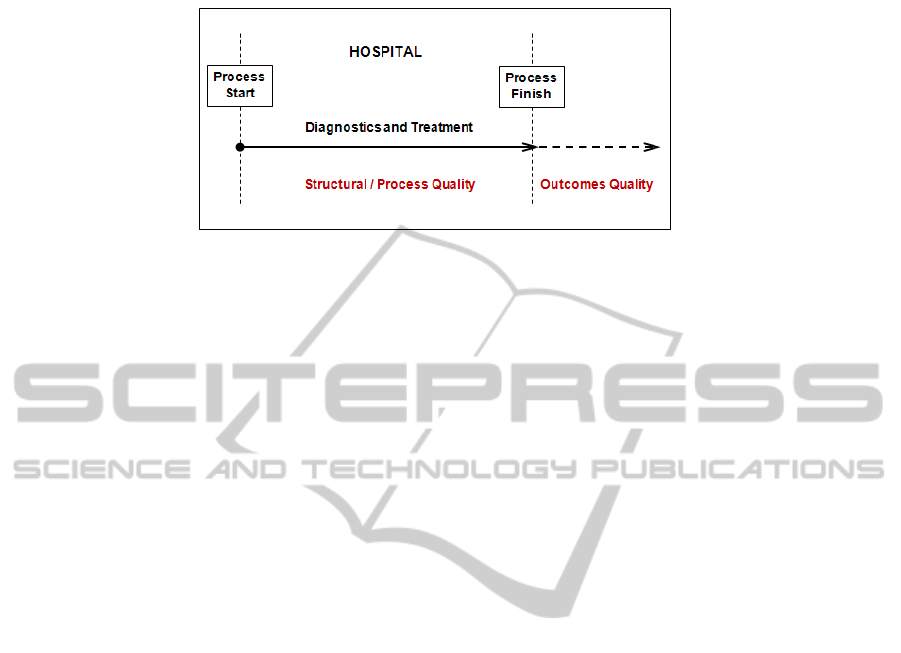
Fig. 2. Quality dimensions and the health care process.
Although the structural quality can be easily measured and outcomes quality is most
significant, process measures are more sensitive to differences in quality of care.
Furthermore they are especially in contrast to outcomes measures easier to interpret
[12]. Process measures such as “door to balloon time” (time from patient arrival at the
hospital [door] to the primary coronary intervention [balloon] in patients admitted
with heart attack) or “order to imaging time” (time from order entry [order] to
completion of diagnostic imaging [imaging]) are direct measures of quality. Whereas
an outcomes quality indicator like “outpatient mortality rate in heart attack patients”
is only an indirect measure. The measurement of outcomes quality is complicated and
depends on the behavior and willingness of patients. In addition, the evaluation time
of results is relevant, because patient’s relation to the treatment process will diminish
over time. As a result, identical hospital services differ in terms of outcomes quality
by the degree of patient involvement and the time of measurement. A lower level of
medical care leads thereby automatically to an increase of iatrogenic risks and to a
simultaneous increase of process costs due to accumulating errors. A maximal
medical care level assures a maximal risk reduction and the highest quality regarding
all quality dimensions: structure, processes and outcomes [13]. Due to the reasons
referred to before, the process quality is focused on in the following.
3.2 Clinical Process Quality
All activities performed within a hospital are processes. These processes are to
identify, analyze, evaluate and control. Health care processes are impacted by quality,
cost and time aspects. Whether the process meets the defined quality requirements, is
dependent on how many faults and risks are accepted during the treatment. In addition
to process quality, also process costs are critical in assessing the process performance.
Thereby the usage of all resources, which are required to provide the process
performance, is considered. Finally, the process cycle time has to be mentioned as an
important factor in determining the process performance. It is composed of processing
times, waiting times and transfer times.
A practical example is the management of time-critical diseases such as heart
attack. The application of new treatment approaches can save time and costs while
increasing quality of care and therewith improving the care process. By using new
imaging modalities such as CT (computed tomography) or novel laboratory markers,
64

in patients with lack of clear signs of a heart attack, it is possible to exclude a vascular
occlusion quickly (time) and safety (quality). Such patients can be discharged within
6-8 hours from the emergency room with a reliable diagnosis (costs) [13].
4 Clinical Standards and Workflow Modeling
4.1 Clinical Pathways and Guidelines
A clinical pathway is an evidence-based treatment process for continuous quality
improvement in patient care [14]. In addition, a clinical pathway serves as the basis
for quality improvement and can be used as an instrument for data collection and
process monitoring [15], [14]. Clinical pathways are important in the context of
quality management and thus help towards the continuous quality improvement in
hospitals. In this case all three in the previous chapter described quality dimensions
are equally used. In addition to the outcomes quality, the process quality is most
important.
Clinical pathways are not interchangeable between different hospitals because they
have to be adapted to local organizational conditions. This includes both
environmental and personnel resources as well as the procedures concerned.
Consequently, each standardized treatment pathway requires an individual adjustment
to the hospital in question. Thus the construction of clinical pathways is time-
consuming. Reference process models that support as patterns the pathways
construction and/or standardized solutions that generate clinical pathways
automatically are desirable [13].
Clinical pathways can be derived using clinical guidelines. Guidelines are
systematically developed recommendations, which support physicians and health care
organizations in the treatment of patients. As recommendations for clinical
diagnostics and treatment of certain diseases they are important for quality of care
management in hospitals. However, they are not binding. For example, guidelines for
diagnostics and treatment of heart attack patients are published by independent
societies such as the German Society of Cardiology [16]. They are based in most
cases on results deduced from recent clinical studies.
4.2 Clinical Workflow Modeling
Clinical workflows are characterized as people-intensive and patient-centered
processes where physicians and clinical staff work closely together using materials,
devices and methods to attend and treat the patient. During a hospital stay, a patient
crosses several departments, which are based on various fields of responsibility and
information system-catchment areas. This set of departmental and system boundaries
represent process interfaces that had to be bridged and taken into account during
modeling. Therefore constructs like sequence, parallelism, optional flows and loops
(without recursion) were modeled using functions, events and connectors and used in
the whole process model as reference patterns. Because the clinical process flow, e.g.
in the field of acute diseases, can vary very often, the underlying process model had to
65
be flexible designed. Therefore the entire process model was divided into 21 modules
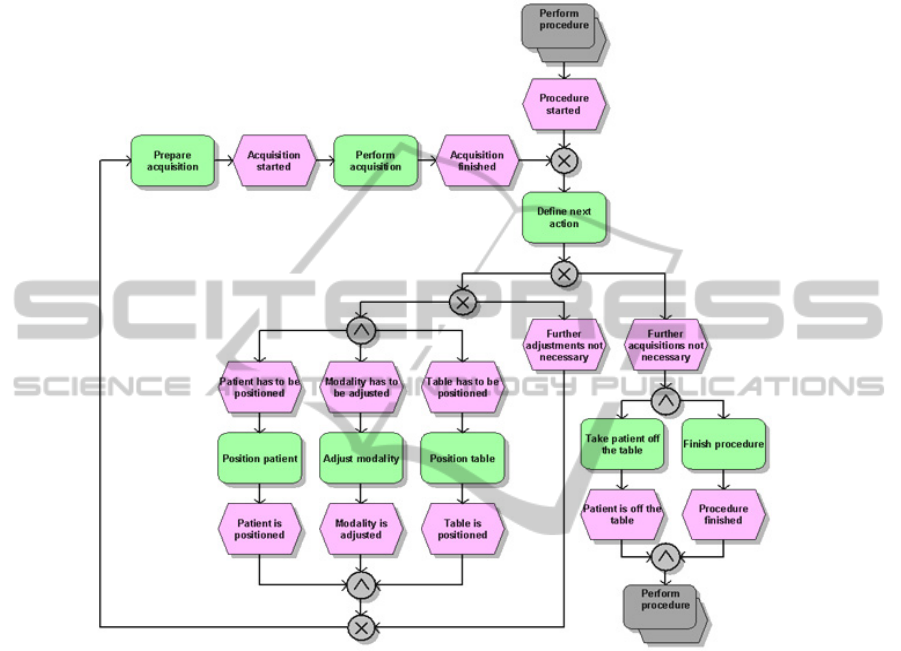
that were arranged hierarchically. Fig. 3 illustrates the EPC-module which models the
workflow at an imaging modality (i.e. device used to acquire images of the body).
Fig. 3. An example of an EPC-module: Sub-process (i.e. imaging procedure) performed at an
imaging modality (e.g. during computed tomography).
The connection between the modules is managed by using the EPC process path
element. The described modularization of the whole end-to-end-process into sub-
processes leads in a higher flexibility of the model. The modules represent therefore
different aspects (e.g. planning of a procedure, performing a procedure or archiving
procedure results) of the whole clinical process and are connected to each other using
process paths. In opposite to the common understanding of the process path element,
it is used in our approach, to establish a hierarchical clustering in the model.
Modeling in this way is efficient, because all modules can be called separately and
run repeatedly without the necessity of embedding redundancies in the model.
Beyond that, the model is easily maintainable and extensible for future purposes (e.g.
model extension to non-hospital processes).
Our reference model was designed primarily to analyze the clinical workflow by
means of process metrics. Secondly it accelerates the modeling of disease-specific
66
and hospital-specific clinical pathways and the measurement of KPIs in hospitals. The
modeling “lifecycle” is initiated by the derivation of a disease-specific model (e.g.
heart attack) from the generic model. Thereby, not required functions and events are
to be removed (e.g. the surgery-sub-process in a typical stroke pathway). Disease-
specific models are also reference models with generic functions and events. To
reduce the complexity of the derivation, a module-oriented approach has to be used.
Because of the flexibility of the model, each of the modules can be separately derived.
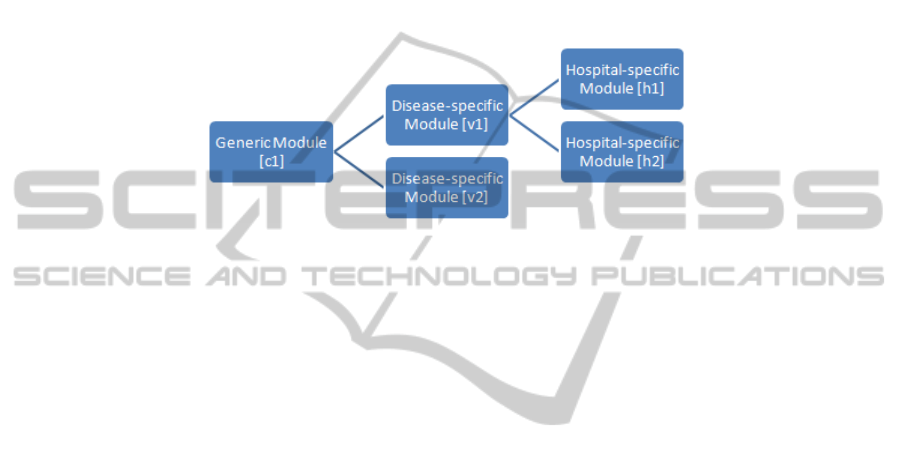
As in Fig. 4 schematically shown, the disease-specific module [v1] can be separately
derived from the generic module [c1]. A derivation of a hospital-specific module [h1]
can be performed in the same manner.
Fig. 4. Taxonomy of disease-specific and hospital-specific module derivation.
The next step is to customize the disease-specific modules in order to transform
them into hospital-specific sub-processes. Therefore all generic functions and events
have to be first redefined. Additionally, their generic naming has to be transformed
into a specific term (e.g. “Procedure” into “ECG”). Furthermore dedicated elements
can be removed (e.g. “Performing CT”, if the hospital doesn’t support computed
tomography examinations) and/or new specific elements can be inserted (e.g. specific
organizational steps).
The generic reference process model represents the top of the whole clinical
process in our approach including all necessary elements and alternatives. The model
denotes the generic set of all possible sub-processes that may be applicable in a
particular hospital. Depending on the disease in question several generic models can
be derived (e.g. for heart attack and/or for stroke). Each of the disease-specific models
can be further transformed into a hospital-specific variant, called in the following
clinical pathway. It represents in our approach the basis for performance measurement
and optimization efforts and demonstrates the status quo regarding the process
performance and quality. Thereby the performance of the clinical inpatient process is
focused on involving clinical roles like clinicians, nurses and technicians performing
the dedicated clinical tasks. However, to preserve the generic model character, there
are not specific roles assigned at the level of the generic and disease-specific level.
5 Workflow Analysis and Performance Measurement
Health care organizations such as hospitals are interested in measures about their
quality of care. A common way to retrieve quality information is to examine the
performance of organizational structure (structural performance) and processes
(process performance) as well as outcomes (outcomes performance) by means of Key
67

Performance Indicators (KPIs) [18]. The challenge is to develop measurable,
significant, appropriate and quality relevant indicators. Such sets of indicators are
being provided by health care organizations in many countries (e.g. Joint Commission
on Accreditation of Healthcare Organizations [19], Agency for Healthcare Research
and Quality [20], National Health Service [21] etc.). In the following, process
indicators are focused on.
In order that indicators can be used in quality management in hospitals, required
data have to be collected. Process indicators can be classified according to quality,
time and cost aspects - as mentioned before - in quality-based, time-based or cost-
related process metrics. Since time plays an important role in acute diseases, time-
based process indicators have been selected for further investigation. In the following
time-based process indicators are called KPIs.
In our approach KPIs are considered as workflow metrics on the basis of existing
clinical standards in the hospital system environment. IT-systems act in this case as
enabler for clinical quality improvement as well as risk and cost reduction. The
missing link between IT and KPIs is drawn by mapping selected KPIs to our newly
developed clinical process model. The information about the predicated IT-system is
stored in our approach in so-called KPI-cards. These are structured and short
descriptions of each KPI considered in our model including further information about
the start- and end-events, the IT-systems activating the events, the calculation of the
KPI from start- and end-events or in combination with other KPIs, practical examples
as well as related KPIs. In addition, the related EPC-modules are referred to.
EPC-events provide a possibility for time measures. Because of the fact, that
events don’t have a time duration (in opposite to functions) they can be registered
with a timestamp. Therefore special events were added to the model (e.g. “Procedure
started” and “Procedure finished” or “Acquisition started” and “Acquisition finished”)
(see Fig. 3). They indicate the start and the finish of the workflow resp. the process
within. Between two of such events the process cycle time can be calculated and
therefore bottlenecks can be detected and analyzed. As an example, the calculated
time difference between “Procedure started” and “Procedure finished” in Fig. 3
provides the duration of the whole imaging procedure including device adjustment
times and possibly more than one image acquisition. The appropriate events are
generated in the radiology information system (RIS). In contrast, the time duration
between “Acquisition started” and “Acquisition finished” provides the precise timing
information about one image acquisition. This allows e.g. detailed workflow and
modality utilization monitoring. As images are generated at the modality (e.g. during
CT), the appropriate events have to be extracted from the modality logfiles. In
general, all events which have to be retrieved in order to measure KPIs are assigned to
a specific information system. In cases of unavailability, we recommend providing a
possibility of automated generation of appropriate IT-timestamps.
6 Conclusions and Outlook
Our paper presents a promising approach for measuring KPIs in health care
environment based on a newly developed EPC-model. However, there exist other
approaches to clinical workflow improvement as presented in this paper too. For
68

example, the Lean Thinking’s Value Stream Modeling, as a patient journey modeling
technique, supports the reengineering of healthcare processes by using the lean
paradigm derived from the field of manufacturing [22]. In future work, such further
approaches and approaches regarding process and workflow mining techniques
[23,24,25] will be considered and compared to the approach introduced in this paper.
Additionally, specialization features that support the automated derivation of the
model to a hospital-specific solution are also future and complementary work.
We evaluated and verified our model and the methodology behind with several
clinicians and medical specialists. Additionally we verified the model using clinical
pathways of several hospitals including amongst others acute pathways for heart
attack and stroke. Furthermore we evaluated the model's fitness for specialization and
time-measurement in cooperation with a large German university hospital.
As standardized method, our model allows the evaluation and analysis of clinical
workflow metrics and thus forms the basis for continuous quality improvement. Since
standardization is an essential element in risk reduction, such an approach can be a
key component of a sustainable risk management system. Therefore the model should
be linked to the IT-infrastructure of a dedicated hospital involving all stakeholders in
the treatment process. The presented approach supports a process-based
benchmarking and thus enables a more transparent standardized internal (over several
departmental and system borders) and external benchmarking (e.g. in form of public
performance measures or quality reports).
References
1. Channin, D. S.: Standards and Interoperability. In: Branstetter, B.F., (eds.) Practical
Imaging Informatics: Foundations and Applications for PACS Professionals, Springer, New
York (2009)
2. Keller, G., Nüttgens, G., Scheer, A.-W.: Semantische Prozeßmodellierung auf der
Grundlage Ereignisgesteuerter Prozeßketten (EPK), Veröffentlichungen des Instituts für
Wirtschaftsinformatik (IWi), Universität des Saarlandes, Heft 89, Saarbrücken (1992)
3. Fettke, P., Loos, P.: Perspectives on Reference Modeling. In: Reference Modeling for
Business Systems Analysis, Fettke, P., Loos, P. (eds.), Idea Group Publishing Inc, London
(2007)
4. Status Quo Prozessmanagement 2010/2011, BPM expo, http://www.bpm-expo.com
5. Sarshar, K., Dominitzki, P., Loos, P.: Einsatz von Ereignisgesteuerten Prozessketten zur
Modellierung von Prozessen in der Krankenhausdomäne – Eine empirische
Methodenevaluation. In: EPK 2005: Geschäftsprozessmanagement mit Ereignisgesteuerten
Prozessketten, pp. 97-116, Proc., 4. Workshop der Gesellschaft für Informatik e.V. (GI),
Hamburg (2005)
6. Object Management Group, Inc., Business Process Model and Notation,
http://www.bpmn.org
7. Object Management Group, Inc., Unified Modeling Language, http://www.uml.org
8. Organization for the Advancement of Structured Information Standards, http://www.oasis-
open.org/home/index.php
9. Davis, R.: Business Process Modelling with ARIS: A practical guide, Springer, London
(2001)
10. vom Brocke, J.: Referenzmodellierung: Gestaltung und Verteilung von Konstruktions-
prozessen, Logos Verlag, Berlin (2003)
69

11. Donabedian, A.: Evaluating the quality of medical care, The Milbank Quarterly, 44, 3, pp.
166-203 (1966)
12. Mant, J.: Process versus outcome indicators in the assessment of quality of health care,
International Journal for Quality in Health Care, 13, 6, pp. 475-480 (2001)
13.Gattnar, E., Ekinci, O.: Qualitätsmanagement im Krankenhaus – Konzepte, Rahmen-
bedingungen und Standards. In: Podium der Wirtschaft, Recht & Soziales, Band 21, VHK,
Altdorf b. Nbg. (2011)
14. Kahla-Witzsch, H.A.: Interprofessionelles Qualitätsmanagement als unverzichtbare
Grundlage für eine erfolgreiche Pfadarbeit – Anregungen aus dem Universitätsklinikum
Frankfurt/Main. In: Praxis Klinischer Pfade: Viele Wege führen zum Ziel, Hellmann, W.
(eds.), Ecomed, Landsberg/Lech (2003)
15. Kahla-Witzsch, H.A., Geisinger, T.: Clinical Pathways in der Krankenhauspraxis,
Kohlhammer, Stuttgart (2004)
16.Deutsche Gesellschaft für Kardiologie, http://www.dgk.org
17.Küttner, T., Roeder, N.: Definition klinischer Behandlungspfade. In: Küttner, T., Roeder, N.
(eds.), Klinische Behandlungspfade – Mit Standards erfolgreicher arbeiten, Deutscher
Ärzte-Verlag, Köln (2007)
18. NHOP, Quality and Outcome Indicators for Acute Health Care Services, National Hospital
Outcomes Program, Australian Government Publishing Service, Canberra (1997)
19. Joint Commission on Accreditation of Healthcare Organizations, http://
www.jointcommission.org
20. Agency for Healthcare Research and Quality, http://www.ahrq.gov
21. National Health Service, http://www.nhs.uk
22. Curry, J. et al,: A Communication Tool to Improve the Patient Journey Modeling Process.
Proceedings of the International Conference of IEEE Engineering in Medicine and Biology
Society. pp. 4726-4730 (2006)
23. Aalst, W.M.P., Business Alignment: Using Process Mining as a Tool for Delta Analysis. In:
Requirements Engineering, Volume 10, No. 3, pp 198-211 (2005)
24. Aalst, W.M.P. et al., Workflow mining: A survey of issues and approaches. In: Data &
Knowledge Engineering, Volume 47, No. 2, pp 237-267 (2003)
25. Wen, L. et al: A Novel Approach of Process Mining with Event Graph. In: Knowledge-
Based and Intelligent Information and Engineering Systems, Volume 6276, pp 131-140
(2010)
70
