
BREATH AND POSITION MONITORING
DURING SLEEPING WITH A DEPTH CAMERA
Meng-Chieh Yu
1
, Huan Wu
2
, Jia-Ling Liou
2
, Ming-Sui Lee
1,2
and Yi-Ping Hung
1,2
1
Graduate Institute of Networking and Multimedia, National Taiwan University, Roosevelt Road, Taipei, Taiwan
2
Department of Computer Science and Information Engineering, National Taiwan University,
Roosevelt Road, Taipei, Taiwan
Keywords: Non-contact breath measurement, Sleep monitoring, Sleep position, Sleep cycle, Depth camera.
Abstract: Sleep monitoring is increasingly seen as a common and important issue. In this paper, a depth analysis
technique was developed to monitor user’s sleep conditions without any physical contact. In this research, a
cross-section method was proposed to detect user’s head and torso from the depth images. Then, the system
can monitor user’s breathing rate, sleep position, and sleep cycle. In order to evaluate the measurement
accuracy of this system, two experiments were conducted. In the first experiment, eight participants with
various body shapes were asked to join the experiment. They were asked to change the sleep positions
(supine and side-lying) every fifteen breathing cycles in two circumstances (sleep with and without a thin
quilt) on the bed. The experimental results showed that the system is promising to detect the head and torso
with various sleeping postures. In the second experiment, a realistic over-night sleep monitoring experiment
was conducted. The experimental results demonstrated that this system is promising to monitor the sleep
conditions in realistic sleep conditions. To conclude, this study is important for providing a non-contact
technology to detect multiple sleep conditions and assist users in better understanding of their sleep quality.
1 INTRODUCTION
Sleep is essential for a person’s mental and physical
health. Studies indicate that sleep plays a critical role
in immune function (Born et al., 1997), metabolism
and endocrine function (Spiegel et al., 1999),
memory, learning (Maquet, 2001), and other vital
functions. However, there are some sleep disorders,
such as sleep apnea, insomnia, hypersomnia,
circadian rhythm disorders, which might interfere
with physical, mental and emotional functioning.
For better understanding of sleep problems, many
sleep centres and research groups are devoted to the
sleep study. Polysomnography (PSG) is a multi-
parametric test used in the study of sleep and as a
diagnostic tool in sleep medicine. It monitors body
functions including brain activity (EEG), eye
movement, muscle activity, heart rhythm, and
breathing while sleeping (Douglas, et al., 1992). In
this study, we focus on the research issues in sleep
cycle, sleep breathing, and sleep positions. For the
measurement of sleep cycle, EEG monitoring is one
of the most accurate methods to detect the period of
non-rapid eye movement (NREM) and rapid eye
movement (REM). However, it is not convenient to
use. In recent years, motion sensor and pressure
sensor array are widely used to monitor user’s sleep
conditions and body movement while sleeping
(Actiwatch, 1998; Fitbit, 2010; WakeMate, 2010), as
well as estimate the sleep cycle and evaluate the
sleep quality. For breath measurement while
sleeping, sleep apnea is one of the most important
sleep disorder characterized by abnormal pauses in
breathing or instances of abnormally low breathing
during sleep. For decades, the breath measurement
methods would direct contact to the user while
monitoring, and it might interfere with the user and
reduce the sleep quality. Although some non-contact
breath measurement methods were proposed in
recent years, such as ultra-wideband (UWB) and
structured light plethysmography (SLP), there still
have some measurement limitations. For sleep
position, in order to prevent sleep apnea, studies
showed that side-lying position is the best sleep
posture for individuals with sleep apnea (Cartwright
et al., 1984; Szollosi et al., 2002; Loord et al., 2007;
12
Yu M., Wu H., Liou J., Lee M. and Hung Y..
BREATH AND POSITION MONITORING DURING SLEEPING WITH A DEPTH CAMERA.
DOI: 10.5220/0003702000120022
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2012), pages 12-22
ISBN: 978-989-8425-88-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

Hoque et al., 2010). A study analysed six common
sleep positions, and concluded that supine positions
were more likely to lead to snoring and a bad night's
sleep (Idzikowski et al., 2003). However, to date,
there has been relatively little research conducted on
the measurement of sleep positions.
In this study, a sleep monitoring system using a
depth camera was proposed to monitor users’
breathing rate, body movement, and sleep position in
bed. Moreover, we evaluated the measurement
accuracy of the system, including the accuracy of
head and torso detection, breath measurement
(compared to RIP), and sleep movement (compared
to Actigraphy). Through the experimental results,
we confirmed that the system could accurately
monitor user’s sleep conditions. This paper is
structured as follows: The first section deals with the
introduction of present sleep studies. The second
section of the article is a review of several breath
measurement methods and activity monitoring while
sleeping. The proposed system design is described in
the third section. The experimental results are
demonstrated in section four followed by the
discussion on some important findings. Finally,
conclusions and suggestions are given for further
research.
2 RELATED WORKS
In this section, we discuss relevant literatures of
breath measurement and sleep cycle monitoring
while sleeping.
2.1 Breath Measurement
while Sleeping
Breathing is important while sleeping. There are
many breathing-related sleep disorders, such as
apnea and hyperventilation syndrome (HVS).
Currently, many methods are proposed to monitor
the breath conditions while sleeping. Most screening
tools consist of an airflow measuring device, a blood
oxygen monitoring device, and the respiratory
inductance plethysmography (RIP). Thermistor (TH)
measurements have been traditionally used to
determine airflow during PSG studies. It is placed
over the nose and mouth and infers airflow by
sensing differences in the temperature of the warmer
expired air and the cooler inhaled ambient air.
However, low accuracy in detecting hypopneas is a
major drawback (BaHamman, 2004). The pulse
oximeter is a medical device that monitors the
oxygen saturation of user’s blood, and changes in
blood volume in the skin. Low oxygen levels in the
blood often occur with sleep apnea and other
respiratory problems (Douglas, et al., 1992).
Respiratory Inductance Plethysmography (RIP)
measures the body movement of chest wall or
abdominal wall caused by breathing exercise (Whyte
et al., 1991; Cantineau et al., 1992), and then the
breathing conditions can be estimated accurately.
However, most of the breath measurement methods
are essential to directly contact to the user while
measuring, and it might affect the user and decrease
the sleep quality.
In recent years, some non-contact breath
measurement methods are developed. A study used
a CCD video camera to detect the optical flow of the
user in bed (Nakajima et al., 2001). PneumaCare
developed a non-invasive method called Structured
Light Plethysmography (SLP), which utilizes the
distortion with movement of a structured pattern of
light to calculate a volume or change in volume of a
textured surface. Another study conducted an
experiment and the results showed that SLP was
comparable in performance to spirometer (Wareham
et al., 2009). Moreover, slit lights projection (Aoki
et al., 2006) is another non-invasive method which
measures the breathing conditions by projecting the
near-infrared multiple slit-light patterns on the user
and measuring the breathing status.
In addition to computer vision-based methods,
there is a non-contact method which uses ultra
wideband (UWB) to measure the breathing status. A
study proposed an application of UWB radar-based
heart and breathing activities for intensive care units
and conventional hospital beds (Staderini, 2002).
Another study used UWB to measure baby’s
breathing and heart rate especially in terms of
opportune apnea detection and sudden infant death
syndrome prevention (Ziganshin et al., 2010).
2.2 Sleep Cycle
For monitoring the sleep activity through movement,
actigraphy has been used to study the sleep patterns
for over 20 years. Actigraphy is a non-invasive
method of monitoring human activity cycles (Sadeh,
et al., 1994). It is useful for determining sleep
patterns and circadian rhythms. The advantage of
actigraphy over traditional PSG is that actigraphy
can conveniently record the sleep activity (Ancoli-
Israel et al., 2003). In recent years, many
commercial products were developed, such as Fitbit,
WakeMate, and Actiwatch. In general, these
products detect the information of time to fall asleep,
time to wake up, and totally sleeping time. A study
BREATH AND POSITION MONITORING DURING SLEEPING WITH A DEPTH CAMERA
13
evaluated the measurement results of actigraphy and
compared to PSG, and the experimental results
showed that sleep parameters from actigraphy
corresponded reasonably well to PSG (Kushida et al.,
2001). In addition, there is a non-contact method
which uses a microphone and an infrared sensor to
monitor the sleep status. Moreover, some studies
utilize motion sensors (accelerometer, piezoelectric
sensor) inside the pillow (Harada et al., 2000) or bed
(Malakuti et al., 2010; Hoque et al., 2010) to
monitor the sleep movement and sleep positions.
However, none of related research in our survey
has a complete study to provide a non-contact and
multi-functioning sleep monitoring technique to
monitor the sleep conditions. In this study, we
developed a non-contact sleep monitoring system
which can monitor user’s sleep position, breathing
condition, and body movement in the same time.
3 SYSTEM DESIGN
In this study, a cross-section object detection method
is proposed to detect user’s head and torso using a
depth camera. The sleep position, body movement,
and breathing condition are monitored once the head
and torso is detected. The procedure of this method
is as follows: First, the view transformation is
estimated. Then, a median filter is adopted to reduce
the image noise after view transformation. Next, a
cross-section method is used to detect user’s head
and torso so that the sleep position and body
movement can be measured. Besides, a breath
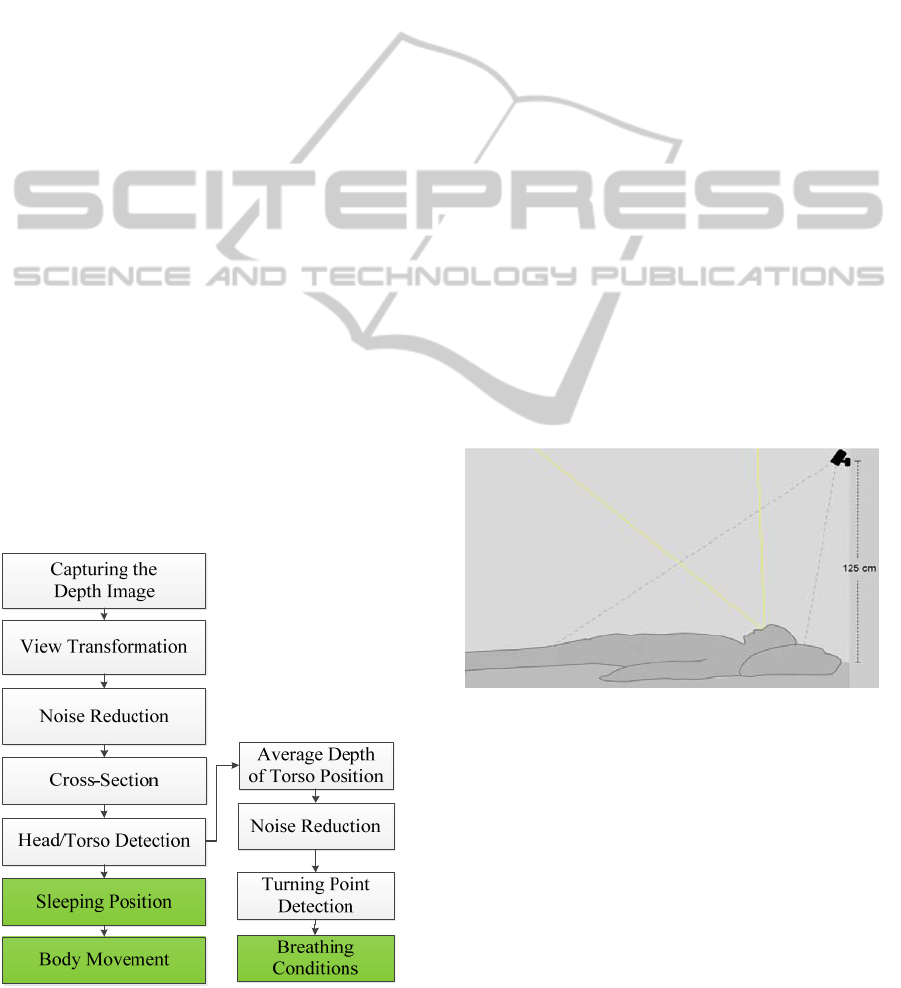
Figure 1: System Framework.
measurement method is proposed to detect the
breathing conditions through the movement of the
torso. The system framework of this system is
shown in Figure 1.
3.1 System Environment
In this system, a depth camera (Microsoft, 2011) is
used to capture the sequence of depth images of the
user on the bed. The depth camera consists of an
infrared laser projector combined with a CMOS
sensor, which captures color images and a depth
images under ambient light condition. In addition,
the depth image can also be captured under the no-
light condition. For the reason of easy setup and
preventing the interference with the sight view of the
user while sleeping, in this study, the depth camera
is placed on the wall behind the head instead of
suspending from the ceiling. Besides, in order to
ensure that the user’s head and torso can be captured,
and for the issues of breath measurement distance
(the shorter the better), the limitation of sensing
distance (larger than 0.8m), the depth camera is
placed in the distance of 125 cm (49.2 inches) from
the bed. The diagram for the system is shown in
Figure 2. The region between gray dotted lines
indicates the sight view of the depth camera, and the
region between yellow lines indicates the sight view
of the user.
Figure 2: System Diagram.
3.2 Depth Image Processing
Although the skeleton of the user body can be
extracted easily through Microsoft Kinect SDK, the
skeleton of body while lying on the bed cannot be
extracted easily. It is because that the background is
too close to the user, and the body might be covered
by a quilt. In this study, a cross-section method is
proposed to detect user’s head and torso with a depth
camera. We process the depth image signals at the
resolution of 320 pixels in width and 240 pixels in
height, and the frame rate is 30 frames per second.
HEALTHINF 2012 - International Conference on Health Informatics
14
View Transformation
In order to determine the cross-sections of the depth
image, we would like to transform the camera view
from the side view to the top view. To do that, we
need to calculate bed’s normal vector first. In order
to rotate the camera view to the top of the bed, three
points and one rotate center point need to be
specified manually. After taking three 3D-points on
the bed and using cross product, the system could
get the normal vector of the bed. Then, these 2D-
points could project to 3D-points in the real world.
Then, we proceed to calculate rotation matrix for the
bed’s normal vector. Once we have the rotation
matrix, we can project all 2D points back to 3D
point-cloud. Again, we project it back to 2D depth
image. However, it will lose some information after
rotating the camera view, so a median filter is used
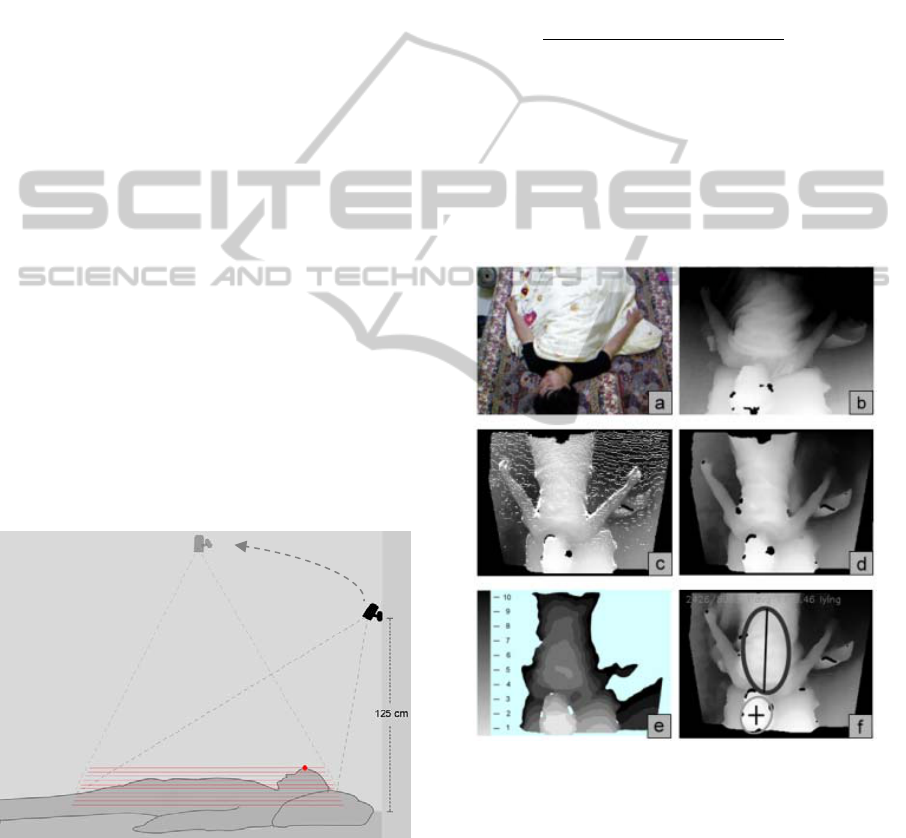
to fill empty holes. Figure 4b shows the original
depth image, and Figure 4c shows the depth image
after view transformation.
Cross-Section Method
We generate several binary images by setting
different thresholds starts from the shallowest point
of the depth image to the depth of the bed. We
generate cross-sections every 2 cm (0.787 inches)
from top to bottom. Generally, the distance between
the highest point of the human body and the bed is
around 18~28 cm, therefore, there would be 9~13
transverse sections of the person from top to bottom.
Figure 3 shows ten cross-sections (red line) from the
highest point of the red point to the bed.
Figure 3: Cross-sections of the lying user from top to
bottom. Red point indicates the highest point of the user.
Head and Torso Detection
By using connect-component analysis, the
components from each cross-section can be
extracted. The concept of this method is to find out
spheres in each cross-section. Once there is a circle
growing larger from top section to bottom section,
we assume that it might be a sphere there. So far,
this algorithm might find other spheres. To decide
the highest sphere, we collect each circle’s
contribution from each section. More circles at the
same location means higher probability to have
sphere there. If sphere candidates have n different
locations, the probability that might be a sphere at
location l is:
() =
∑
#
∑∑
#
(1)
In addition to detecting head from single depth
image, we need to leverage the advantage of video
sequence. Hence, we push every head location found
by each frame into a queue. Then, we use the same
idea to re-locate the highest probability head-like
sphere. This will avoid some occasional misleading
failed detection.
Figure 4: Depth image Processing Procedure of our system.
(a) Captured color image. (b) Captured depth image. (c)
View transformed image. (d) Filtered image. (e) Cross-
section image. (f) Final result of head/torso detection.
Once the head is detected, the next step is to
detect the torso’s ROI (region-of-interest). We adopt
almost the same way as detecting the head, but this
time we track cuboids rather than spheres. However,
there is a problem that the pillow might be
recognized as a torso. Therefore, we reject cuboids if
there is a head on it. Figure 4 shows the processing
BREATH AND POSITION MONITORING DURING SLEEPING WITH A DEPTH CAMERA
15
procedure of head and torso detection in this system.
Head and Torso Detection Algorithm
Inputs:
C := Set of circles from each sections
Cu := Set of cuboid from each sections
Th := threshold distance to determine two different cluster
Outputs:
Head and torso positions
Steps:
1.Classify_components(C,Th)
{
//Classify C into clusters according to distance Th.
1.1 clusters_num = SeqPartition(C,Th)
1.2 voting[cluster_num] //# of member in each
component
1.3 leader[cluster_num] //the biggest sphere size in
individual cluster
1.4 if( clusters_num > 0)
{
1.4.1 Loop for each C
i
element in C
1.4.1.1 num = cluster_number(i)
1.4.1.2 if(voting[num] == 0 OR leader[num]’s
size < Ci’s size )
leader[num] = C
i
End if
1.4.1.3 voting[num] = voting[num] + 1
1.4.2 End loop
1.5 }
1.6 Sort voting and leader array
1.7 Return array and # of cluster
}
2. Q
head
:= a queue that collects head’s position and
location in the video sequence.
Find_head(C)
{
2.1 Th = head_boundary.
2.2 Head = Classify_components(C,Th).
2.3 Push Head into queue Q
head
.
2.4 Final_Head = Classify_components(Q
head
,Th).
}
3. Q
torso
:= a queue that collects torso’s position and
location in the video sequence.
Find_torso(Cu,Head)
{
3.1 Th = torso_bounday
3.2 Remove cuboid from Cu if it intersects with Head.
3.3 Torso = Classify_ components(Cu,Th).
3.4 Push Torso into queue Q
torso
3.5 Remove cuboid from Q if it intersects with Head.
3.6 Final_torso = Classify_ components(Q
torso
,Th).
}
4. Detect_body()
{
4.1 Collect C and Cu from each sections
4.2 if (Head = Find_head(C))
4.2.1 Torso = Find_torso(Cu)
4.3 End if
}
Breath Measurement
The breathing signal can be extracted from the torso
ROI once we detect the head and torso. While the
user is inhaling, his chest wall will expand, and the
average depth value of the torso ROI will decrease;
on the contrary, the average depth value of the torso
ROI will increases while the user is exhaling.
Therefore, the sequential of the average depth value
of the torso ROI is considered as the breathing signal
under the premise that the user is sleeping. For
breath measurement, a turning point detection
algorithm is proposed. At first, a mean filter is used
for reducing the noises caused by the sensing
deviation and body movements. Then, the turning
points of the breathing signal are detected using the
second derivative method. Finally, in order to
eliminate redundant turning points, a dynamic
threshold is applied to find the exact peak points and
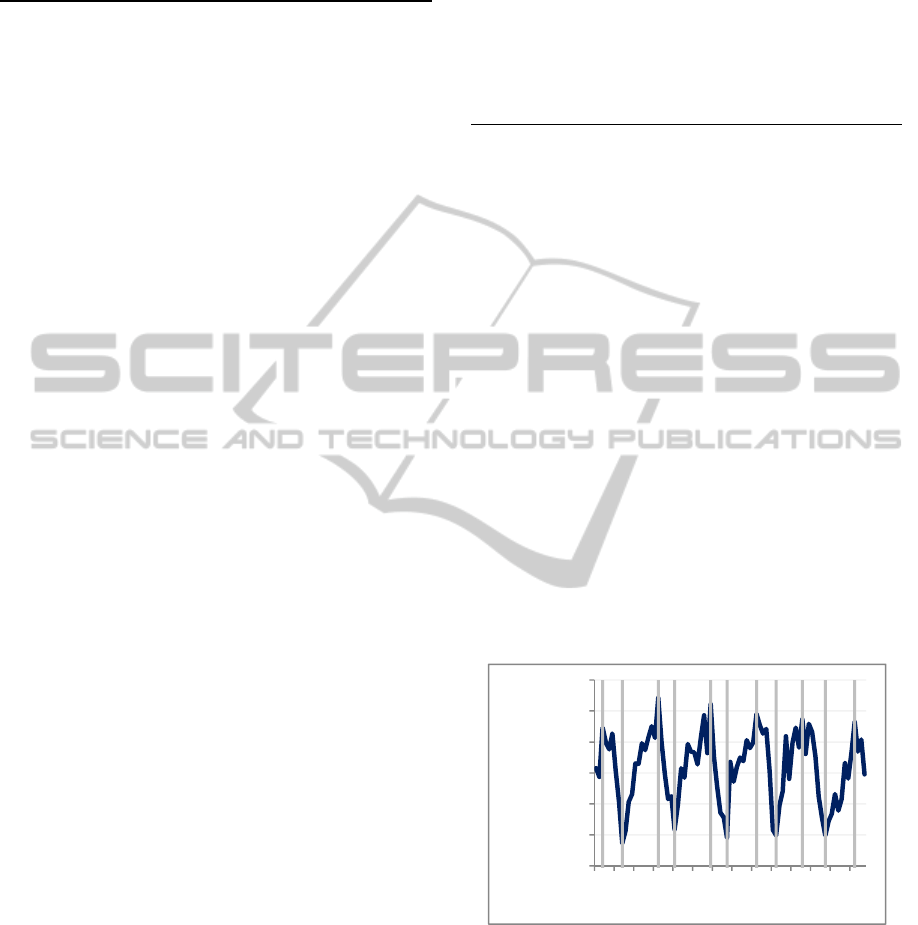
valley points. Figure 5 shows a fragment of the
breathing signal (blue line) and the measurement
results (vertical gray line) during a realistic
overnight sleep.
Figure 5: Breath Measurement. The blue line indicates the
raw breathing signals, and the gray lines indicate the
turning points which we detected.
While the turning points of the breathing signals
are detected, the information of the breathing
conditions can be figured out easily. The breathing
conditions include the breathing rate, breathing
depth, breathing stability, inhalation time, exhalation
time, inhalation/exhalation ratio, and sleep apnea
symptoms.
1193
1193,5
1194
1194,5
1195
1195,5
1196
012345678910111213
Average Distance
(cm)
Time (sec)
HEALTHINF 2012 - International Conference on Health Informatics
16
Body Movement
The body movement is defined as the sum of head
movement and torso movement. The HR
t indicates
the average depth value of the head ROI in time t,
and the TR
t indicates the average depth value of the
head ROI in time t. Then, the absolute difference
value between two adjacent images frames could be
calculated (Equation 2). M
t
indicates the movement
value of the user in time t.
M
=
|
HR
−HR
|
+
|
TR
−TR
|
(2)
Sleep Position
In this system, two main sleep positions (supine
position and side-lying position) can be recognized.
After the head and torso are detected, the highest
point of head ROI and torso ROI can be found. Then,
the ratio of the highest head point to torso point is
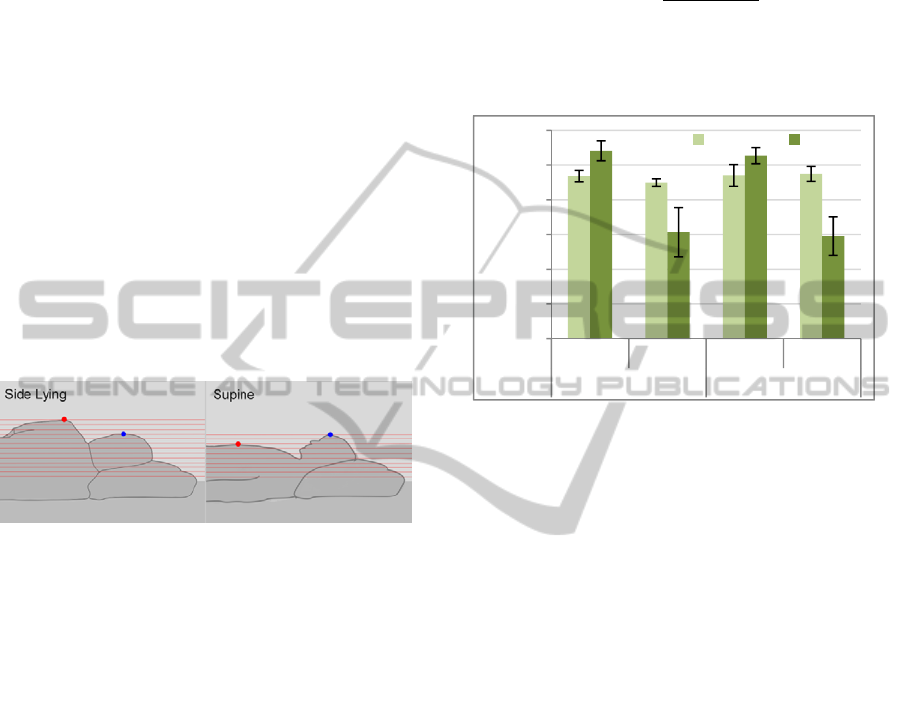
calculated. Figure 6 shows the highest point of head
ROI (blue dot) and torso ROI (red dot) in the side-
lying position and supine position.
Figure 6: Sleep Positions. Red dot indicates the highest
point of torso ROI, and blue dot indicates the highest point
of head ROI.
Next, the sleep position can be classified
according to the ratio defined in equation 3. In order
to find out the threshold to classify the sleep position,
an experiment was conducted to record five
participant’s (two females and three males) highest
points of head ROI and torso ROI in two sleep
positions (side-lying and supine) and two conditions
(sleep with no quilt and sleep with a thin quilt)
(Figure 7). The results revealed that the distance of
the highest head point does not change significantly
in different sleep positions and conditions. However,
the distance of the highest torso point changed
significantly in different sleep positions. The
average ratio is -0.02633 in supine position, and it is
0.0652 in side-lying position. Therefore, the
detection threshold of sleep position is set to the
median value: 0.01. While the ratio is larger than the
threshold value, the sleep position is defined as the
supine position. Otherwise the sleep position is
defined as the side-lying position (equation 4). From
Figure 7, we can observe that the standard deviation
of the body distance is bigger in side-lying position
than others. It is because the highest torso points are
different for female and male. However, our method
can also distinguish the sleep position accurately no
matter no matter the gender.
=
(3)
=
> 0.01
ℎ
(4)
Figure 7: The distance between the depth camera and the
highest point of head ROI and torso ROI in two positions
(supine and side-lying) and two conditions (sleep with no
quilt and sleep with a thin quilt).
3.3 Measurement Limitations
There are some measurement limitations in this
system. First, according to the law of rectilinear
propagation of light, the depth value cannot be
detected while the IR patterns are blocked by objects.
From the experiment results, we found that the most
common problem is that the hand would block some
of the depth IR patterns while side-lying. It might
affect the accuracy of torso detection. Second, the
breathing amplitude of torso movement would be
decreased with the increase of the thickness of quilt.
According to our test, the average breathing
amplitude of the torso movement with no quilt is 0.5
cm and it is 0.35 cm while sleeping with a thin quilt.
The thickness of the thin quilt in our test is 0.6 cm.
However, while sleeping with a thick quilt, such as
thick silk-padding quilts, the system might not
accurately detect the torso movement caused by
breathing exercise.
4 EXPERIMENTS
Two experiments were conducted to evaluate the
measurement accuracy of head/torso detection, sleep
1234
1224
1235
1237
1270
1153
1263
1147
1000
1050
1100
1150
1200
1250
1300
Supine Side Lying Supine Side Lying
Sleep without quilt Sleep with a thin quilt
Distance (cm)
Head Body
BREATH AND POSITION MONITORING DURING SLEEPING WITH A DEPTH CAMERA
17
position, body movement, and breath measurement
of this system. First experiment was mainly
designed to evaluate the measurement reliability for
different users. Second experiment was designed to
evaluate the measurement accuracy in realistic
overnight-sleep condition.
4.1 Experiment I
Experimental Design
Eight participants volunteered to participate in this
experiment (five males and three females). The
average age is 33.8 years old (SD = 17.6), including
two sixty-year old participants, five young
participants (25~30 years old), and a ten-year old
participant. The body mass index (BMI) of them is
in the range between 18.6~29.75. In this experiment,
participants were asked to lie down on the pillow,
and a breathing sensor, RIP (Thought Technology
Ltd., 2010), was used to record the breathing
conditions as the ground truth. During the
experimental procedure, they were asked to change
the sleep position every fifteen breathing cycles. The
procedure of this experiment is in the sequence of
supine, lying on the right side, supine, lying on the
left side, supine, and lying on the right side. Totally,
the participant needed to change the sleep position
five times. Besides, the experimental procedure
needed to be done twice, including a condition that
the participants sleep with a thin quilt, and a
condition that they sleep with no quilt. Before each
task, participants were reminded not to breathe
deliberately.
Experimental Results
The sleep measurement were divided into four
different conditions in this experiment, including
two sleep positions (side-lying and supine) and two
circumstances (sleep with a thin quilt and sleep with
no quilt). For each condition, the total numbers of
correct head detection frames were calculated
manually as well as the total numbers of correct
torso detection frames. The average of accurate rate
and standard deviation in each condition are listed
below. The experimental results showed that while
participants slept with no quilt, the measurement
accuracy of head detection was 98% (SD = 0.036)
while in the side-lying position, and it was 99.3%
(SD = 0.018) in the supine position. Moreover, the
measurement accuracy of torso detection was 91.5%
(SD = 0.16) in the side-lying position, and it was
99.3% (SD = 0.01) in the supine position. Besides,
while participants slept with a thin quilt, the
measurement accuracy of head detection is 96.7%
(SD = 0.11) in the side-lying position, and it was
99.5% (SD = 0.02) in the supine position. Moreover,
the measurement accuracy of torso detection was
94.5% (SD = 0.1) in the side-lying position, and it
was 99.5% (SD = 0.008) in the supine position.
Overall, the average accurate rate was 98.4% in head
detection and 96.4% in torso detection. The
experimental results of head and torso detection are
shown in Figure 8.
Figure 8: Measurement results of head and torso detection
in experiment I.
For breath measurement, the measurement
accuracy is defined as the ratio of the totally
breathing cycles we detected to the totally breathing
cycles the RIP system detected. The measurement
results of the RIP system was regarded as the ground
truth of the breathing conditions. The experimental
results show that while the user sleeps with no quilt,
the measurement accuracy of breathing rate was
81.9% (SD = 0.11) in the side-lying position, and it
was 90.4% (SD = 0.07) in the supine position.
Moreover, while the user sleeps with a thin quilt, the
measurement accuracy of breathing rate was 84.1%
(SD = 0.05) in the side-lying position, and it was
88% (SD = 0.08) in the supine position. Overall, the
Figure 9: Measurement results of breath measurement in
experiment I.
98.0%
99.3%
96.7%
99.5%
91.5%
99.3%
94.5%
99.5%
0%
20%
40%
60%
80%
100%
Side lying Supine Side lying Supine
Sleep without quilt Sleep with a thin quilt
Head Detection Torso Detection
81.9%
90.4%
84.1%
88.0%
0%
20%
40%
60%
80%
100%
Side lying Supine Side lying Supine
Sleep without quil
t
Sleep with a thin quil
t
HEALTHINF 2012 - International Conference on Health Informatics
18

average accurate rate of breath measurement was
86.3%. The experimental results of the breath
measurement are shown in Figure 9.
For sleep position, the experimental results
showed that in the circumstance of sleeping with a
thin quilt, the detection accuracy was 100% (N=24)
in the side-lying position, and it was 100% (N=24)
in the supine position. Besides, while the user slept
with no quilt, the detection accuracy was 95.8%
(N=24) in the side-lying position, and it was 100%
(N=24) in the supine position.
4.2 Experiment I I: Realistic
Overnight-Sleep Monitoring
Experimental Design
The experiment was conducted to ensure that the
system could monitor the realistic overnight-sleep
conditions accurately. A male participant (28 years-
old) volunteered to participate in this experiment.
The same as the first experiment, the breathing
sensor (RIP) was used to measure the breathing
conditions as the ground truth. In addition, an
actigraphy was used to measure the movement of the
non-dominant hand while sleeping (Figure 10).
There was only one limitation that the participant
was asked to lie on the pillow. In this experiment,
the participant was asked to participate in a ten-day
overnight-sleep monitoring experiment. The
experiment did not specify the time to go to the bed,
the time to getting up, and the totally sleeping time.
Besides, we required participants to sleep with a thin
quilt for five days, and to sleep with no quilt for
another five days. Participant’s breathing rate, body
movement, and sleep position were monitored by
our method and compared to the RIP and actigraphy.
Figure 11 shows one of a realistic overnight-sleep
monitoring results in day 3. Figure 11a shows the
measurement results of breathing rate. Red curve
indicates the measurement results of RIP system,
and the blue curve indicates the measurement results
of our system. Lower part of Figure 11a shows the
Figure 10: Experimental Diagram. The breathing sensor
(RIP) and actigraphy are used to detect the breathing rate
and body movement.
sleep positions we detected (blue) and real condition
(red). Figure 11b shows the movement level
detected by an actigraphy, and Figure 11c shows the
movement level detected by our system. In this day,
the participant slept with a thin quilt from 1:30 AM
to 4:53 AM.
Experimental Results
The same with experiment I, the sleep measurement
were divided into four different conditions,
including two sleep positions (side-lying and supine)
and two sleep circumstances (sleep with a thin quilt
and sleep with no quilt). Totally, the participant slept
42 hours in ten nights.
Following shows the experimental results. In the
circumstance of sleeping with no quilt, the
measurement accuracy of head detection was 89.4%
(SD = 0.14) in the side-lying position and it was
99.9% (SD = 0.0007) in the supine position.
Moreover, the measurement accuracy of torso
detection was 89.3% (SD = 0.014) in the side-lying
position and it was 89.3% (SD = 0.0003) in the
supine position. Besides, in the circumstance of
sleeping with a thin quilt, the measurement accuracy
of head detection was 99.9% (SD = 0.007) in the
side-lying position and it was 98.8% (SD = 0.17) in
the supine position. Moreover, the measurement
accuracy of torso detection is 99.4% (SD = 0.0003)
in the side-lying position and it is 99.9% (SD =
0.003) in the supine position. The experimental
results of head and torso detection are shown in
Figure 12. Overall, the average accurate rate of head
detection was 96.7% (SD = 0.073), and the average
accurate rate of torso detection was 96.8% (SD =
0.031).
For body movement, the times of the movement
events in our method and actigraphy were compared.
According to the observation, we observed that big
body movement can be measured both in our system
and actigraphy, such as the event of turning over the
body. Besides, micro-movement could be measured,
(see Figure 11b and 11c).
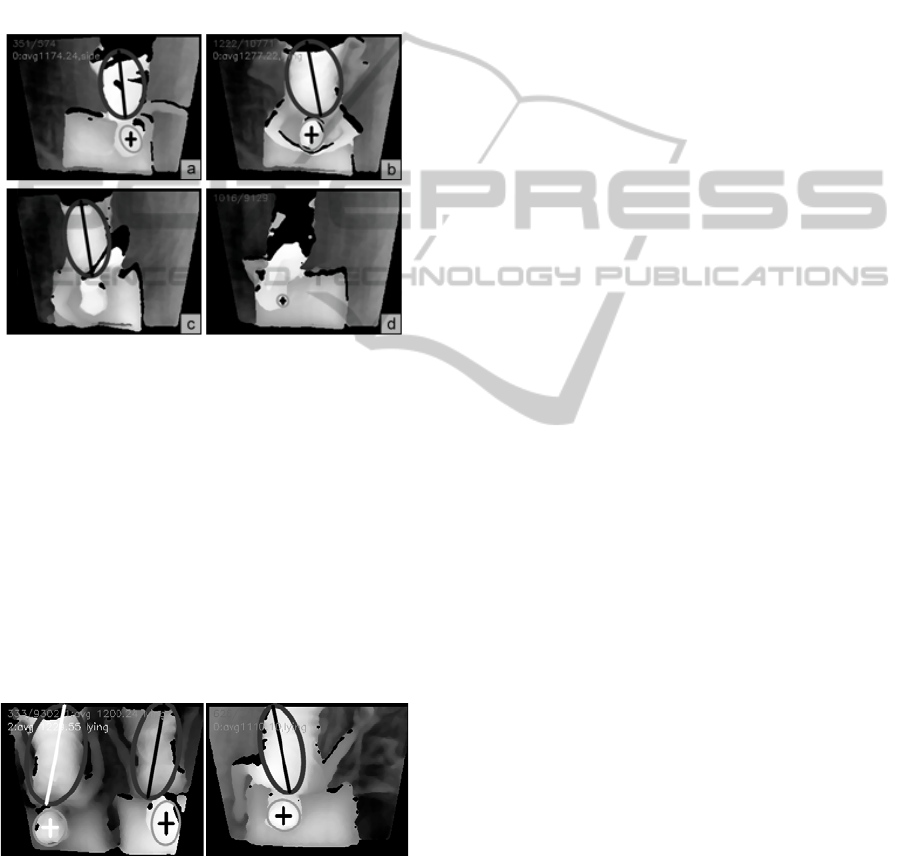
For breath measurement, the measurement
accuracy of breathing rate was 89.7% (SD = 0.05) in
the side-lying position and it was 92.8% (SD = 0.05)
in the supine position in the circumstance of
sleeping with no quilt Moreover, the measurement
accuracy of breathing rate was 92.4% (SD = 0.07) in
the side-lying position, and it was 92.7% (SD = 0.07)
in the supine position. Overall, the average accurate
rate of breath measurement was 92.03% (SD =
0.044). The comparison of the breath measurement
in these different conditions is shown in Figure 13.
For sleep position, the experimental results
showed that in the circumstance of sleeping with a
BREATH AND POSITION MONITORING DURING SLEEPING WITH A DEPTH CAMERA
19
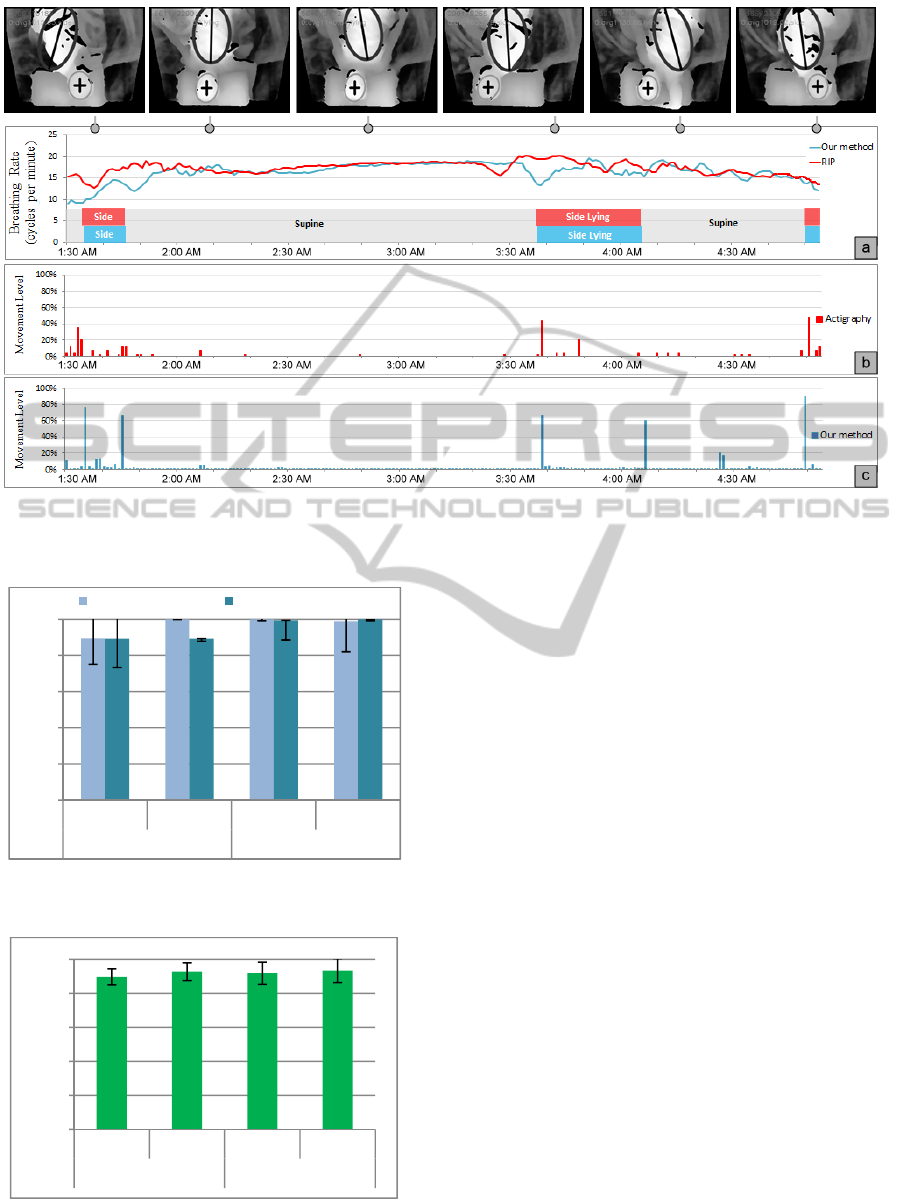
Figure 11: A Realistic Overnight-Sleep Monitoring. Red color indicates the ground truth measured by RIP and actigraphy,
and the blue color indicates the results of our system. (a) The results of breathing rate and sleep positions. (b) The
movement level detected by an actigraphy. (c) The movement level detected by our system.
Figure 12: Measurement results of head and torso
detection in experiment II.
Figure 13: Measurement results of breath measurement in
experiment II.
thin quilt, the detection accuracy was 94.7% (N=19)
in the side-lying position, and it was 100% (N=21)
in the supine position. Besides, while the user slept
with no quilt, the detection accuracy was 88.23%
(N=17) in the side-lying position, and it was 100%
(N=20) in the supine position.
5 DISCUSSIONS
The aim of this section is to summarize, analyse and
discuss the results of experiments and give
guidelines for the future developments.
5.1 Head/Torso Detection
From the experimental results of head and torso
detection, we observed some issues worthy of
discussion. First, while the user slept with a thin
quilt, the overall detection accuracy of torso was
better than uncovered. One reason might be that the
thin quilt could smooth the shape of the torso, and
enhance the measurement accuracy. Second, we
found that the gesture might affect the head
detection. In this system, the head and torso could be
detected accurately under the premise that the shape
of the head or torso is not overlapped by hand or
other objects. Figure 14a and 15b show two special
sleep gestures that can be detected accurately. It is
89.4%
99.9%
99.9%
98.8%
89.3%
89.3%
99.4%
99.9%
0%
20%
40%
60%
80%
100%
Side lying Supine Side lying Supine
Sleep without quilt Sleep with a thin quilt
Head Detection Torso Detection
89.7%
92.8%
91.9%
93.4%
0%
20%
40%
60%
80%
100%
Side lying Supine Side lying Supine
Sleep without quilt Sleep with a thin quilt
HEALTHINF 2012 - International Conference on Health Informatics
20
because that the shape of the head is not overlapped.
However, there are some conditions that the head or
torso could not be detected well. According to the
observation, we found that the head could not be
detected well while the user is scratching (Figure
14c and d). In this condition, the shape of the head
might be changed and no longer a sphere contour. In
this case, the system could not recognize it as a head.
One possible solution method is to detect the hand
position, and then we can estimate the head position
while the head is overlapping by hand.
Figure 14: Special Sleep Postures.
In addition, there are some sleep conditions or
sleep positions that we did not discuss. First, the
algorithm of head and torso detection we proposed
can be applied to detect multiple heads and torsos.
Moreover, a shortest distance pairing procedure is
used to pair the head and torso of specified sleeper.
However, we still have the detection problem while
the users are overlapping. Second, the head and
torso can be detect in the prone position. Howerer,
this system can not recogize whether the user is in
the supine position or prone position now. Figure 15
shows the detection result of the head and torso
detection in the prone position and multiple users.
Figure 15: Other Sleep Conditions. Left: multiple sleepers.
Right: prone position.
5.2 Breath Measurement
From the experimental results of breath
measurement, we observed some phenomenon
which was similar to the conditions of head and
torso detection. First, the measurement accuracy of
breathing is higher while sleeping in the supine
position than in the side-lying position. We observed
that there are more noises in the side-lying position
than in the supine position. Besides, according to our
measurement results, the average amplitude of the
breathing signals is 0.8 cm in the supine position.
However, the average amplitude of the breathing
signals is about 0.5 cm in the side-lying position.
Overall, less signal noises and more breathing
amplitude would increase the measurement accuracy
while sleeping in the supine position. Second, the
overall measurement accuracy of breathing while
sleeping with a thin quilt was better than the
accuracy while sleeping with no quilt. We speculate
that it might because the reason that the thin quilt
reduces the wrinkles of the torso surface. Third, the
movement of the torso is seen as the breathing signal,
but the system cannot identify whether the
movement is caused by breathing exercise or other
exercises. According to the observations of the
measurement results in experiment I, we found that
there were more detection errors while the user is
moving or turning around in bed. In experiment I,
the participants were asked to turn over the body
frequently, and the participant was almost in static
condition in experiment II. That’s the reason that the
measurement accuracy of breathing is lower in
experiment I than in experiment II. One possible
solution method is to suspend the breathing
measurement while the user is moving.
6 CONCLUSIONS AND FUTURE
WORK
In this study, we proposed a depth image sequence
analysis technique to monitor user’s sleep position,
body movement, and breathing rate on the bed
without any physical contact. A depth image-based
processing method is proposed to monitor the
sleeping conditions. The results of experimental I
showed that the proposed method is promising to
detect the head and torso with various sleeping
postures and body shapes. The results of
experimental II showed that the system can
accurately monitor the sleeping conditions.
Therefore, we confirm that the system could provide
relevant sleep information and sleep report to the
user. Furthermore, the sleep parameters which we
detected can provide to the sleep centre to diagnose
the sleep problems. This study is important for
BREATH AND POSITION MONITORING DURING SLEEPING WITH A DEPTH CAMERA
21

providing a non-contact technology to measure the
sleep conditions and assist users in better
understanding of his sleep quality.
In the future, we expect to detect more sleeping
conditions and solve some measurement limitations,
such as the problems of overlapping. Besides, we
will develop a multimedia feedback sleep-assisted
system which can detect the breathing status and
provide appropriate sleeping guidance in real time to
help users shorten the time to fall asleep. In addition,
a web-based browser will be developed to provide
the personalized sleeping information to the user.
ACKNOWLEDGEMENTS
This work was supported by the National Science
Council, Taiwan, under grants NSC 98-2221-E-002-
127-MY3. And many thanks to HealthConn Corp.
(http://hcc.healthconn.com/), who provided many
assistances of the professional knowledge.
REFERENCES
Aoki, H. and Koshiji, K., 2006. Non-contact Respiration
monitoring method for screening sleep respiratory
disturbance using slit light pattern projection. World
Congress on Medical Physics and Biomedical
Engineering, 14(7), 680-683.
Ancoli-Israel, S., Cole, R., Alessi, C., Chambers, M.,
Moorcroft, W., Pollak, C. P., 2003. The role of
actigraphy in the study of sleep and circadian rhythms,
Sleep , 26(3), 342-392.
BaHammam, A., 2004. Comparison of nasal prong pressure
and thermistor measurements for detecting respiratory
events during sleep. Respiration, 71(4), 385-390.
Idzikowski, C., 2003. Sleep position gives personality clue.
BBC News, 16 September 2003.
Born, J., Lange, T., Hansen, K., Molle, M. and Fehm, H.
L., 1997. Effects of sleep and circadian rhythm on
human circulating immune cells. The Journal of
Immunology, 158(9), 4454-4464.
Cantineau, J. P., Escourrou, P., Sartene, R., Gaultier, C.,
and Goldman, M., 1992. Accuracy of respiratory
inductive plethysmography during wakefulness and
sleep in patients with obstructive sleep apnea. Chest,
102(4), 1145-1151.
Cartwright, R. D., 1984. Effect of sleep position on sleep
apnea severit. Sleep, 7(2), 110-114.
Douglas, N., Thomas, S., and Jan, M., 1992. Clinical value
of polysomnography, Lancet, 339, 347-350.
Fitbit, http://www.fitbit.com/ , retrieved on 2011/5.
Harada, T., Sakata, A., Mori, T., and Sato, T., 2000. Sensor
pillow system: monitoring respiration and body movement
in sleep, Intelligent Robots and Systems, 1, pp. 351-356.
Hoque, E., Dickerson, R. F., Stankovic, J. A., 2010.
Monitoring body positions and movements during
sleep using WISPs. Wireless Health, 44-53.
Kushida, C. A., Chang, A., Gadkary, C., Guilleminault,
C., Carrillo, O., and Dement, W.C., 2001. Comparison
of actigraphic, polysomnographic, and subjective
assessment of sleep parameters in sleep-disordered
patients. Sleep Med., 2(5), 389-396.
Microsoft, Kinect, http://www.xbox.com/kinect, retrieved on
2011/3.
Loord, H., and Hultcrantz, E., 2007. Positioner - a method
for preventing sleep apnea. Acta Oto-laryngologica,
127(8), 861-868.
Maquet, P., 2001. The role of sleep in learning and
memory. Science, 294, 1048–1052.
Malakuti, K. and Albu, A. B., 2010. Towards an
intelligent bed sensor: Non-intrusive monitoring of
sleep irregularities with computer vision techniques.
International Conference on Pattern Recognition,
4004-4007.
Nakajima, K., Matsumoto, Y., and Tamura, T., 2001.
Development of real-time image sequence analysis for
evaluating posture change and respiratory rate of a
subject in bed. PHYSIOLOGICAL MEASUREMENT,
22, N21-N28.
Philips Actiwatch, http://www.healthcare.philips.com/ ,
retrieved on 2010/8
PneumaCare, http://www.pneumacare.com/ , retrieved on
2011/6.
Wareham,R., Lasenby,J., Cameron, J., Bridge, P. D., and
Iles, R., 2009. Structured light plethysmography (SLP)
compared to spirometry: a pilot study, European
Respiratory Society Annual Congress.
Sadeh, A., Sharkey, K. M., and Carskadon, M. A., 1994.
Activity-based sleep-wake identification: an empirical
test of methodological issues. Sleep, 17(3), 201-207.
Staderini, E. M., 2002. UWB radars in medicine. Aerospace
and Electronic Systems Magazine, 17(1), 13-18.
Spiegel, K., Leproult, R., and Cauter, D. V., 1999. Impact
of sleep debt on metabolic and endocrine function.
The LANCET, 354(9188), 1435-1439.
Szollosi, I., Roebuck, T., Thompson, B., Naughton, M. T.,
2002. Lateral sleeping position reduces severity of
central sleep apnea/cheyne-stokes respiration, Sleep,
29 (8), 1045-1051.
Thought Technology Ltd., http://www.thoughttechnology.
com/, retrieved on 2010/6.
Wang, C., Ahmed, A., and Hunter, A., 2007. Locating the
upper body of covered humans in application to
diagnosis of obstructive sleep apnea. Proceedings of
the World Congress on Engineering, 662-667.
Whyte, K. F., Gugger, M., Gould, G. A., Molloy, J.,
Wraith, P. K., and Douglas, N. J., 1991. Accuracy of
respiratory inductive plethysmograph in measuring
tidal volume during sleep, Journal of Applied
Physiology, 71(5), 1866-1871.
WakeMate, http://www.wakemate.com/ , retrieved on 2011/5.
Ziganshin, E. G., Numerov, M. A., and Vygolov, S. A.,
2010. UWB baby monitor. Ultrawideband and
Ultrashort Impulse Signals, 159-161.
HEALTHINF 2012 - International Conference on Health Informatics
22
