
DETECTION OF INCONSISTENCIES IN HOSPITAL DATA
CODING
Juliano Gaspar, Fernando Lopes and Alberto Freitas
CIDES – Department of Health Information and Decision Sciences, Porto, Portugal
CINTESIS – Center for Research in Health Technologies and Information Systems, Porto, Portugal
Faculty of Medicine, University of Porto, Porto, Portugal
Keywords: Inconsistencies, Errors, Data quality problems, Hospital databases.
Abstract: Introduction: Health professionals need data, in sufficient quantity and quality, and tools that can manage
the vast amount of available data. They need help for data management and appropriate support for decision
making.
Aim: The focus of this study is to develop a prototype that can contribute to the identification of data quality
problems in clinical and administrative data.
Methods: Methods involve the definition of requisites and business rules, the prototype development and
testing, and the realization of two studies using the prototype.
Results: Studies performed using the prototype resulted in the detection of many data problems and
inconsistencies. Amongst those we can point out, for instance, that 82,000 (15%) episodes had ‘diagnostic
code does not exist in ICD-9-CM table’ and that 783 (0,2%) episodes within ‘female breast cancer’ had the
variable gender equal to ‘male’.
Discussion: This prototype, besides contributing to the detection of data quality problems, is also expected
to be an incentive to the improvement of information system architectures. It shows the importance of the
development of mechanisms to detect and validate data in health environments.
1 INTRODUCTION
Medical databases generally involve all sorts of data
and store a considerable size of information (Kumar
et al., 2008). Data consists, generally, of records
with different type of information and with diverse
characteristics such as age, blood type, weight,
clinical images, diagnosis, lab results, among many
other patient details (Chandola et al., 2009). In the
latest years, with an exponential growth in hospital
information, the volume of electronic clinical
records has also significantly increased. Impaired
with this increase, new interests emerged in the
analysis of such information, thus driving it not only
to be used as a source to make decisions but also to
support hospital management (Freitas et al., 2005).
Amongst the various health services, hospital
focus gains a particular interest because it gathers a
higher complexity and procedures cost. This makes
hospital databases the main focus of various analysis
(Freitas et al., 2005). The display of reliable and
trustworthy information, obtained from solid data, is
vital to help health professionals and technicians in
the process of decision making and also help in
higher levels of hospital management. In this
context, Information Systems are responsible for
making, analyzing and disseminating such data
(Pinto, 2010).
1.1 Data Quality
The data value is directly proportional to its quality.
So, the higher the quality is, the greaters its utility
(Arts et al., 2002). It is important to consider that, to
insure data quality, certain basic rules must be
followed such as coherency, accuracy, integrity and
consistency (Tayi and Ballou, 1998
); (Wang, 1998);
(Silva-Costa et al., 2010). Thus, the importance of
rectify integrity problems, normalize values, fill or
identify missing values, identify redundant
information, among other processes in database
management (Barateiro and Galhardas, 2005).
The quality of data, accordingly to some authors,
is a relative concept and is directly correlated to the
189
Gaspar J., Lopes F. and Freitas A..
DETECTION OF INCONSISTENCIES IN HOSPITAL DATA CODING.
DOI: 10.5220/0003757301890194
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2012), pages 189-194
ISBN: 978-989-8425-88-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

information purpose. The authors use the “fitness for
use” concept that emphasizes the importance of
users’ point of view and their judgment in
information assertiveness (Tayi and Ballou, 1998
);
(Wang, 1998
); (Olson, 2003). Especially in medical
databases, this concept reinforces itself, because data
can have sufficient quality for economic analysis but
insufficient to clinical or epidemiological studies
(Silva-Costa, 2010
); (Cruz-Correia et al., 2009).
In the scenario of hospital department, electronic
data quality problems (DQP) gains a higher attention
because the information has a vital importance for
patient care (Daniel et al., 2008). However, due to a
high level of complexity and integrity inherent to
this activity, maintaining a high quality database is
not an easy chore.
1.2 Medical Data Coding Guidelines
There’s many disparity in health policies and
hospital funding between different countries.
Despite those differences, there are common
methods, characteristics and needs in all hospital
environments which make it possible to define a set
of international rules to analyze and compare
different hospitals in different countries, having in
consideration its’ health records (Pinto, 2010).
After being collected and coded, medical data
concerning patients, usually has billing information
frequently used only for administrative and financial
purposes. This does not prevent them from being
usefull to other areas such as health quality and
health care (Price et al., 2003).
These databases have a huge statistical potential,
due to their large volume and similarity between
hospitals, intitutions or even countries. This
comparation between hospitals is due, mainly, to the
use of a core group of variables named
internationaly as “Minimum Basic Data Set”
(MBDS) (Aylin et al., 2007
); (Romano et al., 1995).
A part of this coded data is generated in the
hospital discharge codification process. In this
process, the information collected from clinical
records, mainly diagnosis and procedures, is
generally coded according to the “International
Classification of Diseases” (ICD). It is also recorded
the “Diagnostic Related Group” (DRG) in which
episode is grouped. The use of ICD-9-CM
1
, along
these past years, has had many purposes such as
1
ICD-9-CM: International Classification of Diseases, Ninth
revision, Clinical Modification.
supporting the health services payment, studding
their costs, evaluate quality, planning future needs
and helpping clinical research (Ginde et al., 2008),
among others.
In Portugal, systematic codification of
hospitalizations in 1989 (Lopes, 2010) and it was
addopted the use of DRG as a hospital “case mix”
measurement. Nowadays, the main hospital
information systems have databases made of clinical
and administrative data, which were compiled
accordingly to the European established MBDS
(Oliván, 1997).
In Portugal, the Health Ministery defines and
publishes regulations that, not only, determine the
prices to be charged by the health delivered in the
National Health Service (NHS), but also clearly
distinguishes between what should be an inpatient or
an ambulatory episodes, among other rules for the
codification in DRG.
The evaluation of clinical coding quality is
essential for the correct attribution of hospital
funding, as hospital evaluation and funding
theirselves depend in DRG grouping (Pinto, 2010).
So, all MBDS potential for hospital management
and research can be compromised if clinical
codification does not have certain levels of quality.
2 AIM
The aim of this study is to develop a prototype for
the detection of data quality problems and
inconsistencies in inpatient and ambulatory episodes
in hospital databases. The prototype is intended to
detect common errors in health related databases and
also contextualize errors in specific medical
specialties.
3 METHODS
Prototype and the studies regarding its use the
development process follow the following
predefined steps:
Analyze the central database structure and the
coding guidelines;
Identify the business rules, define prototype
requisites, implement and realize the tests;
Perform a two studies including data from the
last 10 years, the first from a hospital and second
including data concerning a pre-determined disease
diagnosed in all NHS hospitals.
HEALTHINF 2012 - International Conference on Health Informatics
190
The database used is composed of hospital episodes,
data ambulatory and inpatient data, from medical or
surgical specialties, concerning 96 Portuguese
hospitals with discharges between the years 2000
and 2009, making a total of approximately 12
million records. Access to this data was possible due
to the ACSS
2
collaboration in the HR-QoD
3
project
developed by the Department of Health Information
and Decision Sciences of Faculty of Medicine of
University of Porto. All data used was anonymous
and clinical data was coded in ICD-9-CM.
Based on the defined requisites and business
rules, auxiliary tables were created to store
information from the DQP detected such as error
codes and the errors quantity detected in each
hospital and year. Business rules contain, rules that
validate whether the information contained in a
record is consistent, meaning that it does not present
incongruences between the values of a variable in
relation to values of other variables in the same
episode. If the values are accordingly to regulations
and guidelines of that codifications used in Portugal,
such as ICD-9-CM. These were created and
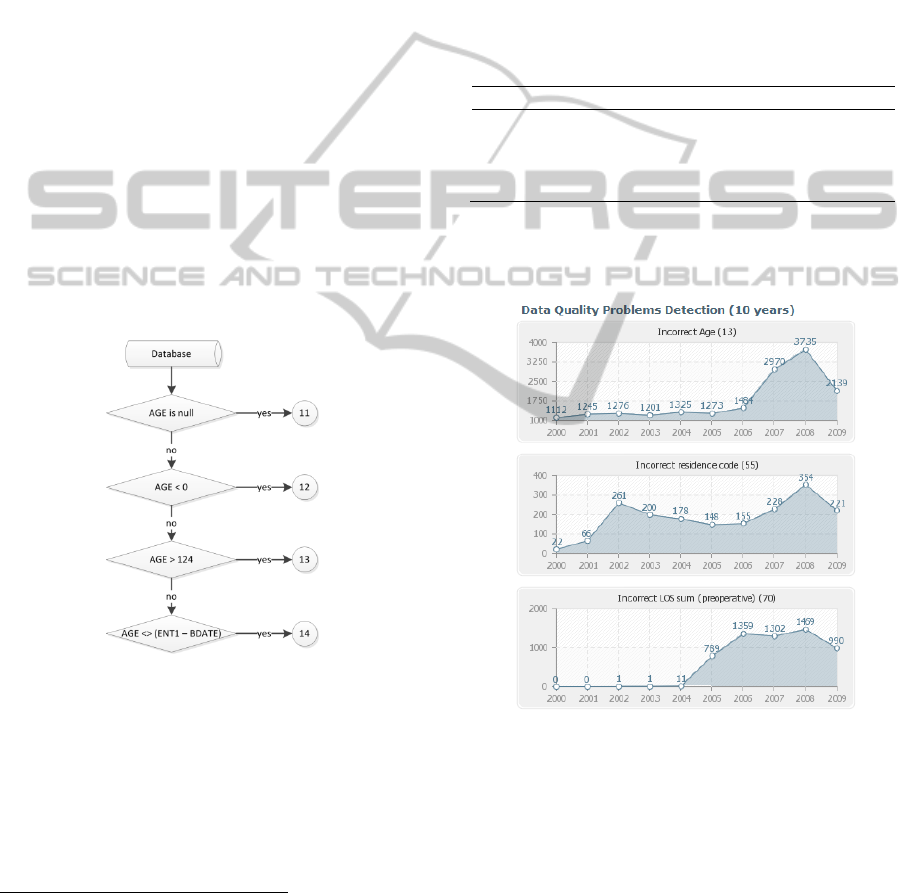
schematized as showed in figure 1.
Figure 1: Business rule to variable “AGE”.
In the implementation of the prototype the
following programming languages were used: PHP,
HTML and JavaScript the Eclipse developing tools
for PHP and Toad for Oracle were also used.
2
ACSS: Administração Central do Sistema de Saúde (in
portuguese).
3
HR-QoD: Quality of data (outliers, inconsistencies and errors) in
hospital inpatient databases: methods and implications for data
modeling, cleansing and analysis.
4 RESULTS
With its’ use it was possible to create reports with
the detection of DQP and respective incongruences.
These reports included the analysis of over 50
different types DQP in the studied data.
As result of a first study, data from a hospital
concerning discharges between the years 2000 and
2009 (inclusive) was selected, totalizing 543,133
hospital episodes. Some of the problems detected are
shown in table 1.
Table 1: DQP Detected.
Problem Description N %
Incorrect length of stay (LOS) 191,282 35.22
Diagnostic code not in
ICD-9-CM
table 82,422 15.18
Procedure code not in
ICD-9-CM
table 9,023 1.66
Principal diagnostic is null 85 0.02
The evolution, in the 10 years of determined
detected DQP can be seen in graphics presented in
figure 2 and 3.
Figure 2: Data Quality Problems within 10 years.
In the figure 2 we can see that, for example, the
growth (after 2007) errors in the variable ‘AGE’
(calculated incorrectly) and also that the total days in
preoperative are incorrectly calculated after 2004.
The figure 3 show a gradual decline of errors
related to ‘weight at birth’, the accentuated increase
of ‘repeated diagnosis’ in the same episodes between
2007 and 2008, the gradual increase related to ‘inter-
hospital transfers’ and identical volumes of errors
between 2000 and 2004 related with ‘LOS sum
(preoperative)’ and ‘surgical date’.
DETECTION OF INCONSISTENCIES IN HOSPITAL DATA CODING
191

Figure 3: Data Quality Problems within 10 years.
For the second study, the pathology Female
Breast Cancer (FBC) was chosen due to a publication
released in January 2011 by INE
4
, stating that in
Portugal 1,635 people died in the year 2009 (INE,
2011) due to FBC and according to WHO
5
, FMC is
the most frequent tumor worldwide. It’s the main
cause of female death internationally (Bastos et al.,
2007); (WHO, 2011).
To this purpose, all episodes with diagnosis of
FBC coded in ICD-9-CM with ‘174.x’ were selected
in all 96 Portuguese hospitals in the last 10 years,
resulting 346,654 records.
Specific queries were applied in order to detect
inconsistencies in the context of codification in this
disease. Table 2 shows the most relevant
inconsistencies detected.
4
INE: Instituto Nacional de Estatística (in Portuguese)
5
WHO: World Health Organization.
Table 2: Contextual DQP Detected.
Contextual Problem Description N %
‘V58.0’ in secundary diagnostics 66,875 19.34
‘V58.1’ in secundary diagnostics 72,281 20.90
‘V10.x’ in principal diagnostic 830 0.24
Episodes with ‘gender’ variable = ‘male’ 783 0.23
From this analysis we can point out 783 records
with value “male” in the variable ‘gender’. This fact
represents a serious DQP because this study is
specifically about FBC. Male Breast Cancer is coded
in ICD-9-CM with ‘175.x’, and so code ‘174.x’ is
restricted to female patients.
5 DISCUSSION
The algorithm was capable of identifying the most
significant DQP existing in the database.
The “Incorrect length of stay (LOS)”, one of the
DQP detected in 35% of total episodes, observes
some particular considerations: (a) the regulation
number 839-A/2009 from the health ministry
informs that “Global Length of Stay” (G-LOS)
concerns the total number of days consumed by each
patient within the hospital, considering the
admission day and ignoring the discharge day (SNS,
2009); (b) a most detailed analysis of this
inconsistency value showed that, despite the
business rule is correct with the in vigor regulation,
this value can be caused by inconsistencies in
informatics applications that calculate the variable
G-LOS; (c) some specialists make their calculations
only with the value of the day in question;
meanwhile other consider also the hours and
minutes, which can cause one day difference in G-
LOS.
DQP occurrences DQP “Diagnostic code not in
ICD-9-CM table” and “Procedure code not in ICD-
9-CM table”, showed in table 1, are due essentially
with the passing years, to the reviewing of some
codes and the modification or others. However, the
process associated to the management of these
modifications is not performed efficiently. This
process would have to store the different versions of
changes made to the ICD-9-CM table used in each
hospital as well as to store the version used in the
codification process instant (Lopes, 2010).
Codification errors on principal diagnosis, such
as the 85 cases presented on table 1, imply the
classification of episodes with DRG 470
(“Ungroupable”) in these cases, the hospital is not
financially compensated for the episode costs (Silva-
Costa et al., 2010).
HEALTHINF 2012 - International Conference on Health Informatics
192

The gradual decrease of DQP related with
‘weight at birth’, presented on figure 1, could be
associated with data validation rules, performed
during data entry, by the different electronic
applications used on NHS hospitals during the last
years.
In figure 3 a gradual increment related to patient
transfers between hospitals after the year 2006 can
be observed. DQP “Code of the reason for the inter-
hospital transfer is null” and “Code of the inter-
hospital transfers is null”, raise the issue that the
lack of these codes could be related to regulations
that the health ministry posted in 2003: (a) a hospital
that transfers a patient to other, by “lack of
resources”, can only receive up to 50% of the
correspondent DRG; (b) the hospital that receives a
transferred patient is limited, in its’ classification, to
a restrict set of DRG.
Despite that these regulations already existed in
2003, only after 2006 all NHS hospitals had these
regulations. Regardless of the cause, it is a fact that
this problem has obvious implications in hospital
reimbursement level.
An analysis to identify the existing relation
between errors found in years 2000 to 2004, in DQP
sum (preoperative) < 0’ and ‘Surgical date <
Admission date’ (Figure 3), revealed that all related
episodes had many patients that were operated in the
emergency service and then admitted in the hospital.
After 2004 the ‘Admission date’ to be considerate
was the lesser date registered, being the emergency
service entry date or the admittance date in the
hospital services.
The identification of 783 cases coded with
‘174.x’ and with the ‘gender’ variable equal to
‘male’, in the second study, is of extreme
importance. Assuming that these records are actually
male patients, this inconsistence represents a 0.23%
impact in this study. However, if the focus of the
studies was Male Breast Cancer, coded in ICD-9-
CM as ‘175.x’, these 783 cases wrongly coded
would correspond to a total of 25% cases of Male
Breast Cancer that may not be considered.
Official coding guidelines (ACSS, 2009) state
that “in admittance of the patient exclusively to
chemotherapy, imunohemoterapy or radiotherapy,
the principal diagnosis code attributed should be
‘V58.x’, and secondary diagnosis should be the ones
representing the cause for treatment”.
After these directives, we can verify that in
139,156 records, 40.2% of total episodes of FBC
(Table 2) present ‘V58.0’ or ‘V58.1x’ as secondary
diagnosis codes. The average rate of this
inconsistency is 64% per year. The directives also
state that the code ‘V10.x’ (‘personal history of
malign cancer’) should always be coded as a
secondary diagnosis, however 830 records were
found with ‘V10.x’ was the principal diagnosis.
6 CONCLUSIONS
This study helped the analysis and identification of
existing DQP in a coded health database, and also
helped in the determination of a profile for the
coding of FBC episodes.
Acknowledge of anomalies in the data may allow
an immediate improvement in their quality, when
the correction is feasible. This acknowledgement is
important for the management of health, both
nationally and regionally, and also locally in each
hospital or health facility.
The results are graphically simple and allow a
direct reading of the most relevant values and are
certainly an asset to help managing and controlling
the efficiency of health facilities.
The visualization of DQP, in graphical format
over 10 years, allowed users, only with a visual
analysis of the evolution of the problem, to quickly
identify possible relationships between the increase
or decrease of a problem and the date of
implementation of certain software in the hospital,
or the adoption of a new standard for procedure..
Effective management of versions, also known
as change management, applied both by managers
and by the NHS hospital managers, in addition to
companies that develop software for health, can help
to prevent problems to happen again, as some of
those presented in this study.
This study is a contribute to the detection of
DQP, and also an incentive to the improvement of
the architecture of existing information systems,
emphasizing the importance of developing
mechanisms and methods for detection and
validation in health. This study also intends to alert
for the impact of these errors in epidemiologic
studies and, as well, in management evaluations and
health related policies.
6.1 Future Works
In the next stages of this study, we intend to
replicate the method used in this study to other
pathologies and apply data mining algorithms to
improve the detection of patterns, abnormal cases,
possible errors or inconsistencies.
DETECTION OF INCONSISTENCIES IN HOSPITAL DATA CODING
193

ACKNOWLEDGEMENTS
The authors would like to thank the support given by
the research project HR-QoD - Quality of data
(outliers, inconsistencies and errors) in hospital
inpatient databases: methods and implications for
data modeling, cleansing and analysis (project
PTDC/SAU-ESA/75660/2006).
REFERENCES
ACSS, (2009). CID-9-MC Guidelines Oficiais para
Codificação: Em vigor a partir de Outubro de 2009
(Lisboa, Administração Central do Sistema de Saúde,
IP).
Arts, D., Keizer, N., and Scheffer, G.-J., (2002). Defining
and Improving Data Quality in Medical Registries: A
Literature Review Case Study, and Generic
Framework. In: J Am Med Inform Assoc 9, 600-611.
Aylin, P., Bottle, A., and Majeed, A., (2007). Use of
administrative data or clinical databases as predictors
of risk of death in hospital: comparison of models. In:
BMJ 334, 1044.
Barateiro, J., and Galhardas, H., (2005). A Survey of Data
Quality Tools. In: Datenbank-Spektrum 5, 15-21.
Bastos, J., Barros, H., and Lunet, N., (2007). Evolução da
Mortalidade por Cancro da Mama em Portugal (1955-
2002). In: Acta Med Port, 139-144.
Chandola, V., Banerjee, A., and Kumar, V., (2009).
Anomaly Detection: A Survey. In: ACM Computing
Surveys 41.
Cruz-Correia, R., Rodrigues, P., Freitas, A., Almeida, F.,
Chen, R., and Costa-Pereira, A., (2009). Data Quality
and Integration Issues in Electronic Health Records. In
Information Discovery on Electronic Health Records.
In: CRC Data Mining and Knowledge Discovery
Series, H. V. C.a. Hall, ed., pp. 55-95.
Daniel, F., Casati, F., Palpanas, T., Chayka, O., and
Cappiello, C., (2008). Enabling Better Decisions
through Quality-aware Reports. In: International
Conference on Information Quality (ICIQ) (USA).
Freitas, A., Brazdil, P., and Costa-Pereira, A., (2005).
Mining Hospital Databases for Management Support.
Paper presented at: IADIS Virtual Multi Conference on
Computer Science and Information Systems, pp. 207-
212.
Ginde, A. A., Tsai, C. L., Blanc, P. G., and Camargo, C.
A., Jr., (2008). Positive predictive value of ICD-9-CM
codes to detect acute exacerbation of COPD in the
emergency department. In: Jt Comm J Qual Patient
Saf 34, 678-680.
INE, (2011). Boletim mensal de estatística: Janeiro de
2011. Available in: http://www.ine.pt. Access In:
02/03/2011.
Kumar, V., Kumar, D., and Singh, R. K., (2008). Outlier
Mining in Medical Databases: An Application of Data
Mining in Health Care Management to Detect
Abnormal Values Presented In Medical Databases. In:
IJCSNS International Journal of Computer Science
and Network Security, 272-277.
Lopes, F., (2010). Portal da Codificação e dos GDH.
Available in: http://portalcodgdh.min-saude.pt.
Access In: 31/10/2010.
Oliván, J. A. S., (1997). Sistemas de información
hospitalarios: el CMBD. In: Scire: representación y
organización del conocimiento 3, 115-130.
Olson, J. E., (2003). Data Quality - The Accuracy
Dimension, Morgan Kaufmann Publishers edn.
Pinto, R., (2010). Sistemas de informações hospitalares de
Brasil, Espanha e Portugal - Semelhanças e diferenças.
In: FIOCRUZ (Rio de Janeiro, Escola Nacional de
Saúde Pública Sergio Arouca), pp. 162.
Price, J., Estrada, C. A., and Thompson, D., (2003).
Administrative Data Versus Corrected Administrative
Data. In: Am J Med Qual 19, 38-44.
Romano, P. S., Zach, A., Luft, H. S., Rainwater, J., Remy,
L. L., and Campa, D., (1995). The California Hospital
Outcomes Project: using administrative data to
compare hospital performance. In: Jt Comm J Qual
Improv 21, 668-682.
Silva-Costa, T., (2010). Indicadores de Produção
Hospitalar - Uma forma de medir a produção dos
hospitais Portugueses (Porto, Faculdade de Medicina
da Universidade do Porto), pp. 172.
Silva-Costa, T., Marques, B., and Freitas, A., (2010).
Problemas de Qualidade de Dados em Bases de Dados
de Internamentos Hospitalares. Paper presented at: 5ª
Conferência Ibérica de Sistemas e Tecnologias de
Informação (Santiago de Compostela).
SNS, (2009). Portaria n.º 839-A/2009 - Ministério da
Saúde de Portugal, M.d. Saúde, ed. (Lisboa, Diário da
República), pp. 4978-(4972) a 4978-(4124).
Tayi, G. K., and Ballou, D. P., (1998). Examining Data
Quality. In: CACM 41, 54-57.
Wang, R. Y., (1998). A Product Perspective on Total Data
Quality Management. In: CACM 41, 58-65.
WHO, (2011). World Health Organization. Available in:
http://www.who.int/en/. Access In: 20/07/2011.
HEALTHINF 2012 - International Conference on Health Informatics
194
