
APPLICATION OF THE PHOTODYNAMIC THERAPY
IN MEDICINE AND DENTISTRY
Literature Review on Photodynamic and Antimicrobial Photodynamic Therapy
Zuzanna Oruba
1
, Maria Chomyszyn-Gajewska
1
and Wojciech Macyk
2
1
Department of Periodontology and Oral Medicine, Jagiellonian University, Montelupich 4, 31-155, Kraków, Poland
2
Faculty of Chemistry, Jagiellonian University, Ingardena 3, 30-060, Kraków, Poland
Keywords: Photodynamic therapy, Antimicrobial photodynamic therapy, Periodontitis.
Abstract: Photodynamic therapy (PDT) is recently being recognized as an attractive, non-invasive and alternative
treatment method for precancerous lesions and superficial cancers. PDT has many advantages when
compared with conventional treatment modalities. It has also been used for the photoinactivation of
microbes. There is an increasing interest in the practical application of antimicrobial photodynamic therapy
(aPDT) in many branches of dentistry, especially in periodontology, for the management of such conditions
as chronic periodontitis or periimplantitis. The aim of the present paper was to discuss the application of
photodynamic therapy in medicine and dentistry. The results of many so far published studies seem to be
very promising indicating at the same time that further research is needed to establish the optimal protocol
for effective photodestruction of tumor cells and microorganisms.
1 INTRODUCTION
Photodynamic therapy (PDT) is a medical treatment
that utilizes light to activate a photosensitizing agent
in the presence of oxygen. It is a noninvasive and
painless medical procedure with relatively little side
effects. Its use in medicine and dentistry is becoming
widespread.
2 PRINCIPLE OF
PHOTODYNAMIC THERAPY
Photodynamic therapy (PDT) involves three agents,
i.e. photosensitizer, light and oxygen. The
administration of a photosensitizer is followed by
irradiation with the light of a specific wavelength
(Takasaki et al., 2009). Upon photon absorption a
molecule of the photosensitizer gets activated and
transforms from its ground state (S
0
) into an excited
singlet state (S
1
). The lifetime of the singlet state is
in the nanosecond timescale (Stochel et al., 2009,
chapter 17), which is too short to react with other
molecules. From this state the drug may decay back
to the ground state by emitting fluorescence or by
internal conversion with energy lost as heat.
However, to obtain a therapeutic photodynamic
effect, the molecule of the photosensitizer must
undergo electron spin conversion to its triplet state
(T
1
). The lifetime of the triplet state is in the
microsecond to millisecond range (Soukos and
Goodson, 2011). The molecule in its triplet state can
again reach the ground state (in the case of light
emission the process is called phosphorescence) or it
can react further with oxygen according to two
different types of mechanisms (Scheme 1) (Soukos
and Goodson, 2011). Type I reaction involves
electron-transfer reaction between the
photosensitizer triplet state and a substrate (O
2
).
When oxygen participates in this process reactive
oxygen species (ROS) (superoxide, hydroxyl radical,
hydrogen peroxide) are produced. They are harmful
to cell membrane integrity and cause irreparable
biological damage. In the type II reaction the
molecule of a photosensitizer in the triplet state
transfers its energy directly to oxygen to form
singlet oxygen (
1
O
2
) which is highly reactive and
induces oxidative cell damage (Takasaki et al., 2009;
Stochel et al., 2009, chapter 17; Soukos and
Goodson, 2011).
190
Oruba Z., Chomyszyn-Gajewska M. and Macyk W..
APPLICATION OF THE PHOTODYNAMIC THERAPY IN MEDICINE AND DENTISTRY - Literature Review on Photodynamic and Antimicrobial
Photodynamic Therapy.
DOI: 10.5220/0003775501900195
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2012), pages 190-195
ISBN: 978-989-8425-91-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)
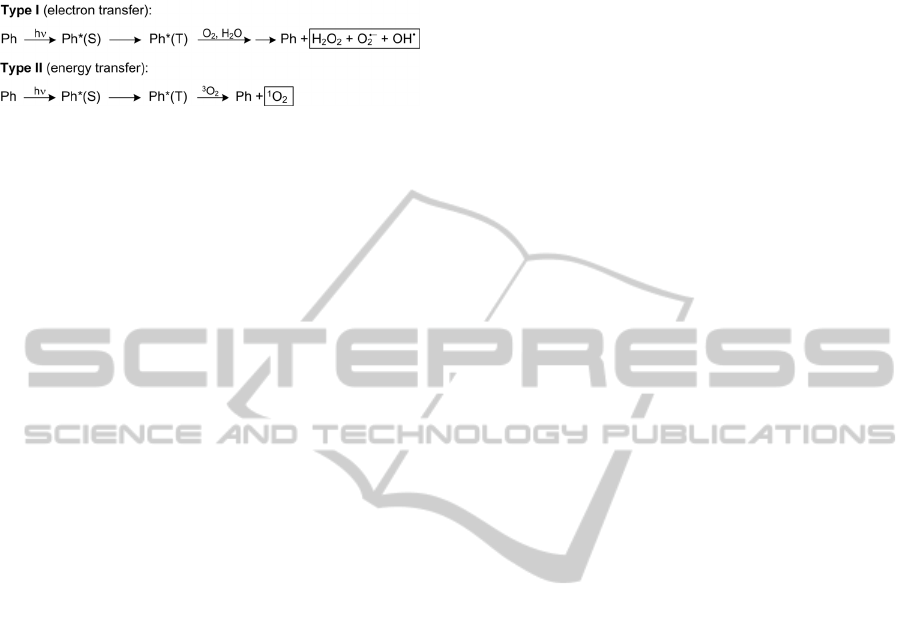
Scheme 1: Two types of mechanisms governing the
photodynamic process. ROS are placed in rectangles; Ph –
a photosensitizer in its singlet (S) or triplet (T) state.
2.1 PDT in the Treatment of Cancer
Photodynamic therapy is a relatively new treatment
modality of localized cancers. Upon administration
of a photosensitizer and its illumination, tumor cells
are being directly killed as a result of oxidative
damage (necrosis and apoptosis). Additionally, the
vasculature of the tumor and surrounding tissues are
damaged, resulting in indirect tumor cells death of
hypoxia and starvation (Stochel et al., 2009, chapter
17); (Triesscheijn et al., 2006). The ideal
photosensitizer for the use in oncology should
possess the following properties: chemical purity,
high binding affinity for tumor cells and low for host
cells, non-toxicity in the dark, minimal risk of
promoting mutagenic processes, high absorption
coefficient within the phototherapeutic window
(620-1000 nm) and as low as possible in the range of
400-600 nm to avoid skin sensitivity to solar
irradiation after drug administration, high quantum
yield of excited triplet state generation (the
efficiency of PDT depends on photophysical
properties of this state) (Stochel et al., 2009, chapter
17). Following photosensitizers are currently
approved for the clinical use: Photofrin (porfimer
sodium), Levulan (5-aminolevulinic acid), Metvix
(methyl ester of ALA), mTHPC (meso-tetra-
hydroxyphenyl-chlorin) (Triesscheijn et al., 2006).
PDT had been applied clinically in the treatment of
bladder cancer, skin cancer, Bowen’s disease, head
and neck cancer, esophageal cancer, Barrett’s
esophagus, endobronchial cancer, actinic keratoses
(Triesscheijn et al., 2006); (Overholt et al., 2007).
In dental surgery, PDT has been applied in the
treatment of oral leukoplakia, a premalignant lesion
of the oral mucosa with a rate of malignant
transformation of 0.1-17% (Spinola Ribeiro et al.,
2010). Upon PDT with the use of ALA as a
photosensitizer in combination with red light, all
authors noted high response-to-treatment rate and a
very low recurrence rate in a long-term observation
(Spinola Ribeiro et al., 2010). Lin et al. (2010)
reported excellent outcomes of PDT in the treatment
of other oral precancerous lesions – oral verrucous
hyperplasia (OVL) and oral erythroleukoplakia
(OEL) (Lin et al., 2010). Upon the use of PDT with
20% ALA irradiated with 635 nm laser light, a
complete response for 100% of OVL lesions and
95% of OEL was achieved after an average of 3.6
and 3.4 treatment sessions, respectively. The authors
concluded, that for oral precancerous lesions ALA-
PDT is one of the best treatments of choice.
2.2 Photodynamic Antimicrobial
Chemotherapy (PACT)
The principle of PACT (also known as antimicrobial
photodynamic therapy, aPDT) is similar to PDT.
Photosensitizers and light (visible or UV) are used in
order to induce phototoxic response, usually via an
oxidative damage (Stochel et al., 2009, chapter 18).
In PACT, the photosensitizer should basically
possess properties similar to those expected for
PDT, with a high binding affinity for
microorganisms, broad spectrum of action and a low
propensity for selecting resistant bacterial strains
(Soukos and Goodson, 2011). The differences in
susceptibility of gram-positive and gram-negative
bacteria have been reported (Takasaki et al., 2009;
Usacheva et al., 2001). Gram-positive bacteria are
generally susceptible to photoinactivation. Gram-
negative bacteria seem to be more resistant to
PACT, mostly because of their additional outer
membrane which decreases the permeability and
reduces the photosensitizer uptake (Takasaki et al.,
2009). Moreover, the surface of gram-negative
bacteria cells is negatively charged, which makes
anionic and neutral photosensitizers ineffective
(Stochel et al., 2009, chapter 18). However,
phenothiazinium dyes (methylene blue and toluidine
blue), which are most commonly used in PACT,
bear pronounced cationic charge and thanks to the
electrostatic interaction can bind to the outer
membrane of both gram-negative and gram-positive
bacteria and penetrate bacterial cells (Soukos and
Goodson, 2011); (Usacheva et al., 2001). Reactive
oxygen species generated upon illumination of the
photosensitizer are lethal to bacteria by oxidizing
cell membrane (lipid peroxidation) causing its
decomposition, followed by destruction of nucleic
acids and proteins (Stochel et al., 2009, chapter 18).
2.3 PACT in Dentistry
2.3.1 Dental Caries
Dental caries is the result of tooth-hard tissue
demineralization in the presence of acids secreted by
supragingival biofilm bacteria (Streptococcus and
APPLICATION OF THE PHOTODYNAMIC THERAPY IN MEDICINE AND DENTISTRY - Literature Review on
Photodynamic and Antimicrobial Photodynamic Therapy
191

Lactinobacillus species) (Soukos and Goodson,
2011). Up to 10-fold reduction of the viability of S.
mutans, the main cariogenic bacteria, was achieved
by toluidine blue mediated PACT, even when the
organisms were embedded in a collagen matrix
mimicking carious dentin (Burns et al., 1995). The
susceptibility of cariogenic bacteria was confirmed
by other authors (Williams et al., 2004). PACT may
be useful in the prevention of caries, management of
early carious lesions and disinfection of carious
cavities before restoration.
2.3.2 Endodontics
The success of the endodontic treatment relies on the
elimination of infection from the root canal system.
The conventional means to achieve it is to perform
chemo-mechanical debridement and irrigation with
disinfectant solutions, like sodium hypochlorite
(NaOCl). However, anatomical complexity of the
root canal system (isthmuses, ramifications,
presence of dentinal tubules) makes complete
removal of bacteria with standard procedures and
medicaments almost impossible (Soukos and
Goodson, 2011). Therefore, the adjunctive
antimicrobial PDT (aPDT) has been employed to
eliminate residual root canal bacteria in many
studies, the results of which seem to be very
promising. The combined use of red light and
methylene blue results in reduction of Enterococcus
faecalis viability by 40 – 97% in the experimentally
infected root canals of extracted human teeth (Foschi
et al., 2007; Silbert et al., 2000; Soukos et al., 2006).
The results of in vivo studies conducted by Bonsor,
Nichol, Reid and Pearson (2005 and 2006) point that
PACT is as effective in root canal system
disinfection as conventional chemo-mechanical
techniques (instrumentation with NaOCl/citric acid
irrigation) (Bonsor et al., 2005; Bonsor et al., 2006).
These authors highlighted also, that aPDT is more
biocompatibile than conventional irrigants. It was
confirmed by Xu et al. (2009), who reported that
although some of the light energy applied to the root
canal escapes from the root apex (<10%), methylene
blue-mediated aPDT is harmless to osteoblasts in the
periapical region. This is not the case for sodium
hypochlorite, which is highly toxic and damages
cells of the periapical tissues (Xu et al., 2009).
2.3.3 Periodontology
Periodontology deals with the diseases of
periodontium (gum, alveolar bone and periodontal
ligament). Chronic periodontitis, the most common
periodontal disease, which refers to approximately
48% of the population (Albandar, 2005) and is a
major cause of tooth loss (Bakrami et al., 2008), is
characterized by a progressive destruction of the
periodontium’s fibers and alveolar bone, resulting in
following clinical symptoms: pathological pockets
or gum recessions, attachment loss, bony defects,
bleeding, hypermobility of the teeth and eventually
tooth loss. Following gram-negative anaerobes are
considered the most harmful for periodontium and
are isolated from the deepest periodontal pockets
and sites with severe bone loss: Porphyromonas
gingivalis, Tanerella forsythia and Treponema
denticola (so called ‘red complex’ according to
Socransky) (Socransky and Haffajee, 2002).
The effective treatment of the periodontal disease
is of a great importance also when general health is
considered, as the relationship between periodontal
disease and several systemic disorders, e.g.
cardiovascular disease, diabetes mellitus,
rheumatoid arthritis, cerebral infarction or
hypertension was proved (Detert et al., 2010;
Seymour et al., 2003; Lagervall et al., 2003).
Effective bacteria eradication is the basis of
periodontal treatment. Standard non-surgical
treatment procedures, like supra- and subgingival
plaque removal, have to be accompanied with some
additional antimicrobial means, like the
administration of antibiotics. However, the use of
antibiotics, delivered systemically or locally, apart
from many other side effects, promotes the
emergence of resistant bacterial strains, which,
according to WHO, is becoming a threatening
problem in healthcare worldwide. From this
standpoint, new and effective antimicrobial
approaches are urgently needed to be introduced.
The interest in use of PACT in periodontology is
considerable. Its effectiveness against
periopathogens has been proved in many in vitro
studies: with the use of toluidine blue (TBO) or
methylene blue (MB) as photosensitizers and a light
wavelength of approximately 632 nm emitted by a
He-Ne laser, significant reductions in the viability of
bacteria were observed (Bhatti et al., 2002; O’Neil et
al., 2002; Chan and Lai, 2003). Matevski et al.
determined optimal PACT parameters for the
effective photoinactivation of P. gingivalis in terms
of light intensity (25 mW/cm
2
), light dose (10 J/cm
2
)
and TBO concentration (12.5 µmol/ml) and applied
them for inactivation of P. gingivalis resuspended in
blood or serum to mimic actual periodontal pocket
conditions. Interestingly, in the presence of blood or
serum, the decline in bacteria viability was still
statistically significant, but there was a large
decrease in effectiveness compared with
BIODEVICES 2012 - International Conference on Biomedical Electronics and Devices
192

blood/serum-free suspensions. Blood and serum
appeared to partially protect P. gingivalis from
PACT. This effect can be explained by a lowered
light penetration through blood and serum (due to
light absorption and scattering by these media) and
by scavenging of photogenerated reactive oxygen
species through oxidation of blood/serum organic
components.
The susceptibility of P. gingivalis to PDT was
also confirmed in animal model study conducted by
Koemerik et al. (2003). Upon the use of 1 mg/ml of
TBO in combination with increasing light doses (6,
12, 24 and 48 J) in rats previously infected with P.
gingivalis, no viable bacteria were detected. After
irradiation, histological examination was carried out.
No adverse effects of PACT on the periodontal
tissues were observed. Even with the highest
concentration of TBO (1 mg/ml) and the highest
light dose tested (48 J) no ulcer on epithelium or
inflammation of the connective tissue were detected.
The authors evaluated the alveolar bone levels of the
maxillary molars by morphometric and radiographic
methods. The results showed that with the use of
TBO concentration of 0.1 and 1 mg/ml in
combination with 48 J of laser light, the bone loss
was significantly reduced in comparison with the
control group that did not receive PACT (Koemerik
et al., 2003). The biodistribution of topically applied
TBO on the gingival tissues was also examined. It
was demonstrated that the photosensitizer penetrated
throughout the epithelium. This fact may have very
advantageous clinical implications, as conventional
periodontal debridement fails to eliminate
pathogenic bacteria that are placed in the soft
tissues. In the study conducted by Fernandes et al.
(2009) PACT was applied as an adjunctive treatment
to scaling and root planning (SRP) to
immunosuppressed and non-immunosuppressed rats
with experimentally ligature-induced periodontitis in
mandibular molars. In rats that received PDT, the
periodontal ligament was found to be intact, with
parallel collagen fibers, lack of an inflammatory
infiltrate and thick alveolar bone, which was not the
case for rats treated only with SRP or SRP and TBO
with no irradiation (Fernandes et al., 2009).
The outcomes of in vivo studies are, however,
divergent. Some authors reported that adjunctive
PACT has a positive effect on periodontal
parameters contributing to the statistically
significant decrease of bleeding and probing depths
and gain of clinical attachment in comparison with
conventional treatment (SRP) (Braun et al., 2008).
In comparison, Polansky, Haas, Heschl and Wimmer
(2009) concluded, that PACT does not provide
additional benefits to conventional periodontal
treatment, although visibly larger reductions of
bleeding indices were seen among the patients that
received PACT than in the control group, however
these differences turned out to be statistically
insignificant (Polansky et al., 2009). Similar results
were obtained by other authors (Chondros et al.,
2009). The differences in the outcomes of in vitro
and in vivo studies indicate that more detailed
research is needed in this field.
2.3.4 Periimplantitis
Periimplantitis is an inflammatory condition that
affects soft and hard tissues surrounding an
osseointegrated dental implant and may lead to its
failure. The causative flora is similar to that one
responsible for the development of periodontal
disease (A. actinomycetemcomitans, P. gingivalis, P.
intermedia) (Takasaki et al., 2009). In an animal
split-mouth study, Shibli et al. (2006) compared
histometrically the outcomes of conventional
periimplantitis management (debridement + guided
bone regeneration) with those of conventional
management combined with TBO-mediated PACT
in dogs with ligature-induces periimplantitis. The
use of PACT resulted in a greater bone gain – the
mean percentage of re-osseointegration was 31-41%
for the test group and 0-14% for the control group
(Shibli et al. 2006). Haas, Baron, Doertbudak and
Watzek (2000) used TBO-mediated PACT in
combination with soft laser (906 nm) as an adjunct
to autogenous bone augmentation in 17 patients with
periimplantitis. The mean radiographic bone gain 4
months after the procedure was 2 mm (maxilla – 2.5
mm; mandible – 1.9 mm), what can be considered as
an excellent clinical outcome (Haas et al., 2000).
2.3.5 Soft Tissue Therapy
The effectiveness of PACT in the treatment of
recurrent herpes labialis (RHL) was also
investigated (Sperandio et al., 2009). Great clinical
outcomes were achieved for treating already
established RHL vesicles, compared to conventional
treatment with the use of antiviral compounds.
Patients reported an immediate pain relief after the
procedure. No recurrence was observed in a 6-month
period (Sperandio et al., 2009).
2.4 Towards Increased Effectiveness
The reduced susceptibility of P. gingivalis and other
periopathogens to PACT in vivo can be explained by
the fact, that periodontitis is a biofilm-related
APPLICATION OF THE PHOTODYNAMIC THERAPY IN MEDICINE AND DENTISTRY - Literature Review on
Photodynamic and Antimicrobial Photodynamic Therapy
193

infection. The penetration of the photosensitizer
solution into the bacterial biofilm is decreased in
comparison to the suspensions of bacteria used in in
vitro studies. Therefore, to enhance the effectiveness
of PACT, the development of novel delivery and
targeting approaches may be required. One strategy
to improve the targeting was proposed by Bhatti et
al. (2000). The authors used a conjugate of TBO and
murine monoclonal antibody (Ab-TBO) to
specifically target P. gingivalis in the presence of S.
sanguis or human gingival fibroblasts (HGFs) in
vitro. It was demonstrated that with the use of Ab-
TBO conjugate a high selectivity and efficiency in
the killing of P. gingivalis can be achieved. Such an
approach could enable the killing of important
periopathogens without collateral damage either to
host tissues or to the normal oral microflora.
3 CONCLUSIONS
PDT and PACT are non-invasive, relatively
inexpensive, painless to the patient with little or no
side-effects. The outcomes of presented in vitro and
in vivo studies are very promising. However, more
research is still needed in this field for optimizing
the protocol of clinical application, improving
specific targeting of tumor cells and bacteria and
introducing new groups of photosensitizers.
REFERENCES
Albandar, J. M., (2005). Epidemiology and risk factors of
periodontal disease. Dental Clinics of North America,
49, 517-532.
Bahrami, G., Vaeth, M., Kirkevang, L. L., Wenzel, A.,
Isidor, F., (2008). Risk factor for tooth loss in an adult
population: radiographic study. Journal of Clinical
Periodontology, 35, 1059-1065.
Bhatti, M., MacRobert, A., Henderson, B., Shepherd, P.,
Cridland, J., Wilson, M., (2000). Antibody-targeted
lethal photosensitization of Porphyromonas gingivalis.
Antimicrobial Agents and Chemotherapy, 44, 2615-
2618.
Bhatti, M., MacRobert, A., Henderson, B., Wilson, M.,
(2002). Exposure of Porphyromonas gingivalis to red
light in the presence of the light-activated
antimicrobial agent toluidine blue decreases
membrane fluidity. Current Microbiology, 45: 118-
122.
Bonsor, S. J., Nichol, R., Reid, T. M. S., Pearson, G. J.,
(2005). An alternative regimen for root canal
disinfection. British Dental Journal, 201, 101-105
Bonsor, S. J., Nichol, R., Reid, T. M. S., Pearson, G. J.,
(2006). Microbiological evaluation of photo-activated
disinfection in endodontics (An in vivo study). British
Dental Journal, 200: 337-341.
Braun, A., Dehn, C., Krause, F., Jepsen, S., (2008). Short-
term clinical effects of adjunctive antimicrobial
photodynamic therapy in periodontal treatment: a
randomized clinical trial. Journal of Clinical
Periodontology, 35: 877-884.
Burns, T., Wilson, M., Pearson, G. J., (1995). Effect of
dentine and collagen on the lethal photosensitization
of Streptococcus mutans. Caries Research, 29(3): 192-
197
Chan, Y., Lai, C. H., (2003). Bactericidal effects of
different laser wavelength on periodontopathic germs
in photodynamic therapy. Lasers in Medical Science,
18(1), 51-55.
Chondros, P., Nikolidakis, D., Christodoulides, N.,
Roessler, R., Gutknecht, N., Sculean, A., (2009).
Photodynamic therapy as adjunct to non-surgical
treatment in patients on periodontal maintenance: a
randomized controlled clinical trial. Lasers in Medical
Science, 24: 681-688.
Detert, J., Pischon, N., Burmester, G. R., Buttgereit, F.,
(2010). The association between rheumatoid arthritis
and periodontal disease. Arthritis Research &
Therapy, 12: 218-224.
Fernandes, L. A., de Almeida, J. M., Theodoro, L. H.,
Bosco, A. F., Nagata, M. J. H., Martins, T. M.,
Okamoto, T., Garcia, V. G., (2009). Treatment of
experimental periodontal disease by photodynamic
therapy in immunosprressed rats. Journal of Clinical
Periodontology, 36: 219-228.
Foschi, F., Fontana, C. R., Ruggiero, K., Riani, R., Vera,
A., Doukas, A. G., Pagonis, T. C., Kent, R.,
Stashenko, P. P., Soukos, N. S., (2007). Photodynamic
inactivation of Enterococcus faecalis in dental root
canals in vitro. Lasers in Surgery and Medicine, 39:
782-787.
Haas, R., Baron, M., Doertbudak, O., Watzek, G., (2000).
Lethal photosensitization, autogenous bone and e-
PTFE membrane for the treatment of peri-implantitis:
preliminary results. The International Journal of Oral
& Maxillofacial Implants, 15: 374-382.
Koemerik, N., Nakanishi, H., MacRobert, A. J.,
Henderson, B., Speight, P., Wilson, M., (2003). In
vivo killing of Porphyromonas gingivalis by toluidine
blue-mediated photosensitization in an animal model.
Antimicrobial Agents & Chemotherapy, 47: 932-940.
Lagervall, M., Jansson, L., Bergstroem, J., (2003).
Systemic disorders in patients with periodontal
disease. Journal of Clinical Periodontology, 30: 293-
299.
Lin, H. P., Chen, H. M., Yu, C. H., Yang, H., Wang, Y. P.,
Chiang, C. P., (2010). Topical photodynamic therapy
is very effective for oral verrucous hyperplasia and
oral erythroleukoplakia. Journal of Oral Pathology &
Medicine, 39: 624-630.
Matevski, D., Weersink, R., Tenenbaum, H. C., Wilson,
B., Ellen, R. P., Lepine, G., (2003). Lethal
photosensitization of periodontal pathogens be a red-
filtered Xenon lamp in vitro. Journal of Periodontal
Research, 38: 428-435.
BIODEVICES 2012 - International Conference on Biomedical Electronics and Devices
194

O’Neil, J. F., Hope, C. K., Wilson, M., (2002). Oral
bacteria in multispecies biofilms can be killed by red
light in the presence of toluidine blue. Lasers in
Surgery & Medicine, 31: 86-90.
Overholt, B. F., Wang, K. K., Burdick, J. S., Lightdale, C.
J., Kimmey, M., Nava, H. R., Sivak, M. V., Nishioka,
N., Barr, H., Marcon, N., Pedrosa, M., Bronner, M. P.,
Grace, M., Depot, M., (2007). Five-year efficacy and
safety of photodynamic therapy with Photofrin in
Barrett’s high grade dysplasia. Gastrointestinal
Endoscopy, 66: 460-468.
Polansky, R., Haas, M., Heschl, A., Wimmer, G., (2009).
Clinical effectiveness of photodynamic therapy in the
treatment of periodontitis. Journal of Clinical
Periodontology, 36: 575-580.
Seymour, R. A., Preshaw, P. M., Thomason, J. M., Ellis, J.
S., Steele, J. G., (2003). Cardiovascular diseases and
periodontology. Journal of Clinical Periodontology,
30: 279-292.
Shibli, A. J., Martins, M. C., Ribeiro, F. S., Garcia, V. G.,
Nociti, F. H. Jr, Marcantonio, E. Jr., (2006). Lethal
photosensitization and guided bone regeneration in
treatment of peri-implantitis: an experimental study in
dogs. Clinical Oral Implants Research, 17: 273-281.
Silbert, T. B. P., Milburn, G. J., Walsch, L., (2000).
Disinfection of root canals by laser dye
photosensitization. Journal of Dental Research, 79:
569.
Socransky, S. S., Haffajee, A. D., (2002). Dental biofilms:
difficult therapeutic targets. Periodontology 2000, 28,
12-55.
Soukos, N. S., Chen, P. S., Morris, J. T., Ruggiero, K.,
Abernethy, A. D., Som, S., Foschi, F., Doucette, S.,
Bammann, L. L., Fontana, C. R., Doukas, A. G.,
Stashenko, P. P., (2006). Photodynamic therapy for
endodontic disinfection. Journal of Endodontics, 32:
979-984.
Soukos, N. S., Goodson, J. M., (2011). Photodynamic
therapy in the control of oral biofilms. Periodontology
2000, 55(1), 143-166.
Sperandio, F. F., Marotti, J., Aranha, A. C., Eduardo, Cde
P., (2009). Photodynamic therapy for the treatment of
recurrent herpes labialis: preliminary results. General
Dentistry, 57: 415-419.
Spinola Ribeiro, A., Ribeiro Sales, P., Aparecida da Silva,
T., Alves Mesquita, R., (2010) A review of the
nonsurgical treatment of oral leukoplakia.
International Journal of Dentistry, (2010), Article ID
186018.
Stochel, G., Brindell, M., Macyk, W., Stasicka, Z.,
Szacilowski, K., (2009). Bioinorganic Photochemistry,
John Wiley & Sons
Takasaki, A. A., Aoki, A., Mizutani, K., Schwarz, F.,
Sculean, A., Wang C. Y., Koshy, G., Romanos, G.,
Ishikawa, I., Izumi, Y., (2009). Application of
antimicrobial photodynamic therapy in periodontal
and peri-implant diseases. Periodontology 2000,
51(1), 109-140.
Triesscheijn, M., Baas, P., Schellens, J. H., Stewart, F. A.,
(2006). Photodynamic therapy in oncology. The
Oncologist, 11, 1034-1044.
Usacheva, M. N., Teichert, M. C., Biel, M. A., (2001)
Comparison of the methylene blue and toluidine blue
photobacterial efficacy against gram-positive and
gram-negative microorganisms. Lasers in Surgery and
Medicine, 29: 165-173.
Williams, J. A., Pearson, G. J., Colles, M. J., Wilson, M.,
(2004).The photoactivated antibacterial action of
toluidine blue O in a collagen matrix and in carious
dentine.Caries Research, 38(6): 530-536.
Xu, Y., Young, M., Battaglino, R., Leslie, M., Fontana,
C., Pagonis, T. C., Kent, R., Soukos, N. S., (2009).
Endodontic antimicrobial photodynamic therapy:
safety assessment in mammalian cell cultures. Journal
of Endodontics, 35, 1567-1572.
APPLICATION OF THE PHOTODYNAMIC THERAPY IN MEDICINE AND DENTISTRY - Literature Review on
Photodynamic and Antimicrobial Photodynamic Therapy
195
