
A SECURE PERSONAL HEALTH RECORD REPOSITORY
Tiago Pedrosa
1,3
, Rui Pedro Lopes
1,3
, Jo˜ao C. Santos
2,3
, Carlos Costa
3
and Jos´e Lu´ıs Oliveira
3
1
Department of Informatics and Communication, Polytechnic Institute of Braganc¸a, Braganc¸a, Portugal
2
Department of Electrotechnics Engineering, Coimbra Institute of Engineering, Coimbra, Portugal
3
IEETA, University of Aveiro, Aveiro, Portugal
Keywords:
EHR, PHR, Security, Repositories, Indexing.
Abstract:
Due to strict regulatory, ethic and legal issues, Electronic Health Record (EHR) systems have been mainly de-
ployed in federated health care scenarios. This situation have been hindering the wide adoption of EHRs, con-
tributing to delaying the establishment of a competitive market where contributions from different providers
could take full advantage of information exchange and regular practitioners’ collaboration. Moreover, with
the increasing awareness of medical subjects, patients are demanding more control over their own personal
data - Personal Health Record (PHR). This paper presents a secure PHR repository which access is controlled
through the joint use of a Virtual Health Card Service (VHCS) and an access Broker. This solution can be
deployed in any public or private storage service since it behaves as a sandbox system which access pol-
icy is defined externally. To assure a friendly query-retrieve interaction the whole repository is indexed, and
separated clinical events are kept independently to increase the efficiency of cipher and encipher algorithms.
1 INTRODUCTION
Electronic Health Records (EHR) can be defined as
digital record that aggregate all data acquired during
patient care on the healthcare system. Soon captured
the attention of practitioners, policy makers and pa-
tients since they are essential to better clinical ser-
vices integration and to health information sharing.
However, EHRs have mainly been deployed in more
or less enclosed health care scenarios. Strict regula-
tory, ethic and legal constrains (Hodge Jr et al., 1999;
Shabo, 2006), have been hindering the wide adoption
of EHRs, contributing to delaying the establishment
of a competitive market where different providers
could take full advantage of information exchange
and regular practitioners’ collaboration. Moreover
patients are demanding more control over their own
personal data.
To cope with these new user requirements, sev-
eral Personal Health Record (PHR) solutions have
been developed, enabling users to keep record of their
medical data. Examples of such system are, for in-
stance, Google Health, Microsoft HealthVault and
Dossia (Eysenbach, 2008). These web-based PHRs
are mostly based on a central repository and on a set
of core features that, in some cases, can be extended
by external third-party services. A major difference
between EHR and PHR is related to the responsibil-
ity for maintaining the information and for specify-
ing the access control policy. In the former model the
accountable are the healthcare institutions and their
professionals, while in the PHR it is the patient that
owns this responsibility. Despite this typical opera-
tional model, several PHR can also be automatically
populated from systems where the data is generated.
However, for this scenario to be possible, it will be
necessary that EHR systems generate the adequate re-
ports of clinical events and that could interact directly
with those external PHR systems.
The exchange and storage of health information is
a major security challenge, mainly its disruption may
compromise seriously personal privacy. The idea of
having an enterprise with access to all health infor-
mation of a citizen is unlikely to occur because the
risk of information discloser is higher and more dis-
astrous than in a scattered scenario. Moreover, the
Big Brother scenario also appears whenever central-
ization is suggested, despite of the guardian of the in-
formation is an enterprise or the government, and this
vision also slows down the adoption of the different
solutions. This paper presents a secure PHR reposi-
tory where access is controlled through the joint use
of a Virtual Health Card Service (VHCS) and an ac-
cess Broker. Several security features were decou-
pled along both components to assure a double con-
sensus when manipulating the data behind. It can
243
Pedrosa T., Pedro Lopes R., C. Santos J., Costa C. and Luis Oliveira J..
A SECURE PERSONAL HEALTH RECORD REPOSITORY.
DOI: 10.5220/0003781802430248
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2012), pages 243-248
ISBN: 978-989-8425-88-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

be deployed in any public or private storage service
since it acts as a sandbox system which access pol-
icy is defined externally. To assure an efficient user
interface, the whole repository is indexed and sepa-
rate clinical events are kept independently to increase
the efficiency of cipher-decipher and query-retrieve
algorithms. This strategy enables the citizen to safely
deposit information on the PHR repository, since not
even the repository administrator can discloser it. Un-
der an explicit owner’s authorization, the Broker may
enable other services to access or upload new data in
the PHR.
2 BACKGROUND
EHRs and PHRs can share the record architecture,
but they differ in the data custody ownership and
the management responsibilities. The PHR can be
a self-contained registry, maintained and controlled
by the subject of care, based on a specific portable
data storage device, some entry in a web service
provider or even a component of an Integrated Care
EHR (ICEHR). In the EHR case healthcare providers
are responsible for its maintenance. Different types
of EHR exist, but one that is more promising is the
ICEHR, that acts as a repository of all the health in-
formation of a patient during is life time (ISO/TC 215,
2005).
For achieving a functional EHR, interoperabil-
ity between producers and consumers of information
is needed. Standardization appears as the solution
to enable the communication between different sys-
tems. These efforts can be divided in two main areas:
the communication standard and the document stan-
dard (Sunyaev et al., 2008). The former refers to how
systems can communicate with each other and the lat-
ter describes how information is stored to ensure a
correct interpretation by other systems. The results
of researching the available standards has evidenced
interoperability barriers.
Diverse documents standards exists, as HL7
specifies the Clinical Document Architecture
(CDA) (Dolin et al., 2006), ASTM the Continuity of
Care Document (CCD) and the Continuity of Care
Record (CCR) (Ferranti et al., 2006) that are con-
strains over the CDA and the OpenEHR (OpenEHR,
2007) uses archetypes for defining the record struc-
ture. Those formats have is the ability to extract a
record or a subset of a record in a XML format where
the DTD defines the record structure. This provides
an easier way to export data from one system to
another.
The increased mobility and free market in health
care provisioning pushed the information to be scat-
tered through the providers. A solution can be the use
of an integrated access mechanism to the disperse in-
formation. The integrator has to know the location of
the information and how to retrieve it in a secure way.
This linkage information can be stored in the integra-
tor database, or to an extend electronic health card
to support that service (Ferreira Pol´onia et al., 2005;
Costa et al., 2003).
In a wider concept of mobility it is not feasible
that all worldwide patients will have the same type
of card. Another open question is that services and
users can’t make use of the information of the patient
if the card is not present. To overcome that difficulties
was proposed a Service Oriented Architecture (SOA),
making use of a Virtual Health Card Service (VHCS),
that mimics the behavior of the physical card (Pedrosa
et al., 2009). Combined with a centralized access
control mechanism that implements the intent consent
policy and with a proxy. The proxy uses the informa-
tion inside a VHC, namely the credentials of the pa-
tient to the repository, the access policy to apply to the
requester user, and the URLs to the scattered reposi-
tories to retrieve the information and create a unique
EHR read-only view (Pedrosa et al., 2010).
The tight regulatory framework that health care
services have to comply, limits their will to give ac-
cess to their systems. Therefore it will limit the use
of the previous solution. A solution that appears is
centralization of the information in one repository.
The EHR healthcare system will create and deposit
on the repository the information related to the pa-
tient attendance. If all systems this procedure, the in-
formation in the repository will enable the creation of
the ICEHR. PHRs make use of services for importing
information, but as the record management is done
by the patient, medical staff tends to question the in-
tegrity of the data.
One of the main concerns about PHR is its privacy,
as the data inside any healthcare provider allows ac-
cess to any PHR, it can potentially open the system to
large-scale disclosures (Ray and Wimalasiri, 2006).
3 PROPOSED SOLUTION
The proposed solution mimics the process for storing
safe deposit boxes inside banks. A procurator is re-
sponsible for managing the deposited goods, which,
in our case, correspond to the information stored in
health records. The citizen will authorize the procu-
rator to deposit and withdraw information from the
safe deposit to answer the needs of third party ac-
tors, previously approved by the citizen. An addi-
HEALTHINF 2012 - International Conference on Health Informatics
244
tional level of protection is added, by defining several
small safes inside a larger safe. The keys for those
small safes will be stored in a different and secure
place (the VHCS), so the information will not be visi-
ble to the bank or to the procurator. When a requester
needs access to the information, he will ask the procu-
rator to provide the data and for that he also provides
a safe box that can only be opened by the procura-
tor, through the keys stored in the VHCS. The procu-
rator, after consulting the privileges of the requester,
will unlock the safe and retrieve the small safe deposit
boxes that contain the required information and tem-
porarily store it in a secure place. The citizen’s safes
will be opened and, according to the requester privi-
leges, the information will be copied to his requesting
safe, which will be then returned to him.
For depositing information, the requester asks the
procurator to bring a safe that will be used to put the
information in. Then, the procurator will take the safe
back, and store it in the citizen’s larger safe deposit
box inside the bank. This approach means that neither
the bank nor the procurator can access the informa-
tion inside the safe, but allows him to manage it. To
get into the details of the architecture, we provide an
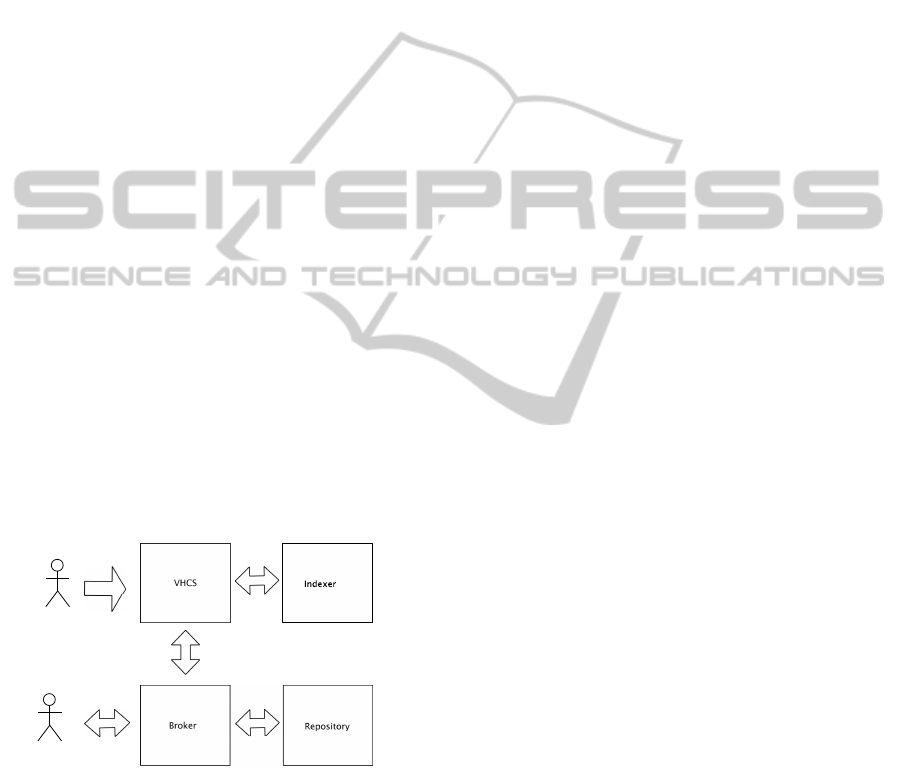
overviewof the actors and services involved. The Vir-
tual Health Card Service (VHCS) represent the secure
key deposit; the Broker represents the procurator; the
Repository represent the bank; and the Indexer will
enable a selective retrieval from the Repository (Fig-
ure 1). We use a Service Oriented Architecture that
makes use of SSL certificates, signed by a Certificate
Authority (CA), to establish confidence between the
actors and software components. The record is pop-
User/Service
Patient
Figure 1: Wide overview of several actors and services.
ulated with information resulting from several con-
tributions, associated with the different actors, when
they upload the information resultant from medical
activity. All the contributions are stored and ciphered
individually inside the repository. In the request pro-
cess these contributions are retrieved from the reposi-
tory, deciphered, reassembled and ciphered using the
requester key. This assures that the information in
transit is always encrypted and that the only service
that can read the information is the VHCS. In the
store procedure, the information generated by a med-
ical exam, for example, is ciphered using the patient’s
public key and stored in the VHCS. When sending
this information to the Repository, it is ciphered with
the public key of the receiver.
The Repository is a storage service that enables
a client to request or to store bulks of data associ-
ated to a specific identifier. The identifier is unique
per patient and it is used to associate the information
with a specific patient. The only way to associate the
stored information to a specific patient is through the
VHCS. The Broker is the only service that can con-
tact directly the repository. It acts as a middleman
between the users and services that need access to the
repository. It has to validate the users and fulfill their
requests through the VHCS when needed.
The creation of a Virtual Health Card by the pa-
tient is the first step to enable the use of a secure
PHR repository. This phase is composed by the pa-
tient credentials generation (public/private key pair),
the initialization of a repository i.e. configuring the
repository end point, and the credentials that will al-
low the broker to query that Virtual Health Card. The
users and services that want to make use of the patient
information on the repository or wants to save new in-
formation will use the services provided by the Bro-
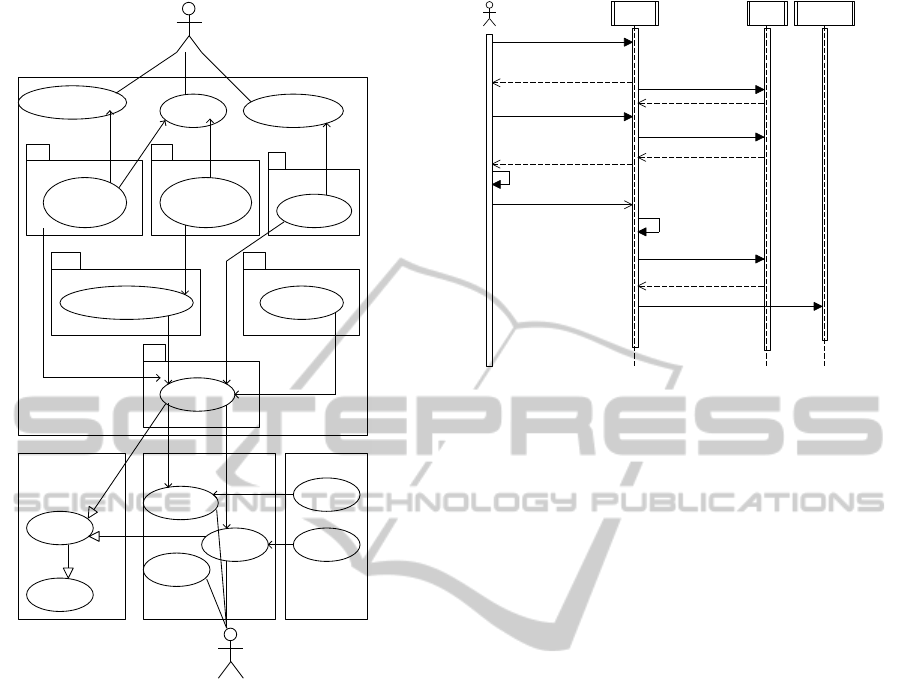
ker (Figure 2). The VHCS components are directly
related to patient functions, supported by the follow-
ing components: the Patient Credential, the Access
Control and Repository Management. It also provides
functions and interfaces to be used by the Broker.
The Patient Credential manage public and private
patient keys. The Cryptographic component is re-
sponsible of manipulating those keys in a secure way
and it also provides cryptographicfunctions to manip-
ulate the ciphered block enforcing that the private key
never leaves the VHCS. The Access Control compo-
nent stores the policy defined by the patient to reg-
ulate the access of the users and services that want
to gain access to the repository. It stores the public
key of the user/service and the type of the access he
has to the information. The Repository Management
component is responsible for managing the Reposi-
tory store and the credentials required to gain access.
The Reassemble component provides a way to ag-
gregate the requested individual contributionsin a sin-
gle one. During this phase the access control is en-
forced by the discard of information that the request-
ing user does not have access.
The Broker interface component provides access
to functions that the Broker will need to perform. It
enables the Broker to check the access policy, to know
what Repository to contact and the required creden-
A SECURE PERSONAL HEALTH RECORD REPOSITORY
245
Repository Management
Access Control
Cryptographic Component
Patient Credentials
Broker Interface
Reassembler
Backend
Indexer
Services
Indexer
EHR reassembler
Manage Repostiories
BrokerServices
Retrieve
Store
Repository
Broker
Patient Credentials
Management
Crytographic Functionality
Repository
Credentials
Management
Policy
Management
VHCS
Store Data
Request Data
Registry
User/Service
Define Access Policy
Create VHC
Patient
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Uses
Figure 2: Interaction between users and services compo-
nents.
tials. It also enables the Broker to request the public
key of a patient and invokes the ciphering/deciphering
of data through the Cryptography component using
the patient keys.
The Broker components are directly related with
actions that other users/services perform on the pa-
tient repository. First, the users/services have to cre-
ate an account on the Broker, which will check for the
validity of the CA signature, and stores the public key
of the requester. This registry on the Broker is not
only used for users/services authentication. A patient
can also use this to retrieve the public key of users or
services that may want to use the VHCS access con-
trol component. The Broker makes use of the VHCS
capabilities through the broker interface, and together
they enable storing and retrieving of information to
and from the Repository. The Broker manipulates the
information using a closed envelope concept as the
information is always ciphered to the receiver, to the
patient or to user/service that request information.
Figure 3 explains how an external service or user
Repos
VHCS
Broker
Ac t o r
7: SendPatientPublicKey
6: ASKPatientPublicKey
9: CypherForPatient
8: SendPatientPublicKey
5: ASKPatientPublicKey
13: SendReposCredentials
11: CypherRecord
4: Check ok
14: Store
12: AskRepoCredentials
3: CheckPolicy
2: Check ok
10: SavePatinetData
1: Login
Figure 3: Storing information on repository.
can store information on the repository. When a
user/service wants to save new information of a pa-
tient on the Repository it contacts the Broker. First
it challenges the login and checks the authorization
policy on the VHCS. After success, the actor will
ask the public key of the patient. To be able to an-
swer, the Broker requests the patient public key to the
VHCS and forwards it to the user/service. The later
ciphers the information with the given public key and
sends the result back to the Broker. The Broker ci-
phers again using its private key and requests the pa-
tient repository information to the VHCS. Finally, it
uses this information to store the information on the
Repository.
The first ciphering procedure ensures that the in-
formation sent to the Broker can only by read by us-
ing the patient’s private key, stored on the VHCS. The
second ciphering forces the Broker to interact with the
information stored on the inside the repository. The
double ciphering obliges the Broker and VHCS to co-
operate in order to manipulate the data.
Sometimes, the requester only needs access to a
subset of information, relieving the burden and the
overload of processing and sending the full data set.
To optimize this process, an indexing service is pro-
vided, enabling some search capabilities over the pa-
tient repository. The proposed architecture contem-
plates an independent indexing service that stores
searchable information. This Indexer accepts queries
and returns PHR repository entries that fulfill the
request, avoiding unnecessary manipulation of data
pieces.
Every time a new piece of patient clinical data is
archived, the Indexer securely stores a set of associ-
ated meta-information,including the eventtype, some
coded clinical details, creation date, producer infor-
HEALTHINF 2012 - International Conference on Health Informatics
246

mation and repository data location. Every patient
has its own set of index files that are ciphered with
his credentials. When creating new data in the Repos-
itory, the actor must create indexing information and
cipher it with patient public key. Both information
blocks, patient data and index metadata, are sent to
the Broker. Here, the index is delivered to Indexer
Service via VHCS and the patient record is stored in
the Repository.
The Index service is only accessible through
VHCS, which controls all access to searching oper-
ations. When an actor needs to search information,
it requests the patient public key to encrypt the query
that is sent to Broker (Figure 4). This provider will
check the actor access policies before forwarding the
request to the VHCS. Here, the query is decrypted
and injected in the Index engine. The query results,
i.e. the data repository references, are returned to the
Broker via VHCS. The Broker then gets the patient
repository information and uses it to retrieve the con-
tributions from the Repository. Next it will decipher
it using Broker’s private key and send the result to
the VHCS along with the public key of the requester.
The VHCS deciphers the received information using
the patient private key, it reassembles the various con-
tributions and ciphers it using the public key of the
requester. In the end, the result will be sent back to
the Broker, which forwards the data to the requester.
The information detained by Indexer module is only
Indexer
Repos
VHCS
Bro ker
Ac tor
13: DecipherQuery
8: CipherQuery
7: SendPatientPublicKey
5: SendPatientPublicKey
6: SendPatientPublicKey
4: ASKPatientPublicKey
3: ASKPatientPublicKey
16: SendReferences
15: SendReferences
14: GetReferences
12: GetReferences
20: SendPatiendRecord
19: RetrieveData
11: Chec k ok
24: SendRecordCypherRequester
18: SendReposCredentials
23: Reassembler
17: AskRepoCredentials
22: DecipherRecord
10: CheckPolicy
25: SendRecordCypherRequester
2: Check ok
21: DecipherRecord
9: GetSelectPatinetData
1: L ogin
Figure 4: Selective Retrieving from repository.
readable by VHCS because it is ciphered with the pa-
tient public key. Moreover, the information stored in
the Repository and Indexer can only be related by a
third secure entity – the VHCS. This approach enables
search operations over a ciphered repository, with-
out disclosing patient information during the process.
The Broker cannot use actor queries information or
Indexer results to extrapolate what kind of data exists
inside patient Repository.
This approach grants that the information is al-
ways transmitted in a closed envelope concept and
that the only actor that can read the information is the
requester. Moreover, the Broker and the VHCS have
to work together to gain access to the information on
the repository.
Although the record can follow virtually any data
format, for our proposal, we have chosen XML. Since
the record format is transparent in terms of ciphering
and storage, the producers and consumers only have
to agree on a common format for enabling collabo-
ration in the creation of the PHR. If not, they must
at least support interchangeable schemas to enable a
common understandable format. The only component
that has to be defined according to a specific format is
the re-assembler in the VHCS.
The use of XML allows saving the record struc-
ture as well the data. The structure can provide in-
formation about the type of contribution that exists on
the record, even when the data is ciphered. It is true
that the data itself could be protected, but a specific
structure for saving a type of a lab test result or medi-
cal procedure can reveal, the kind of test or procedure
the patient made. This would allow guessing patient
pathologies and diseases.
4 IMPLEMENTATION
The prototype is being developed in Java EE 6), over
Glassfish application server. All components are de-
ployed as Enterprise Java Beans. The interfaces be-
tween the components will be implemented via web-
services over HTTPS. The client authentication is
configured and requested in the application server,
being transparent to the developer. The OpenSSL
was chosen as public key cryptographic framework
and as digital credential management (users and ser-
vices) platform it was used the OpenCA bundle. A
Crypto API (Legion of the Bouncy Castle, 2010) is
used to manipulate certificates and for cryptographic
functions.
The Repository Service is a file system oriented
storage structure, using a unique subdirectory per pa-
tient, each with a random identification number. Each
patient directory stores the ciphered clinical records
submitted to Repository Service by the Broker. Each
structured record file receives a sequence number that
A SECURE PERSONAL HEALTH RECORD REPOSITORY
247

unequivocally relates it to the patient index informa-
tion stored in Index system.
To test this prototype, a Google Health account
is being used to create a test record. Using the Data
Exchange tool (Mount Tabor, 2010) the record is ex-
ported to a file. That file is uploaded to our Repository
via our Broker to test the solution. The inverse pro-
cess will be also tested.
5 CONCLUSIONS
Personal Health Records have recently appeared as a
solution that allows patients to keep track of their own
clinical history. With the increasing availability of
medical information in the Internet, citizens now have
access to a tremendous amount of data sources, which
provide information such as diseases symptoms, di-
agnostics, treatments, drugs, physicians, and many
others. This situation is leading to better informed
citizens, but with much more complex requirements
– health information gathering and privacy assurance
are two critical examples.
This paper presents a secure PHR repository that
combines the notion of a safe deposit with the ability
to securely share clinical data. This particular feature
enables the integration with external services upon
an explicit authorization by the patient. In this way,
much of the data that is uploaded in the repository
can come directly from EHR systems, which allevi-
ates the user from the burden of record updating. The
aggregation of all these contributions enables a com-
prehensive overview of the patient medical status and
relevant historic information. Moreover, patient’s per-
sonal registries can also be kept in this system.
To assure security requirements, the information
in transit is always ciphered. On storage operations,
the system uses the patient public key and on retrieval
it applies the public key of the requester. In the store
procedure a second entity, the Broker, will also cipher
the data before storing it in the repository. The only
component that can read the sandbox record is a vir-
tual card component (VHCS), but without access to
its content. Despite holding the repository credentials
and the private key of the patient to decipher the data,
the VHCS would need that the Brokeralso retrieve the
data from repository. The proposed solution provides
a search capability through an indexing service that
maintains links to metadata of all the PHR contribu-
tions, allowing a selective retrieve from the repository
whenever a query is executed.
REFERENCES
Costa, C., Oliveira, J., Silva, A., et al. (2003). A new con-
cept for an integrated healthcare access model. The
new navigators: from professionals to patients: pro-
ceedings of MIE2003, page 101.
Dolin, R., Alschuler, L., Boyer, S., Beebe, C., Behlen, F.,
Biron, P., and Shabo Shvo, A. (2006). Hl7 clinical
document architecture, release 2. Journal of the Amer-
ican Medical Informatics Association, 13(1):30.
Eysenbach, G. (2008). Medicine 2.0: social networking,
collaboration, participation, apomediation, and open-
ness. Journal of Medical Internet Research, 10(3).
Ferranti, J., Musser, R., Kawamoto, K., and Hammond, W.
(2006). The clinical document architecture and the
continuity of care record. British Medical Journal,
13(3):245.
Ferreira Pol´onia, D., Costa, C., and Oliveira, J. (2005). Ar-
chitecture evaluation for the implementation of a re-
gional integrated electronic health record. In Press, I.,
editor, Proceedings of MIE2005. IOS Press.
Hodge Jr, J., Gostin, L., and Jacobson, P. (1999). Legal
issues concerning electronic health information: pri-
vacy, quality, and liability. Jama, 282(15):1466.
ISO/TC 215 (2005). Health informatics - electronic
health record - definition, scope, and context - iso/tr
20514:2005(e). Technical report, ISO.
Legion of the Bouncy Castle (2010). The Legion of
the Bouncy Castle. http://www.bouncycastle.org/
java.html, Last Checked: 1 June 2010.
Mount Tabor (2010). Mount tabor and google
health. http://www.mttaboros.com/GHPartners.html,
Last Checked: 1 June 2010.
OpenEHR (2007). Introducing openehr - revision 1.1. Tech-
nical report, OpenEHR.
Pedrosa, T., Costa, C., Lopes, R., and Oliveira, J. (2009).
Virtual health card system. Inforum 2009.
Pedrosa, T., Lopes, R., Santos, J., Costa, C., and Oliveira,
J. (2010). Towards an EHR architecture for mobile
citizens. In HealthInf 2010 Proccedings.
Ray, P. and Wimalasiri, J. (2006). The need for technical
solutions for maintaining the privacy of EHR. In IEEE
Engineering in Medicine and Biology Society.
Shabo, A. (2006). A global socio-economic-medico-legal
model for the sustainability of longitudinal electronic
health records-part 2. Methods of information in
medicine, 45(3):240.
Sunyaev, A., Leimeister, J., Schweiger, A., and Krcmar, H.
(2008). It-standards and standardization approaches in
healthcare. Encyclopedia of Healthcare Information
Systems.
HEALTHINF 2012 - International Conference on Health Informatics
248
