
AN IMMERSIVE VIRTUAL ENVIRONMENT FOR PHANTOM LIMB
PAIN REHABILITATION
Steve Pettifer
1
, Toby Howard
1
, Ben Blundell
1
, David Edwards
1
and Ilan Lieberman
2
1
School of Computer Science, The University of Manchester, Oxford Road, Manchester, M13 9PL, U.K.
2
University Hospital of South Manchester NHS Foundation Trust, Wythenshawe Hospital,
Southmoor Road, Manchester, M23 9LT, U.K.
Keywords:
Virtual Environments, Phantom Limb Pain.
Abstract:
Phantom Limb Pain is a debilitating condition that affects a significant percentage of patients after loss of
an arm or leg. These patients experience chronic pain and other unpleasant sensations in the missing limb,
and the pain resists treatment. Previous research has demonstrated that pain levels can be reduced in some
patients when they are immersed in a virtual environment that presents a 3D computer graphics visualisation
of their missing limb, the movements of which are controlled by sensors attached to the remaining limb. In
this paper we describe a novel approach to the implementation of such a system, using the Kinect game device
for limb motion tracking, in conjunction with wireless motion sensors worn by the patient. We present some
preliminary, but very encouraging, results based on an informal trial with a patient.
1 INTRODUCTION
We present an interactive wireless computer graph-
ics virtual environment (VE) designed to form part of
a treatment regime for amputee patients who suffer
from the debilitating effects of Phantom Limb Pain.
We implement the VE using the Kinect motion track-
ing device, wireless inertial sensors, OpenGL, and the
Cinder C++ library. In this paper we begin with an
introduction to the condition of Phantom Limb Pain,
and then present an overview our our prototype VE,
presenting some preliminary results and observations
from an informal trial with an amputee patient.
2 BACKGROUND
Following the loss of a limb, whether by surgery
or trauma, it is common for amputees to report the
sensation that their missing limb remains attached to
their body (one of the earliest reports being(Mitchell,
1872)). Sometimes under volitional control, while
in other cases frozen in a specific position, these so-
called ‘phantom limbs’ often present such a vivid il-
lusion that it takes conscious effort for the amputee to
adjust to not using the missing limb as part of their
everyday lives (Jensen and Nikolajsen, 1994). Many
amputees experience some form of Phantom Limb
Pain (PLP), and although studies vary in their meth-
ods of classifying PLP, it is generally accepted that
between 60% and 85% of amputees suffer from some
degree of PLP (Kooijman et al., 2000; Desmond and
MacLachlan, 2006; Ephraim et al., 2005; Ehde et al.,
2000; Black et al., 2009).
The manifestation of PLP varies according to the
individual, including feelings of clenching, burning,
stabbing, severe itching and ‘electric shocks’, which
are often associated with a sense that the phantom
limb is contorted or misshapen in some way (Flor,
2002). Severe PLP (which occurs in around 25%
of sufferers) has been shown to cause societal with-
drawal for extended periods (Sherman et al., 1984),
and amputees with PLP are less likely to use a pros-
thetic limb, which often restricts their normal activi-
ties (Dolezal et al., 1998), and they are prone to de-
pression (Murray, 2005). According to the former Na-
tional Amputee Statistical Database (now ()limbless),
each year in the UK there are 5,500 new referrals to
prosthetic service centres, and 62,000 prosthesis users
in total (NASDAB, 2002). The number of amputees
worldwide is not reliably known, but studies in indi-
vidual countries suggest a figure well in the millions
(for example, (Zeigler-Graham et al., 2008) report
1.7 million amputees in the USA alone).
It was originally thought that PLP was caused by
nerve and tissue damage at the site of the amputation,
426
Pettifer S., Howard T., Blundell B., Edwards D. and Lieberman I..
AN IMMERSIVE VIRTUAL ENVIRONMENT FOR PHANTOM LIMB PAIN REHABILITATION.
DOI: 10.5220/0003831704260433
In Proceedings of the International Conference on Computer Graphics Theory and Applications (GRAPP-2012), pages 426-433
ISBN: 978-989-8565-02-0
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

and was therefore neuropathic pain, much the same
as that caused by a burn or a cut. However PLP has
proved resistant to the traditional range of pharma-
ceutical e.g.(Bone et al., 2002), surgical, and psycho-
logical pain management techniques (Kooijman et al.,
2000). Coupled with the realisation that children born
with missing limbs (where the problem is congenital
rather than caused by trauma) may also suffer from
PLP, this led to a hypothesis that the brain is in some
sense ‘hard-wired’ to expect signals from four limbs,
and that PLP results from a mismatch between this
mental template and the signals being generated by
the body itself (Flor et al., 1995; Borsook et al., 1998;
McCabe et al., 2005).
2.1 Visual Therapy
In 1996, psychologist V. K. Ramachandran devised an
experiment using a ‘mirror box’ (Ramachandran and
Rogers-Ramachandran, 1996) that allowed amputees
to view a reflection of their anatomical limb in the
visual space occupied by their phantom limb. He re-
ported that the mirror box induced vivid sensations of
movements originating from patients’ phantom limbs,
and in some cases relieved their PLP. Since then, oth-
ers have experimented with alternative visual thera-
pies such as the use of video e.g. (Giraux and Sirigu,
2003) or transcranial direct current stimulation e.g.
(Soler et al., 2010) with comparable results.
Hypothesising that interactive visual therapies
may work in similar ways to Ramachandran’s box,
around 2006 a number of research groups indepen-
dently began investigating the use of synthetic com-
puter graphics and virtual environments as a means
of reproducing the positive effects of the mirror box,
but without its physical limitations. MacLachlan’s
group developed an ‘augmented mirror box’ system
in which a data-glove worn on the amputee’s remain-
ing anatomical limb was used to track hand movement
and finger flexion (Desmond et al., 2006). This was
used to control the movement of a synthetic repre-
sentation of their phantom limb which was displayed
on a flat screen that replaced the mirror box’s mir-
ror. The limb could be customised in detail to reflect
any perceived distortions or contortions experienced
by the user. Of the three participants in the study,
two reported an intensification of their phantom ex-
perience, one reported gaining increased control over
their phantom fingers, and one reported a reduction
in their phantom pain. (Cole et al., 2009) took a dif-
ferent approach, instrumenting the stump of the af-
fected limb itself, and tracking its movement in order
to control the virtual representation. From a cohort of
seven upper limb and seven lower limb amputees, five
subjects in each group reported some control over the
movement of their phantom limb, and reported reduc-
tions in their PLP.
Our own previous work (Murray et al., 2006c;
Murray et al., 2010; Murray et al., 2005; Murray
et al., 2006c; Murray et al., 2006b; Murray et al.,
2007b; Murray et al., 2007a) like MacLachlan’s sys-
tem, tracked the movement of the anatomical limb
using a data-glove, transposing this motion to the
computer-generated image of a virtual limb. Unlike
MacLachlan, our system was a fully immersive en-
vironment, presented to the user via a tracked, head-
mounted display. In a small-scale trial, five partici-
pants whose PLP had resisted all other forms of treat-
ment used our system on a weekly basis; four reported
tangible reduction in their pain levels; two found they
gained some control over their phantom limb’s posi-
tion, being able to manoeuvre it into a more comfort-
able state; and one found that they were even able to
exercise some control over the stump of their ampu-
tated limb, which had previously been paralysed for
over twelve years.
In what, for a clinical application, would be con-
sidered very small-scale trials, all three approaches
demonstrated some success in allowing some (but no-
tably, not all) of the participants to gain a degree of
agency over their phantom limb and a measurable re-
duction in their pain levels. Given such small studies,
it is clearly premature to make any profound claims
about the effectiveness of the therapies. However, at
the same time, it is difficult to ignore the potential
of this approach as a non-invasive mechanism for re-
ducing the considerable suffering of millions of am-
putees.
2.2 The Potential of Virtual
Environments for Treating PLP
Two recent reviews of the use of virtual reality for
pain control cautiously conclude that virtual environ-
ment ‘distraction may be a useful tool for clinicians
who work with a variety of pain problems’ (Mal-
loy and Milling, 2010) and that ‘VR [Virtual Real-
ity] is emerging as both a viable first-line interven-
tion and as an adjunctive therapy to pharmacologic
agents’ (Mahrer and Gold, 2009). A further system-
atic review, which includes the use of mirror therapy
for the treatment of Chronic Regional Pain Syndrome
(a phenomenon thought to have similar causes to PLP
(Sato et al., 2010)) finds that there is value in such an
approach for the treatment of upper limb pain (Ezen-
dam et al., 2009). It must be noted that none of these
reviews specifically address the use of virtual reality
as a therapy for PLP: Mahrer and Gold and Malloy
AN IMMERSIVE VIRTUAL ENVIRONMENT FOR PHANTOM LIMB PAIN REHABILITATION
427

et al. examine pain caused by physical trauma such
as burns or surgery, whereas Ezendam et al. examine
only the reduction in pain as a result of the use of a
physical mirror box. We hypothesise, however, that
since visual therapies can be shown to improve PLP,
and that synthetic computer graphics can be used to
create illusions that reduce pain, the virtual environ-
ment approach to PLP reduction is a worthwhile av-
enue of research.
All three studies emphasise the need for further
work to better understand these effects. Mahrer et
al. highlight the need for ‘greater scientific rigor, in-
creased sample sizes, sound methodology, and in-
creased attention to individual user characteristics’
(Mahrer and Gold, 2009) in future studies. Meeting
such criteria using the systems described previously,
however, is likely to present a significant practical
challenge: all three systems were built using bespoke
hardware and software, making them difficult to repli-
cate in order to scale up to the kind of large scale trials
necessary to clinically validate their use as effective
therapies. In our own case it rapidly became impossi-
ble to source replacement parts for the specialist com-
ponents as they developed faults (suppliers of virtual
reality equipment are notoriously transient), and the
only existing installation of our system became unus-
able.
Since these initial trials, however, there have
been dramatic advances in computer graphics and re-
lated technologies: wearable displays, unencumbered
tracking devices and powerful 3D graphics engines
are now available as off-the-shelf consumer goods for
PCs, games consoles and home entertainment sys-
tems. Although these devices are in some cases of
lower quality than their specialist counterparts, be-
cause they are designed for general consumer use they
are more robust, cheaper and more easily available.
Driven by the demands of the computer games and
entertainment market, it seems likely that the quality
of these devices is only set to improve, and that their
future availability is essentially guaranteed. For ex-
ample, several groups (Calderwood et al., 2009; Lee,
2008; Scherfgen and Herpers, 2009; Sko and Gardner,
2009) have implemented virtual environments using
the Nintendo Wii (Nintendo Wii, 2011).
With the aim of producing a system that could
easily be replicated in order to support large-scale
clinical trials, we embarked upon a project to re-
produce our previous experimental setup using only
consumer-grade hardware. The remainder of this pa-
per describes this system, which we call ‘PLP2’.
3 SYSTEM DESIGN AND
IMPLEMENTATION
Our previous system used electromagnetic tracking,
with wired sensors attached the patient’s head and
anatomical limb. While providing reasonably accu-
rate absolute six degrees-of-freedom (DOF) tracking
and thus needing no calibration as such, these devices
required cumbersome wiring, and were also sensi-
tive to metal objects and electrical cabling which dis-
torted the tracking space, making finding a location
to carry out experiments difficult. Equipping the pa-
tient with the sensors required specialist training, and
patients needed careful supervision during their ses-
sions to avoid becoming entangled in the numerous
cables. With the exception of the video feed, our
new system requires no cables and is not sensitive to
metal/electricity in the environment.
The PLP2 system engages the patient in gameplay,
as shown in Figure 1. There are two games, both of
which aim simply to give the patient a purpose to en-
gage with the environment in a way that causes them
to move their virtual limb. In both scenarios, the pa-
tient remains standing but is able to turn around and
has space to move a few steps in any direction. In
the ball-following game, the patient uses their virtual
limb to track the position of a ball, which moves ran-
domly around their position while remaining ‘within
reach’). In the tic-tac-toe game, the ‘game grid’ is
represented by a 3 x 3 array of spheres, where the
patient indicates their move by touching the relevant
sphere. In each game the patient’s task is to use their
intact limb for interaction. The patient wears an ordi-
nary baseball cap, instrumented with lightweight sen-
sors for tracking head movement, sending data wire-
lessly to the control computer. The patient’s anatomi-
cally intact limb is tracked using the Kinect motion
tracking device (Xbox 360 Kinect, 2011), and the
tracked movements are used to control a computer
graphical representation of the missing limb in the vir-
tual environment. The patient views the VE immer-
sively using a Vuzix VR920 headset (Vuzix, 2011).
The Vuzix was chosen for its reasonably high resolu-
tion screen (monoscopic, with two 640x480 panels),
its lightweight build and the addition of a rubber ‘eye-
shield’ that blocks external light, creating a more im-
mersive experience.
Figure 2 shows the software architecture of the
system, which uses only cross-platform components
(though our experiments have been conducted using
Mac OS X 10.6). The Cinder graphics library (Cinder,
2011) provides basic functionality and cross-platform
graphics support. OpenNI (OpenNI, 2011) and the
NITE Middleware (NITE, 2011) allows the Kinect to
GRAPP 2012 - International Conference on Computer Graphics Theory and Applications
428
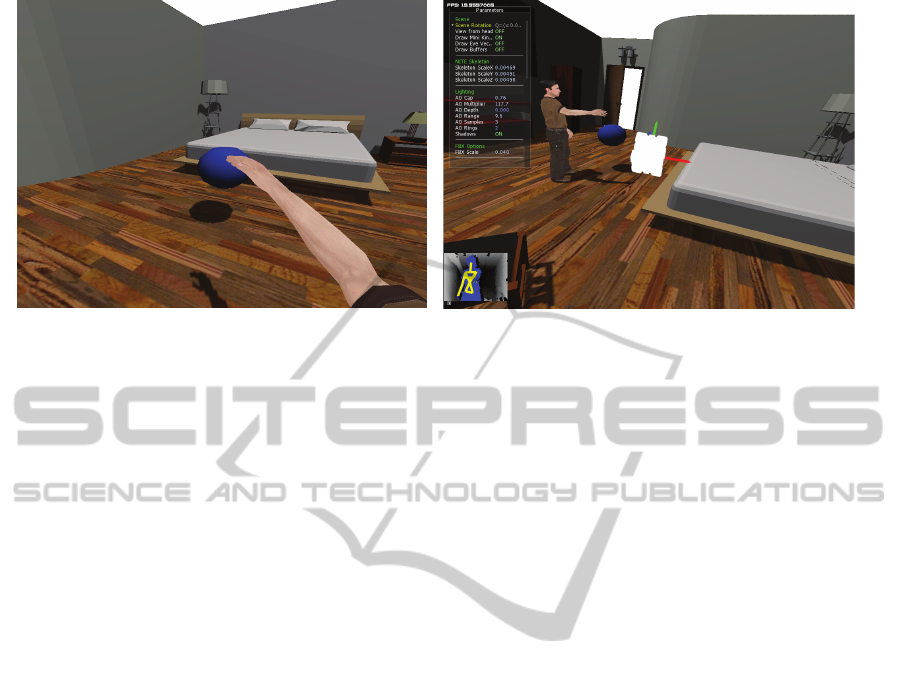
(a) (b)
Figure 1: Screenshots of the system in use. Panel (a) shows the virtual environment as seen by the participant playing the
‘ball following’ game. Panel (b) shows the same environment as seen by the operator, with the environment’s control display
in the top left of the image, and the Kinect’s skeleton tracking window at bottom left.
be linked to Cinder in order to detect and track par-
ticipants. NITE provides basic information on the po-
sition and orientation of a set number of limbs and
joints for each detected person. A capture pose is re-
quired by the OpenNI middleware in order to estimate
the lengths of the limbs within the system. This must
take place before any skeleton tracking can begin.
This calibration step is performed per-patient, and our
prototype implementation requires an anatomically
complete image, which for an amputee patient may
involve an assistant temporarily holding a ‘dummy’
limb (constructed from cardboard) in place.
To determine the orientation of the patient’s head,
a six-DOF Inertial Measurement Unit from Spark-
fun (Sparkfun, 2011) is linked to an XBee IEEE Stan-
dard 802.15.4 radio (XBee, 2011) run by a lithium
polymer battery. The unit is attached to the patient’s
baseball cap. Orientation is computed using Kalman
filtering (K
´
alm
´
an, 1960; Welch, 2009) and an ini-
tial rest point. Raw data from the three gyroscopes
and three accelerometers are sent wirelessly over the
XBee wireless link to the computer running the sim-
ulation.
With the orientation of the head from the gyro-
scope and the orientation of the body and the position
of the joints from the Kinect, a simple 3D skinned
representation of the participant can be created in 3D.
Models are generated from FBX files (FBX, 2011)
which support the generation of bones, clusters and
associated weights needed to deform a model cor-
rectly.
4 RESULTS
Our goal has been to build a cheap, portable, non-
intrusive system for experiments in use of virtual en-
vironments for PLP rehabilitation, with the aim of
replicating – and then, through larger-scale trials –
bettering the results observed in previous VE/PLP
experiments which used more expensive and fragile
equipment. To this end, we have built a prototype
system that uses mostly ‘off the shelf’ cheap, easily
available and replaceable components, and designed
tasks within the virtual environment that work within
the constraints of the hardware. From a purely ‘virtual
reality technology’ perspective, we believe the results
are very encouraging; for the overall cost of the sys-
tem (an order of magnitude cheaper than our previous
technology), the virtual environment is comparable in
quality, and because of the wireless tracking, using
the system is considerably simpler and more comfort-
able for the patient. The system’s current limitations
(awkward initial calibration, cumulative drift in the
gyroscope data, and lack of finger flexion or hand ro-
tation tracking), we believe can be addressed in future
developments.
Perhaps more positive than the technological re-
sults, however, have been the system’s effects during
a preliminary, and highly informal, trial with one am-
putee patient. The trial was intended to give us basic
feedback on the behaviour and ‘feel’ of the system
from a patient’s point of view, rather than to invoke
any therapeutic effect. The patient had, five years pre-
viously, undertaken trials with our first VR PLP sys-
tem, and had experienced reduction in pain lasting
AN IMMERSIVE VIRTUAL ENVIRONMENT FOR PHANTOM LIMB PAIN REHABILITATION
429
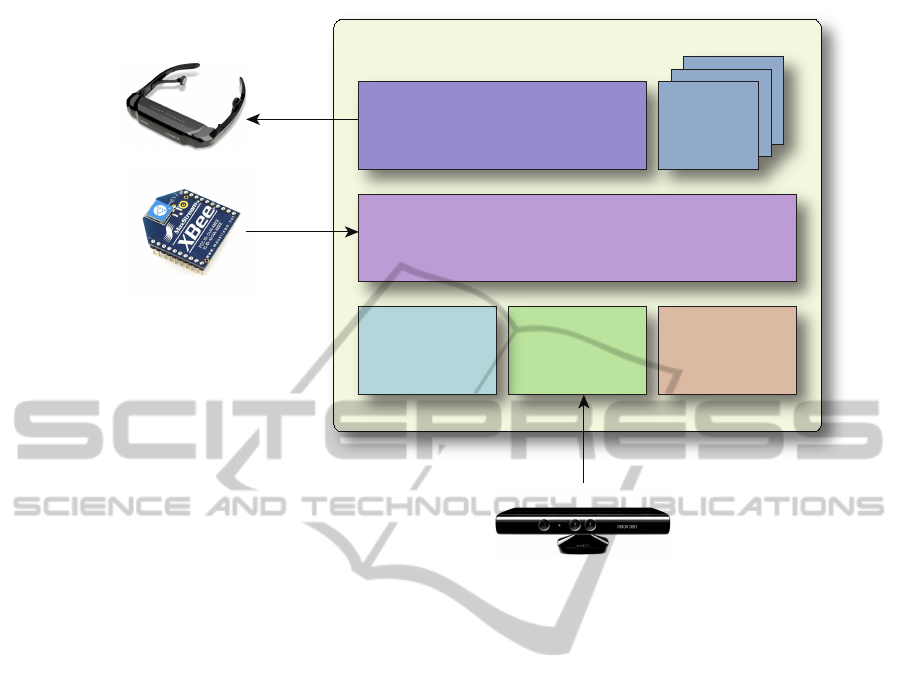
OpenNI &
NITE
Middleware
FBX SDK
Libraries
Cinder &
Boost
Libraries
Phantom Limb 2
Library
Phantom Limb 2
Environment Engine
Game
Plugins
Kinect(tm) Motion Tracker
Vuzix HMD
XBee Wireless
Transponder
Figure 2: Architecture of the PLP2 system, showing the relationship between the main software components and the hardware
devices.
for several days after each use. In the PLP2 trial,
which lasted three hours, the patient was introduced
to the system and after 15 minutes of free acclimati-
sation to the virtual environment and the limb track-
ing, was asked to play the games. On arrival, the pa-
tient reported their pain level as 8 (on the Numerical
Rating Scale of 10, with 0= no pain and 10=worst).
After 30 minutes using the PLP2 system, the pa-
tient reported his pain level had reduced to 2.5. A
short video illustrating the informal trial is available
at http://aig.cs.man.ac.uk/research/plp2.
5 CONCLUSIONS AND FUTURE
WORK
Our first conclusion is simply that it is possible to de-
sign and build a VE system for exploring PLP using
primarily ‘off the shelf’ components. Our second is
that, though taking into account all possible techno-
logical and psychological issues, the number of vari-
ables to control for in future trials of this technology is
daunting, it is nevertheless interesting to observe that
the three approaches to VR PLP therapy described in
Section 2 all had broadly comparable levels of suc-
cess in reducing pain; and this in spite of them taking
radically different approaches to tracking and render-
ing (indeed, they appear to share no common tech-
nology). Even in our informal short trial reported in
Section 4 – which again shares no common technol-
ogy with our previous experimental setup – the patient
reported a non-trivial therapeutic effect. We note that
the various studies cited here of parameters relating to
VR pain reduction all use VR as a source of distrac-
tion from physical/neuropathic pain. It has been sug-
gested that the between-patient variability in response
to visual therapy is related more to the patient’s sus-
ceptibility to the virtual visual feedback than to physi-
cal factors (Mercier and Sirigu, 2009). Because of the
substantial variation in the techniques and parameters
that have been explored in this space with comparable
results, we speculate further that whatever the causes
of PLP, the therapeutic effect of VR is as much an ef-
fect of the process of gaining agency over a phantom
limb using a virtual representation, as it is of any spe-
cific feature or parameter of the virtual environment.
There remain many interesting questions to be ad-
dressed, which include: how important is the dimen-
sionality of the virtual environment? In our previous
system, the patient saw a true stereo view, from left
GRAPP 2012 - International Conference on Computer Graphics Theory and Applications
430

and right images in the head-mounted display’s re-
spective eye-screens; in PLP2, we currently present
the patient with a 2D view of the VE. This leads to
the general issue of photorealism – what roles, if any,
do the quality of the image, the frame-rate, and the
graphical realism play in any reduction of pain felt by
the patient? Some authors (such as (Hoffman et al.,
2006)) believe that display quality is an important fac-
tor. From our experience we remain unconvinced that
this is necessarily true.
Our research into the use of virtual environments
for PLP rehabilitation is ongoing, and our immedi-
ate plans are to improve PLP2 to enable us to address
the issues of inaccurate tracking and tracking drift, to
engineer a system which is more robust, and to use
the improved system for a set of formal clinic trials
with our project partners, where we will conduct ex-
periments to assess the contributions that factors such
as dimensionality and ‘realism’ make to therapeutic
value.
REFERENCES
Anderson-Barnes, V. C., McAuliffe, C., Swanberg, K. M.,
and Tsao, J. W. (2009). Phantom limb pain–a phe-
nomenon of proprioceptive memory? Med. Hypothe-
ses, 73:555–558.
Black, L. M., Persons, R. K., and Jamieson, B. (2009). Clin-
ical inquiries. What is the best way to manage phan-
tom limb pain? J Fam Pract, 58:155–158.
Bone, M., Critchley, P., and Buggy, D. J. (2002).
Gabapentin in postamputation phantom limb pain: a
randomized, double-blind, placebo-controlled, cross-
over study. Reg Anesth Pain Med, 27:481–486.
Borsook, D., Becerra, L., Fishman, S., Edwards, A., Jen-
nings, C. L., Stojanovic, M., Papinicolas, L., Ra-
machandran, V. S., Gonzalez, R. G., and Breiter, H.
(1998). Acute plasticity in the human somatosensory
cortex following amputation. Neuroreport, 9:1013–
1017.
Bowsher, D., Rigge, M., and Sopp, L. (1991). Prevalence
of chronic pain in the british population: A telephone
survey of 1037 households. Pain Clinic, 4:223–230.
Brodie, E. E., Whyte, A., and Waller, B. (2003). Increased
motor control of a phantom leg in humans results from
the visual feedback of a virtual leg. Neurosci Letters,
2(341):167–169.
Calderwood, M. D., Kelly, J., McNamara, T. P., and Bo-
denheimer, B. (2009). Adding head tracking to desk-
top virtual reality with the wii remote as an aid to
spatial cognition. In Proceedings of the 6th Sympo-
sium on Applied Perception in Graphics and Visual-
ization, APGV ’09, pages 125–125, New York, NY,
USA. ACM.
Casale, R., Alaa, L., Mallick, M., and Ring, H. (2009).
Phantom limb related phenomena and their rehabilita-
tion after lower limb amputation. Eur J Phys Rehabil
Med, 45:559–566.
Chertoff, D. B., Schatz, S. L., McDaniel, R., and Bowers,
C. A. (2008). Improving presence theory through ex-
periential design. Presence: Teleoper. Virtual Envi-
ron., 17:405–413.
Cinder (2011). libcinder.org.
Claypool, M. and Claypool, K. (2009). Perspectives, frame
rates and resolutions: it’s all in the game. In Proceed-
ings of the 4th International Conference on Founda-
tions of Digital Games, FDG ’09, pages 42–49, New
York, NY, USA. ACM.
Cole, J., Crowle, S., Austwick, G., and Slater, D. H. (2009).
Exploratory findings with virtual reality for phantom
limb pain; from stump motion to agency and analge-
sia. Disabil Rehabil, 31:846–854.
Dahlquist, L. M., Herbert, L. J., Weiss, K. E., and Jimeno,
M. (2010). Virtual-reality distraction and cold-pressor
pain tolerance: does avatar point of view matter? Cy-
berpsychol Behav Soc Netw, 13:587–591.
Desmond, D. M. and MacLachlan, M. (2006). Affective
distress and amputation-related pain among older men
with long-term, traumatic limb amputations. J Pain
Symptom Manage, 31:362–368.
Desmond, D. M., O’Neill, K., Paor, A. D., McDarby, G.,
and MacLachlan, M. (2006). Augmenting the reality
of phantom limbs: Three case studies using an aug-
mented mirror box procedure. Journal of Prosthetics
and Orthotics, 18(3):74–79.
Dolezal, J. M., Vernick, S. H., Khan, N., Lutz, D., and
Tyndall, C. (1998). Factors associated with use and
nonuse of an ak prosthesis in a rural, southern, geri-
atric population. Int J Rehabil Health, 4(4):245–251.
Ehde, D. M., Czerniecki, J. M., Smith, D. G., Campbell,
K. M., Edwards, W. T., Jensen, M. P., and Robinson,
L. R. (2000). Chronic phantom sensations, phantom
pain, residual limb pain, and other regional pain af-
ter lower limb amputation. Arch Phys Med Rehabil,
81:1039–1044.
Eisemann, E., Assarsson, U., Schwarz, M., and Wimmer,
M. (2009). Casting shadows in real time. In ACM
SIGGRAPH ASIA 2009 Courses, SIGGRAPH ASIA
’09, New York, NY, USA. ACM.
Ephraim, P. L., Wegener, S. T., MacKenzie, E. J., Dilling-
ham, T. R., and Pezzin, L. E. (2005). Phantom pain,
residual limb pain, and back pain in amputees: re-
sults of a national survey. Arch Phys Med Rehabil,
86:1910–1919.
Ezendam, D., Bongers, R. M., and Jannink, M. J. (2009).
Systematic review of the effectiveness of mirror ther-
apy in upper extremity function. Disabil Rehabil,
31:2135–2149.
FBX (2011). usa.autodesk.com.
Flor, H. (2002). Phantom-limb pain: characteristics, causes,
and treatment. Lancet Neurol, 1:182–189.
Flor, H., Elbert, T., Knecht, S., Wienbruch, C., Pantev,
C., Birbaumer, N., Larbig, W., and Taub, E. (1995).
Phantom-limb pain as a perceptual correlate of corti-
cal reorganization following arm amputation. Nature,
375:482–484.
AN IMMERSIVE VIRTUAL ENVIRONMENT FOR PHANTOM LIMB PAIN REHABILITATION
431

Gibson, S., Cook, J., Howard, T., and Hubbold, R. J.
(2002). ICARUS: Interactive reconstruction from un-
calibrated images sequences. In SIGGRAPH 2002
Sketches and Applications Programme. San Antonio,
Texas.
Giraux, P. and Sirigu, A. (2003). Illusory movements of
the paralyzed limb restore motor cortex activity. Neu-
roimage, 20 Suppl 1:S107–111.
Giummarra, M. J., Georgiou-Karistianis, N., Nicholls,
M. E., Gibson, S. J., Chou, M., and Bradshaw, J. L.
(2011). The menacing phantom: What pulls the trig-
ger? Eur J Pain, 15:1–8.
Group, A. I. (2010). aig.cs.man.ac.uk.
Gutierrez-Maldonado, J., Gutierrez-Martinez, O., Loreto,
D., Penaloza, C., and Nieto, R. (2010). Presence, in-
volvement and efficacy of a virtual reality intervention
on pain. Stud Health Technol Inform, 154:97–101.
Gutierrez-Martinez, O., Gutierrez-Maldonado, J., and
Loreto-Quijada, D. (2011). Control over the virtual
environment influences the presence and efficacy of a
virtual reality intervention on pain. Stud Health Tech-
nol Inform, 167:111–115.
H
¨
ansel, A., Lenggenhager, B., von K
¨
anel, R., Curatolo, M.,
and Blanke, O. (2011). Seeing and identifying with a
virtual body decreases pain perception. Eur J Pain.
Hoffman, H. G., Seibel, E. J., Richards, T. L., Furness,
T. A., Patterson, D. R., and Sharar, S. R. (2006). Vir-
tual reality helmet display quality influences the mag-
nitude of virtual reality analgesia. J Pain, 7:843–850.
Hoffman, H. G., Sharar, S. R., Coda, B., Everett, J. J., Ciol,
M., Richards, T., and Patterson, D. R. (2004). Manip-
ulating presence influences the magnitude of virtual
reality analgesia. Pain, 111:162–168.
Hubbold, R., Cook, J., Keates, M., Gibson, S., Howard,
T., Murta, A., West, A., and Pettifer, S. (2001).
GNU/MAVERIK : A micro-kernel for large-scale vir-
tual environments. Presence: Teloperators and Vir-
tual Environments, 10:22–34. ISSN 1054-7460.
Jensen, T. S. and Nikolajsen, L. (1994). Phantom limb pain
and other phenomena after amputation. Churchill
Livingstone.
K
´
alm
´
an, R. E. (1960). A new approach to linear filtering
and prediction problems. Transactions of the ASME—
Journal of Basic Engineering, 82(D):35–45.
Katz, J. (1992). Psychophysiological contribution to phan-
tom limbs. Can J Psychiatr, 37:282–282.
Kooijman, C. M., Dijkstra, P. U., Geertzen, J. H., Elzinga,
A., and van der Schans, C. P. (2000). Phantom pain
and phantom sensations in upper limb amputees: an
epidemiological study. Pain, 87:33–41.
Krieg, J. C. (1993). Accuracy, resolution, latency and speed;
key factors in virtual reality tracking environments. In
Proceedings of the 3rd annual virtual reality confer-
ence and exhibition on VR becomes a business, pages
90–100, Westport, CT, USA. Meckler Corporation.
Lamounier, E., Lopes, K., Cardoso, A., Andrade, A., and
Soares, A. (2010). On the use of virtual and aug-
mented reality for upper limb prostheses training and
simulation. Conf Proc IEEE Eng Med Biol Soc,
2010:2451–2454.
LaViola, Jr., J. J. and Litwiller, T. (2011). Evaluating the
benefits of 3d stereo in modern video games. In Pro-
ceedings of the 2011 annual conference on Human
factors in computing systems, CHI ’11, pages 2345–
2354, New York, NY, USA. ACM.
Lee, J. C. (2008). Hacking the nintendo wii remote. IEEE
Pervasive Computing, 7:39–45.
Leyvand, T., Meekhof, C., Wei, Y.-C., Sun, J., and Guo, B.
(2011). Kinect identity: Technology and experience.
Computer, 44:94–96.
Liebermann, D. I. (2010). Mirror Box Therapy. mirrorbox-
therapy.com.
Limbless Statistics (2011). www.limbless-statistics.org.
Lindeman, R. W. and Beckhaus, S. (2009). Crafting mem-
orable vr experiences using experiential fidelity. In
Proceedings of the 16th ACM Symposium on Virtual
Reality Software and Technology, VRST ’09, pages
187–190, New York, NY, USA. ACM.
MacLachlan, M., McDonald, M., and Waloch, J. (2004).
Mirror treatment of lower limb phantom pain: a case
study. Disabil Rehabil, 26:901–904.
Mahrer, N. E. and Gold, J. I. (2009). The use of virtual
reality for pain control: a review. Curr Pain Headache
Rep, 13:100–109.
Malloy, K. M. and Milling, L. S. (2010). The effectiveness
of virtual reality distraction for pain reduction: a sys-
tematic review. Clin Psychol Rev, 30:1011–1018.
Manchikanti, L. and Singh, V. (2004). Managing phantom
pain. Pain Physician, 7:365–375.
McCabe, C. S., Haigh, R. C., Halligan, P. W., and Blake,
D. R. (2005). Simulating sensorymotor incongru-
ence in healthy volunteers: implications for a cortical
model of pain. Rheumatology, 44(4):509–516.
Mercier, C. and Sirigu, A. (2009). Training with virtual
visual feedback to alleviate phantom limb pain. Neu-
rorehabil Neural Repair, 23:587–594.
Mitchell, S. W. (1872). Injuries of nerves and their
consequences. J. B. Lippincott. Digitised at
www.archive.org/details/injuriesofnerves00mitcuoft.
Murray, C. D. (2005). The social meanings of prosthesis
use. J Health Psychol, 3(10):425–441.
Murray, C. D., Patchick, E., Caillette, F., Howard, T., and
Pettifer, S. (2006a). Can immersive virtual reality re-
duce phantom limb pain? Medicine meets virtual re-
ality: Accelerating change in healthcare, pages 407–
412.
Murray, C. D., Patchick, E., Pettifer, S., and Howard, T.
(2006b). Investigating the efficacy of a virtual mir-
ror box in treating phantom limb pain in a sample
of chronic sufferers. In Sharkey, P., Brooks, T.,
and Cobb, S., editors, Proceedings of The 6th In-
ternational Conference on Disability, Virtual Reality
and Associated Technologies, pages 167–174, Esb-
jerg, Denmark. ISBN 7 049 98 65 3.
Murray, C. D., Patchick, E., Pettifer, S., Howard, T., Kalka-
rni, J., and Bamford, C. (2007a). Investigating the
efficacy of a virtual mirror box in treating phantom
limb pain in a sample of chronic sufferers. Interna-
tional Journal of Disability and Human Development,
5(3):227–234.
GRAPP 2012 - International Conference on Computer Graphics Theory and Applications
432

Murray, C. D., Pettifer, S., Caillette, F., Patchick, E., and
Howard, T. (2005). Immersive virtual reality as a re-
habilitative technology for phantom limb experience.
Proc IWVR 2005 4th Int Workshop Virtual Rehabi,
pages 144–151.
Murray, C. D., Pettifer, S., Caillette, F., Patchick, E., and
Howard, T. (2006c). Immersive virtual reality as a re-
habilitative technology for phantom limb experience:
A protocol. CyberPsychol Behav, 2(9):167–170.
Murray, C. D., Pettifer, S., Howard, T., E. Patchick, F. C.,
and Murray, J. (2010). Virtual solutions to phan-
tom problems: Using immersive virtual reality to treat
phantom limb pain. In Murray, C., editor, Amputation,
Prosthesis and Phantom Limb Pain, pages 175–197.
Springer. ISBN 0387874615.
Murray, C. D., Pettifer, S., Howard, T., Patchick, E., Kalka-
rni, J., and Bamford, C. (2007b). The treatment
of phantom limb pain using immersive virtual real-
ity: three case studies. Disability and Rehabilita-
tion, 29(18):1465–1469. ISSN 1464-5165 (electronic)
0963-8288 (paper).
NASDAB (2002). National Amputation Statistical
Database Annual Report. The Department of Health,
Social Services and Public Safety (UK).
Nintendo Wii (2011). www.nintendo.com/wii.
NITE (2011). www.primesense.com.
OpenNI (2011). www.openni.org.
Pettifer, S. R., Thorne, D., McDermott, P., Marsh, J.,
Vill
´
eger, A., Kell, D. B., and Attwood, T. K. (2009).
Visualising biological data: a semantic approach to
tool and database integration. BMC Bioinformatics,
16.
Radio 4, B. (2006). The Material World. www.bbc.co.uk/
radio4/science/thematerialworld 20061123.shtml.
Ramachandran, V. S. and Rogers-Ramachandran, D.
(1996). Synaesthesia in phantom limbs induced with
mirrors. Proc Biol Sci, 341:377–386.
Rutter, C. E., Dahlquist, L. M., and Weiss, K. E. (2009).
Sustained efficacy of virtual reality distraction. J Pain,
10:391–397.
Sato, K., Fukumori, S., Matsusaki, T., Maruo, T., Ishikawa,
S., Nishie, H., Takata, K., Mizuhara, H., Mi-
zobuchi, S., Nakatsuka, H., Matsumi, M., Gofuku, A.,
Yokoyama, M., and Morita, K. (2010). Nonimmer-
sive virtual reality mirror visual feedback therapy and
its application for the treatment of complex regional
pain syndrome: an open-label pilot study. Pain Med,
11:622–629.
Scherfgen, D. and Herpers, R. (2009). 3d tracking using
multiple nintendo wii remotes: a simple consumer
hardware tracking approach. In Proceedings of the
2009 Conference on Future Play on @ GDC Canada,
Future Play ’09, pages 31–32, New York, NY, USA.
ACM.
Serafin, S. (2004). Sound design to enhance presence in
photorealistic virtual reality. In Proceedings of the
10th Meeting of the International Conference on Au-
ditory Display. International Community for Auditory
Display.
Sherman, R. A., Sherman, C. J., and Parker, L. (1984).
Chronic phantom and stump pain among american
veterans: results of a survey. Pain, 18:83–89.
Sko, T. and Gardner, H. (2009). The wiimote with multi-
ple sensor bars: creating an affordable, virtual reality
controller. In Proceedings of the 10th International
Conference NZ Chapter of the ACM’s Special Interest
Group on Human-Computer Interaction, CHINZ ’09,
pages 41–44, New York, NY, USA. ACM.
Slater, M. and Steed, A. (2000). A virtual presence counter.
Presence: Teleoper. Virtual Environ., 9:413–434.
Soler, M. D., Kumru, H., Pelayo, R., Vidal, J., Tormos,
J. M., Fregni, F., Navarro, X., and Pascual-Leone, A.
(2010). Effectiveness of transcranial direct current
stimulation and visual illusion on neuropathic pain in
spinal cord injury. Brain, 133:2565–2577.
Sparkfun (2011). www.sparkfun.com.
Vuzix (2011). www.vuzix.com/consumer/products vr920.h
tml.
Welch, G. F. (2009). History: The use of the kalman filter
for human motion tracking in virtual reality. Presence:
Teleoper. Virtual Environ., 18:72–91.
Wender, R., Hoffman, H. G., Hunner, H. H., Seibel, E. J.,
Patterson, D. R., and Sharar, S. R. (2009). Interactivity
influences the magnitude of virtual reality analgesia. J
Cyber Ther Rehabil, 2:27–33.
Williamson, G. M., Schulz, R., Bridges, M. W., and Behan,
A. M. (1994). Social and psychological factors in ad-
justment to limb amputation. J Soc Behav Personal,
3(10):425–441.
Witmer, B. G. and Singer, M. J. (1998). Measuring pres-
ence in virtual environments: A presence question-
naire. Presence: Teleoper. Virtual Environ., 7:225–
240.
XBee (2011). www.digi.com/xbee.
Xbox 360 Kinect (2011). www.xbox.com/kinect.
Zeigler-Graham, K., MacKenzie, E. J., L.Ephraim, P., Trav-
ison, T. G., and Brookmeyer, R. (2008). Estimating
the prevalence of limb loss in the United States - 2005
to 2050. Archives of Physical Medicine and Rehabili-
tation, 89:422–429.
AN IMMERSIVE VIRTUAL ENVIRONMENT FOR PHANTOM LIMB PAIN REHABILITATION
433
