
Using Enterprise Ontology for Improving the National Health System
Demonstrated in the Case of a Pharmacy and an Emergency Department
David Dias, Carlos Mendes and Miguel Mira da Silva
Instituto Superior Técnico, Technical University of Lisbon, Avenida Rovisco Pais, Lisboa, Portugal
Keywords: Enterprise Ontology (EO), Enterprise Reengineering, Operational Processes, Design Engineering
Methodology for Organizations (DEMO), Emergency Department (ED), Pharmacy.
Abstract: The global healthcare spending has constantly increased in the last decades, and there is data showing
inefficiency in resource consumption that is not reflected in healthcare improvement. The need to introduce
new ways to do the same thing at a lower cost is rational. To address this, we propose a method based on
Design Engineering Methodology for Organizations (DEMO) to find non value-added transactions that
must be redesigned to simplify processes. This methodology was chosen as a basis for our solution because
it provides a better understanding of the dynamics of an organization, and allows a good alignment between
the enterprise design and operation. A demonstration was accomplished within an Emergency Medical
Service and a Pharmacy, making it possible to find transactions that can be improved or automated.
Evaluation was carried out by means of interviews, the Four Principles from Österle et al., and the Moody
and Shanks Quality Framework. Results prove that the method yields an adequate and clear process view
and is reliable when it comes to improving healthcare operational processes.
1 INTRODUCTION
In a world of growing business dynamics, high rates
of technological advances and organizational
changes, organizations need to be effectively and
continuously redesigned and reengineered in order
to achieve strategic and operational success. The
inefficiency of processes and the lack of innovation
are the main reasons for strategic failures, entailing
serious consequences for business (Kotter, 1996)
(Henriques, Tribolet and Hoogervorst, 2010).
These strong external forces and the need for
innovation also challenge the healthcare system. Its
organizations need to improve treatments, eliminate
non value-added activities, reduce waiting time and
expenses, treat more patients, and implement new
technological services. Besides these challenges, the
healthcare system suffers from problems of
operational management, and its processes are
considered inefficient (Christensen, Grossman and
Hwang, 2009) (Kaplan and Porter, 2011).
A frightening factor is that not only its
expenditure accounts for 10% of the Gross Domestic
Product (GDP) in developed countries, but there is
also an increasing trend, as depicted in Figure 1.
Other than that, there is data indicating that cost and
quality are not correlated, and showing inefficiency
in resource consumption, which is not reflected in
improved quality of care. Consequently, the quality
of life may be affected because of a knock-on effect
on the economy, increase in tax rates and insurance
contributions, disinvestment in other public services,
and increased difficulties to afford healthcare
services (Kaplan and Porter, 2011) (Walshe and
Smith, 2010). Hence, this research stems from the
assumption that many healthcare processes have
become inefficient and unsustainable, which affects
the management of the healthcare system.
Figure 1: Global evolution of healthcare expenditure –
adapted from OECD Website (OECD, 2012).
Although the problem is identified as a need for
redesign and reengineering, some authors argue that
there is no strong and reliable method to solve this
441
Dias D., Mendes C. and Mira da Silva M..
Using Enterprise Ontology for Improving the National Health System - Demonstrated in the Case of a Pharmacy and an Emergency Department.
DOI: 10.5220/0004133004410451
In Proceedings of the International Conference on Knowledge Engineering and Ontology Development (SSEO-2012), pages 441-451
ISBN: 978-989-8565-30-3
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

problem (Dietz and Hoogervorst, 2008). It is
estimated that over 70% of strategic initiatives such
as Total Quality Management, Business Process
Reengineering, and Six Sigma, among others, tend
to fail (Mintzberg, 1994) (Lifvergren and et al.,
2010). In this context, we addressed three main
reasons for this: 1) The lack of integration among
the various enterprise elements at the design level;
2) The inability to deal with the enterprise dynamics
at the operational level due to weak enterprise
construction models; and 3) The need to change
management that advocates the development of self-
awareness within the organization (Dias, Lapão and
Silva, 2012) (Dias et al., 2012) (Henriques, Tribolet
and Hoogervorst, 2010).
Following this, our research proposes an
approach based on the theories of Enterprise
Ontology (EO) and the corresponding methodology
– Design and Engineering Methodology for
Organizations (DEMO). We chose this approach as
a foundation for our proposal, because it is
considered to provide a better understanding of an
organization’s dynamics, has a strong and well-
formed theory, allows a good alignment between the
enterprise design and operation, and it also enables a
unified reengineering strategy (Dietz, 2006)
(Reijswoud, Mulder and Dietz, 1999). Therefore, we
enunciate the research problem as: Using EO to
propose improvements in the healthcare system.
This research was conducted by using the Design
Science Research Methodology (DSRM) that aims
at creating and evaluating artifacts to solve relevant
organizational problems (Henver and et al., 2004).
The obtained artifact is a method that provides
guidance on how to find improvements through a set
of steps. In order to demonstrate the proposal, we are
applying it within medical organizations, such as an
Emergency Department (ED) and a Pharmacy.
Besides the possible improvements in each
organization, we are also interested in analyzing the
interactions between these two so that we can
conclude how they can improve cooperation.
To evaluate the proposed artifact we used: 1)
The framework proposed in (Pries-Heje, Baskerville
and Venable, 2004), 2) Demonstrations of the utility
of the method; 3) Interviews with practitioners; 3)
The Four Principles from (Österle et al., 2011) to
evaluate the artifact; and 4) The Moody and Shanks
Quality Management Framework (Moody and
Shanks, 2003) to evaluate the produced models.
The steps from the DSRM are reflected upon in
the sections of this paper, which is structured as
follows. In Section 1 we just introduced our problem
and motivation. Then, a brief overview of the
literature is provided (Section 2). Afterwards, we
identify the objectives of the solution and describe
the proposal to redesign the healthcare processes
(Section 3). Next we present case studies where the
proposal was applied as demonstration (Section 4).
In Section 5, we describe the evaluation strategy and
discuss the results of applying the proposal. Finally,
we draw some conclusions in Section 6.
2 RELATED WORK
This section gives a brief overview of the Quality
Management (QM) and EO Sections 2.1 and 2.2.
2.1 Quality Management
Edwards Deming, one of the main and originator
sources in QM, defended that organizations could
increase quality and reduce costs by adopting
appropriate principles of management. He identified
seven constructs as main drivers: visionary
leadership, internal and external cooperation,
learning, process management, continuous
improvement, employee fulfillment, and customer
satisfaction (Rungtusanatham et al., 1998). Hence,
authors defend that these topics are considered
crucial not only to compete and prosper, but also to
merely survive against external forces (Kotter,
1996). In response to the need of QM and
continuous improvement, different methodologies
and strategies appeared, such as Organization
Design and Engineering methodologies, Lean, Six
Sigma, Total Quality Management, among others
(Mintzberg, 1994) (Lifvergren and et al., 2010).
Lean is considered one of the most used in the
management of the healthcare system (Burgess and
Radnor, 2010). It is typically grounded in the PDCA
Operating Framework, and focus on the waste
removal to deliver an improved flow time. The
PDCA cycle suggests that all work should be
measured and performed to standards, and it is
composed by the following steps: 1) Plan: recognize
an opportunity and plan a change, its needed steps,
and results’ prediction; 2) Do: test the change using
small-scale studies as trials under controlled
conditions; 3) Check or study: changes are tested in
small-scale studies to examine its results, and if
process improvements were verified, it should be
considered the implementation on a broader scale; 4)
Act: implement the changes in a broader scale and
then repeat the cycle again with a differ plan
(Womack and Jones, 2003).
KEOD2012-InternationalConferenceonKnowledgeEngineeringandOntologyDevelopment
442
Some of the benefits of the QM and particularly
Lean in the healthcare management are the reduction
of processing and waiting time, decline in the
mortality rate, increase in quality through a
reduction of errors, decrease in the service costs and
resource expenditure, better warehouse
management, and increased employee motivation
and customer satisfaction (Fillingham, 2007)
(García-Porres, J; et al., 2008) (Radnor, 2010). On
the other hand, some authors point out some
drawbacks, such as the high rate of failed
implementations, the mischaracterization or
degradation of services, and the loss of
organization’s essence (Burgess and Radnor, 2010).
The Improvement Quantification is considered
another topic related with the QM, which helps to
make decisions and prioritize improvements based
on the expected return and feasibility. There are
different approaches that may help a manager to
make informed and just-in-time decisions about
improvements. For example, costing models that
may help to identify the cost from each activity,
allowing for a greater knowledge about its indirect
and variable costs (Kaplan and Porter, 2011).
2.2 Enterprise Ontology
Enterprise Ontology (EO) is a theory that has its
roots in the PSI-Theory (Performance in Social
Interaction), and is perceived as a model for
describing and understanding the enterprise
construction and operation at the level of human
interactions, allowing a better understanding of the
operation. Dietz brings a complementary view of the
EO, in which ontology is viewed as the “highest
level” conceptual model, fully independent of how
the enterprise is implemented. It is an enterprise
context based concept that is considered the highest
conceptual model and helps ensure integrated
enterprise. It also guides the transition from
ontological models to construction models, which
means that it assists in engineering activities (Dietz,
2006) (Henriques, Tribolet and Hoogervorst, 2010).
Unlike other methodologies, EO is considered to
provide a deep understanding of the dynamics of an
organization with a strong and well-formed theory
that allows a good alignment between the enterprise
design and the enterprise operation (Henriques,
Tribolet and Hoogervorst, 2010).
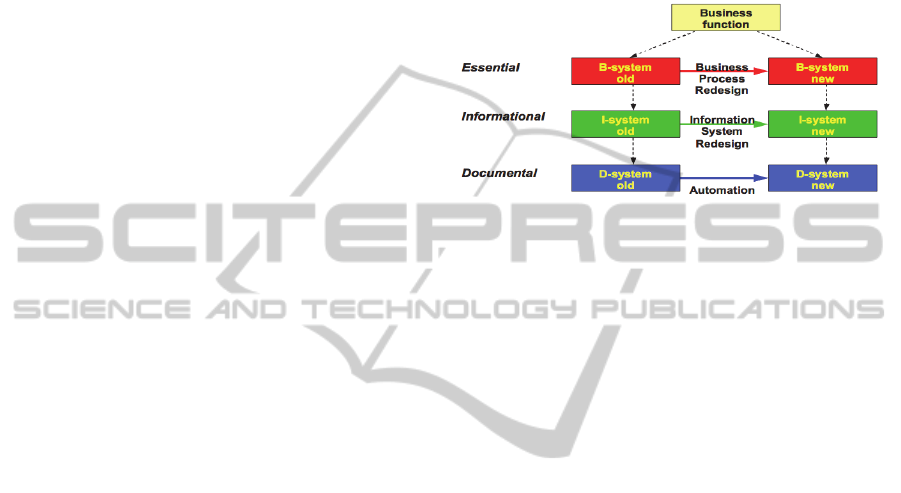
Its particular methodology, DEMO, provides a
structured working approach for modeling,
(re)designing and (re)engineering of organizations
by layering it into three parts, and focusing only on
the one that refers directly to the complete
knowledge of the enterprise – the Ontological or
Essential Layer, which is considered to affect the
other two layers (Informational and Documental), as
illustrated in Figure 2. Focusing only on the essence
conducts to a reduction in the complexity of the
obtained diagrams, considered in over 90%
(Reijswoud, Mulder and Dietz, 1999) (Dietz and
Hoogervorst, 2008).
Figure 2: The layered integration of an enterprise and its
transformation activities (Reijswoud et al., 1999).
Regarding DEMO methodology, it consists of
four interrelated aspect models, represented by
particular diagrams, lists and tables, as illustrated in
Figure 3. The Construction Model (CM) details the
identified transactions types and associated actor
roles, as well as the information links between the
actor roles and the information banks. The Process
Model (PM) specifies the state and transaction
spaces, and it is partially based on the information
defined on the CM concerning which actor roles
perform the coordination acts. In addition, PM also
contains the causal and conditional relationships
between transactions, which determine the possible
trajectories between transactions. The State Model
(SM) specifies the information banks and the state
space of the production world: the object classes, the
fact types, and the result types, as well as the
existential laws that hold. The Action Model (AM)
specifies the action rules that serve as guidelines for
the actors in dealing with every coordination step,
which are grouped according to the distinguished
actor roles. The bottom layers from the ontological
triangle integrate concepts defined in the upper
aspect models, as depicted in Figure 3. For further
reading about the EO, DEMO methodology, and the
four axioms significant to understand the
methodology we refer (Dietz, 2006).
UsingEnterpriseOntologyforImprovingtheNationalHealthSystem-DemonstratedintheCaseofaPharmacyandan
EmergencyDepartment
443

Figure 3: The ontological triangle with aspect models and
diagrams of DEMO (Dietz, 2006).
There are some examples in the healthcare
system in which EO was applied to study its internal
transactions and simplify their analysis. These
contributions validated that EO avoids the lack of
integration among the various enterprise elements at
the design level and produces strong enterprise
construction models (Maij and et al., 2000) (Habing
and et al., 2001) (Maij and et al., 2002). In addition,
we can find examples of using EO to improve
operational processes (Reijswoud, Mulder and Dietz,
1999) due to its differentiated and structured
working approach focused on the essential design of
the organization.
3 PROPOSAL
This section corresponds to the definition of the
objectives for the solution and the design and
development steps of DSRM.
3.1 Objectives of the Solution
In order to overcome the problem statement about
the inefficiency and unsustainability of the
healthcare system, different approaches are
identified. Nevertheless, some authors still argue
that there is not a reliable method to solve these
problems. It is estimated that over 70% of strategic
initiatives such as Total Quality Management,
business process reengineering (BPR), and Six
Sigma, among others, tend to fail (Mintzberg, 1994)
(Dietz and Hoogervorst, 2008) (Lifvergren and et
al., 2010). Furthermore, Dietz also adds that the
current literature on enterprise engineering consists
merely of best practices, without an integrating
theory and a clear definition of the field (Dietz,
2006). Inline with that conclusion, Caetano et al.
demonstrated that when comparing BPMN and
DEMO models, there was a set of implicit and
missing actions in BPMN, proving that it does not
provide means to assess the actual consistency and
completeness of a business process, due to the lack
of formal semantics and unclear construct
description (Caetano, Assis and Tribolet, 2011).
Following this, our research seeks to define an
artifact method based on the theories of EO because
of the strengths described previously, namely the
benefits previously described, the properties of
correctness and completeness it assures in its
models, and the properties of essentialness and
conciseness, which help to construct and analyze
(more) models, making it possible to design the
healthcare system and seek for inter-organizational
cooperation improvements between its units. The
improved alignment between the enterprise design
and operation leads to an improved self-awareness
within healthcare organizations. In addition, EO
clearly defines three notions that we considered
relevant in governing the enterprise dynamics and to
identify improvements in the healthcare system:
competence, authority, and responsibility, as
explained in the Operation Axiom (Dietz, 2006).
Most of these notions are absent or not clear defined
in other enterprise modeling techniques (Dietz,
2006) (Henriques, Tribolet and Hoogervorst, 2010).
To take advantage from some already proven
benefits from Lean for the QM and Continuous
Improvement, particularly in the healthcare system,
we intend to combine the analysis from EO with the
improvement identification from Lean. This way,
the EO may be considered as input for the Plan step
of the PDCA Operating Framework, to help with the
identification of opportunities. In other words, from
DEMO models one may identify improvements (as
suggested in the Plan step), and in the end produce
and Organization Redesign model that reflects the
change plan. To identify improvements one should
consider the existing standards on Healthcare
Management, BPR, and improvement quantification.
The following steps from PDCA cycle are out of the
thesis’ scope, as they need the creation of prototypes
and implementation in a broader scale.
In short, our main objective is to propose a
method based on EO to find non value-added
transactions, and redesign them to improve the
healthcare management. Other goals are to
demonstrate, evaluate and communicate the artifact,
to show its efficiency and efficacy. To do that are
applying the proposal to different units of the
healthcare system. Besides the possible
improvements in each healthcare unit, we are also
interested in analyzing the interactions between
them so that we can conclude how they can improve
KEOD2012-InternationalConferenceonKnowledgeEngineeringandOntologyDevelopment
444
cooperation, as part of the demonstration.
3.2 Proposed Artifact Method
This section belongs to the design and development
step of DSRM, in which we present a different
artifact (Österle et al., 2011) to identify innovations
to improve the healthcare management. It considers
the contributions from EO (Dietz, 2006), some
additional steps from Lean (García-Porres, J; et al.,
2008).
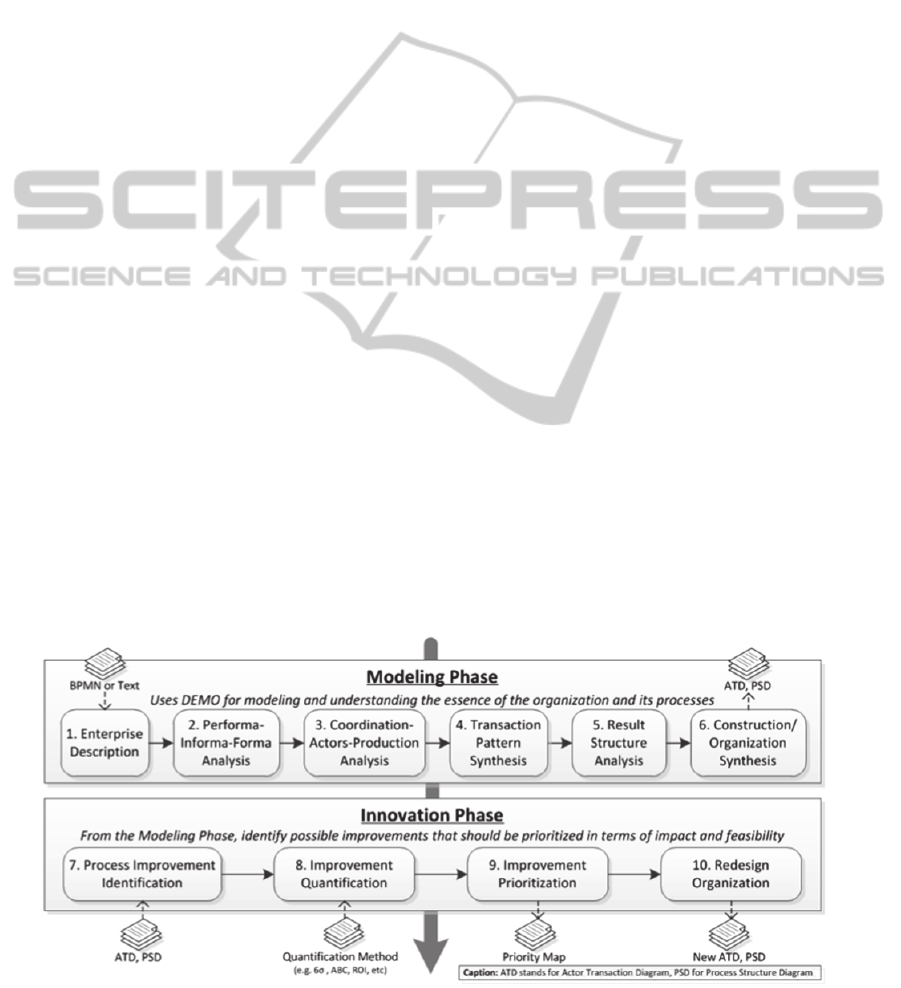
The proposal starts with the Modeling Phase,
which uses EO to study the organization and its
processes. To construct its diagrams, it consists of a
defined sequence of steps (illustrated in Figure 4)
that begins with a textual or process representation
of an organization, and ends with an aspect model.
The sequence of steps is described in previous
publications (Mendes, Ferreira and Silva, 2012).
As result, this phase provides a structured
working approach by layering the organization into
three parts, and focusing only on the one that
directly refers to the complete knowledge of the
organization and independent of the implementation
– the Ontological Layer. In this research we focus
on the Construction and Process Models, which
include the Actor Transaction Diagram (ATD) and
Process Structure Diagram (PSD).
The proposal continues with the Innovation
Phase, which is based on four additional steps from
Lean to assist in the Continuous Improvement and
the QM process. These steps consist on the Plan step
of the Lean PDCA Operating Framework that
recognizes an opportunity and plans the change.
Therefore, this phase identifies possible
improvements from the previous models, prioritizes
them in terms of impact and feasibility, and then
proposes redesigned models for the organization. As
result, this phase gives the appropriate tackle to
handle the transformation process, and helps to
choose the most profitable improvements first.
Figure 4 illustrates the proposal including its inputs
and outputs, and subsequently we describe its steps.
The first step from the Innovation Phase is the
Process Improvement Identification, which identifies
improvements from the organization models
obtained in the Modeling Phase, considering the
contributions and standards from the related work.
Considering the ATD, one can identify transactions
that do not seem essential and may be removed,
changed, or automated. These transactions may be
identified with the help of practitioners or literature.
Then, using the PSD, one can change the network of
communicative commitments to shorten processes,
change precedencies, or move conditional
relationships, which leads to shorten cycle (and
waiting) times. This step is based on (Reijswoud,
Mulder and Dietz, 1999) (Dietz and Hoogervorst,
2008).
Afterwards, the improvements are quantified
using some metrics that must be established in terms
of feasibility and impact. Some common metrics are
the time invested in each transaction compared to
the total time spent on the whole service, people
involved, management frameworks, associated
defect, or other analytical methods (e.g. costing
models, financial analysis, etc.). The chosen theory
or method is not part of this thesis’ scope (one can
choose the most suitable).
Then, the improvements are prioritized in terms
of impact and feasibility, which helps to choose the
most profitable improvements for the available
resources. This is then represented in a map divided
Figure 4: Graphical representation of the proposed method.
UsingEnterpriseOntologyforImprovingtheNationalHealthSystem-DemonstratedintheCaseofaPharmacyandan
EmergencyDepartment
445
into four quadrants, being the X-axis the feasibility
to accomplish it, and the Y-axis the quantified
impact. Each improvement is placed in a particular
quadrant, being the ones that fit into the superior
diagonal the ones that are more important to
implement (with higher impact and feasibility).
After choosing the most profitable
improvements, the organization is redesigned to
include the decisions. Alternatively, one can deepen
some analysis by including more information in the
Enterprise Description, or producing other aspect
models from DEMO. Having the redesigned
organization models with the results from the
Innovation Phase, it should be prepared a proposal
with specific implementation strategies (i.e. the plan
with the needed steps). Afterwards, one should
continue with the next steps from the PDCA cycle
(Do, Check and Act) to implement the planned
changes, beyond this thesis’ scope.
To sum up, this method replaces the analysis
from Lean by a Modeling Phase based on EO,
incorporating its contributions to achieve models
considered formally correct, easier to analyze, and
enabling a unified reengineering strategy (Dietz,
2006).
4 DEMONSTRATION
This section corresponds to the demonstration step
of DSRM. In the following sections we apply the
proposed method to an ED and to a Pharmacy. We
do not fully apply the six steps of the modeling
phase due to space limitation. Nevertheless, these
steps are demonstrated in previous publications
(Mendes, Ferreira and Silva, 2011) (Mendes,
Ferreira and Silva, 2012).
In this demonstration we will focus more on the
demonstration at the Pharmacy and its possible
improvements to increase cooperation with the ED.
4.1 Emergency Department
To demonstrate the method, we applied it to the
internal operation of an ED in a hospital near Lisbon
with more than 100,000 admissions per year,
expecting that by eliminating wasteful transactions,
it would be possible to improve processes without
compromising the organization. To conduct the
demonstration, we interviewed 5 patients and 10
practitioners (the ED director, physicians and nurses,
and health services researchers), namely to obtain
the enterprise description.
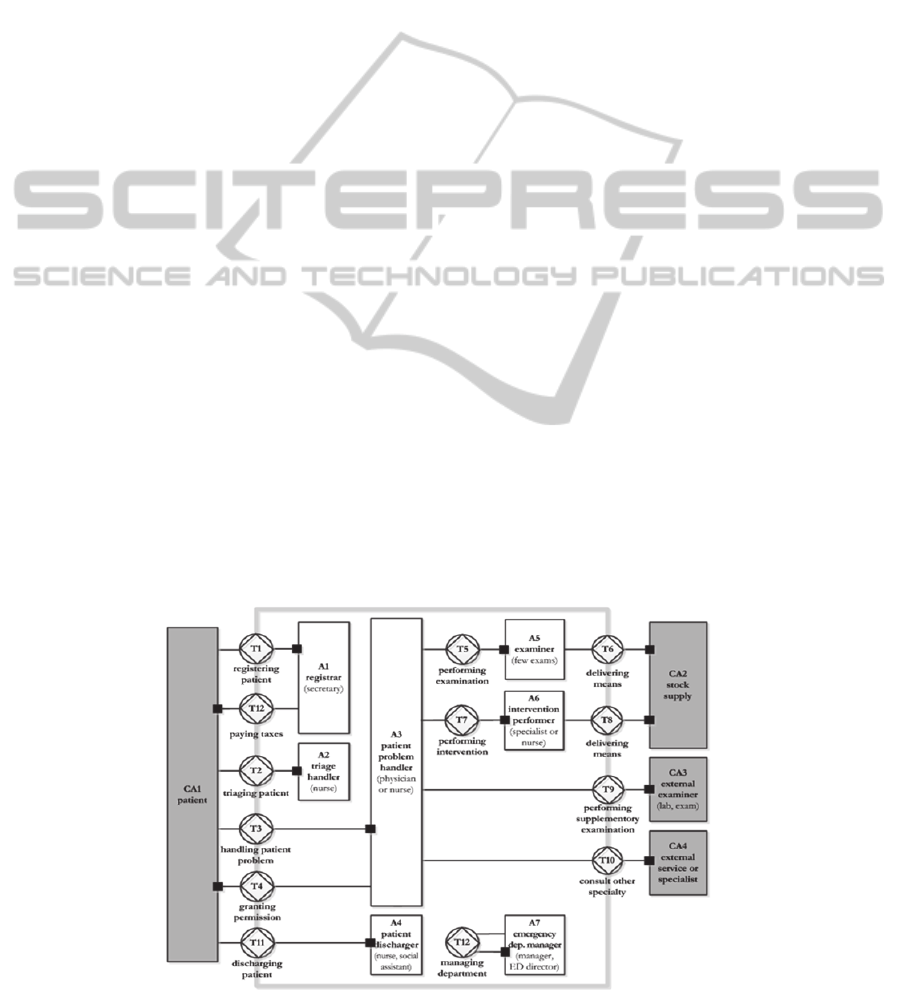
From the enterprise description and after the first
two analyses from the proposed method, we defined
the transactions by clustering the identified acts and
facts in what is denominated by Transaction Pattern
Synthesis. The results are presented below in the
ATD (Figure 5), according to the Transaction
Axiom from EO (Dietz, 2006).
In the ATD, a transaction is represented using a
diamond in a disk. Each transaction is connected to
two boxes, representing the initiator and executor
actor roles. The initiator is connected to the
transaction symbol using a solid line, while the
executor is connected to the transaction using a solid
line ending in a black square. The grey boxes refer
to composite actor roles, i.e. elements whose exact
structure is not known. All the environmental
elements, i.e. elements outside the organization that
we are studying, are represented with grey boxes for
Figure 5: Actor Transaction Diagram (ATD) of the Emergency Department.
KEOD2012-InternationalConferenceonKnowledgeEngineeringandOntologyDevelopment
446
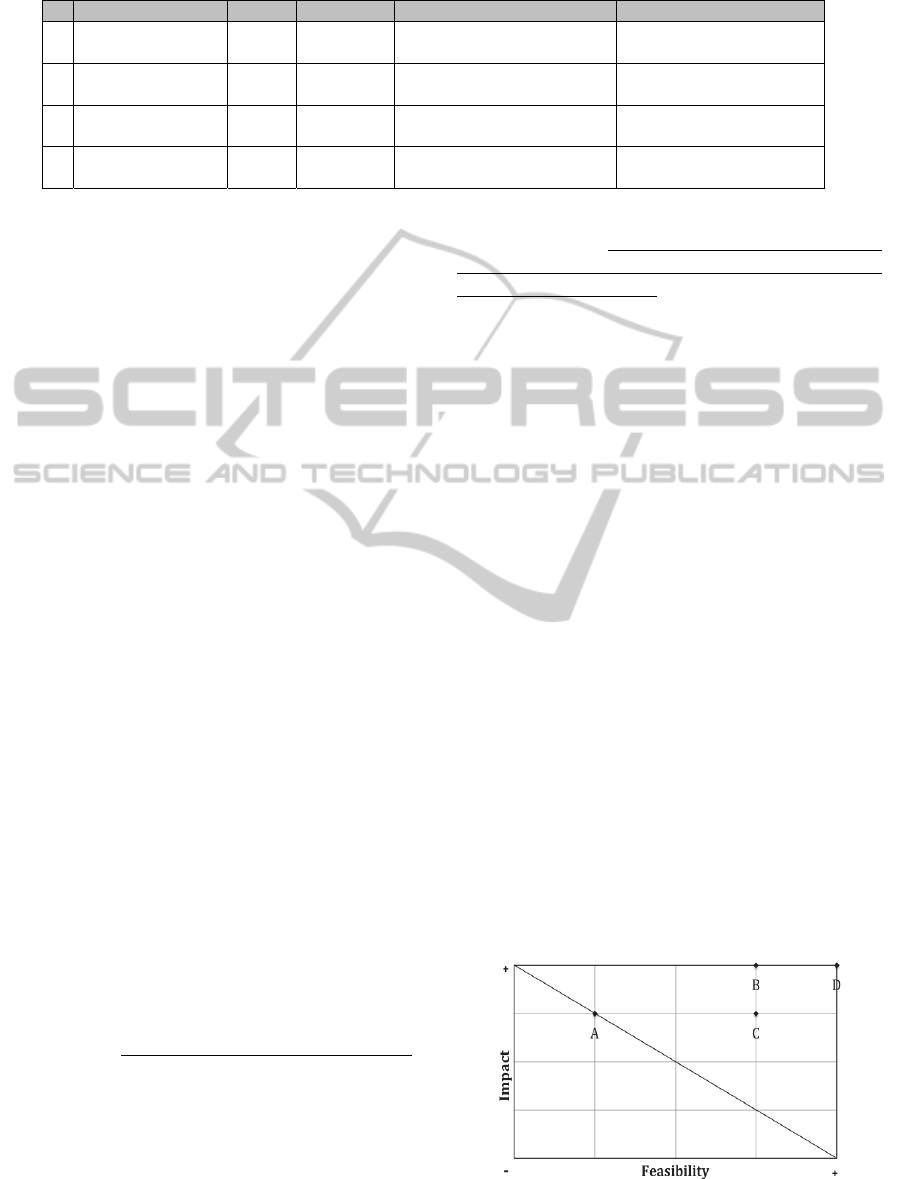
Table 1: Improvements identification in the ED with its corresponding impact and feasibility (from 1 to 5).
that reason. This also means that we can represent
the studied organization with a grey box when
referring to the kernel of the organization, which can
be further specified by using elementary actor roles
represented by white boxes.
As depicted in this model, new patients are
registered to the hospital (T1); then they go through
a triage process (T2); after that, patients’ problems
are handled (T3); and finally, they are discharged
(T11). These four transactions are initiated by an
external actor, the patient. They are respectively
requested to the registrar, triage handler, patient
problem handler, and patient discharger that
execute them.
The handling of the patients’ problems may lead
to the following actions: performing some urgent
internal examinations (T5); performing medical
interventions (T7); performing supplementary
examinations (T9); and consulting another external
specialty (T10). Since these tasks have different
responsibilities, four different actors are discerned:
examiner, intervention performer, external
examiner, and external service or specialist. The
first two are internal actors, used for urgent
examinations and interventions (i.e. specific
interventions may need specialists, such as a surgery
or a psychiatry episode). The last two are used for
non-urgent situations, such as some extended
interventions or supplementary examinations. In
addition, there are two transactions concerning the
delivery of means (T6 and T8), a transaction
concerning the patients’ permission (T4), and finally
the payment transaction (T12).
In the Innovation Phase, one must identify
process improvements from the obtained diagrams.
First, after some analysis from the ATD, one may
conclude that transaction T1 can be removed
(improvement A from Table 1), since the patient can
register during the triage (T2), or at least it is
possible to automate T1 through a computer terminal
with a standardized electronic form (improvement
B). In fact, the secretary performs non-value added
tasks, and consequently this actor could be allocated
to other activities.
With the PSD (obtained from the ATD), one can
conclude that it is not efficient having to go through
several iterations and actors to be forwarded to
another external service (specialist or examiner in
T10). For example, instead of being forwarded
immediately after triage, patients need to be
admitted (T1), triaged (T2), and seen by a physician
(T3) to be finally forwarded to another specialty
outside the ED. This leads to unnecessary
consumption of resources, higher waste of time, and
the patient leaves without being treated in the ED.
There is some related work suggesting strategies of
Fast-Tracking (improvement C) and Provided
Directed Queuing (improvement D) to anticipate the
resolution of some patients’ problems. These
strategies are claimed to improve waiting time,
customer satisfaction, length of stay, and resource
expenditure (Medeiros and et al., 2008).
In Table 1 we quantify the improvements in
which we want to work at. To infer the level of
impact, we consider that the elimination of a
transaction has a higher impact than a precedence
change. Avoiding a transaction conducts to the same
classification as its elimination or automation.
Avoiding an actor has even higher impact, because it
eliminates the transaction and reduces the costs with
human and physical resources. Finally, to assess the
feasibility we considered that more changes to the
service leads to lower feasibility (i.e. hardware,
software or people involved). The presented values
were obtained with the help of the interviewed
practitioners for this demonstration purpose.
Figure 6: Priority Map of the Emergency Department.
# Im
p
rovement Im
p
act Feasibilit
y
Im
p
act descri
p
tion Feasibilit
y
descri
p
tion
A
Patient registers in
the triage
4 2
Avoid transaction T1 and
transfer responsibility to A2
Triage should be fast
B
Automation in the
register of patients
5 4
Avoid transaction T1 and
actor A1
Computer terminal requires
new hardware and software
C
Provided Directed
Queuing
5 5
May eliminate transaction
executions and reduce flow
Reallocate only one
physician
D Fast-Track System 4 4
May eliminate transaction
executions and reduce flow
Reallocate physician and a
new space
UsingEnterpriseOntologyforImprovingtheNationalHealthSystem-DemonstratedintheCaseofaPharmacyandan
EmergencyDepartment
447
The priority map (Figure 6) addresses the impact
and feasibility levels from the last step: D shows
large impact and feasibility, followed by B and C.
We could apply a more formal method for the
improvement quantification, but this would not
change the method itself.
4.2 Pharmacy
Similarly to the previous experiment, we
interviewed 6 practitioners (the pharmacy director,
pharmacists, technicians, and some researchers), to
obtain the enterprise description and validate the
obtained results. These interviews included 50% of
the practitioners from the studied pharmacy, and 2
external and independent practitioners.
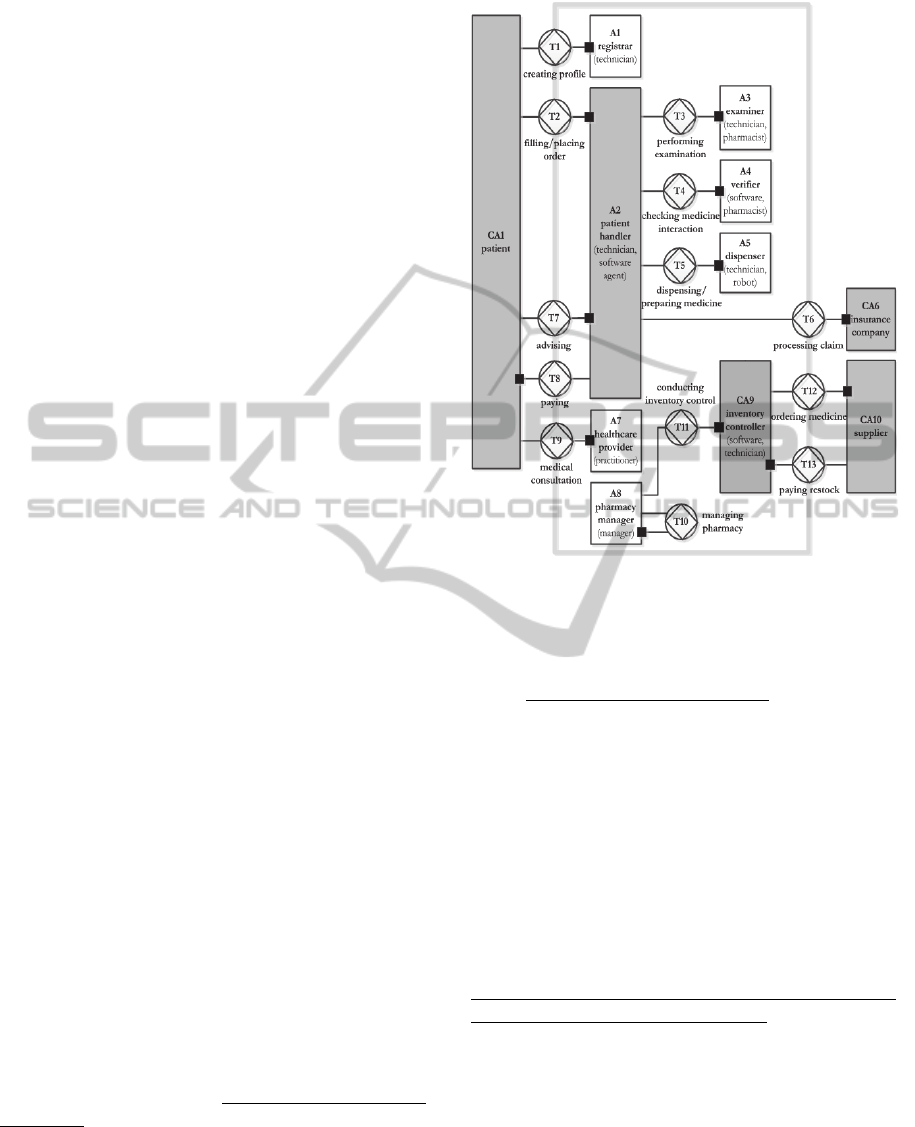
In Figure 7 we present the ATD. As depicted in
this mode, patients may choose to create a profile in
the pharmacy (T1), fill a prescription for a medicine
(T2), get advice about medication or health-related
issues (T7), and attend to a consultation with a
specialist (T8). These transactions are initiated by an
external actor, the patient. They are respectively
requested to the registrar and the patient handler
(composite actor role) that execute them.
The handling of patients may in turn lead to the
following transactions: performing examinations
that can go from a simple diagnostic to laboratory
analysis (T3), checking medicine interactions (T4),
dispensing or preparing medicines (T5) and
processing the claim to check for reimbursements
(T6). Since these actions have different
responsibilities, four different actors roles are
discerned: examiner, verifier, dispenser, and
insurance company (external actor role). After
handling patients, they have to pay for the medicines
or the provided services (T9).
In addition, there are transactions concerning the
pharmacy management (T10), the inventory control
(T11), the medicine supply (T12), and their payment
(T13). Three action roles are discerned: pharmacy
manager, inventory controller, and supplier. Finally,
it is possible to schedule some kinds of medical
appointments in the pharmacy with paramedics or
other healthcare professionals. This corresponds to
the transaction T8 executed by the patient handler.
In the Innovation Phase we identified four main
improvements. First, the transaction T11 can be
automated (improvement A from Table 2), since the
inventory control process requires more human
intervention, but does not consider demand
forecasting due to the lack of decision support
systems. In addition, there is a need to verify the
arrival of products manually to check their prices,
Figure 7: Actor Transaction Diagram (ATD) of the
Pharmacy.
quantities and expiration dates.
The second main improvement (improvement B)
is the automation of transaction T5 to use a robot
instead of a human to dispense or prepare medicines.
Despite being a well-known and documented
improvement, our analysis revealed that this was a
bottleneck with great impact in the number of
employees and service time. Without a robot, a
pharmacy needs more employees available and there
is a higher waiting-time to get medicine. They also
help in the storage of the ordered medicines, and
help identifying drugs that are almost expiring
(without any human intervention), which reduces the
waste of products.
The third improvement (improvement C) is the
overlapping of responsibilities between hospitals and
pharmacies in T2, T3 and T8. In spite of
pharmacists’ skills, patients need to seek a physician
or a hospital to have a prescription, even for
recurring or vulgar situations, such as an antibiotic.
In addition, there are other legal restrictions
hampering the existence of medical consultations or
specialties in the pharmacies. This overlapping and
the need to resort to hospitals are considered to
increase the cost of the national healthcare system
(Walshe et al., 2010).
The last improvement (improvement D) is the
KEOD2012-InternationalConferenceonKnowledgeEngineeringandOntologyDevelopment
448
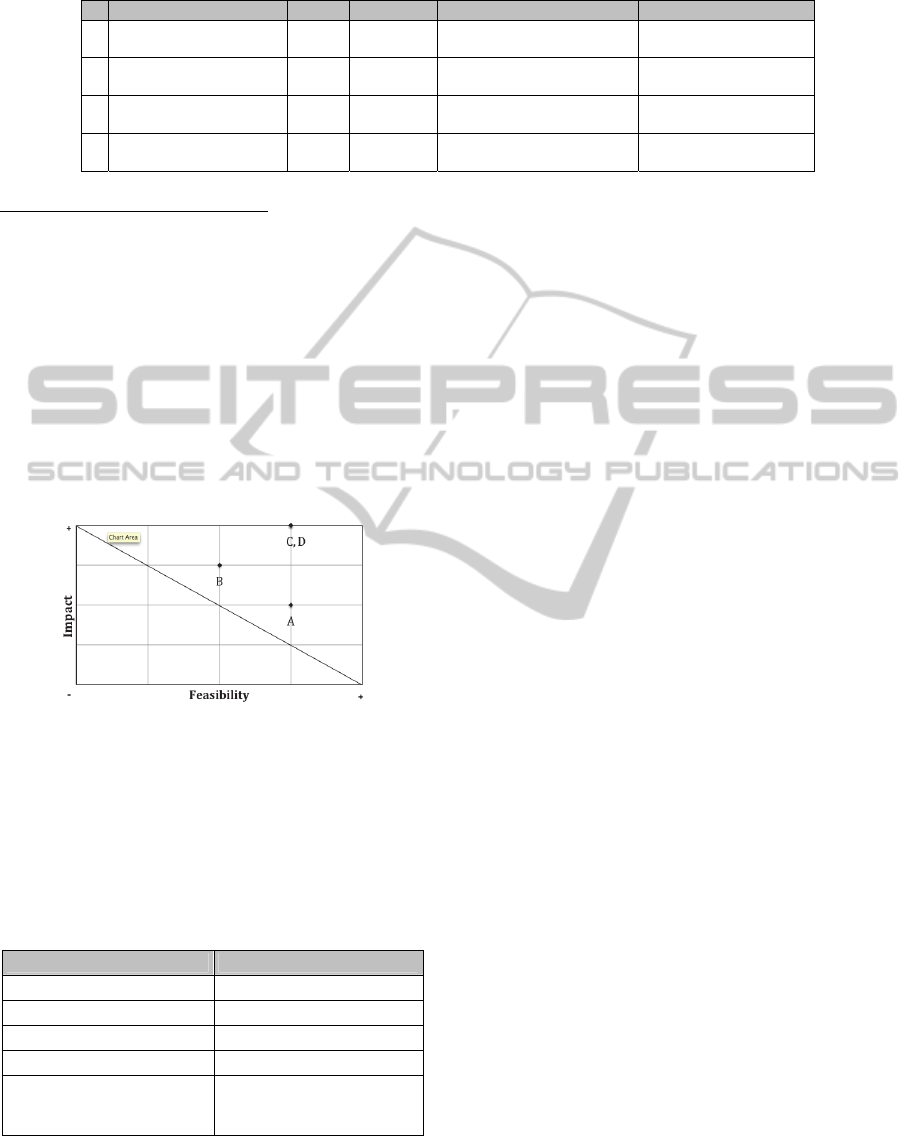
Table 2: Improvements identification with its corresponding impact and feasibility (from 1 to 5).
elimination of the transaction T1, since there should
be a unified Patient Healthcare Record for all
healthcare organizations, to avoid duplication of
information, improve access to information, and
avoid wasting time creating profiles in different
healthcare organizations (Dias et al., 2012).
In Table 2 we quantify the improvements in
which we want to work. To infer the level of impact,
we consider the same assumptions described in
Section 4.1. The priority map (Figure 8) shows that
improvements C and D have a larger impact and
feasibility, followed by B and A. Again we could
apply a formal method for the quantification, but this
would not change the method itself.
Figure 8: Priority Map of the Pharmacy.
To sum up, we may conclude that there is room
for improvements in the ED and the Pharmacy.
Analyzing those results together we also may find
that it is possible to improve their cooperation since
we find some overlapped transactions (Table 3).
Table 3: Overlapped transactions between ED and
Pharmacy.
ED Transactions Pharmacy Transactions
T1 – Register Patient T1 – Creating Profile
T3 – Handling Patient T2 – Filling prescription
T3 – Handling Patient T9 – Medical Consultation
T5 – Performing Examin. T3 – Performing Examin.
T6, T8, T12 – Management
and stock supply transactions
T10 to T12 – Management
and stock supply
transactions
From the previous table we may find that both
organizations would benefit from having a unified
Patient Healthcare Record to avoid the creation of
new registers. In both organizations their
professionals have studies and skills to prescribe
medications, but only physicians may do it due to
legal reasons in Portugal, and both organizations
share some exams and medical specialties.
5 EVALUATION
This section corresponds to the evaluation step of
DSRM.
To evaluate the proposal, we used the framework
proposed in (Pries-Heje, Baskerville and Venable,
2004), which aims to help researchers to build
strategies for evaluating the outcome of a DSRM.
This framework identifies what is actually
evaluated, when the evaluation takes place, and
how it is evaluated. To answer the third question,
we based on different authors to propose a strategy
with steps outlined to evaluate a DSRM artifact
method. The evaluation strategy entails the
following steps: 1) Constructing scenarios to
demonstrate the artifact and how to use it to solve
the research question; 2) Feedback through
interviews with practitioners; 3) The Moody and
Shanks Quality Management Framework to
assess the quality of the produced models (Moody
and Shanks, 2003); and 4) The Four Principles
proposed by (Österle et al., 2011) to evaluate a
DSRM artifact.
This evaluation method follows the design
evaluation guideline within DSRM (Henver and et
al., 2004). In this research we have mainly used the
descriptive evaluation method to assess the artifact,
which uses relevant research to build a convincing
argument for the artifact’s utility, and constructs
detailed scenarios around the artifact to demonstrate
the utility. Nevertheless, the observational and
analytical methods could also be used, but this
would involve introducing observable metrics,
conducting socio-technical experiments, and
selecting modeling tasks that would allow such
measurement (Henver et al., 2004; Caetano, 2008).
Such evaluation is beyond the scope of this research.
# Im
p
rovement Im
p
act Feasibilit
y
Im
p
act descri
p
tion Feasibilit
y
descri
p
tion
A
Automation in the
inventory control
3 4
Reduce waste of time, avoid
errors in inventory control
Improve Supply Chain
Management software
B
Automation in medicine
preparation or dispense
4 3
Avoid human intervention,
reduce waste of time
New hardware (robot)
and software
C
Avoid overlapping of
responsibilities
5 4
Avoid duplication/overlap of
transactions, reduce spending
Need to change rules,
change resistance
D
Eliminate profile creation
(unified patient records)
5 4
May eliminate transactions
and reduce flow
Change legal restrictions,
change resistance
UsingEnterpriseOntologyforImprovingtheNationalHealthSystem-DemonstratedintheCaseofaPharmacyandan
EmergencyDepartment
449

The framework proposed in (Pries-Heje et al.,
2004) was formulated as follows:
What was actually evaluated? The
evaluated artifact was the method described
in Section 3, which is a DSRM artifact
method. This evaluation represents an
artifact design process, since it is defined as
a set of activities, methods and practices that
can be used to guide a procedure workflow to
improve the healthcare management;
When was it evaluated? It was evaluated
after the artifact construction, and after the
demonstration. Therefore, the evaluation
strategy is ex post, since it was performed
after the design artifact development;
How is it evaluated? To evaluate the artifact
and its results we used the described strategy,
which are applied below. This represents a
naturalistic evaluation since it is conducted
using a real artifact in a real organization
facing real problems as a case of study.
The demonstration reveled that: A) The
proposal is generic enough to be applied in different
healthcare organizations; B) It is a formal method,
with a list of specific steps to follow; C) From a
given enterprise description anyone can achieve
similar enterprise models, as Dietz suggests (Dietz,
2006); D) From the obtained models it is possible to
find non value-added transactions and from them
suggest and prioritize improvements; and F) It is
possible to obtain a redesigned organization. In other
words, it was possible to demonstrate the artifact’s
utility, and how to use it to solve the research
problem.
The feedback from the interviews (using the
same practitioners referred to in the Demonstration)
was rather positive because: 1) They validated the
importance of the research problem and the
motivations behind the proposal; 2) They understood
and agreed with the obtained models (after
explaining them), which were considered to properly
depict the studied organizations; 3) Improvements
were discussed and the interviewees agreed that the
ones we identified were sometimes similar to those
suggested by them; 4) Practitioners concluded that
the proposal could be applied effectively and
efficiently to solve the research problem, regardless
of whom applies it. Overall, practitioners showed a
good acceptance and enthusiasm for this innovative
approach.
From the Moody and Shanks Quality
Framework, almost all quality factors were
accomplished. Only understandability was partially,
and implementability was not. The first factor as
practitioners find models difficult to interpret
needing an adaptation period. The second one as
models are implementation independent (describing
only the essence of organizations).
The Four Principles from (Österle et al., 2011)
were also accomplished. 1) Abstraction: the artifact
can be applied to any healthcare service from a
given enterprise description; 2) Originality: the
proposed artifact is not present in the body of
knowledge of the domain since it was designed by
relating different subjects, such as healthcare
management, BPR, EO and Lean; 3) Justification:
the artifact is supported by the related work,
described by textual and graphical representations,
and it was justified and validated in different ways;
4) Benefit: the artifact provides a structured working
approach for reengineering, it leads to differentiated
and well-grounded improvements, and provides a
better understanding of the dynamics of an
organization, among other benefits when compared
to existing methodologies.
6 CONCLUSIONS
Considering this research’s objectives and
evaluation, we may conclude that the expectations
were largely achieved since it was possible to: a)
Formulate the method; b) Demonstrate its use in two
real case studies; c) Find non value-added
transactions when applying it; d) Suggest redesign
improvements; and e) Get validation and positive
feedback from practitioners about the method and its
results.
We may also conclude that it is possible to easily
identify redesign innovations to solve overlapping
issues in organizations, since DEMO is regarded as a
methodology that produces models considered
concise and essential, which help to construct and
analyze more models in a shorter period of time. In
addition, because the designs are also considered
coherent, comprehensive and consistent, this gives
strength to the obtained models, as described in
(Dietz, 2006).
To conclude, it is expected that healthcare
organizations may use some of the described
advantages of the proposal to solve the problems of
inefficiency and unsustainability in the healthcare
system. Furthermore, it can also be a contribution
towards helping the healthcare professionals to
validate processes and improve their way of
working, even if the proposed artifact is used
together with other existent methods.
To sum up, we may answer to the raised problem
and objective statements that: 1) It is possible to use
KEOD2012-InternationalConferenceonKnowledgeEngineeringandOntologyDevelopment
450

the EO to propose improvements in the National
Health System; and 2) It is possible to create a
DEMO based method to find non value-added
transactions that could be redesigned.
To complete the cycle of the DSRM, the
communication step is being achieved through
scientific publications and their presentation, aimed
at the practitioners and researchers within the
science area.
As future work, further research is being
performed to better quantify the impact and
feasibility of the proposed improvements during the
demonstration, namely by including costing models
to the obtained DEMO diagrams. Furthermore, the
proposal should be expanded to consider the
remaining application of Lean PDCA cycle and
other EO models, such as Action and Interstiction
Models, which can be useful in the redesign of
information systems (inline with previous researches
(Reijswoud et al., 1999)).
REFERENCES
Burgess, N. and Radnor, Z. J. (2010) 'How is lean being
applied to health? Classifying approaches to lean
implementation in the NHS', The 14th Annual
International Research Society for Public
Management (IRSPM) Conference, Berne.
Christensen, C. M., Grossman, J. H. and Hwang, J. (2009)
The Innovator's Prescription - A disruptive solution for
Health Care, New York: McGraw Hill.
Dias, D., Lapão, L., Silva, M. and Helfert, M. (2012)
'Using Enterprise Ontology for Improving Emergency
Management in Hospitals', 24th European Medical
Informatics Conference, Pisa. Accepted in 2012.
Dias, D., Xie, S. and Silva, M. (2012) 'Using Enterprise
Ontology Methodology to Assess the Quality of
Information Exchange', 18th Americas Conference on
Information Systems, Seattle. Accepted in 2012.
Dietz, J. (2006) Enterprise Ontology - Theory and
Methodology, Delft: Springer.
Dietz, J. and Hoogervorst, J. (2008) 'Enterprise Ontology
in Enterprise Engineering', ACM Symposium on
Applied Computing, New York, 572-579.
Fillingham, D. (2007) 'Can lean save lives?', Leadership in
Health Services, UK, 231-241.
García-Porres, J; et al. (2008) 'Lean six sigma applied to a
process innovation in a mexican health institute's
imaging department', 30th Annual International IEEE
EMBS Conference, 20-24 August, pp. 5125-5128.
Habing, N. et al. (2001) 'Activity patterns in healthcare -
indentifyinf building blocks for the CPR', ACM
SIGGROUP Bulletin, vol. 22, August.
Henriques, M., Tribolet, J. and Hoogervorst, J. (2010)
'Enterprise Governance and DEMO: a reference
method to guide enterprise (re)design and operation
with DEMO', CAPSI, Viana do Castelo.
Henver, A. et al. (2004) 'Design Science in Information
Systems Research', MIS Quartely, vol. 28, no. 1, pp.
75-105.
Hines, P., Holweg, M. and Rich, N. (2004) 'Learning to
evolve: A review of contemporary lean thinking',
International Journal of Operations and Production
Management, vol. 24, no. 10, pp. 994-1011.
Kaplan, R. and Porter, M. (2011) 'How to solve the cost
crisis in health care', Harvard Business Review,
September.
Kotter, J. (1996) Leading Change: Why Transformation
Efforts Fail, Boston: Harvard Business School Press.
Laudon, K. and Laudon, J. (2010) Management
Information Systems, New Jersey: Pearson.
Lifvergren, S. et al. (2010) 'Lessons from Sweden's first
large-scale implementation of Six Sigma in
healthcare', Springer, pp. 117-128.
Maij, E. et al. (2000) 'A process view of medical practice
by modeling communicative acts', Methods of
Information in Medicine, pp. 56-62.
Maij, E. et al. (2002) 'Use cases and DEMO: aligning
functional feautures of ICT-infrastructure to business
processes', International Journal of Medical
Informatics, pp. 179-191.
Medeiros, D. et al. (2008) 'Improving patient flow in a
hospital emergency department', Winter Simulation
Conference, Austin, 1526-1531.
Mendes, C., Ferreira, J. and Silva, M. (2011) 'Comparing
Service Using DEMO', Paris.
Mendes, C., Ferreira, J. and Silva, M. (2012) 'Identifying
Services from a Service Provider and Customer
Perspectives',
Communications in Computer and
Information Science, Springer. Accepted in 2012.
Mintzberg, H. (1994) 'The rise and fall of strategic
planning', New York.
Moody, D. and Shanks, G. (2003) 'Improving the Quality
of Data Models: Empirical Validation of a Quality
Management Framework', Information Systems, vol.
28, pp. 619-650.
OECD (2012), http://stats.oecd.org/ [Feb 2012].
Österle, H. et al. (2011) 'Memorandum on Design-
Oriented Information Systems Research', European
Journal on Information Systems, vol. 20, pp. 7-10.
Pries-Heje, J., Baskerville, R. and Venable, J. (2004)
Strategies for Design Science Research Evaluation,
16th European Conference on Information Systems,
pp. 255-266.
Radnor, Z. (2010) 'Transferring Lean in to Government',
Journal of Manufacturing and Technology
Management, vol. 21, pp. 411-428.
Reijswoud, V., Mulder, H. and Dietz, J. (1999)
'Communicative Action Based Business Process and
Information Systems Modelling with DEMO',
International Journal of Information Systems.
Walshe, K. and Smith, J. (2010) Healthcare Management,
Berkshire: Open University Press.
UsingEnterpriseOntologyforImprovingtheNationalHealthSystem-DemonstratedintheCaseofaPharmacyandan
EmergencyDepartment
451
