
Voluntary Eye Movement Patterns while Viewing
Müller-Lyer Illusion
A New Screening Method for Scotoma Patients
Mika Haapala
1
, Antti Rantanen
1
, Aura Falck
2
, Anja Tuulonen
3
, Eero Väyrynen
4
, Tapio Seppänen
4
and Seppo J. Laukka
1
1
Learning Research Laboratory, University of Oulu, Oulu, Finland
2
Department of Ophthalmology, Oulu University Hospital, Oulu, Finland
3
Tays Eye Centre, Tampere University Hospital, Tampere, Finland
4
Department of Computer Science and Engineering, University of Oulu, Oulu, Finland
Keywords: Scotoma, Screening, Eye Movement Pattern, Müller-Lyer Figure.
Abstract: Diabetic maculopathy and especially advanced glaucoma are the most common eye diseases involving
scotomas, blind spots in the visual field. The risk of having scotomas increases significantly with age and
over 60 million people worldwide suffer from different forms of glaucoma of whom at least are half are not
aware of the eye disease. One of the most common scotoma diagnosis tests is perimetry, a visual field test,
which produces a complete map of the visual field, but may not be suitable for large screening of
population. We are aiming to develop a new portable screening device for cost effective screening of eye
diseases. We studied voluntary eye movement patterns evoked by Myller-Lyer illusion figure. Our study
material included six scotoma patients (two with Maculopahia Diabetica, and four with Glaucoma simplex)
and six control subjects. We recorded eye movement patterns with a portable Tobii T120 eye-tracker system
on which a Müller-Lyer figure was projected. As a result, the variation of the y-component of the eye
movement trajectory indicates that the scotoma subjects had more vertical variation in their eye movement
pattern than the control subjects (P< .01). The preliminary experiment suggests that further prospective
studies using our method of analyzing eye movement patterns is warranted with larger sampale sizes and
different types and stages of defects.
1 INTRODUCTION
Visual field defects are common consequences of
different eye diseases. There are different types of
defects, e.g. altitudinal field defects, bitemporal and
homonymous field defects as well as peripheral and
central scotomas. Earlier studies have shown that
patients with central scotoma develop different
fixation (i.e. during fixation the eye is maintained on
a single location) strategies to compensate their
impaired visual field (Sunnes et al., 2005);
(Schuchard, 2005); (Duret et al., 1999). These
fixation strategies involve the use of preferred retinal
locus (PRL). By using PRL, a patient can fixate the
seeing retina on to the object of interest so that the
scotoma is moved away from the object of interest.
We hypothesized that special eye movements related
to these strategies could be detected from the eye
movement data while viewing a visual illusion
figure.
In visual illusion the visual sensation differs
from reality (Gregory, 1998). One of the most
studied visual illusions is a century old Müller-Lyer
illusion. Even though it has a long history of study,
its mechanism is still obscure (Bodanko et al., 2009).
Müller-Lyer illusion is also known as an arrow
illusion. A line with arrow heads pointing out (i.e.
closed part of the figure) looks shorter than a line
with arrow heads pointing in (i.e. open part of the
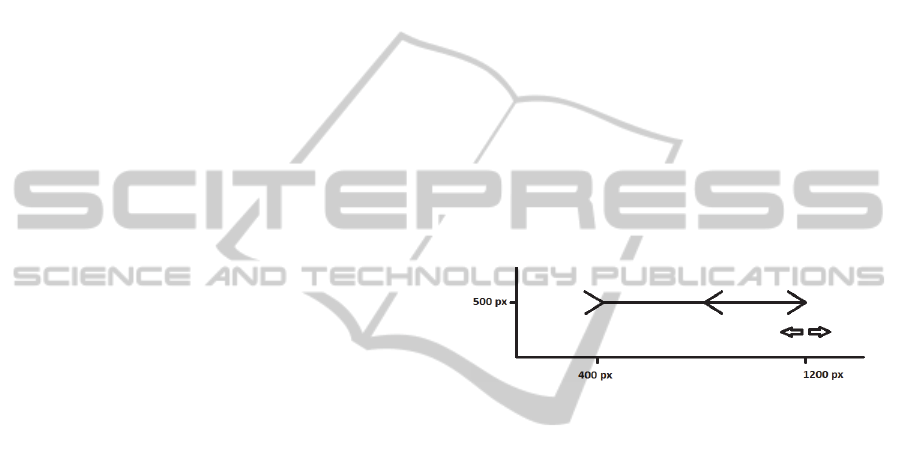
figure). We used the so called Brentano version in
which the arrow heads are drawn on to a single line
(Fig. 1). We use this well-known illusion
innovatively to evoke voluntary eye movements
while viewing the illusion and, further, to compare
the eye movement data between people with and
without central scotoma.
267
Haapala M., Rantanen A., Falck A., Tuulonen A., Väyrynen E., Seppänen T. and J. Laukka S..
Voluntary Eye Movement Patterns while Viewing Müller-Lyer Illusion - A New Screening Method for Scotoma Patients.
DOI: 10.5220/0004188202670270
In Proceedings of the International Conference on Bio-inspired Systems and Signal Processing (BIOSIGNALS-2013), pages 267-270
ISBN: 978-989-8565-36-5
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)
Diabetic maculopathy and especially advanced
glaucoma are typical eye diseases causing central
scotoma. The damage inflicted by glaucoma is
related to optic nerve head, nerve fiber layer and
visual field. Too high intraocular pressure destroys
retinal fiber pathways leading to defects on the
visual field (scotomas) starting typically from the
peripheral visual field. It has been estimated that
glaucoma is one of the leading causes of blindness
together with diabetic eye disease. The risk of
having glaucoma increases significantly with age.
Some 60 million people worldwide suffer from the
disease, half of them unawares. Demographical
studies and screenings of population have shown
that especially open angle glaucoma patients have
not been detected by the opportunistic case finding
and there is lack of simple appropriate screening
methods (Wong, 2004).
One of the most common glaucoma diagnostic
test is perimetry, a visual field test, which produces
map of the visual field (Humphrey´s and Octopus
static perimetries and Goldmann´s kinetic
perimetry). These methods have been approved for
clinical studies, but they may not be suitable for
large screening of the population.
Our aim was to test the hypothesis and develop a
new method of collecting and analyzing eye
movement data in order to advance the development
of a new portable screening device for patients with
central scotoma patients.
2 MATERIALS AND METHODS
2.1 Data Collection
Total of 12 voluntary subjects participated in the
experiment: six scotoma patients and six control
subjects. Two of the six scotoma patients were
diagnosed with Maculopahia Diabetica and four
patients were diagnosed with Glaucoma simplex.
The scotoma patients were recruited at routine
checkups at the University Hospital of Oulu. The
scotoma group included 4 male and 2 female
patients aged between 30 and 74 years, with the
mean 62.8 years.
The control group consisted of 3 male and 3
female students and faculty members of the
University of Oulu who were aged between 23-30
years with the mean 27.2 years.
The eye movements of the subjects were
recorded using a Tobii T120 Eye Tracker. Tobii
T120 records eye movements using an enhanced
version of the commonly used Pupil Centre Corneal
Reflection (PCCR) technique. The resolution of the
Tobii T120 tft-display, on which the Müller-Lyer
figure (M-L) was presented, was 1280x1024 pixels.
The line length of the presented M-L figure was 22.5
cm and the line thickness was 0.79 mm, see Fig. 1.
The M-L illusion figure consisted of a starting error
of 7.5 cm: the closed part of the figure was two
times longer than the open part of the figure. The
starting error was added in order to clearly show that
the line which was to be adjusted, with closed
arrowheads, was considerably longer than the line
with open arrowheads. The visual angle of the
presented M-L figure was 21.2 degrees (i.e. the
angle opening from the viewer towards the ends of
the line). The angle of the M-L figure arrow head
was 45 degrees and its length was 2cm. The sample
rate of the Tobii T120 Eye Tracker was 17 ms (60
Hz). The eye tracker was controlled by a laptop
computer. The M-L figure was presented on the eye
tracker screen by EMMI® software (LudoCraft Ltd,
Oulu, Finland).
Figure 1: Brentano version of the Müller-Lyer figure as
presented on screen. The closed side was adjusted.
The subject was sitting approximately 60 cm
from the Tobii T120 tft-monitor. A total of five right
pointing M-L figures were presented consecutively
on the screen using EMMI® software. The subject
was instructed to adjust M-L figure´s lines to be
equally long using the left and right arrow buttons of
a keyboard. After the adjustment of each M-L
figure, the subject had to press the enter-key.
2.2 Data Processing
Each Tobii T120 recording consists of a sequence of
triplets (t,x,y) following the eye movement
trajectory on the monitor, in which t is the
timestamp and x/y are the coordinates of a trajectory
point. These data points were further assigned to the
same fixation if the velocity remained below a
threshold of 30 degrees per second. In addition, the
maximum allowed time between fixations was set to
75 milliseconds and the maximum allowed angle
between fixations was set to 0.5 degrees; and the
minimum allowed fixation duration was set to 60
milliseconds.
EMMI® software recorded the participants’
BIOSIGNALS2013-InternationalConferenceonBio-inspiredSystemsandSignalProcessing
268

visuo-motor activity and the magnitude of the
illusion at a sample rate of 17 ms (60 Hz). The data
from the Tobii eye tracker and EMMI® software
were integrated and synchronized with an algorithm
written in Matlab programming language.
Several indices of eye movement dynamics were
computed for both eyes while watching the M-L
figures: the illusion magnitude, the number of
fixations, the duration of fixation, the standard
deviation of the vertical direction on the display, and
the standard deviation of the horizontal direction on
the display. Differences between the groups were
analyzed statistically using the Mann-Whitney U –
test.
3 RESULTS
First we compared the magnitude of illusion, the
mean number of fixations and fixation durations
between the Scotoma Group and the Control Group.
Table 1 shows that the illusion magnitude was
higher in the Scotoma group (M=38.03%,
SD=35.30) than in the Control group (M=35.57%,
SD= 14.26) but the differences were not statistically
significant. The mean number of fixations in the
Scotoma Group was 307.83 (SD= 118.16), and in
the Control Group 221.17 (SD= 73.70). There was
no statistical difference between the groups. The
mean duration of fixations was significantly longer
in the Scotoma Group (M=774.50 ms, SD=221.03)
than in the Control Group (M=527.33 ms,
SD=138.11) with P<.01.
Table 1: Illusion magnitudes, mean number of fixations,
and mean duration of fixations (** P< .01).
Groups Magnitude %
Mean number
of fixations
Mean duration
of fixation, ms
Scotoma Group 38.03 % 307.83 774.50**
Control Group 35.57 % 221.17 527.33
Figure 2: Scatter dot chart of the eye movements (i.e. eye
positions in pixels, y- versus x-coordinates) for the
Scotoma Group (right eye on the left; left eye on the
right).
Figure 3: Scatter dot chart of the eye movements (i.e. eye
positions in pixels, y- versus x-coordinates) for the
Control Group (right eye on the left; left eye on the right).
Then we compared the standard deviations of x-
and y-coordinates separately (i.e. eye movements)
between the groups. The most significant difference
in the eye movement data was the variance in the y-
component of the eye movement trajectory over the
M-L figure. For visualization purposes scatter dot
charts of both eyes were drawn separately for both
groups (see Fig. 2 and Fig. 3).
The standard deviation of y-coordinate was
significantly greater in the Scotoma Group than in
the Control Group in both eyes (P< .01) (see Table
2).
Table 2: Standard deviations of y-coordinates of the eye
movement trajectories for the Scotoma Group and the
Control Group, subjects presented separately.
Subjects Scotoma Group Control Group
Right eye SD (pixels) SD (pixels)
1 60.2 24.22
2 73.46 21.95
3 58.6 24.5
4 69.33 17.96
5 35.63 19.03
6 69.3 18.78
Left eye SD (pixels) SD (pixels)
1 69.12 25.39
2 38.1 20.92
3 41.34 23.24
4 64.91 20.55
5 36.01 18.37
6 69.96 17.82
The standard deviations of the x-coordinates of
the right and left eye did not differ between the
groups (see Table 3).
4 CONCLUSIONS
We recorded voluntary eye movements of the
Scotoma group and the Control group, consisting of
six subjects each, while viewing the Müller-Lyer
illusion figure. We analysed the data in regards to
illusion magnitude, number and duration of fixations
and the x- and y-coordinates of the eye’s trajectories
across the screen and compared these parameters
VoluntaryEyeMovementPatternswhileViewingMüller-LyerIllusion-ANewScreeningMethodforScotomaPatients
269
between the Scotoma and Control groups.
The main novel finding was that the eye
movement dynamics differ significantly between the
Scotoma and the Control group. This observation
was confirmed with two interrelated parameters: the
vertical variation of eye trajectories over the
M-L figure (P<.01) and the fixation duration
(P<.01).
The different trajectories are an indication of
compensatory eye movements: Scotoma patients
compensate their visual field deficiencies with
abnormal eye movement trajectories. The longer
fixation duration is also an indication of
compensation for scotomas in the Scotoma Group
(Duret et al., 1999).
The presented novel method warrants further
research with larger sample size as well as different
types and stages of eye diseases.
Table 3: Standard deviations of the x-coordinates of the
eye movement trajectories for the Scotoma Group and the
Control Group, subjects presented separately.
Subjects Scotoma Group Control Group
Right eye SD (pixels) SD (pixels)
1
184.71 177.17
2
179.59 204.13
3
198.02 220.03
4
263.45 228.36
5
181.59 170.24
6
261.28 189.45
Left eye SD (pixels) SD (pixels)
1
186.51 172.34
2
165.09 201.16
3
183.95 223.07
4
284.06 235.73
5
179.03 166.59
6
246.01 186.18
REFERENCES
Bodanko, V. M., Semenov, L. A., 2009. Perception of
Visual Image Size by School Students of Different
Ages. Human Physiology, 2009, vol. 35, No. 1, 15-19.
Developing the clinical components of a complex
intervention for glaucoma screening trial: a mixed
method study. BMC Medical Research Methodology
2011, vol. 11, iss. 1, 54-63.
Duret, F., Buquet, C., Charlier, J., Mermoud, C., Viviani,
P. Safran, A. B., 1999. Refixation strategies in four
patients with macular disorders. Neuro-
Ophthalmology, 1999, vol. 22, No. 4, s. 209-220.
Gregory, R., L., 1998. Visual illusion. In: Gregory R., L.
(Ed.). The Oxford companion to the mind. New York:
Oxford university press.
Schuchard, R. A., 2005. Preferred retinal loci and macular
scotoma characteristics in patients with age related
macular degeneration. Canadien Journal of
Ophthalmology; 40:303-3012.
Sunnes, J. S., Applegate, C. A., 2005. Long-Term Follow-
up of Fixation Patterns in Eyes With Central Scotomas
From Geographic Atropy That Is Associated With
Age. Related Macular Degeneration. American
Journal of Ophthalmology 2005;140:1085-1093.
Wong, E. Y. H., Rait, J. E. J. L., Vu, H. T. V., Le, A.,
McCarry, C.. Detection of Undiagnosed Glaucoma by
Eye Health Professionals. Ophthalmology
2004;111:1508-1514.
BIOSIGNALS2013-InternationalConferenceonBio-inspiredSystemsandSignalProcessing
270
