
Electronic Health Records Research in a Health Sector Environment
with Multiple Provider Types
Samantha S. R. Crossfield and Susan E. Clamp
Leeds Institute for Health Sciences, University of Leeds, 101 Clarendon Road, Leeds, U.K.
Keywords: Research Database, Shared Health Records Access, EPR, Patient Record Access, Researchone, Multiple
Health Providers, Clinical System, Database Validation.
Abstract: Where healthcare provision is divided into provider types, such as child health and palliative care, it is
difficult for researchers to access comprehensive healthcare data. Integrated electronic health records offer
an opportunity for cross-provider type care research. In this paper a new model for accessing such data is
justified using the critical success factors as determined from an established research data provider. This
validates a model that will enhance integrated health research for the benefit of clinical practice across
multiple provider types.
1 INTRODUCTION
In gaining health and social data for research, and
transferring results into clinical practice, the
consideration of multiple health provider types that
are treating a patient is often relevant and yet
receives little attention. Electronic health record
(EHR) data is increasingly being used in research
due to their widespread use in clinical practice for
gathering detailed and structured data. EHRs are
often non-shareable, used in only the health unit that
generated them, such as a general practice or a
hospital ward (ISO/TR 20514, 2004). Such records
cannot comprehensively represent to the research
community the health of patients who receive care in
multiple settings. Alternative structures with EHR
data sharing between clinicians at different health
units can improve clinical practice and reduce errors
(Twomey et al., 2004); (Ammenworth et al., 2008).
Research on integrated EHRs has enhanced
healthcare through investigating clinical practice
through a whole systems approach. Research using
integrated EHRs in England has nonetheless
remained infrequent due to accessibility issues.
Health care in many countries including Spain,
UK and Germany is delivered through multiple
provider types working with independence. These
care providers struggle with an outcome of this
specialisation which is often termed ‘silo working’
wherein service deliverers with different aims and
professional languages gather information on
separate aspects of patient care (Wilson et al., 2007);
(Kawonga et al., 2012) and store these in unrelated,
closed silos. These records may not be shared with
other health units, let alone across provider types. As
a consequence each unit holds partial patient records
rather than the entirety of the patient’s medical
history. With closed systems it becomes difficult to
share timely and pertinent information, such as
diagnoses, allergies, medication and professional
insights with other healthcare providers that are also
intervening with and monitoring the health of the
patient. This results in issues of duplication and
missing data. Patient information held in such silos
provides less support to patients that cross care
provider types and reduces the capacity to perform
longitudinal assessments (Kuperman, 2011).
This silo issue is also of relevance for the
research community who consider patient health in
an array of fields including health informatics,
epidemiology, health economics, clinical care and
medicine. Traditional data collection involves such
invasive, timely and resource-intensive methods as
conducting interviews and questionnaires. The
increasingly routine use of EHRs in clinical practice,
including by 76% of European general practitioners
(Dobrey et al., 2008), makes EHRs an efficient
source of large cohort research data. The capacity
for large EHR cohorts facilitates research on low
frequency incidences or diagnoses. This enabled
identification of the correlation between emergency
104
S. R. Crossfield S. and E. Clamp S..
Electronic Health Records Research in a Health Sector Environment with Multiple Provider Types.
DOI: 10.5220/0004245701040111
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2013), pages 104-111
ISBN: 978-989-8565-37-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)
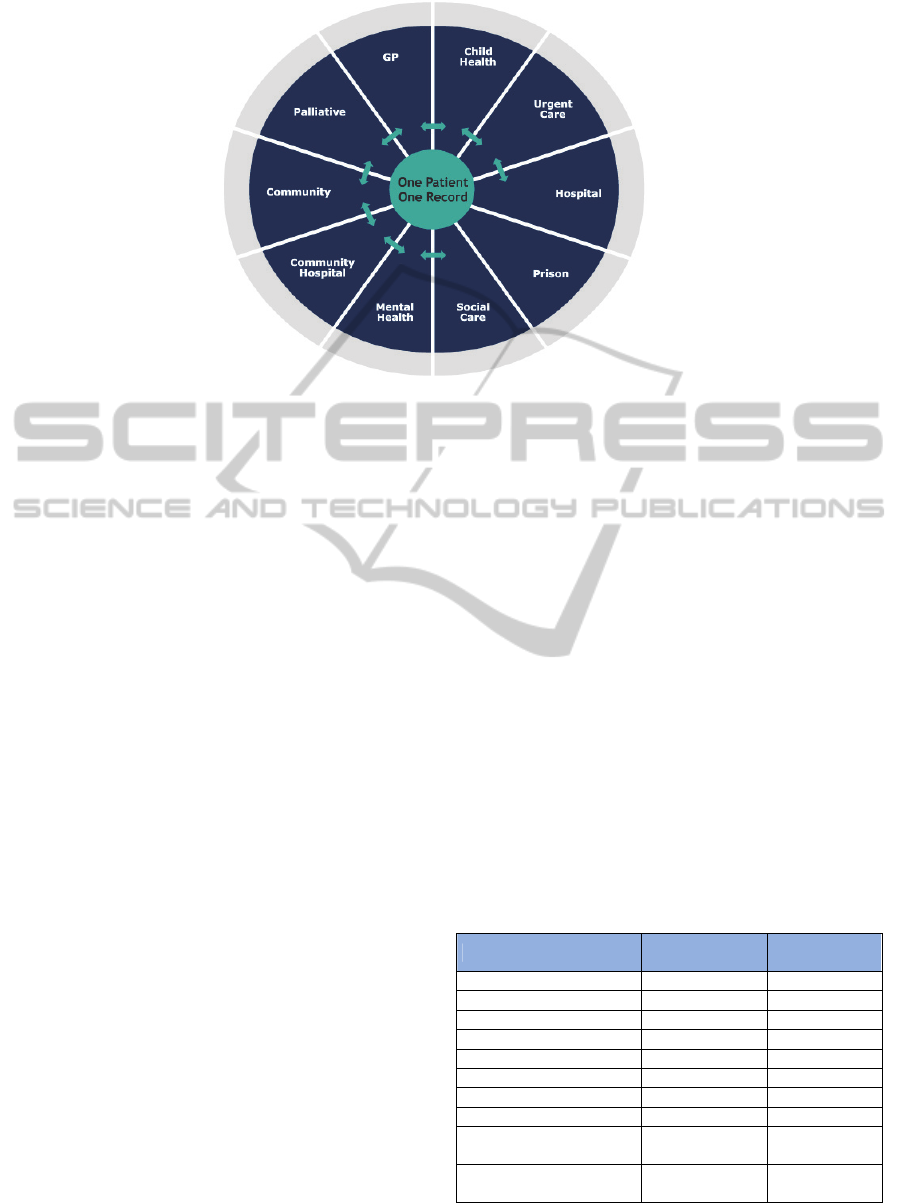
Figure 1: Healthcare provider types in which SystmOne is used and between which information can be shared with the
exception of prison data. In hospitals SystmOne provides patient administration, clinical record viewing, bed management,
accident and emergency, e-prescribing and e-discharge.
department waiting times and outcomes of mortality
and readmission, identified using the records of over
14.5 million emergency department attendances
(Guttmann et al., 2011). However patient data
dispersal in EHRs across multiple provider types
necessitates the requirement of identifiable data for
undertaking data linkage. This brings security issues
and the time taken to gather and link siloed data
reduces the timeliness of cross-provider research.
Further time on the part of the researchers and the
data providers is required to update the research
dataset. The ethical issues surrounding the
identification of relevant patients and in developing
a fully informed consent mechanism remain.
Nevertheless such research has successful results
and was crucial in resolving the Autism-MMR
vaccine dispute (Taylor et al., 1999). In using non-
shared EHR data researchers face the same
constraints as clinicians, in not being able to view
the full patient pathway in a timely, cost-effective
and secure, audited manner.
In May 2012 the Department of Health in
England issued a call for efficient EHR research.
QResearch has an established ten year record in
supporting this. QResearch is a UK-based not-for-
profit general practice EHR research database. It
was developed with the aim of consolidating de-
identified, siloed EHR data from a large
representative cohort of general practices, with the
aim of providing data for ethical research purposes
(Hippisley-Cox et al., 2004). It has facilitated such
research as the development of tools for identifying
patients at risk of developing cardiovascular disease
(CVD) and diabetes (Hippisley-Cox et al., 2008);
(Hippisley-Cox et al., 2009). Such developments
using non-comprehensive, non-shared records may
have limited external validity and global relevance
both within and beyond general practice. This may
influence their usage in clinical practice as 66% of
clinicians who identify the need to perform a global
CVD risk assessment fail to follow the guidelines by
employing such a tool, valuing subjective
assessment alone (Graham et al., 2006). Cross-
provider EHR research will be required in answering
this call issued by the Department of Health in a
health sector environment with multiple care
provider types.
Table 1: Approximate count of units and patients with a
relationship recorded on SystmOne from ten care provider
types. Other provider types using SystmOne include
Speech and Occupational Therapies, Community and
Social Services, Dietetics, Palliative Care, School Nurses
and Endocrinology.
Health care provider type
Patients with data
on SystmOne
Count of units
using SystmOne
General Practice 19 million 1900
Child Health 6 million 50
District Nursing 5 million 1250
Health Visitor 2.4 million 180
Out of Hours 2.9 million 120
Physiotherapy 1.3 million 60
Acute Hospital 1.1 million 10
Podiatry 1.1 million 40
Community Primary Care
Clinic
948,000 270
Minor Injuries / Accident
and Emergency
864,000 50
There are well established alternatives to non-
ElectronicHealthRecordsResearchinaHealthSectorEnvironmentwithMultipleProviderTypes
105

integrated clinical practice and research. Kaiser
Permanente provides comprehensive care packages
to 8 million patients in America, with shared
standards between care providers. In the UK
SystmOne is a centrally hosted clinical system
provided by TPP that enables record sharing
between many of the health provider types in the
National Health Service (NHS) (Figure 1). For 15
years its centralised database has contained one
integrated EHR per patient.
From this, data is shared
with the patient and across the health units that use
SystmOne, where access rights are legitimate.
Through SystmOne 25 million patients have a
shareable record (Table 1) that facilitates integrated
care (Stoves et al., 2010). Both Kaiser Permanente
and SystmOne exemplify long-standing alternatives
that reduce the ‘silo effect’ in healthcare.
Integrated EHRs assist in cross-provider type
care management that efficiently utilises resources.
Integration at Kaiser Permanente units contributes to
the number of bed stays being 3.5 times fewer than
in the NHS for 11 leading causes (Ham et al., 2003).
Benefits from EHR sharing are indicated by patient
management improvements in cases that involve
professionals from primary and secondary care
sectors, such as are frequent in the treatment of long-
term conditions. In the case of diabetes management
this is evidenced by, for example, secondary care
consultants referring more frequently to an EHR
where the patient’s general practitioner (GP) is also
registered with SystmOne as the record would
contain updates since the previous outpatient
appointment and contains the advice of other
specialists, recent medications and blood test results
(Keen and Denby, 2009). This replaces reliance
upon physical meetings, patient awareness or being
able to telephone other care providers (Stoves et al.,
2010). Comprehensive information allows
consultants to review and communicate medication
modifications, while enabling primary care nurses to
monitor ongoing treatments and identify where
patients have non-attendance at other services (Keen
and Denby, 2009). Shared records also assist in
prompt medicine reconciliation between care
settings, identifying errors in 38% of prescriptions
(Moore et al., 2011). Clinical system integration
delivers the benefits of an “electronic highway”
envisioned by the NHS National Programme for IT
(Department of Health, 2003).
The benefits that integrated records bring to
clinical practice, in terms of the timely provision of
comprehensive information-sharing, could also be
brought to the research community. Integrated EHR
Kaiser data supports research that considers care
provision across multiple provider types. Clinical
practice has altered internationally in response to
links uncovered between hospital admissions and
drugs such as Vioxx being issued in ambulatory
(primary) care settings (Graham et al., 2005);
(Cheetham et al., 2009). Using shared EHRs in
research replaces linkage exercises that involve
identifiable data and result in biased, incomplete
datasets (Bohensky et al., 2010). Shared EHRs
enable research on the otherwise lost
communications between care providers, such as
referral trails. Research on cross-provider type
records could validate siloed research in a cost-
effective, timely manner and inform clinical practice
that occurs in integrated settings.
The aim of this paper is to determine the capacity
of a new research database, ResearchOne, to
facilitate cross-provider EHR research in the UK.
ResearchOne is a not-for-profit organisation with
ethical approval to extract de-identified EHR data
from the centralised, cross-provider SystmOne
database into ResearchOne. From here secure,
audited access to records data by the research
community has the purpose of developing research
that improves healthcare. This model must be
investigated in order to justify that ResearchOne
may bring benefits to research in the way that
SystmOne does for clinical practice.
2 METHOD
The method was designed to assess the capacity of
the ResearchOne database to support EHR research
and to justify its potential benefits to integrated
records research using English health data.
Information regarding SystmOne and ResearchOne
were determined from the ResearchOne Database
Protocol and through interviews (Crossfield et al.,
2012). QResearch is specifically designed for EHR
research in the UK and was taken as an academically
established ‘standard’. The key features of
QResearch were taken as critical success factors, as
justified in Table 2, against which the model
presented by the ResearchOne database was
appraised. These factors are the headings in the
following section. From this ResearchOne could be
validated with the potential to perform to the
existing standard for a research database of NHS
data, in order that it can facilitate cross-provider
research.
HEALTHINF2013-InternationalConferenceonHealthInformatics
106

Table 2: Features of the QResearch general practice EHR
research database, with reasoning behind their necessity.
Critical factor Reason
Data consolidation
The database assists researchers in
accessing data that has been
consolidated from many health
units and so reduces the invasion,
time and cost for clinicians and
researchers, who must otherwise
perform repeated extracts.
Large cohort of
research EHR data
Larger sample sizes bring both
power and validity to research
outcomes, enabling more research
questions to be addressed (Cohen,
1992).
De-identified EHR data
De-identification of EHR data
protects privacy and permits
research access without a public
health mandate or consent, which
could not be feasibly and non-
invasively acquired for a
significantly large cohort
(Lowrance, 2003); (Wellcome
Trust, 2009).
Representative
coverage
The external validity of a research
outcome depends upon it being
derived from a representative
sample of the population.
Ethical research
practice
Success relies upon the database
being securely developed and used
for ethical purposes.
3 RESULTS
3.1 Data Consolidation
QResearch facilitates research on EHR data
consolidated from over 650 non-integrated general
practice (GP) databases (Vinogradova et al., 2012).
The ResearchOne database can similarly hold EHR
data contributed by multiple practices. Moreover it
can hold data from other unit types, as it mirrors the
successful infrastructure of SystmOne and so it
meets this critical success factor. SystmOne
integrates data from multiple units into one
centralised record per patient and so no
consolidation is required in order to extract data in
SystmOne from multiple provider settings into the
ResearchOne database.
Data linkages to other sources undertaken by
QResearch are also feasible with ResearchOne.
QResearch links GP EHR information to socio-
economic, Hospital Episode Statistics (HES),
disease-specific registry and death registration data
(Hippisley-Cox et al., 2008); (Hippisley-Cox and
Stables, 2011). ResearchOne has national ethical and
governance approval to perform such linkages and
will likewise consolidate such information
(Crossfield et al., 2012). An NHS National Institute
for Health Research funded study, Improving
Prevention of Vascular Events in Primary Care, has
successfully piloted the capacity to link
ResearchOne data to HES and Myocardial
Ischaemia National Audit Project (MINAP) data.
3.2 Large Cohort of Research EHR
Data
General practice involvement in QResearch has
grown steadily to over 650, surpassing the original
aim of 500 practices (Hippisley-Cox et al, 2004);
(Vinogradova et al., 2012). SystmOne hosts patient
information for more than 25 million patients across
England from more than 4500 units that may
participate in ResearchOne. This includes 1900
general practices, 110 community services and 50
palliative care units (Table 1). Prison data recorded
in SystmOne cannot be extracted into the
ResearchOne database. TPP already hosts this data
in SystmOne and has the data management skills
and capacity to hold such a large cohort of records
from multiple provider types in ResearchOne.
3.3 De-identified EHR Data
Both the ResearchOne database and QResearch have
a nationally approved governance framework under
which they can hold only de-identified data. Neither
database can contain free text with potentially
identifiable data, nor full dates of birth or death.
Furthermore, given the comprehensiveness of cross-
provider type records, the ResearchOne database
excludes diagnostic cases that are present in fewer
than five records. QResearch requires consent from
each practice in order to access their databases to
perform the data extraction. While SystmOne is
centrally hosted, ResearchOne follows this practice
in requesting consent from contributing health units,
and also provides the opportunity for patients to ‘opt
out’. Consent is electronically audited through
SystmOne, the centralisation of which ensures that
any changes will automatically update ResearchOne
within seven days.
3.4 Representative Coverage
QResearch practices are “spread throughout the
UK”, offering representative general practice
coverage (Hippisley-Cox et al., 2004, p.49).
ResearchOne has the capacity to provide an
England-wide representation of cross-provider type
healthcare, through the more than 4500 invited units.
ElectronicHealthRecordsResearchinaHealthSectorEnvironmentwithMultipleProviderTypes
107

England is divided into 433 lower tiers of local
government – Local Authorities - of which over
85% have patient representation on SystmOne.
There are more than 25 million patients contributing
to 300 million years of patient records,
geographically distributed across England. Of these
patients 13 million are registered with more than one
care unit on SystmOne, and 118,000 patients are
actively receiving care from five or more units that
use SystmOne. SystmOne holds 4.8 billion
diagnostic codes, inputted by clinicians whose
specialties range from ante-natal to geriatric,
rehabilitation to neuropathology. This coverage is
across community, primary and secondary care. The
capacity for representation also covers the indices
for rurality and deprivation defined by the UK
Economic and Social Data Service (2012).
3.5 Ethical Research Practice
QResearch and ResearchOne are specifically
designed for ethical research access with the aim of
improving healthcare. The frameworks for both
QResearch and ResearchOne have been developed
with ethical and governance approval from the
relevant national bodies (Hippisley-Cox and Stables,
2011); (Crossfield et al., 2012). Any change in
policy is reviewed by the national boards and a
database committee of patients and clinical
professionals along with experts in informatics,
database architecture and governance. ResearchOne
and QResearch have an approved framework to
review data requests based on the benefit of project
proposals to clinical practice and whether they will
produce publishable results (Hippisley-Cox and
Stables, 2011); (Crossfield et al., 2012). Ethical
accessibility of both QResearch and ResearchOne is
supported by their being not-for-profit organisations.
With SystmOne data existing centrally, the cost of
ResearchOne maintenance is low, which reduces the
cost further for the research community. Remote
access to the secure ResearchOne data warehouse is
audited for the purpose of maintaining this ethical
practice.
4 DISCUSSION
The results of this investigation show that
ResearchOne matches the capacity of the existing
standard of a research database with EHR data.
ResearchOne has been nationally approved to
extract de-identified EHR data from consenting
health units. There is potential for the inclusion of
data from a large cohort of shared EHRs with
representative coverage both geographically and
demographically across England. The framework
has been designed to ethically support research that
delivers benefit to patient health.
4.1 Further Research Capacities
ResearchOne has the capacity to perform beyond
this standard. The ResearchOne database has the
potential to maintain data from multiple units across
more provider types in England than the current
standard, and so can support more comprehensive
and representative research between and within
these areas of healthcare. As this data is integrated
via SystmOne, no biased and potentially unsecure
linkage exercises are required. This is beneficial
because Bohensky et al. (2010) reviewed linkage
sensitivity to range between 74-98%. The capacity
to extract data from centralised records moves the
ResearchOne database beyond the current standard
of consolidating data from isolated units. This does
not disturb clinical practice and reduces the cost of
extraction, with this saving being passed to the
research community. The centralisation of
SystmOne maintains an up-to-date audit of unit
consent and also enables a patient to opt out of the
ResearchOne database by informing just one of their
care providers. Such further capacity is of relevance
in ethically supporting the research community to
enhance healthcare.
A further factor that assists in health research is
the timeliness of the data used, and EHRs can and
should provide timely information (Powell and
Buchan, 2005). Timely data is required for research
in order to reflect the evolving field of clinical
practice in a country with changing population and
health demographics. The centralisation of
SystmOne ensures that research data could reflect
real-time clinical developments, without affecting
SystmOne users. The ResearchOne database
framework involves updates from SystmOne at least
every seven days; this could not be compared to the
QResearch full database update frequencies that
could not be found to be listed. Items can be
extracted more frequently should this be required for
public health surveillance purposes. A further reason
for timeliness is that consent withdrawal from the
ResearchOne database results in their data being
removed within seven days. Timely data provision
can occur securely at minimum cost due to the
centralised nature of SystmOne, which is a more
speedy and accurate alternative than linking data
from multiple provider sources.
HEALTHINF2013-InternationalConferenceonHealthInformatics
108

ResearchOne has the capacity to bring the
benefits of record-sharing into the research arena.
SystmOne data that is extracted into ResearchOne is
not consolidated from multiple settings, but rather it
is integrated between them. Shared EHRs can record
data that isolated records cannot, even when linked,
portray. Through ResearchOne the integrated care
records of more than 25 million patients have the
capacity to support research, with information from
over 4500 health units in primary, secondary and
social care (Table 1). With integrated EHRs there is
less missing data that could impact on research
validity and similarly no duplication of data if, for
example, a patient moves to a new unit on the same
clinical system. This presents a more comprehensive
view of the health sector and the delivery of patient
care.
4.2 Next Steps
The capacity of ResearchOne to maintain a large
cohort of de-identified EHR data from multiple
provider types depends upon unit participation. The
joining process is simple and extracts will not
inconvenience SystmOne users given its centralised
nature. Data providers can be assured that the
ResearchOne database is maintained under the same
security principles as SystmOne in an NHS-
accredited data centre. The aim of ResearchOne, to
relay research outcomes back into clinical practice,
assures that it is beneficial to contribute to the
ethically approved process. The success of
QResearch should assist SystmOne users, some of
whom may have contributed to QResearch
previously, in recognising this beneficial invitation.
The opportunity to participate in ResearchOne has
begun to be rolled out to health units on SystmOne
and is successfully indicating the realisation of the
capacity of ResearchOne.
The aim of ResearchOne includes not only
pulling data for research purposes, but pushing
outcomes back into healthcare. Results must be
openly published, and where these have relevance to
clinical care across many provider types, they can
initiate more comprehensive healthcare benefits.
SystmOne will incorporate developments so that the
clinical system continually improves the support it
provides to over 120,000 clinicians across multiple
provider types. This cyclical, evaluative model of
clinical practice and research that is encapsulated in
SystmOne and ResearchOne can be envisioned as a
global model for the future.
ResearchOne will facilitate research both for
validation purposes and in novel areas. Explorations
will compare ResearchOne data with national
statistics to validate its representative coverage.
Research performed on other datasets will be
validated using the ResearchOne database. The
impact of integrated and isolated EHR data on
research will also be investigated, to explore the role
of ResearchOne. Research projects may use data
from single or multiple care provider types, as well
as national statistics and registry data that are
incorporated into the database. In this way
ResearchOne aims to facilitate results that are of
relevance across all units that are contributing data.
The global capacity for EHR research is
continually increasing. Progression in science,
particularly in the fields of security technology and
machine learning, will lead to data mining of entire
EHRs. The anonymisation of free text through
advancements in natural language programming, and
the reduction of human involvement in data analysis
will open up the capacities of EHRs to ethically
support research. The number and types of units
across which SystmOne provides integrated EHRs is
increasing, with a recent number of acute
deployments being made, so that ResearchOne has
increasing potential to represent comprehensive care
in England. With future developments ResearchOne
will increasingly support research that benefits
healthcare.
5 CONCLUSIONS
The contribution of EHRs to research is increasing,
but is hindered by the division of data across
healthcare units as a result of the ‘silo effect’ in
clinical care. Benefits in integrated care delivery
have been evidenced from record-sharing.
ResearchOne offers an alternative for research using
shared EHR data. The model of the ResearchOne
database has been critiqued using the success factors
of QResearch, an established provider of EHR
research data in the UK. ResearchOne meets this
existing standard and brings further developments to
the research community, especially in terms of the
timely provision of integrated, cross-provider type
data and in feeding results back into clinical care.
This offers a global model for integrated evolution
between clinicians, patients and research.
REFERENCES
Ammenworth, E., Schnell-Inderst, P., Machan, C., Siebert,
U., 2008. The effect of electronic prescribing on
ElectronicHealthRecordsResearchinaHealthSectorEnvironmentwithMultipleProviderTypes
109

medication errors and adverse drug events: a
systematic review. Journal of the American Medical
Informatics Association. 15(5): 585-600.
Bohensky, M.A., Jolley, D., Sundararajan, V., Evans, S. et
al., 2010. Data Linkage: A powerful research tool with
potential problems. BMC Health Services Research.
10(1): 346.
Cheetham, T.C., Levy, G., Niu. F., Bixler, F., 2009
Gastrointestinal Safety of Nonsteroidal Anti-
inflammatory Drugs and Selective Cyclooxygenase-2
Inhibitors in Patients on Warfarin. The Annals of
Pharmacotherapy. 43(11): 1765-1773.
Cohen, J., 1992. A power primer. Psychological Bulletin.
112(1): 155-159.
Crossfield, S.S.R., Bates, C.J., Parry, J., 2012.
ResearchOne Database Protocol. Copyright
ResearchOne 2012
Department of Health, 2003. Making IT happen:
information about the National Programme for IT.
[Accessed 27.07.2012] URL: www.dh.gov.uk
/en/Publicationsandstatistics/
Department of Health, 2012. The power of information:
putting all of us in control of the health and care
information we need. Crown Copyright: London.
Dobrey A., Haesner M., Hüsing T., Korte W.B., Meyer I.,
2008. Benchmarking ICT Use Among General
Practitioners in Europe: Final Report. Empirica.
Germany: Bonn.
Economic and Social Data Service. [Accessed on
28.08.201] URL: hwww.ccsr.ac.uk/esds/variables/
Graham, D.J., Campen, D., Hui, R., Spence, M. et al.,
2005. Risk of acute myocardial infarction and sudden
cardiac death in patients treated with cyclo-oxygenase
2 selective and non-selective non-steroidal anti-
inflammatory drugs: nested case-control study. The
Lancet. 365(9458): 475-481.
Graham, I.M., Stewart, M., Hertog, M.G.L., 2006. Factors
impeding the implementation of cardiovascular
prevention guidelines: findings from a survey
conducted by the European Society of Cardiology.
European Journal of Preventative Cardiology 13(5):
839-845.
Guttmann, A., Schull, M.J., Vermeulen, M.J. & Stukel,
T.A., 2011. Association between waiting times and
short term mortality and hospital admission after
departure from emergency department: population
based cohort study from Ontario, Canada. British
Medical Journal 342: d2983.
Ham, C., York, N., Sutch, S., Shaw, R., 2003. Hospital
bed utilisation in the NHS, Kaiser Permanente, and the
US Medicare programme: analysis of routine data.
British Medical Journal 327: 1257.
Hippisley-Cox, J., Stables, D., Pringle, M., 2004.
QRESEARCH: a new general practice database for
research. Informatics in Primary Care 12: 49-50.
Hippisley-Cox, J., Coupland, C., Vinogradova, Y.,
Robson, J. et al., 2008. Predicting cardiovascular risk
in England and Wales: prospective derivation and
validation of QRISK2. British Medical Journal 336
(7659): 1475-1482.
Hippisley-Cox, J., Coupland, C., Robson, J., Sheikh, A. et
al., 2009. Predicting risk of type 2 diabetes in England
and Wales: prospective derivation and validation of
QDScore. British Medical Journal. 338: b880.
Hippisley-Cox, J., Stables, D., 2011. QRESEARCH: An
Ethical High Quality General Practice Database for
Research. Copyright QRESEARCH 2011.
ISO/TR 20514., 2004. Health Informatics – Electronic
Health Record – Definition, Scope, and Context. ISO
Technical Report. [Accessed 21.08.2012] URL:
www.iso.org/iso/
Kawonga, M., Blaauw, D., Fonn, S., 2012. Aligning
vertical interventions to health systems: a case study of
the HIV monitoring and evaluation system in South
Africa. Health Research Policy and Systems. 10(2): 1-
13.
Keen, J., Denby, T., 2009. Partnerships in the Digital Age.
In: J. GLASBY, H. DICKINSON, ed. International
Perspectives on Health and Social Care: Partnerships
Working In Action. Sussex: Blackwell Publishing Ltd;
2009. 95-107. ISBN-10: 1444322591.
Kuperman, G.J., 2011. Health-information exchange: why
are we doing it, and what are we doing? Journal of the
American Informatics Association. 18: 678-682.
Lowrance, W., 2003. Learning from experience: privacy
and the secondary use of data in health research.
Journal of Health Services Research and Policy. 8(1):
2-7.
Moore, P., Armitage, G., Wright, J., Dobrzanski, S. et al.,
2011. Medicines Reconciliation Using a Shared
Electronic Health Care Record. Journal of Patient
Safety. 7(3): 148-154.
Powell, J., Buchan, I., 2005. Electronic Health Records
Should Support Clinical Research. Journal of Medical
Internet Research 7(1): e4 URL:
www.jmir.org/2005/1/e4/
Stoves, J., Connolly, J., Cheung, C.K., Grange, A. et al.,
2010. Electronic consultation as an alternative to
hospital referral for patients with chronic kidney
disease: a novel application for networked electronic
health records to improve the accessibility and
efficiency of healthcare. Quality and Safety in Health
Care. 19(5): e54 PMID: 20554576.
Taylor, B., Miller, E., Farrington, C.P., Petropolous, M-C.,
1999. Autism and measles, mumps, and rubella
vaccine: no epidemiological evidence for a causal
association. The Lancet. 353: 2026-2029.
Twomey, P., Whittaker A., Jervis C., 2004.
Implementation of the National Service Framework
for Diabetes: initial opportunities for a PCT to
facilitate practice and health community action plans –
year one experience. Quality in Primary Care. 12 (3):
213-218.
Vinogradova, Y., Coupland, C., Hippisley-Cox, J., 2012.
Exposure to bisphosphonates and risk of cancer: a
protocol for nested case–control studies using the
QResearch primary care database. BMJ Open. 2:
e000548.
Wellcome Trust, 2009. Towards Consensus for Best
Practice: Use of patient records from general practice
HEALTHINF2013-InternationalConferenceonHealthInformatics
110

for research. [accessed 01.08.2012] URL:
www.wellcome.ac.uk/GPrecords.
Wilson, R., Baines, S., Cornford, J., Martin, M., 2007.
‘Trying to do a jigsaw without the picture on the box’:
understanding the challenges of care integration in the
context of single assessment for older people in
England. International Journal of Integrated Care. 7:
1-11.
ElectronicHealthRecordsResearchinaHealthSectorEnvironmentwithMultipleProviderTypes
111
