
Automatic Wheeze and Respiratory Phase Detectors to Evaluate
Respiratory Physiotherapy in LRTI
A Preliminary Study
João Dinis
1,2
, Ana Oliveira
1
, Cátia Pinho
1,2
, Guilherme Campos
2
, João Rodrigues
2
and Alda Marques
1
1
School of Health Sciences, University of Aveiro (ESSUA), Campus Universitário de Santiago, Aveiro, Portugal
2
Institute of Electronics and Telematics Engineering of Aveiro (IEETA), University of Aveiro,
Campus Universitário de Santiago, Aveiro, Portugal
Keywords: Wheezing, Respiratory Phases, Respiratory Physiotherapy, Lower Respiratory Tract Infection.
Abstract: Respiratory physiotherapy is a gold standard intervention for chronic respiratory conditions. However, its
application in acute respiratory diseases (e.g., LRTI) is not well established. The objective and reliable
measurement of adventitious lung sounds (ALS), such as wheezes, has the potential to contribute to
respiratory physiotherapy evidence base. This paper reports on the implementation of reliable and published
automatic wheeze and respiratory phase detectors to assess wheezing parameters pre/post respiratory
physiotherapy treatment in patients with LRTI. Twenty patients with LRTI were randomly allocated to
control group, which received standard medication treatment, or experimental group, which received
standard medication plus respiratory physiotherapy treatment. Respiratory sounds were recorded in seven
chest locations. Wheeze parameters, namely occupation rate, main frequency, duration and type were
obtained per respiratory phase. Wheeze occupation rate was statistically significantly reduced in both
groups following treatment (p<0.001). There was a greater reduction in wheeze occupation rate in the
experimental group reaching statistical significance for the inspiratory phase (p=0.019). This promising
result indicates the potential value of respiratory physiotherapy in LRTI. It also highlights the potential to
use acoustic methods to establish respiratory physiotherapy efficacy.
1 INTRODUCTION
Lower respiratory tract infection (LRTI) covers a
wide range of diseases from a mild mucosal
colonisation or infection, an acute exacerbation of
chronic bronchitis/chronic obstructive pulmonary
disease (COPD), to an overwhelming parenchymal
infection such as community acquired pneumonia
(CAP) (Woodhead et al., 2011).
It is estimated that the annual incidence of adult
people with LRTIs consulting healthcare providers
ranges from 8-124 per 1000 population in Europe
(Ward and Ayres, 2000) and more than 5 million
cases of CAP occur annually in the United States of
America, especially in the winter months (Graham,
2008). Any age group can be affected however,
LRTI is more common in those under 5 and above
45 years old (Graham, 2008).
Respiratory physiotherapy has been recognised
as an important component in the treatment of
respiratory patients. Evidence of benefit has been
demonstrated in chronic respiratory conditions
(Garrod and Lasserson, 2007). However, there is a
need to establish efficacy in acute respiratory
diseases (e.g., LRTI).
It is widely accepted that adventitious lung
sounds (ALS), namely crackles and wheezes,
contain important information about pulmonary
dysfunctions (Laennec, 1935). Wheezes have been
the most common type of ALS investigated for
diagnostic purposes using the stethoscope (Earis and
Cheetham, 2000).
Wheezes are pitch-based sounds sustained for
longer than 100 ms with frequencies above 100 Hz.
It can be classified as monophonic (single
frequency) or polyphonic (multiple frequencies) and
occur mostly during expiration, however they can
also be heard during inspiration in more severe cases
(Sovijärvi et al., 2000). This ALS can be heard in
several diseases involving narrowing of airway
calibre (Meslier et al., 1995). Although COPD and
asthma are the main respiratory diseases presenting
233
Dinis J., Oliveira A., Pinho C., Campos G., Rodrigues J. and Marques A..
Automatic Wheeze and Respiratory Phase Detectors to Evaluate Respiratory Physiotherapy in LRTI - A Preliminary Study.
DOI: 10.5220/0004246702330238
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2013), pages 233-238
ISBN: 978-989-8565-37-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

wheezes (Waris et al., 1998), this type of ALS also
contributes to the diagnosis and monitoring of LRTI
(Woodhead et al., 2011).
According to the European Respiratory Society
(ERS) guidelines (Charbonneau et al., 2000), the
percentage of the respiratory cycle occupied by
wheezes is of special interest - the higher the
percentage the more severe the disease is (Sovijärvi
et al., 2000). Previous studies have shown an
association between the degree of bronchial
obstruction and the proportion of the respiratory
cycle occupied by wheezing (Baughman and
Loudon, 1984). However, additional measurements
such as the number of wheezing peaks, their main
frequencies, duration, timing in respiratory cycle and
location of the recording (chest wall or trachea) can
also be relevant and should be calculated if possible
(Piirilä et al., 2000). In order to address these
parameters an automatic acoustic approach is
desirable.
Several algorithms have been proposed to detect
wheeze parameters (Taplidou and Hadjileontiadis,
2007); (Qiu et al., 2005) and respiratory phases (Huq
and Moussavi, 2010); (Yildirim et al., 2008).
Taplidou and Hadjileontiadis’ (2007) algorithm has
been reported as the one with the best performance
(Oliveira et al., 2011). For respiratory phase
detection, Huq and Moussavi’s (2010) algorithm is
the most recent and overcomes limitations reported
by previous studies.
Therefore, this paper reports on the
implementation of a reliable and published
automatic wheeze and respiratory phase detectors to
assess wheezing parameters pre/post respiratory
physiotherapy treatment in patients with LRTI.
2 METHODS
A randomised controlled trial was conducted.
Ethical approval was obtained from the Ethics
Committee of Hospital Infante D. Pedro, Aveiro,
Portugal.
2.1 Procedures
Patients were eligible for the study if they presented
with cough and at least one of the following
symptoms: sputum, dyspnoea, wheezes or chest pain
(Woodhead et al., 2011), at the emergency
department of the Hospital Infante D. Pedro (Aveiro,
Portugal). Twenty participants (10 males) diagnosed
with LTRI by the physician, according to the LRTI
guidelines (Moher et al., 2010); (Woodhead et al.,
2011), were recruited for the study. A simple
randomisation (Moher et al., 2010) was use to
allocate patients to the control group or experimental
group.
The control group was treated with standard
medication, i.e. antibiotics, and the experimental
group received the same standard medication plus
respiratory physiotherapy for acute respiratory
conditions. A physiotherapy protocol was carried out
three times per week (British Thoracic Society,
2001) for 3 weeks (Woodhead et al., 2011)
accomplishing a total of 9 sessions. Each session
lasted on average 90±15 minutes (American College
of Sports Medicine, 2006). The intervention protocol
consisted of: i) breathing retraining techniques to
reduce energy costs of breathing and dyspnoea
(American College of Sports Medicine, 2006); ii)
inspiratory techniques such as incentive spirometry
to increase pulmonary expansion (Weiner et al.,
1997), prevent atelectasis and aid at sputum
clearance (Postiaux, 2004); iii) airway clearance
techniques such as the active cycle of breathing to
mobilize and clear excess bronchial secretions
(Pryor and Prasad, 2008); iv) exercises for thoracic
mobility, expansion and flexibility to increase
pulmonary volumes; v) aerobic training (walking
and cycling) at 60-80% of the patient maximal
cardiac frequency to increase tolerance to physical
activity and improve the physical fitness of the
patient (American Association of Cardiovascular
and Pulmonary Rehabilitation, 2006), vi)
educational support about the disease and lifestyles
to ensure on going effective intervention and to
provide the patient with some control over the
disease and vii) prescription of home exercises.
All treatment sessions were held in a well-
equipped room at University of Aveiro.
2.2 Data Collection
Data were collected by two researchers in a clinical
setting within 24 hours of hospital presentation and
after 3 weeks of treatment, the time taken to recover
from a LRTI (Woodhead et al., 2011).
2.2.1 Demographic, Anthropometric and
Lung Function
Demographic and anthropometric data was first
collected (height and weight to calculate the body
mass index). Lung function evaluation involved the
collection of forced expiratory volume in 1 second
(FEV
1
) and forced vital capacity (FVC) with the
spirometer MicroLab Micro Medical 36-ML3500-
HEALTHINF2013-InternationalConferenceonHealthInformatics
234
MK8, UK, following the ERS guidelines (Miller,
2005).
2.2.2 Respiratory Sounds
Respiratory sound recordings were performed
according to the Computerized Respiratory Sound
Analysis (CORSA) guidelines for short-term
acquisitions, in a clinical room, i.e., participants
were in a seated-upright position and lung sound
data was collected using seven modified analogue
stethoscopes (Classic II S.E., 3M™ Litman®, St.
Paul, MN, USA). Each stethoscope was attached to
the body using an adhesive tape (Leukosilk®, BSN
Medical GmbH, Hamburg, Germany) in seven chest
locations, i.e., trachea, left and right anterior, lateral
and posterior regions. Respiratory sounds were
collected by custom-made microphone and
preamplifier circuit (Intelligent Sensing
Anywhere®, Coimbra, Portugal) inserted into the
main tube of each stethoscope. The resulting
analogue signals were further amplified and
converted to digital by a multi-channel audio
interface (M-Audio® ProFire 2626, Irwindale, CA,
USA). The signal was converted with a 24-bit
resolution at a sampling rate of 44100 samples per
second in each channel and recorded in wave format
on a laptop computer. A diagram of the recording
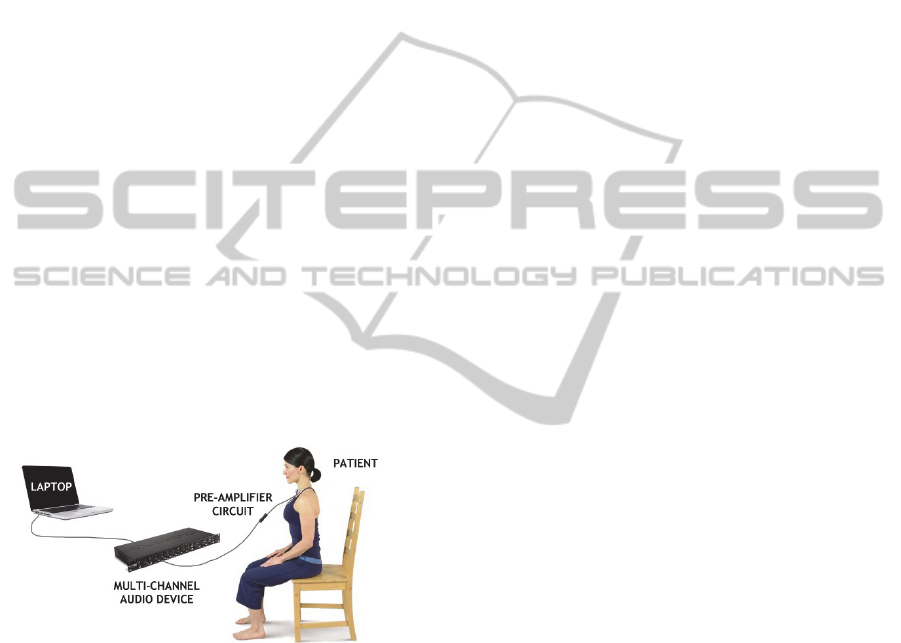
setup is shown in figure 1.
Figure 1: Diagram of the recording setup for one
stethoscope.
The average time between the first (pre-
treatment) and the second respiratory sound
recording session (post treatment) was 22.0±8.8
days for the control group and 22.8±3.1 for the
experimental group. Three repetitions per participant
(20 seconds each) were performed in each time.
2.3 Automatic Detection Algorithms
Taplidou and Hadjileontiadis (2007) automatic
wheeze detector and Huq and Moussavi (2010)
automatic respiratory phase detector were
implemented, as they have been shown to be reliable
(overall performance of 94.6% (2007) with an
accuracy of 93.1% (2010)). The combination
between these two algorithms allowed the
calculation of the wheeze occupation rate in each
respiratory phase (i.e., inspiration, expiration) of the
recorded signals.
The following sections present a brief description
of these algorithms.
2.3.1 Wheeze Detection Algorithm
Wheezes were detected using the algorithm
described by Taplidou and Hadjileontiadis (2007).
This algorithm is based on the Short-time Fourier
transform (STFT), proposed by Gabor (Gabor,
1946), which is a classical method for analysing
non-stationary signals. This technique is a Fourier-
related transform used to determine the sinusoidal
frequency and phase content of local sections of a
signal as it changes over time. The Fourier transform
of the resulting signal is taken as the window is slid
along the time axis, resulting in a two-dimensional
representation of the signal, where x
t
is the signal
and ω denotes the spectral window.
STFT
x
t
≡X
τ,ω
x
t
.ω
tτ
e
dt
In the implemented algorithm, the signal is digitally
filtered (band pass 60-2100Hz, order-8 Butterworth)
and resampled (to 5512s
-1
) before the STFT
calculation. To remove noise from the STFT signal,
a smoothing procedure based on box filtering, also
known as mean-filtering, estimates the trend of the
frequency content of the windowed signal at each
time instant. Peaks higher than a specific magnitude
threshold are then selected. These peaks are then
classified as wheezes or non-wheezes according to a
set of criteria that include local maxima, peak
coexistence and continuity in time.
The algorithm allowed the calculation of
different parameters, e.g., starting and ending time
as well as fundamental frequency of each detected
wheeze. It was also possible to classify the wheeze
according to its type (monophonic or polyphonic).
2.3.2 Respiratory Phase Detection
Algorithm
For the respiratory phase detection, an algorithm
using only tracheal sounds was implemented (Huq
and Moussavi, 2010). Because of the synchronized
multi-channel acquisition, the detected phases and
onsets on the tracheal sounds were used to calculate
the wheeze occupation rate in the other six places,
where the acoustic signal was acquired.
AutomaticWheezeandRespiratoryPhaseDetectorstoEvaluateRespiratoryPhysiotherapyinLRTI-APreliminaryStudy
235
Similarly to the wheeze detector algorithm, the
signal was firstly digitally filtered (band pass 150-
800Hz, order-10 Butterworth filter) and resampled
(to 10240 s
-1
). The selected filtering band was used
to minimise the effect of heart sounds and high
frequency noises. In this algorithm, several
parameters were collected from the duration, volume
and shape of the tracheal breath sound envelope in
each phase. For this purpose the logarithmic
variance (LV) of the filtered sound signals was
calculated. As the LV of the breath sounds resemble
a fully rectified flow signal, respiratory onsets (i.e.,
starting sample of a respiratory phase) can also be
detected. Using the majority-vote of parameters
between adjacent phases, they can be classified as
inspiration or expiration.
2.4 Statistical Analyses
Statistical analysis was conducted using SPSS®
19.0. Differences between parameters in the first
(pre-treatment) and the second respiratory sound
recording (post treatment) were explored with paired
samples T-test. Wheeze occupation rate (R), main
frequency (F) and type of wheeze (T) evaluated on
both inspiratory and expiratory phase recordings
were analysed. R value was established in the range
zero to one (where 0 was given when no wheezes
were detected and 1 when the respiratory phase was
fully occupied). The T was classified as 0 if
monophonic or as 1 if polyphonic.
Statistically significant differences between
groups (control vs. experimental group) at each
parameter assessed on pre and post treatment was
explored to evaluate the impact of the respiratory
physiotherapy. For this purpose also an independent
samples T-test analysis was performed.
Data were expressed as mean and standard
deviation (Mean±SD). Significance level was set at
p<0.05.
3 RESULTS
A total of twenty participants (10 males) diagnosed
with LTRI enrolled in this pilot study. Eleven
patients (4 males) composed the control group while
the experimental group was composed by 9 patients
(6 males). The sample is characterised in Table 1.
Paired sample t-test results for pre-post treatment
analysis on control and experimental groups are
present in Table 2. A statistically significant
decrease was observed in both inspiration and
expiration wheeze occupation rate in both groups.
Table 1: Sample characterisation.
Age (yrs) BMI (kg/m
2
) FVC
PP
(%) FEV
1-PP
(%)
CG 52.9 ± 18.3 26.1 ± 5.2 75.7 ± 21.6 72.2 ± 29.8
EG 49.9 ± 23.2 23.4 ± 4.6 62.6 ± 25.9 62.2 ± 29.0
T 56.0 ± 13.7 24.9 ± 4.9 69.8 ± 23.9 67.7 ± 28.2
CG – Control group; EG – Experimental group; T- Total; BMI –
Body mass index; FVC
PP
– percentage predicted of forced vital
capacity; FEV
1PP
– percentage predicted of force expiratory
volume in 1 second.
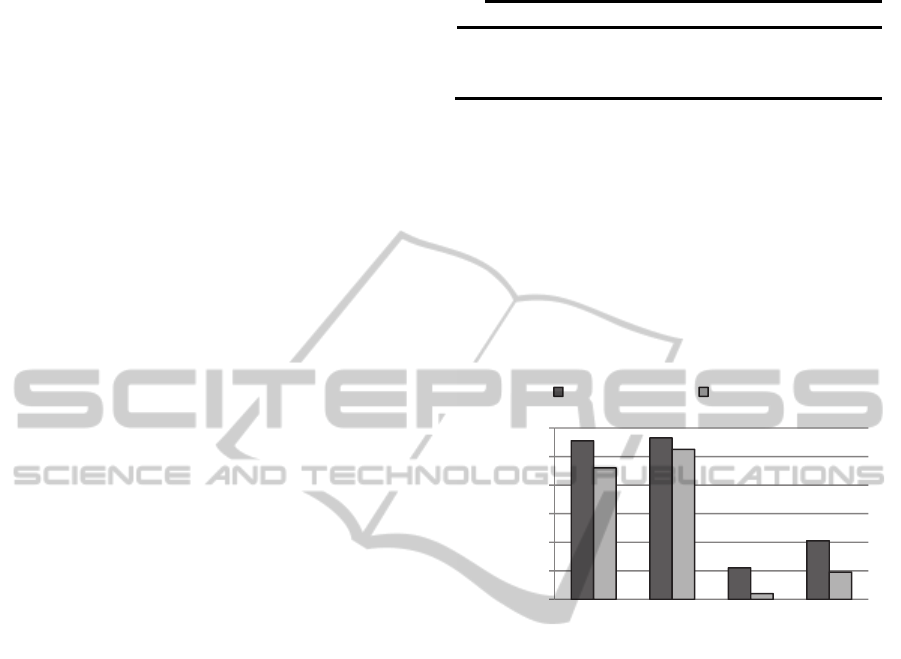
The difference in wheeze occupation rate
between both studied groups is presented in Table 3.
A superior reduction in occupation rate in both
inspiratory and expiratory respiratory phases (figure
2), after physiotherapy treatment was observed,
reaching statistical significance for the inspiratory
phase (p=0.019).
Figure 2: Wheezes occupation rate differences between
control and physiotherapy groups. Significance level set to
*p<0.05.
4 DISCUSSION
The combination between different algorithms
contributes to establish objective measures to assess
the effect of respiratory physiotherapy in patients
with acute respiratory diseases (e.g., LRTI).
The values collected at baseline for FEV1
pp
(67.7
± 28.2) and FVC
pp
(69.8 ± 23.9) were lower than
those previously reported for patients with LRTI.
Melbye et al. (1994) found that FEV1
pp
in patients
with upper or lower respiratory tract infection was
90% of the predicted value, however various factors
could affect this value, such as cough, dyspnoea and
smoking habits. Such factors were highly prevalent
in the present sample. Furthermore, in the study of
Melbye et al. (1994) the spirometry test was
performed in the standing position while in the
present study patients presented with severe
symptoms of pain, cough and dyspnoea and were
instructed to perform the test in the sitting position,
0,00
0,02
0,04
0,06
0,08
0,10
0,12
Wheeze Occuptaion Rate
Control Group Experimental Group
R
I - Pre
p = 0.061
p = 0.019
*
R
E-Pre
R
I - Post
R
E-Post
HEALTHINF2013-InternationalConferenceonHealthInformatics
236

Table 2: Paired sample t-test results for pre-post treatment analysis on control and experimental groups.
Control Group Experimental Group
Pre Post p t Pre Post p t
R
I
(%)
0.111 ± 0.148 0.022 ± 0.062
< 0.001 5.462 0.092 ± 0.141 0.004 ± 0.019 < 0.001 4.777
R
E
(%)
0.113 ± 0.132 0.041 ± 0.077
< 0.001 4.392 0.105 ± 0.153 0.019 ± 0.054 < 0.001 4.402
F
I
(Hz)
241.3 ± 60.1 415.5 ± 201.1 0.195 -1.554 360.3 ± 221.1 1402 ± 1531 0.555 -0.841
F
E
(Hz)
221.2 ± 85.6 396.8 ± 208.1 0.243 -1.368 423.2 ± 168.6 432.8 ± 269.1 0.915 -0.111
T
I
(%)
0.050 ± 0.111 0.032 ± 0.074 0.374 1.000 0.083 ± 0.117 0.000 ± 0.000 0.500 1.000
T
E
(%)
0.107 ± 0.220 0.106 ± 0.301 0.999 0.001 0.238 ± 0.224 0.142 ± 0.377 0.652 0.475
R - wheeze occupation rate; F - main frequency; T - type of wheeze. Subscript I and E stand for inspiration and expiration, respectively.
Significance level set to p<0.05.
which could also have affected the test performance.
Table 3: Paired sample t-test results for the two groups.
CG EG p t
R
I - Pre
0.111 ± 0.148 0.092 ± 0.141 0.455 0.618
R
E - Pre
0.113 ± 0.132 0.105 ± 0.153 0.749 0.282
R
I - Post
0.022 ± 0.062 0.004 ± 0.019
0.019 2.762
R
E - Post
0.041 ± 0.077 0.019 ± 0.054 0.061 1.907
CG - Control group; EG - experimental group; R - wheeze
occupation rate; Subscript I and E stand for inspiration and
expiration, respectively. Significance level set to p<0.05.
There were no significant differences in
inspiratory and expiratory wheezes occupation rates
pre-treatment. This shows that both studied groups
were similar in terms of wheezes parameters at
baseline assessment.
The results of pre/post treatment analysis (table
2) showed significant statistical decrease in both
inspiratory and expiratory wheeze occupation rate
for control and experimental groups. This was an
expected outcome, because both groups received, at
least, standard medication treatment i.e., antibiotics.
The experimental group, which received respiratory
physiotherapy, presented a significantly lower
inspiratory wheeze occupation rate (p=0.019) and a
pattern of decreased expiratory wheeze occupation
rate (p=0.061). As previously stated by Sovijärvi et
al., (2000), more severe cases of respiratory
infection can also present wheezes in the inspiratory
phase. The sharp decrease on inspiratory wheeze
occupation rate seems to suggest that the respiratory
physiotherapy plays an important role on patients
with more severe conditions. Another result that
supports this theory is the non-existence of
inspiratory polyphonic wheezes post-treatment in the
experimental group, and, although not statistically
significant, a sharp decrease in the expiratory
polyphonic wheezes.
5 CONCLUSIONS
This study suggests that by combining respiratory
physiotherapy with the standard medical therapy
more effective results in the reduction of respiratory
wheeze can be achieved in patients with LRTI.
Furthermore, the use of wheeze and respiratory
phase detectors appears to be a responsive measure
to evaluate the efficacy of treatments in LRTI.
Further research to assess responsiveness with a
larger sample is nevertheless needed.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the funding
provided to this project, “Sounds4Health”, by
Quadro de Referência Estratégico Nacional
(QREN), on a partnership between University of
Aveiro and ISA (Intelligence Sensing Anywhere).
The authors would also like to thank to
physicians at Hospital Infante D. Pedro for their help
during the recruiting phase of the study and to all
participants.
REFERENCES
American Association of Cardiovascular and Pulmonary
Rehabilitation, 2006. Guidelines for pulmonary
rehabilitation programs, USA, Human Kinetics.
American College of Sports Medicine, 2006. Guidelines
for Exercise Testing and Prescription, Philadelphia,
Lippincott Williams and Wilkins.
Baughman, R. P. & Loudon, R. G., 1984. Quantitation of
wheezing in acute asthma. Chest, 86, 718-22.
British Thoracic Society, 2001. Pulmonary rehabilitation.
Thorax, 56, 827-34.
Charbonneau, G., Ademovic, E., Cheetham, B.,
Malmberg, L., Vanderschoot, J. & Sovijärvi, A., 2000.
AutomaticWheezeandRespiratoryPhaseDetectorstoEvaluateRespiratoryPhysiotherapyinLRTI-APreliminaryStudy
237

Basic techniques for respiratory sound analysis. Eur
Respir Rev., 10, 625-635.
Earis, J. & Cheetham, B., 2000. Future perspectives for
respiratory sound research. Eur Respir Rev, 10, 641-
646.
Gabor, D. 1946. Theory of communication. Journal of the
IEEE, 93, 429-457.
Garrod, R. & Lasserson, T., 2007. Role of physiotherapy
in the management of chronic lung diseases: an
overview of systematic reviews. Respiratory
Medicine, 101, 2429-2436.
Graham, D., 2008. The patient with possible pneumonia.
The Foundation Years, 4, 14-19.
Huq, S. & Moussavi, Z., 2010. Automatic Breath Phase
Detection Using Only Tracheal Sounds. 2010 Annual
International Conference of the Ieee Engineering in
Medicine and Biology Society (Embc), 272-275.
Laennec, R., 1935. A treatise on the diseases of the chest
and mediate auscultation, New York, Samuel Wood
and Sons.
Melbye, H., Kongerud, J. & Vorland, L., 1994. Reversible
airflow limitation in adults with respiratory infection.
Eur Respir J, 7, 1239-45.
Meslier, N., Charbonneau, G. & Racineux, J. L., 1995.
Wheezes. European respiratory journal, 8, 1942-8.
Miller, M. R. 2005. Standardisation of spirometry.
European Respiratory Journal, 26, 319-338.
Moher, D., Hopewell, S., Schulz, K. F., Montori, V.,
Gotzsche, P. C., Devereaux, P. J., Elbourne, D., Egger,
M. & Altman, D. G., 2010. CONSORT 2010
explanation and elaboration: updated guidelines for
reporting parallel group randomised trials. BMJ, 340,
c869.
Oliveira, D., Pinho, C., Marques, A. & Dinis, J., 2011.
Validation of a time-frequency wheeze detector in
cystic fibrosis: A pilot study. Eur Respirator J, 38,
92s.
Piirilä, P., Sovijärvi, A., Earis, J., Rossi, M., Dalmasso, F.,
Stoneman, S. & Vanderschoot, J., 2000. Reporting
results of respiratory sound analysis. European
Respiratory Review, 10, 636-640.
Postiaux, G., 2004. Fisioterapia respiratória pediátrica, o
tratamento guiado por ausculta pulmonar.
Pryor, J. & Prasad, S., 2008. Physiotherapy for
Respiratory and Cardiac Problems: Adults and
Paediatrics, UK, Churchill Livingstone.
Qiu, Y., Whittaker, A. R., Lucas, M. & Anderson, K.,
2005. Automatic wheeze detection based on auditory
modelling. Proceedings of the Institution of
Mechanical Engineers Part H-Journal of Engineering
in Medicine, 219, 219-227.
Sovijärvi, A., Malmberg, L., Charbonneau, G.,
Vanderschoot, J., Dalmasso, F., Sacco, C., Rossi, M.
& Earis, J. E., 2000. Characteristics of breath sounds
and adventitious respiratory sounds. Eur Respir Rev,
10, 591–596.
Taplidou, S. A. & Hadjileontiadis, L. J., 2007. Wheeze
detection based on time-frequency analysis of breath
sounds. Computers in Biology and Medicine, 37,
1073-1083.
Ward, D. & Ayres, J., 2000. Pneumonia and acute
bronchitis. The European respiratory journal
Supplement, 5, 105-127.
Waris, M., Helisto, P., Haltsonen, S., Saarinen, A. &
Sovijarvi, A. R., 1998. A new method for automatic
wheeze detection. Technol Health Care, 6, 33-40.
Weiner, P., Man, A., Weiner, M., Rabner, M., Waizman,
J., Magadle, R., Zamir, D. & Greiff, Y., 1997. The
effect of incentive spirometry and inspiratory muscle
training on pulmonary function after lung resection. J
Thorac Cardiovasc Surg, 113, 552-7.
Woodhead, M., Blasi, F., Ewig, S., Garau, J., Huchon, G.,
Ieven, M., Ortqvist, A., Schaberg, T., Torres, A., van
der Heijden, G., Read, R., Verheij, T. J. M., Soc, E. R.
& Microbiology, E. S. C., 2011. Guidelines for the
management of adult lower respiratory tract infections
- Summary. Clinical Microbiology and Infection, 17,
1-24.
Yildirim, I., Ansari, R. & Moussavi, Z., 2008. Automated
Respiratory Phase and Onset Detection Using Only
Chest Sound Signal. 2008 30th Annual International
Conference of the IEEE Engineering in Medicine and
Biology Society, Vols 1-8, 2578-2581.
HEALTHINF2013-InternationalConferenceonHealthInformatics
238
