
The PartoPen in Training and Clinical Use
Two Preliminary Studies in Kenya
Heather Underwood, S. Revi Sterling and John K. Bennett
University of Colorado Boulder, Boulder, U.S.A.
Keywords: Partograph, Digital Pen, ICTD, Health Informatics, Maternal Health.
Abstract: This paper presents the findings from two studies of the PartoPen system – a digital pen software
application that enhances the partograph, a paper-based labor-monitoring tool used extensively in
developing regions. The PartoPen provides nurses with real-time decision support, instructions, and patient-
specific reminders by playing short audio clips when a nurse records data on the existing paper partograph
form. Previous studies have shown that correct use of the partograph significantly reduces pregnancy
complications; however, the partograph is not always reliably or correctly completed due to resource and
training challenges commonly found in developing world clinics. The PartoPen system addresses several
significant barriers to correct partograph use in developing countries. The preliminary studies described in
this paper examine how the PartoPen system affects classroom-based partograph training among nursing
students at the University of Nairobi, and partograph completion and accuracy in actual labor and delivery
situations by nurse-midwives at Kenyatta National Hospital in Nairobi, Kenya. The initial results of these
studies indicate that using the PartoPen system enhances student performance on partograph worksheets,
and that use of the PartoPen system in labor wards positively affects partograph completion rates and
nurses’ level of expertise using the partograph form.
1 INTRODUCTION
In 2010 the World Health Organization (WHO)
estimated that 287,000 women die every year due to
pregnancy related complications (WHO, 2010). The
vast majority (99%) of annual maternal deaths occur
in developing countries. Many of these deaths can be
prevented with skilled care before, during, and after
childbirth (WHO, 2010). In addition, the rate of
maternal morbidities, which include fistula, uterine
rupture and prolapse, and mental health concerns, is
estimated to be between 15 and 20 million cases per
year. Treatment for these complications, when
available, costs an estimated $6.8 billion per year
(Stanton, 2010).
The WHO advocates the paper partograph as the
single most effective tool for monitoring labor and
reducing labor complications in developing
countries. The partograph facilitates the tracking of
maternal condition, fetal condition, and cervical
dilation versus time during labor (Friedman, 1954).
Used correctly, the partograph can serve as a tool for
early detection of serious maternal and fetal
complications during labor. Early detection of
pregnancy complications, especially in rural clinics,
allows transport decisions to be made in time for a
woman to reach a regional facility capable of
performing emergency obstetric procedures.
However, in order to be effective, the partograph
must be used correctly. A recent study in Kenya
reported that while 88.2% of the 1057 evaluated
patient records contained a partograph, only 23.8%
of the forms had been used correctly (Mugerwa et al.
2012). This is not unusual for developing countries
where lack of training and continuing education,
exacerbated by limited resources, represent serious
barriers to effective partograph use (Lawn & Kerber,
2006; Levin, 2011; Lavender et al. 2011).
The goal of the PartoPen project is to increase
the effectiveness of the partograph using an
interactive digital pen with custom software,
together with partograph forms printed with a
background dot pattern that is recognized by the pen
(Underwood 2011, Underwood et al. 2012). The
digital pen uses internal handwriting recognition and
paper-based location awareness to interpret the
measurements made on the partograph form. These
interpreted measurements can then trigger alerts for
112
Underwood H., Sterling S. and K. Bennett J..
The PartoPen in Training and Clinical Use - Two Preliminary Studies in Kenya.
DOI: 10.5220/0004251101120121
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2013), pages 112-121
ISBN: 978-989-8565-37-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

attending health care providers when conditions
arise that require additional observation or
intervention. In addition, timers on the digital pen
can be triggered when measurements are plotted in
order to provide audio reminders to take routine
patient measurements at specified time intervals.
The PartoPen thus provides a low-cost, and intuitive
solution that addresses several of the identified
barriers to successful partograph use, including form
complexity and data interpretation challenges.
This paper describes two preliminary studies that
examined the PartoPen in use in Nairobi, Kenya
from June 2012 – August 2012; the first was
conducted with ninety-five third and fourth-year
nursing students at the University of Nairobi School
of Nursing Sciences, and the second, with nurse
midwives in the labor wards of Kenyatta National
Hospital (KNH) and Pumwani Maternity Hospital
(PMH) over a period of one month. The principal
findings of these two studies, reported in more detail
below, are (1) the PartoPen improved the ability of
nursing students to accurately complete partograph
worksheets using synthetic maternal data, (2) use of
the PartoPen during actual labor increases both the
rate of partograph completion, and partograph
accuracy, and (3) that the PartoPen was readily
accepted and adopted by both students and
practitioners.
2 RELATED WORK
There is a large body of research that examines the
potential relationships between paper-based systems
and digital tools, particularly mobile phones. Mobile
phone tools have been designed to simplify data
collection (Hartung et al. 2010), improve community
health worker performance and effectiveness
(Grameen Foundation, 2010; Parikh, 2005;
Sherwani, 2007; Svoronos, 2010; Derenzi, 2008),
and digitize data from paper forms (Dell et al, 2012;
Ratan et al., 2010).
Digital pens offer the unique affordances of
retaining the physical motion of natural writing, and
simultaneous creation of a paper and digital record.
Digital pens have been customized for context-
specific research tools (Yeh et al., 2006; Cowan et
al., 2011; Song et al., 2011; Landau et al., 2008) due
to their programmability, portability, audio and note
synchronization, and their ability to digitize sketches
as well as handwritten notes for easy transmission
via email. A specific example of how digital pens
have been used in a healthcare setting is the
TraumaPen (Sarcevic, 2010). The TraumaPen
integrates paper emergency patient intake forms
with a digital display component in the exam room
to reduce redundancy of verbal data transmission
between health care practitioners.
Prior research on improving the paper
partograph form includes the ePartogram device
developed by Jhpiego (Jhpiego, 2011), and the
partograph e-Learning tool created by the WHO
(Mathai, 2010). Jhpiego is currently testing three
ePartogram implementations, which include an
Android tablet application, a digital clipboard
system, and a custom hardware solution, but at this
time, no data has been collected or analysed for any
of these models. The WHO e-Learning tool is
distributed to facilities like KNH via CD-ROM.
However, the CD-ROMs are not given to every
student or directly incorporated into the nursing
curriculum. Single copies of the tool are often
passed from student to student throughout the
academic year, placing the primary responsibility for
learning the material upon the students themselves.
Less than half of the students who participated in the
PartoPen study had used the eLearning tool.
To the best of our knowledge, the PartoPen
system is the only standalone digital partograph
solution that can be used interchangeably as a
training tool and in active labor theaters without
altering the currently paper-based system or
requiring significant additional training for the
technology itself.
3 THE PartoPen SYSTEM
The current implementation of the PartoPen system
uses the Livescribe 2GB Echo digital pens, which
can capture and synchronize audio and handwritten
text, and digitize handwritten notes into searchable
and printable PDF documents. These pens use an
infrared camera in the tip of the pen that is triggered
when a user presses the pen tip to a piece of paper.
The camera captures a pre-printed unique dot pattern
(see Figure 1) at a rate of 70 images per second.
Each printed dot contains location information,
which the pen interprets and uses to perform
location-specific functions, such as play an audio
instruction prompt when an instruction button is
tapped or trigger a decision-support prompt when a
birth attendant plots a measurement indicating
abnormal labor. The digital pens also include a
speaker, a microphone, a 3.5mm audio headphone
jack, up to 8GB of memory storage (approximately
800 hours of audio recording storage), an OLED
display, a rechargeable lithium-ion battery, and a
micro-USB connector for charging and data transfer
(Figure 2). Ink cartridges can be easily ordered and
replaced.
ThePartoPeninTrainingandClinicalUse-TwoPreliminaryStudiesinKenya
113
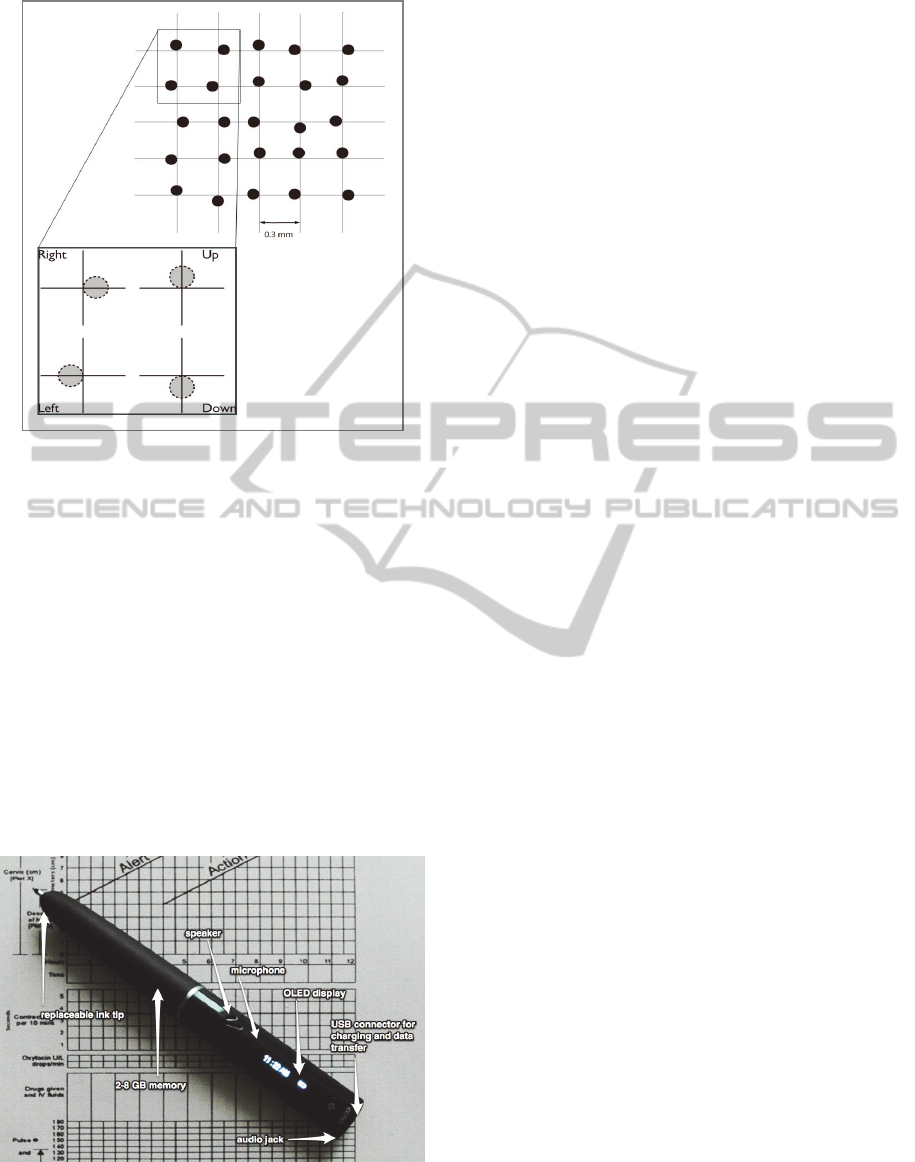
Figure 1: The Dot Positioning System (DPS) uses printed
microdots, as seen above, arranged in specific patterns.
The dot pattern allows the digital pen to determine where
on the form it is placed, thus allowing the pen to interact
in meaningful ways with specific form regions. The dot
pattern is patented by Anoto AB Group.
The PartoPen provides partograph training
instructions, task-oriented reminders, and context-
specific audio feedback in real time. Tapping the pen
in different areas on the partograph form provides
audio instructions taken directly from the WHO
partograph manual, which reinforces birth attendant
training. The pen detects abnormal labor progression
by analyzing data entered on the partograph form,
and provides audio and text-based feedback to
encourage birth-attendants to take appropriate
action.
Figure 2: The digital pen used in the PartoPen system is
depicted. The speaker, microphone, OLED display, USB
connector, audio jack, memory storage, and replaceable
ink tip are identified.
The PartoPen is appropriate for use in resource-
challenged environments. It does not require
network connectivity to operate, and uses a
rechargeable lithium ion battery that can be charged
using a standard cell phone charger. The dot pattern,
printed on the partograph forms using a standard
laser printer and printer paper, allows the pen to
synchronize written text with recorded audio. Most
importantly, the PartoPen is low cost, durable,
consumes very little power, requires minimal
training, and enhances – rather than replaces – the
common paper tool in near-ubiquitous use in the
developing world.
4 NURSING STUDENT STUDY
The nursing student study took place at the
University of Nairobi (UoN) School of Nursing
Sciences in Nairobi, Kenya. The university is closely
affiliated with KNH, and the nursing students at
UoN perform clinical rotations in the maternity
wards at KNH. The goals of the nursing student
study were to establish a baseline of common
partograph errors based on the type of error (e.g.,
incorrect values, incorrect form location, or incorrect
action based on entered data), determine if using the
PartoPen decreases the number of common
partograph errors in relation to the established
baseline, and approximate the amount of training
needed to use the PartoPen and access the majority
of the built-in functionality.
4.1 Methodology
4.1.1 Participants
Ninety-five nursing students in their third and fourth
years of study participated in the study. Local
research assistants recruited participants from the
population of 148 third and fourth year nursing
students at the UoN. All students had previously
been taught how to use the partograph to monitor
labor during a 10-15 minutes in-class discussion as
part of the nursing curriculum, and during their
clinical rotations in the maternity wards.
The 95 student participants were separated by
year (i.e., third or fourth year nursing students) and
then randomly divided into three groups, resulting in
six total groups. Group 1 was the control group, and
Groups 2 and 3 were the intervention groups, which
focused on the discoverability of the functionality,
and the affect on partograph performance,
respectively. Group 1 students completed a
partograph worksheet task with a PartoPen in “silent
HEALTHINF2013-InternationalConferenceonHealthInformatics
114

logging mode,” and received no instructions on how
to use the technology. In the “silent logging mode”
the digital pen records student answers, and logs
when and where on the form student answers would
have triggered feedback from a fully functional
PartoPen. This control group provided a baseline for
students’ performance on the partograph worksheet
task.
Group 2 completed the same worksheet task, but
used a fully functional PartoPen in “use” mode. The
PartoPen software in “use” mode for the student
pilot has two main components: instructions and
decision support. For the nursing student study with
nursing students completing a partograph worksheet,
the reminders (enabled only for the maternity ward
study) were disabled. In addition, playing pre-
recorded spoken audio provided the decision
support, in contrast to the maternity ward decision
support, which was provided by scrolling text across
the OLED display.
Group 2 received no training on how to use the
technology. In “use” mode, the digital pen logs
when errors are made on the form, which will be
compared to the baseline results recorded from the
first class of students. Students in this group will
receive audio feedback from the pen when data is
entered incorrectly on the form, and thus, corrected
errors will also be recorded in this mode. The data
collected from this group tested the discoverability
and intuitiveness of the PartoPen functionality.
Group 3 received a fully functional PartoPen in
“use” mode and a 15-minute introduction and
demonstration of the PartoPen system before
completing the partograph worksheet task. The
digital pen will be recording errors, corrections, and
all marks made on the partograph form. By
comparing the results of Group 3 with the results of
Group 2, researchers will determine the affect of
providing a PartoPen tutorial on partograph
performance. Groups 2 and 3 attempt to simulate
PartoPen deployments in which students/nurses do
and do not receive training prior to using the device.
Given that most of the PartoPen functionality is
“pushed” to users just by normally completing a
partograph form, researchers hypothesize that
training on the PartoPen system should not
significantly alter the results of participants with the
same level of prior partograph knowledge – Groups
2 and 3 respectively.
4.1.2 Partograph Worksheet Grading
For all student groups, the partograph worksheets
consisted of two patient case studies and two blank
partograph forms printed with the dot pattern. The
students were asked to record the patient data on the
blank partograph forms as if they were actively
monitoring that patient during labor.
The principal investigator created a grading
scheme based on the partograph grading schemes
currently used to evaluate nursing students during
clinical rotations. Each measurement category on the
partograph (e.g., fetal heart rate, contractions, pulse,
etc.) was graded in five sub-categories out of a set
number of points specific to the particular case
study. The five sub-categories included
“measurement present”, “mark accurate”, “correct
symbol”, “plotted on correct time line”, and “correct
spacing”. In the grading example shown in Figure 3,
the partograph form sections are listed vertically in
the far-left column, and the sub-categories and
possible point totals run horizontally along the top of
the spreadsheet. The cells that have been grayed-out
represent categories that are not applicable to the
specific case study.
Figure 3: An example of the grading spreadsheet used for grading the worksheets in the teaching and training study.
Partograph form sections are listed vertically in the left hand column, grading sub-categories are listed horizontally across
the top of the spreadsheet, and points possible for each category are listed in red. Grayed out cells indicate that these
categories were not applicable to the case study being graded.
ThePartoPeninTrainingandClinicalUse-TwoPreliminaryStudiesinKenya
115

Three research assistants graded all 95
worksheets according to the grading scheme
described above, and each student was given an
overall worksheet grade based on the total number
of points possible for the two case studies they
received.
4.1.3 Focus Groups
After completing the worksheet task, 5-10 students
from each group were randomly selected to
participate in a focus group discussion. The goals of
the focus group discussion were to gain an
understanding of current partograph training
programs used at the study site, determine students’
perceptions about the partograph form as a labor
monitoring tool, and to record students’ perceptions
of the PartoPen system as an in-class training and
active labor monitoring tool. The focus group
discussions took between 15 and 30 minutes, and
student responses were audio recorded using a
digital pen and later transcribed.
4.2 Preliminary Results
4.2.1 Quantitative Results
Using the grading scheme outlined in section 4.1.2,
scores were calculated as a percentage of total points
correct out of the total possible points. Researchers
performed an unpaired t-test to determine any
significant difference between groups, particularly if
Groups 2 and 3 showed any improvement in
performance over Group 1 – the control group. Due
to time constraints and limited grading resources,
only the data from fourth year students is presented
here. Group 1 from year four, which used the
PartoPen in silent logging mode to complete the
worksheet had an average score of 58%, which
means that on average students in this group
correctly plotted 58% of the measurements from
both case studies in the worksheet with the highest
possible score being 100%. The average score for
Group 2, which used the PartoPen in “use” mode but
received no instructions, was 63%. And the average
score for Group 3, which used the PartoPen in “use”
mode and received instructions, was 66%. The
difference in the average scores for the worksheet
task suggest that use of and training on the PartoPen
facilitated more accurate data recording on the
partograph forms.
Table 1: Average scores on worksheet completion task for
fourth year students divided by PartoPen functionality
group number. This table illustrates an increase in student
performance with increasing PartoPen functionality and
training.
Group # and PartoPen Mode Avg. Score
Group 1 – silent logging mode 58%
Group 2 – use mode, no training 63%
Group 3 – use mode, training 66%
In each worksheet, students received two patient
case studies. All students received the “Mrs. B” case
study, and either “Mrs. C” or “Mrs. A.” The three
case studies represent three possible labor outcomes.
Mrs. A’s data represents an uncomplicated, timely
labor that progresses without medical intervention.
Mrs. B’s data illustrates a case of prolonged or
obstructed labor, which is addressed by the
administration of oxytocin – a labor-inducing drug.
Finally, Mrs. C’s labor progression data illustrates
an increasing number of complications, including
fetal distress, and ultimately results in a cesarean
section. Thirty-four instructional audio prompts are
available for all students and all patient case studies.
However, only the Group 3 students were informed
how to access the instruction prompts by tapping the
pen on the text to the left of the graphs on the form.
The average scores for each group based on patient
case study are shown in Table 2. Using an unpaired
t-test, the difference between Group 1 and Group 3
for the patient case study Mrs. C, was found to be
significant (p-value = .0267). These data could
suggest that for more challenging or complex labor
cases, the availability and utilization of the
instruction prompts promotes more accurate form
completion.
Table 2: Average scores on worksheet completion task for
fourth year students divided by patient case study and
group number. This table illustrates a significant
difference (p-value = .0267, between Group 1 and Group 3
for the most complex patient case study: Mrs. C.
Mrs. A Mrs. B Mrs. C
Group 1 61.3% 58.6% 52.0%
Group 2 63.5% 62.9% 62.9%
Group 3 65.2% 62.7% 72.2%
4.2.2 Qualitative Results
Qualitative data from the focus groups examined
three factors: students’ previous partograph training,
students’ perceptions about the usefulness and
effectiveness of the partograph as a labor monitoring
tool, and students’ feedback on PartoPen usability.
Students explained that the in-class introduction
of the partograph ranged from a 5-15 minute
HEALTHINF2013-InternationalConferenceonHealthInformatics
116

explanation by the lecturer. Lecturers reportedly
demonstrated the partograph, but did not
consistently fill one out completely in class.
Students themselves did not practice filling out the
partograph form. Students gained the majority of
their experience using the partograph during their
clinical rotations in the maternity wards. Individual
experiences using the partograph in maternity wards
fluctuated due to the number of nurses in the ward
available to facilitate partograph training and the
number of patients per day in the ward requiring a
partograph (i.e., in active labor).
Students expressed that recording the
contractions is the most difficult part of the normal
partograph form because of having to remember the
different shading styles that indicate contraction
duration. Students also experience challenges when
plotting the descent of the fetal head, moulding, and
liquor (i.e., amniotic fluid). All of the students who
participated in the focus groups from Groups 2 and 3
expressed that the PartoPen significantly mitigated
these challenges and made the difficult form sections
easier to fill out. One student commented: “In a
classroom setup, it would be good because it will
really help when we are first learning [the
partograph]. It solidifies the basic things we need to
know.” Another student said: “At first, when you
asked us what action to take when a measurement
was made across the alert line, we were silent. But
now, after we used it, we all know right away what
to do.”
Students suggested several feature changes to
improve the PartoPen for student use. The
suggestions include modifying the form itself to
make the boxes larger and thus easier for entering
data into (the PartoPen system used the standard
WHO partograph form), and developing a flexible
instruction-creation platform so that instructions can
be easily modified to keep up with changes to WHO
and Kenya Ministry of Health protocols. Several
students also voiced concern that one unintended
consequence of the PartoPen might be a decrease in
situational awareness, creating too great a reliance
on the pen for instructions and decision support in an
actual labor and delivery scenario. This was
explored in the maternity ward study, and was not
observed by researchers or stated by nurse
participants.
The PartoPen study at the UoN suggests that
using the PartoPen system in classrooms can
improve students’ ability to correctly complete a
partograph form. The study results also suggest that
training on the PartoPen device does not
significantly affect student performance on
partograph completion tasks. The results of the
teaching and training study support the hypothesis
that a significant increase in partograph completion
and accuracy can be achieved with little or no
training on the device itself due to the intuitive
design, push-based functionality, and enhancement –
rather than replacement – of the current paper-based
system.
5 MATERNITY WARD STUDY
The second PartoPen study took place at Kenyatta
National Hospital (KNH) and Pumwani Maternity
Hospital (PMH). The goals of this study were to
evaluate the PartoPen for usability in labor wards,
determine if PartoPen use impacts partograph
completion, and to investigate the broader impacts
of the PartoPen on patient care and maternal health
outcomes.
5.1 Methodology
The maternity ward study evaluated partograph
completion rates for the month immediately prior to
the introduction of the PartoPen, and for the month
when the PartoPen was in use. “Completion” was
measured using a partograph completion rubric
previously developed by KNH staff for hospital
administrative purposes. According to this rubric, a
complete partograph has measurements for all of the
partograph form sections, and a complete labor
summary. A research assistant scanned the 369
partograph forms completed in the month prior to
PartoPen introduction. During the month of
PartoPen use, 457 partograph forms were initiated.
There were three phases in the introduction of
the PartoPen system at KNH and PMH: (1) training
nurses how to use the PartoPen system, (2)
introducing the PartoPen system for use during 2-3
shifts per day, and (3) establishing sustainable
infrastructure and gradually reducing researcher
supervision in the labor wards.
During the first phase, small groups of nurses
received a 10-20 minute introduction to the project
and were trained on how to effectively use the
system during their shift. Nurses were given a
demonstration of the PartoPen functionality to
introduce them to features of the system (reminders,
audio decision-support, and additional instruction
access), as well as a brief tutorial on exchanging
pens during shift changes.
In phase two, researchers introduced the
PartoPen system in both KNH and PMH labor wards
during the day shifts – approximately 7:30AM until
6:00PM. During the introduction week, the PartoPen
ThePartoPeninTrainingandClinicalUse-TwoPreliminaryStudiesinKenya
117

functionality and the study design were adjusted to
fit various environmental factors that had previously
been unknown, such as modifying reminder sounds
and text wording to account for noisy and busy
environments, and simplifying the patient reminder
ID system to allow nurses to create short,
personalized identifiers for patients, rather than
relying on the handwriting recognition in the pen to
capture the patient’s full name.
Table 3: Survey questions that nurses were asked to
answer after three weeks of using the PartoPen system.
Nurse Survey Questions
1) Before the PartoPen project, how would you rate
your level of expertise using the partograph form (on a
scale of 1 – 10)?
2) After the PartoPen project, how would you rate your
level of expertise using the partograph form (on a scale
of 1 – 10)?
3) On average, how many patients in active labor do
you care for during one night shift? (Circle one of the
ranges below)
4) On average, how many patients in active labor do
you care for during one day shift? (Circle one of the
ranges below)
5) Before the PartoPen project, for what percentage of
your patients did you complete a partograph? (Circle
one of the ranges below)
6) After the PartoPen project, for what percentage of
your patients did you complete a partograph? (Circle
one of the ranges below)
7) On a scale of 1 – 10, rate your satisfaction with the
PartoPen project in terms of usability (i.e., ease of use,
functionality, instruction clarity, etc.)
8) On a scale of 1 – 10, rate your satisfaction with the
PartoPen project in terms of usefulness (i.e., level of
patient care, level of job satisfaction, amount of time
spent on tasks, etc.)
During the third phase, no changes were made to
the code or the study design in order to keep study
conditions consistent for data collection purposes.
Quantitative data was collected using a back-end
logging system on the digital pens, which was
downloaded every day at the beginning of the
morning shift. Data logged by the pens included the
following time-stamped variables: when audio
prompts were played, which audio prompts were
played when measurements were made, how many
times instruction buttons were tapped, when the
partograph form was started and completed, and
which pen completed the form. Qualitative
observations were also recorded during the three
weeks of PartoPen use.
At the end of the three-week use period, nurses
were asked to complete a survey on their experience
before and during the PartoPen project (see Table 3).
5.2 PartoPen Software Implementation
In the PartoPen implementations at KNH and PMH,
half-hour and four-hour reminders were enabled and
activated by plotting a fetal heart rate measurement
or a cervical dilation measurement, respectively.
When a reminder would play, the patient’s name and
the type of measurement needed would scroll five
times across the OLED display.
Throughout the labor monitoring process, if a
nurse plots a measurement indicating potential labor
abnormality, the decision support functionality is
activated, a sound is played, and text scrolls across
the OLED display indicating the available options
for the patient.
The number of audio instructions for the
maternity ward implementation was reduced,
because researchers discovered that nurses rarely
used the audio instruction functionality, and the
audio was unnecessarily taking up valuable space on
the pen. The most common instance of nurses using
the instruction buttons was to teach students doing
their clinical rotations how to use the partograph. To
better facilitate the process of nurses using the
system to teach students, researchers added the full
set of audio prompts back onto the pens during the
first week of implementing the system in the labor
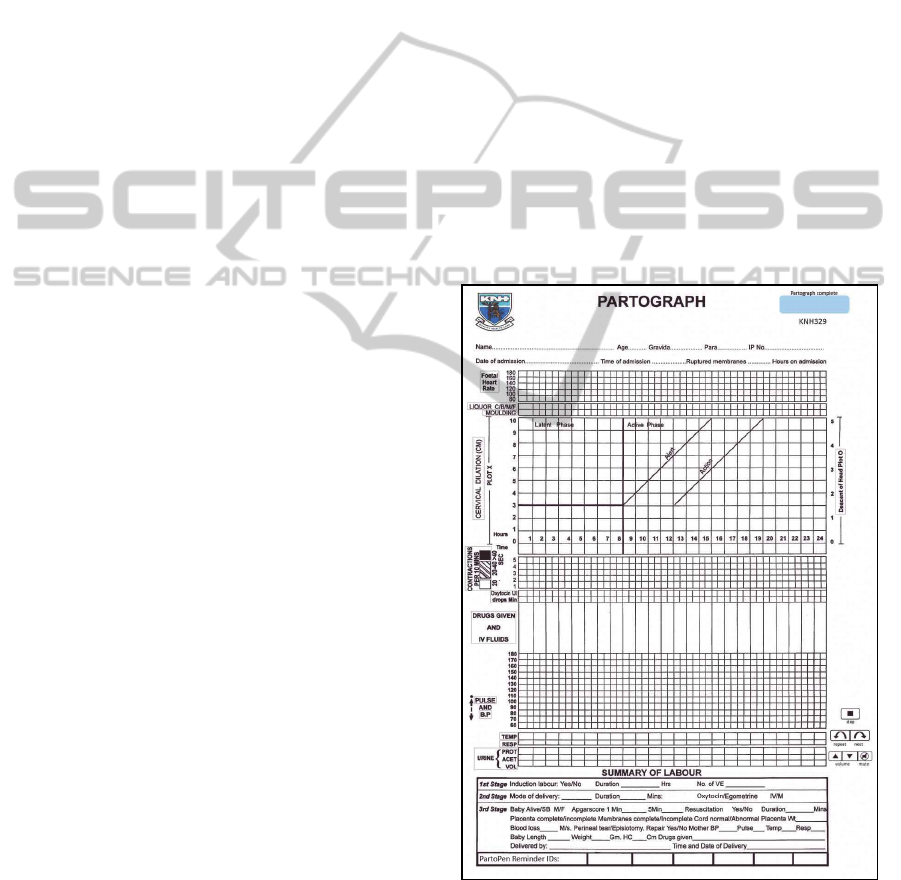
wards. In the Appendix, the partograph that was
used for the KNH maternity ward study is shown.
The boxes (buttons) around the text on the left side
of the form can be tapped repeatedly to access the
use instructions mentioned above.
5.3 Preliminary Results
5.3.1 Quantitative Results
During the maternity ward study three types of
quantitative data were collected: the 369 scored
patient partographs collected prior to PartoPen
introduction, scored patient partographs during the
period of PartoPen use, and survey responses from
nurses who had completed the three-week usage
period. This paper focuses on the results of the
surveys, as data analysis on the partograph forms is
not yet complete.
After three weeks of using the PartoPen system
consistently on every shift, nurses were asked to fill
out a short survey that captured demographic
information about the participant, and gathered
HEALTHINF2013-InternationalConferenceonHealthInformatics
118

before-and-after information about PartoPen use.
The survey consisted of eight Likert scale questions,
and six free-form response questions.
On average, nurses self-reported an
improvement of +2, on a scale of 1 to 10, in
partograph expertise during the PartoPen project, a 9
out of 10 for usability of the PartoPen, and a 9.2 out
of 10 for usefulness. Nurses also reported that the
number of partographs they completed during the
PartoPen study was, on average, 25% more than
they completed before the study. This increase in
partograph completion rates is supported by initial
data analysis on the partograph forms, and by an
internal report by the hospital administration. In
addition to the functionality provided by the
PartoPen, which encouraged higher rates of
partograph completion, the general increase in
conversation and interest in the partograph due to
the PartoPen study was also a likely contributing
factor to the improved partograph completion rates.
Overall, the quantitative data gathered from the
surveys suggest an increase in partograph
knowledge among nurses, an increase in the number
of partographs completed, and strongly positive
perceptions of the PartoPen’s usability and
usefulness.
5.3.2 Qualitative Observations
During the first week of the PartoPen
implementation, researchers were present in the
labor wards from 7:30AM until 6:00PM to answer
questions, facilitate PartoPen handoffs during shift
changes, and to observe usage of the PartoPens. The
most significant observations fall into two
categories: digital pen design and PartoPen
functionality.
Digital Pen Design
The nurses emphasized the necessity of a functional
cap for the pens to keep ink from getting on their
uniforms. One nurse, after getting pen on her
uniform, remarked “Here, take it back, I won't use it
unless there is a cap - or I'll bring you my laundry!"
Caps for the pens were the distributed to the nurses,
although the currently available cap for the
Livescribe Echo pen was considered difficult to use.
A makeshift lanyard system was created to allow
nurses to wear the pens around their necks, but a
shirt clip or similar way to attach the pen to a pocket
would be preferred. Other pen design improvement
suggestions included having different colors of ink
available, and making the pen thinner and lighter.
PartoPen Functionality Observations & Changes
During the first week of the study (the
implementation and training phase), researchers
observed nurses getting reminders from the pen,
shaking their heads, and dismissing the reminder.
Upon further investigation, researchers realized that
the reminders nurses were receiving were for
patients who had already delivered or had received a
cesarean section. New functionality was added to the
PartoPen that enabled a reminder ID system and a
reminder cancelation system. The reminder ID
system (pictured in the Appendix under the
“Summary of Labor” section) was implemented to
give nurses a way to create custom identifiers for
patients that would scroll across the display when a
reminder for that patient was triggered. Nurses write
the identifier in one of the reminder ID boxes at the
bottom of the form when a patient is admitted. The
handwriting recognition engine in the pen interprets
and stores this identifier and displays it for all future
reminders for this patient. The reminder cancelation
system addresses the issue of outstanding reminders
for a patient that has already delivered or has been
prescribed a cesarean section. A blue box at the top
of the form (pictured in the Appendix in the top
right-hand corner of the form) was created for nurses
to sign their initials in once a patient has delivered or
has been transferred for a cesarean section. The act
of signing in the blue box cancels any existing
reminders for that patient, and thus nurses will not
receive unnecessary reminders.
The reminder and decision support functionality
used in the maternity ward study relied on distinct
pen tones and scrolling text on the pen. Nurses
informed the researchers that while this
implementation did reduce the distractions
associated with long audio prompts, they were
unable to look at the OLED display to see which
patient needed an exam if they were in the middle of
another delivery. The text displayed for both
reminders and decision support prompts is only
scrolled five times before the display returns to
showing the current clock time. Several
modifications could be made to address this problem
including implementing a repeat button that will re-
scroll the most recent text, continuing to scroll the
text until the nurse uses the pen again, or
implementing an audio based reminder system that
uses an audio recording (made by the nurses
themselves) of the patient’s name, which is played
back for that patient’s reminders. The last solution is
currently being developed, and will be tested in the
next iteration of PartoPen studies.
Displaying the time on the OLED display on the
pens proved to be one of the most important features
of the PartoPen system. Because measurements and
exams are time-based, and each observation is
ThePartoPeninTrainingandClinicalUse-TwoPreliminaryStudiesinKenya
119

associated with the time it is taken, nurses often ask
each other for the clock time. Nurses often use their
mobile phones to get the time, but hospitals are
increasingly restricting the use of personal phones
during nurses’ shifts to reduce distractions and
increase nurses’ involvement with the patients.
Nurses therefore began using the PartoPen to
determine the exact time measurements were taken,
increasing the accuracy of recorded data.
6 CONCLUSIONS & FUTURE
WORK
The preliminary results of the nursing student study
indicate that student performance on a partograph
worksheet completion task improves when using the
fully functional PartoPen system. A significant
finding of this study was that the PartoPen
significantly improved student scores on the more
complex patient case study, suggesting that
reinforcement of existing knowledge, and real-time
decision-making may be amplified and improved by
using the PartoPen system. Based on the positive
results from the student study at UoN, researchers
are currently working with other Kenyan nursing
schools to integrate the PartoPen into their existing
nursing curricula. Additionally, the authors intend to
examine how the PartoPen can be used to facilitate
initial training on the partograph, and the transition
from in-class partograph instruction to clinical use of
the partograph form.
While the maternity ward study is on going,
preliminary results suggest that using the PartoPen
system increases partograph completion rates and
increases nurses’ accuracy when completing
partographs. In addition, nurses were satisfied with
both the usability and the usefulness of the PartoPen,
suggesting that continued and sustainable use is
possible in this environment.
After the three-week period of PartoPen use,
twenty pens were left at KNH to continue being used
by nurses in the labor wards. At the time of writing,
these pens have been in use at KNH for a total of
seven weeks, and data continues to be collected and
analysed by local researchers.
Future work on the PartoPen project will focus
on expanding the number of study sites to include
clinics at various levels of healthcare, including rural
health clinics, dispensaries, and district level
facilities. Future research will also expand on the
nursing student study data described in this paper,
and evaluating the impact of long-term PartoPen use
in the classroom, and how this affects performance
among students during clinical rotations and
evaluations.
The next step in determining the impact of the
PartoPen system is to expand the goals of the study
from looking solely at completion rates to include
how partograph completion (or incompletion) affects
patient outcomes. Currently researchers are
collaborating with a larger maternal health project
based at KNH to study the effects of PartoPen use
on maternal and fetal outcomes.
ACKNOWLEDGEMENTS
This research is funded by a Gates Grand Challenge
in Global Health grant, a National Science
Foundation Graduate Research Fellowship, and by
the ATLAS Institute at the University of Colorado
Boulder. We would like to thank the leadership of
KNH, PMH, and the UoN, particularly Dr. John
Ong’ech and Dr. Grace Omoni, for their support and
cooperation during the PartoPen studies, and all of
the students, nurses, and staff who participated in the
studies. Maya Appley, Addie Crawley, Sara
Rosenblum, and Vincent Ochieng contributed
significantly to this study.
REFERENCES
World Health Organization. 2010. Fact Sheet. World
Health Organization Media Center for Maternal
mortality. Retrieved June 20, 2011
http://www.who.int/mediacentre/factsheets/fs348/en/in
dex.html
Stanton, M.E. 2010. A case for investment in maternal
survival and health. Presentation at the Woodrow
Wilson International Centre for Scholars, Washington,
DC [online]. Available from:
http://www.wilsoncenter.org/events/docs/Mary%20Ell
en%20Stanton%20Presentation.pdf [Accessed 30
April 2012].
Friedman, E., 1954. The graphic analysis of labor.
American Journal of Obstetrics and Gynecology, vol.
68, no. 6, pp. 1568-1575.
Mugerwa, K. Y., Namagembe, I., Ononge, S., Omoni, G.,
Mwuiva, M., Wasiche, J. The use of Partographs in
Public Health Facilities in Kenya. Available from:
http://www.rcqhc.org/download/FP_DOCS/Final_pap
er_Kenya.pdf [Accessed 30, April, 2012].
Lawn, J. and Kerber, K. 2006. Opportunities for Africa’s
newborns: Practical data, policy and programmatic
support for newborn care in Africa. Geneva: World
Health Organization.
Levin, L. 2011. Use of the Partograph: Effectiveness,
Training, Modifications, and Barriers: A Literature
HEALTHINF2013-InternationalConferenceonHealthInformatics
120
Review. Washington, DC, United States Agency for
International Development, Fistula Care,
EngenderHealth: 28.
Lavender, T., Omoni, G., Lee, K., Wakasiaka, S., Waitit,
J., Mathai, M. 2011. Students’ experiences of using
the partograph in Kenyan labour wards. African
Journal of Midwifery and Women’s Health 5(3):117-
122.
Underwood, H. 2011. Using a Digital Pen to Improve
Labor Monitoring and Reinforce Birth Attendant
Training. University of Colorado at Boulder, ATLAS
Institute. Retrieved August 1, 2011 from
http://www.colorado.edu/atlas/technicalreports.
Underwood, H., Sterling, S. R., Bennett, J., 2012.
Improving Maternal Labor Monitoring in Kenya
Using Digital Pen Technology: A User Evaluation.
Proc. Global Humanitarian Technology Conference,
2012.
Hartung, C., Anowka, Y., Brunette, W., Lerer, A., Tseng,
C., Borriello, G. 2010. Open Data Kit: Tools to Build
Information Services for Developing Regions. In
Proceedings of the ACM/IEEE Conference on
Information and Communication Technology for
Development (London, United Kingdom, December
13-16, 2010).
Grameen Foundation. 2010. Mobile Technology for
Community Health. Retrieved July 2, 2011 from
http://www.grameenfoundation.org/what-we-
do/technology/mobile-health
Parikh, T. 2005. CAM: A Mobile Interaction Framework
for Digitizing Paper Processes in the Developing
World. In Proceedings of ACM Symposium on User
Interface Software and Technology (UIST) (Seattle,
Washington, October 23-26, 2005).
Sherwani, J. et al., 2007. HealthLine : Speech-based
Access to Health Information by Low-literate Users.
Svoronos, T. et al., 2010. CommCare : Automated Quality
Improvement To Strengthen Community-Based
Health The Need for Quality Improvement for CHWs.
Health (San Francisco).
Derenzi, B., Mitchell, M., Schellenberg, D., Lesh, N.,
Sims, C., Maokola, W., 2008. e-IMCI : Improving
Pediatric Health Care in Low-Income Countries.
Dell, N., Breit, N., Crawford, J., 2012. Digitizing Paper
Forms with Mobile Imaging Technologies. Second
Annual Symposium on Computing for Development.
Ratan, A. L., Chakraborty, S., Chitnis, P. V., Toyama, K.,
Ooi, K. S., Phiong, M., Koenig, M. 2010. Managing
microfinance with paper, pen and digital slate. Scientia
196(36).
Yeh, R., Liao, C. et al. 2006. ButterflyNet: a mobile
capture and access system for field biology research.
In Proceedings of the SIGCHI conference on Human
Factors in computing systems (Montreal, Quebec,
Canada, April 22-27, 2006).
Cowan, L. P., Griswold, W., Weibel, N., Hollan, J. 2011.
UbiSketch: Bringing Sketching out of the Closet. La
Jolla, University of California, San Diego: 10.
Song, H., Benko, H., et al. 2011. Grips and gestures on a
multi-touch pen. In Proceedings of the 2011 annual
conference on Human factors in computing systems
(Vancouver, BC, Canada, May 7-12, 2011).
Landau, S., Bourquin, G., van Schaack, A., Miele, J. 2008.
Demonstration of a universally accessible audio-haptic
transit map built on a digital pen-based platform. 3rd
International Haptic and Auditory interaction Design
Workshop (Jyvaskyla, Finland, September 15-16,
2008).
Sarcevic, A. 2010. TraumaPen: Supporting
Documentation and Situational Awareness through
Real-Time Data Capture and Presentation in Safety-
Critical Work. Computer Science Department Tech
Report. University of Colorado at Boulder
Jhpiego Corporation. 2011. E-Partogram. Saving Lives at
Birth: A Grand Challenge for Development. Retrieved
from http://www.savinglivesatbirth.net/summaries/35
Mathai, M. 2010. WHO Partograph E-learning Course.
World Health Organization. Retrieved from
http://streaming.jointokyo.org/viewerportal/vmc/playe
r.do?eventContentId=995
APPENDIX
ThePartoPeninTrainingandClinicalUse-TwoPreliminaryStudiesinKenya
121
